Abstract
Despite the fact that the effect of sex on the occurrence of cancers has been studied extensively, it remains unclear whether sex modifies familial aggregation of cancers. We explored sex-specific familial aggregation of cancers in a large population-based historical cohort study. We combined cancer and population registry data, inferring familial relationships from birth municipality-surname-sex (MNS) combinations. Our data consisted of 391,529 incident primary cancers in 377,210 individuals with 319,872 different MNS combinations. Cumulative sex-specific numbers of cancers were compared to expected cumulative incidence. Familial cancer risks were similar between the sexes in our population-wide analysis. Families with concordant cancer in both sexes exhibited similar sex-specific cancer risks. However, some families had exceptionally high sex-specific cumulative cancer incidence. We identified six families with exceptionally strong aggregation in males: three families with thyroid cancer (ratio between observed and expected incidence 184.6; 95% credible interval (95% CI) 33.1–1012.7, 173.4 (95% CI 65.4–374.3), and 161.4 (95% CI 29.6–785.7), one with stomach (ratio 14.4 (95% CI 6.9–37.2)), colon (ratio 15.5 (95% CI 5.7–56.3)) cancers and one with chronic lymphocytic leukaemia (ratio 33.5 (95% CI 17.2–207.6)). Our results imply that familial aggregation of cancers shows no sex-specific preference. However, the atypical sex-specific aggregation of stomach cancer, colon cancer, thyroid cancer and chronic lymphocytic leukaemia in certain families is difficult to fully explain with present knowledge of possible causes, and could yield useful knowledge if explored further.
Similar content being viewed by others
Introduction
Global disparities in the incidence of cancers between males and females are well documented1. Incidence differences of varying magnitude between the sexes are observed in almost all cancers: yearly incidence rates are greater in men in almost all non-sex-specific malignancies, except thyroid cancer2,3. This phenomenon has classically been explained by biological differences, in addition to unequal exposure to environmental, lifestyle and occupational factors. For example, in Sweden, peaks in lung cancer incidence over time have followed the divergent prevalence peaks of smoking in males and females4. The contribution of biological mechanisms is, for example, supported by patterns of sex differences in childhood cancers5. Sex-dependent modification of environmental effects also occurs, as for example the incidence rate of hepatocellular carcinoma is different in men and women with chronic hepatitis B infection, but not with hepatitis C infection6.
Familial aggregation of cancer can be caused by both genetic and shared environmental factors7, as well as stochastic phenomena. The offspring and siblings of cancer patients are at a significantly increased risk of cancer8,9. Familial aggregation can also be modified by parental lifestyles, such as physical inactivity, being passed onward to children10.
Sex does not appear to greatly modify the risk of familial cancer, as parent–offspring pairs of concordant cancer patients in Sweden exhibited abnormal sex-specific aggregation of only thyroid adenocarcinoma in male offspring of the proband11. Singular studies of familial cancers have observed sex-related aggregation effects12,13.
While sex disparities of cancer result from a complex interplay of different factors14, in some cases cancer may result rather directly due to predisposing genetic variants in the sex chromosomes, as a few X-linked cancer syndromes have been described15. Mutations in sex chromosomes have been implicated to have numerous roles in cancer16. Thus, it seems plausible that germline variation in sex chromosomes affects lifetime cancer risk as well. However, associations of sex and lifetime risk of familial cancer has been studied rarely. Thus, additional studies are warranted; detecting associations in an epidemiological setting would allow the formulation of additional research hypotheses, which in turn might reveal novel information about cancer biology and may be of importance in monitoring families with cancer.
We studied population-based sex-specific familial aggregation of cancers, inferring familial relationships indicated by shared surnames at birth and birth municipalities of cancer patients. Our model is an extension of the model introduced by Kaasinen et al.17 to include sex-specific effects. Finns are a population isolate with a unique history of bottleneck events, and subsequent genetic drift. This, in parallel with the whole-population setting of our study, provides a unique perspective on this seldom studied subject. There appears to be no sex-specific difference in aggregation population-wide, but individual families may be affected by rare phenomena as we observed notable sex-specific cancer clusters.
Methods
We explored familial sex-specific aggregation of cancers in a population-based historical cohort setting. We used all diagnosed primary cancers reported in the Finnish Cancer Registry (FCR) starting from 1953 up until the end of 2016. Cancers were classified on the basis of topography, morphology and behaviour codes based on ICD-O-3, and grouped to ICD-10-equivalent groups according to official FCR classification18,19. From this data we filtered non-sex-specific cancer types that are recorded and reported in FCR’s yearly statistics. Breast cancer, which can also occur in males, was left out of the analysis due to the very large observation differential. Of the hematologic malignancies, we included major ICD-10 cancer types that had a long and reliable time series in the registry, dating back to at least the 1960s. Non-hodgkin lymphomas were excluded from the analysis as these are separated in FCR’s yearly statistics, and many of the malignancies comprising this group are individually too rare for reliable inference. The Digital and Population Data Service Agency of Finland collects and stores data in the Finnish Population Information System (PIS) of people who are born in or immigrate to Finland, until their emigration or death. From PIS we obtained the number of people born in each municipality, with each surname, of each sex and in each year, totaling 8,256,557 people (DVV permit 617/410/07). People were tabulated by municipality, name, and sex, creating 1 774 080 municipality-name-sex (MNS) combinations. The combination of the same birth municipality and surname at birth was the basis for inference of familiality17,20. A minimum of two people for each combination was required to reduce computational burden and stabilise the statistical inference, reducing the number to 609,406 MNS combinations.
We linked the personal identity codes of cancer patients (FCR data, permit SSY-2011-0002) to PIS data to retrieve their surnames at birth and birth municipalities (DVV permit VRK/41405/2017-2). We limited cancer patients to those born between 1870 and 2010 to reduce random variation from very small birth cohorts. We restricted the age of onset of cancers to below 80 years of age, as cancer diagnoses tend to be less reliable in the very elderly. Only primary cancer diagnoses were considered, once for each cancer type per individual. Twenty-eight study subjects without information on sex were removed. Thus, our data consisted of 391,529 cancer diagnoses in 377,210 individuals (Table 1), in 319,872 MNS combinations.
The study protocol, its use of human data, and methodology have been evaluated and approved by the Finnish Institute for Health and Welfare (THL permit 151/5.05.00/2017) and the Ethics Committee of the Hospital district of Helsinki and Uusimaa (HUS/2509/2016). All work involving patient data was carried out in accordance with the Declaration of Helsinki.
Informed consent from study participants was unnecessary as the study utilised administrative registry data not based on consent (based on the Act on the Finnish Institute for Health and Welfare 668/2008 (cancer information), Act on the Population Information System 661/2009 (other than health information) and the Act on the Secondary Use of Health and Social Data (552/2019)).
The observed number of cancers in each MNS combination was compared with an expected number, which was obtained by applying the standard cancer incidence in Finland to the MNS combination by birth cohort. The ratio between the observed and the expected number until the end of follow-up (end of 2016) is called standardised cumulative incidence ratio (SCIR) as it follows the approach of standardised incidence ratio (SIR)21, with the exception that cumulative incidences are utilised instead of age-specific rates. SCIR was used to quantify cancer risk in each MNS combination compared to the average risk in the population.
SCIRs were modelled using a hierarchical Bayesian Poisson regression. Based on the distribution of SCIRs in site-specific MNS combinations, we simulated two risk coefficients for each combination. The regression model was fitted separately to the data of each site and sex using Markov chain Monte Carlo simulation. Bayesian hierarchical modelling was used as a statistical smoothing method to manage the problem of multiple comparisons due to the large number of combinations of family name and municipality. The computation of all MNS combinations is prohibitively cumbersome due to their large number, and because the aim of this study was to differentiate inferred families by their cancer risk, we excluded from each analysis all MNS combinations with no cancers. The model, prior distributions, details of the simulation, and a directed acyclic graph of the model are available in Online Resource 1.
For each site and sex, we estimated the proportion of cancers in the high versus low risk coefficient groups (risk coefficient group proportion), SCIR averages both overall and in the higher coefficient group, and the ratio of these SCIR averages (SCIR ratio). We compared derived proportions of groups between sites and sexes, based on the assumption that SCIR distribution shape, and thus risk coefficient group proportion, was insensitive to the scale of SCIRs within each analysis. We estimated male–female ratios of the risk coefficient group proportion and the SCIR ratio.
In addition, we calculated cancer-specific posterior probabilities of the risk coefficient group proportion and normalised SCIR estimates in each MNS combination. We compared the amount of MNS combinations with higher risk coefficient posterior probability over 0.9 between males and females. We examined the full detailed cancer histories for MNS combinations with higher risk coefficient posterior probability over 0.95. For SCIRs we chose to use the median as a summary statistic as some SCIR posterior distributions were skewed, in which cases the arithmetic mean was shifted towards the tail of the distribution and the median was more robust. Normalised SCIRs were derived from the posterior medians of MNS combination SCIRs by subtracting each MNS combination’s SCIR median from its respective cancer-sex analysis set’s median SCIR, and dividing it by the standard deviation. Normalised SCIR thus measures an MNS combination’s divergence from the site-and-sex SCIR median as the number of standard deviations from the median, enabling the detection of atypical SCIRs. A subset of MN combinations presenting concordant cancer in both sexes was extracted from the data to study intra-family effects, yielding 20,925 such combinations with a total of 61,855 individuals.
Data processing was done using R version 3.5.1 utilising the package data.table version 1.12.2. Figures were generated using R package ggplot2 version 3.2.122.
Results
Cancer sites for which more than 55% of all diagnosed individuals were female included the gallbladder and bile ducts, anus, thyroid gland, as well as brain, meninges, and central nervous system (CNS, Table 1). Similar numbers of cancer in both sexes were observed in salivary gland cancer, colon cancer, melanoma of the skin, myeloma and other plasma cell tumours, and acute myeloid leukaemia (AML). The remaining 18 sites had an excess of diagnoses in males. Males had on average a much higher excess number of familial cancers in the lung and trachea (1.48 cancers per MNS vs. 1.14 in females). The thyroid gland was the only site with a noticeable excess of familial female cancers (1.09 cancers per MNS vs. 1.03 in males).
Male–female ratios of the risk coefficient group proportions and SCIR ratios are shown in Table 2, with complete aggregate results available in Online Resource 2. No differential familial aggregation between sexes was observed. Male–female ratio of SCIR varied from 0.87 (95% credible interval (95% CI) 0.35–1.73) in nose and sinuses to 1.04 (95% CI 0.41–2.19) in chronic myeloid leukaemia. The most deviated male/female ratio of risk coefficient group proportion with reasonable variation was in the lung and trachea (0.83 (95% CI 0.61–1.12)), with a male–female SCIR ratio of 0.95 (95% CI 0.87–1.04). The risk coefficient group proportion of male lung and trachea cancers was 0.53 and for females 0.64 (Online Resource 2).
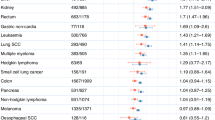
Next we attempted to detect any atypically aggregating families for all cancer sites by normalising the posterior SCIR medians by each site-and-sex grouping (Fig. 1). In most studied cancers, posterior SCIR median distributions were very similar between the sexes. Male MNS combinations tended to have higher cancer risks. Males had more high-risk MNS combinations in the stomach (21 clusters more than females), colon (16), oesophagus (13), pancreas (11), CNS (10), kidney (10), liver (8), rectum and rectosigmoid (6), CLL (5), larynx and epiglottis (5), AML (3), acute lymphoblastic leukaemia/lymphoma (ALL, 3), lip (1), and myeloma and other plasma cell tumours (1). Females had more high-risk MNS combinations in the thyroid gland (25), lung and trachea (5), melanoma of the skin (4), and gallbladder and bile ducts (4). Posterior probabilities of higher risk coefficient > 0.95 were identified only in male MNS combinations with clustered observations. These were in thyroid cancer (three clusters, with (1) two medullary carcinomas; SCIR 184.6 (95% CI 33.1–1012.7), normalised SCIR 6.68, (2) two papillary carcinomas; SCIR 161.4 (95% CI 29.6–785.7), normalised SCIR 5.6, (3) four medullary carcinomas, one follicular carcinoma, and one epithelial carcinoma; SCIR 173.4 (95% CI 65.4–374.3), normalised SCIR 6.15), colon cancer (one cluster with three adenocarcinomas; SCIR 15.5 (95% CI 5.7–56.3), normalised SCIR 5.40), CLL (one cluster of three individuals; SCIR 33.5 (95% CI 17.2–207.6), normalised SCIR 5.88), and stomach cancer (one cluster, with three adenocarcinomas, two diffuse type adenocarcinomas, and one carcinoid tumour; SCIR 14.4 (95% CI 6.9–37.2), normalised SCIR 8.14). These clusters exhibited no concordant cancer in women, except the six-patient thyroid cancer cluster which included a thyroid cancer observation in one woman. The stomach cancer cluster also co-occurred with two female lung cancers and one Hodgkin lymphoma.
Normalised standardised cumulative incidence ratio (SCIR) estimates of municipality-name-sex combinations. Violin plots for central 95% of normalised SCIRs. MNS combinations allocated to higher risk coefficient group with probability greater than 90% are indicated by dots, with red colour and larger dot size used to emphasise most extreme probabilities (greater than 95%). Sites presented in the same order as in Tables 1 and 2, with abbreviated names. SG salivary glands, SI small intestine, rectal rectum and rectosigmoid, biliary gallbladder and bile ducts, nasal nose and sinuses, larynx larynx and epiglottis, lung lung and trachea, melanoma melanoma of the skin, urinary bladder and urinary tract, CNS brain, meninges, and central nervous system, TG thyroid gland, HL Hodgkin lymphoma, myeloma myeloma and other plasma cell tumours, ALL acute lymphoblastic leukaemia/lymphoma, CLL chronic lymphocytic leukaemia, AML acute myeloid leukaemia, CML chronic myeloid leukaemia.
As higher risk coefficient assignment with P > 0.95 was only observed in males, we examined whether sex affected risk coefficient assignment by studying MN combinations with concordant cancer in males and females. Males and females are likely to be categorised similarly in each MN combination. This is indicated in the contour plot in Fig. 2a, in which male and female higher risk coefficient posterior probabilities are plotted for all sites combined. Lung and trachea cancers are numerous enough to show up in the figure as their own separate cluster, which has been isolated in Fig. 2b. In the central 10% of MN combinations with concordant lung cancer in the contour plot, females are ~ 0.15 more likely to be assigned a higher risk coefficient. In colon cancer (Fig. 2c) the contours are skewed towards a higher probability in males, implying a family-level effect similar to the whole-population aggregation result of an elevated male–female ratio of colon cancer risk coefficient group proportion, shown in Table 1. A visualisation of thyroid gland clusters is shown in Fig. 2d to emphasise the sex difference in the cluster with six male observations and one female observation.
Higher risk coefficient posterior probability (high risk) in males versus in females, in inferred families with concordant cancer. (a) All sites, (b) lung and trachea, (c) colon, (d) thyroid gland. Contours start from ~ 99% of data points encompassed, followed by 90%, after which decrements are by each 10%. Observations remaining outside the largest contour visualised as points. Diagonal line drawn as a visual reference for equal male and female risk coefficient posterior probability.
Discussion
We studied sex-specific familial aggregation of cancer with nationwide population-based registry data. No population-wide differential of familial aggregation between males and females was detected in any of the studied cancers. Singular cancer clusters of inferred families emerged, with the largest cancer risk increases observed in male MNS combinations with thyroid cancer, colon cancer, CLL, and stomach cancer. Risk coefficient assignment probabilities of MN combinations with concordant cancer follow a correlated pattern between males and females in our simulations, indicating only minor or rare sex-dependent modification of familial risk.
In this study, we inferred familial relationships from birth surname and birth municipality combinations utilising information extracted from a population registry, an approach which has been previously applied with success in Finnish cancer studies17,20. This has allowed us to use all cancers in Finland in the current analysis, with the large number of data points available improving statistical power to detect MNS combinations with high cancer risk. Our statistical modelling accounts for complex random variation between clusters, and decreases false positive findings by utilising Bayesian shrinkage. The high quality of cancer registration for decades and the quality of the population registry decrease biases and variation from these data23,24.
As we lack both historical data of population levels in each municipality and the death or emigration years of individuals not present in the FCR, we are unable to calculate person-years at risk in each MNS. This prevents the calculation of expected number of cases by age group and subsequently SIRs, and thus we use SCIR as our measure. Our model estimates SCIR for a cancer only in MNS combinations with observations, while expected cancer rates are calculated based on the whole population prior to inference. This biases the model offset, which in turn overestimates risk with a varying degree and makes direct comparison of different sex-and-site analyses unfeasible. Thus, we mainly use our sex-and-site-specific risk metrics as intermediate results when describing effects between sexes and inferred families. The purpose of our dichotomous risk categorisation in simulations was to manage the low number of cancers in each MNS combination, due to which the SCIR estimates were unstable. This limitation was counteracted by the large number and high variability of families and family sizes, with which we were able to identify the distributions of SCIRs in MNS combinations for each cancer site.
The method of inferring familial relationships by surname at birth has two challenges. First, common surnames can be shared by multiple individuals with no particular familial relation, leading to inevitable misclassification of some unrelated individuals as being related. The range of surnames in use is large, however. For example, according to DVV open data, the 50 most common surnames in 2020 accounted for approximately 6.5% of the population, and the 10 most common for 1.9%. Familial misclassification is considered to be non-differential, as healthy individuals and persons with cancer are misclassified similarly. Previous studies using non-sex-specific MN combinations inferred from surname and birth municipality17,20 have validated their findings with genealogy, with the majority of inferred families in observed high-risk clusters consisting of first-degree relatives.
The second challenge is that some MNS combinations and cancer families are misclassified as affected children might not have the same surname at birth as the affected same-sex parent. Finnish women have customarily taken their husband’s surname upon marriage, and children born in the marriage typically receive their father’s surname at birth. Similarly, male MNS combinations may be misclassified if a male offspring is born out of wedlock, as they may receive the mother’s surname. The magnitude of this effect is difficult to assess exhaustively. Changing surname upon marriage was mandatory through the 1930s to 1980s, but before this time the custom has varied in adoption over time, by region, and by socioeconomic group25. Children born out of wedlock have received their mother’s surname by default. Children born out of wedlock numbered 7–9% from the late nineteenth century until the Soviet-Finnish wars, after which the rate reduced to around 5% until the 1970s26. Since then the rate has steadily increased to a contemporary rate of 40–45% according to data from Statistics Finland. Both female and male MNS combinations had a median size of 12.
Lung and trachea cancer analyses were consistently deviating towards excess risk in females. Lung cancer risk is increased in the offspring of lung cancer patients regardless of the affected parent’s sex, with offspring cancer male–female ratios skewing towards an excess in females11. Young never-smoker women have an abundance of lung adenocarcinoma27, and molecular studies support that the phenotype is distinct from what is observed in smokers, and likely contributed to by cancer syndromes and other predisposing genetic factors28. Tobacco smoking is known to increase the risk of lung cancer, and it has been a wide-spread habit in Finnish males aged 15–64 with roughly 35% having been daily smokers in the 1970s and 23% in 201029. The incidence patterns of male lung cancer may thus be fundamentally different from other combinations in our analysis. A similar but less pronounced effect may also be present in females due to passive smoking30.
The cluster analysis shows three clusters of male thyroid cancer with high SCIRs and a very high posterior probability of higher risk coefficient. A combination of a low background rate and an elevated familial risk in males, inverting the sex ratio when familial observations are compared to the sex ratio in background incidence, has previously been described in thyroid adenocarcinoma11. A similar effect may cause our cluster observations, with the exception that the morphological spectrum we observed was mixed.
Of all the clusters found in our data, the stomach cancer cluster with six patients was the most deviated from its respective group (median SCIR 8.14 standard deviations from male stomach cancer SCIR median as indicated by normalised SCIR). Stomach adenocarcinomas and carcinoid tumours are observed in the tumour spectrums of multiple hereditary cancer syndromes31,32, but there seems to be no overlap in strong genetic predisposition to the two tumour types.
Conclusions
Our results imply that familial aggregation of cancers shows no sex-specific preference. However, the atypical sex-specific aggregation of stomach cancer, colon cancer, thyroid cancer and chronic lymphocytic leukaemia in certain families is difficult to fully explain with present knowledge of possible causes, and could yield useful knowledge if explored further.
Data availability
The data underlying this study cannot be shared due to permissions that restricts our ability to share the research data on ethical and legal grounds. Similar permission to use administrative health data from various register keepers can be applied from Findata, the Social and Health Data Permit Authority. Requests to access these data can be submitted to Findata: https://findata.fi/en/.
Abbreviations
- ALL:
-
Acute lymphoblastic leukaemia/lymphoma
- AML:
-
Acute myeloid leukaemia
- Biliary (in Fig. 1):
-
Gallbladder and bile ducts
- CLL:
-
Chronic lymphocytic leukaemia
- CML:
-
Chronic myeloid leukaemia
- CNS:
-
Brain, meninges, and central nervous system
- FAP:
-
Familial adenomatous polyposis
- FCR:
-
Finnish Cancer Registry
- HL:
-
Hodgkin lymphoma
- Larynx (in Fig. 1):
-
Larynx and epiglottis
- Lung (in Fig. 1):
-
Lung and trachea
- Melanoma (in Fig. 1):
-
Melanoma of the skin
- MN:
-
Municipality-name
- MNS:
-
Municipality-name-sex
- Myeloma (in Fig. 1):
-
Myeloma and other plasma cell tumours
- Nasal (in Fig. 1):
-
Nose and sinuses
- PIS:
-
Population Information System
- Rectal (in Fig. 1):
-
Rectum and rectosigmoid
- SCIR:
-
Standardised cumulative incidence ratio
- SG:
-
Salivary glands
- SI:
-
Small intestine
- TG:
-
Thyroid gland
- Urinary (in Fig. 1):
-
Bladder and urinary tract
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
Edgren, G., Liang, L., Adami, H.-O. & Chang, E. T. Enigmatic sex disparities in cancer incidence. Eur. J. Epidemiol. 27, 187–196. https://doi.org/10.1007/s10654-011-9647-5 (2012).
Zheng, D. et al. Sexual dimorphism in the incidence of human cancers. BMC Cancer 19, 684. https://doi.org/10.1186/s12885-019-5902-z (2019).
Li, X., Mutanen, P. & Hemminki, K. Gender-specific incidence trends in lung cancer by histological type in Sweden, 1958–1996. Eur. J. Cancer Prev. 10, 227–235. https://doi.org/10.1097/00008469-200106000-00005 (2001).
Ashley, D. J. A male-female differential in tumour incidence. Br. J. Cancer 23, 21–25. https://doi.org/10.1038/bjc.1969.3 (1969).
Huang, Y.-T. et al. Lifetime risk and sex difference of hepatocellular carcinoma among patients with chronic hepatitis B and C. J. Clin. Oncol. 29, 3643–3650. https://doi.org/10.1200/jco.2011.36.2335 (2011).
Guo, S.-W. Familial aggregation of environmental risk factors and familial aggregation of disease. Am. J. Epidemiol. 151, 1121–1131. https://doi.org/10.1093/oxfordjournals.aje.a010156 (2000).
Dong, C. & Hemminki, K. Modification of cancer risks in offspring by sibling and parental cancers from 2,112,616 nuclear families. Int. J. Cancer 92, 144–150 (2001).
Frank, C., Fallah, M., Sundquist, J., Hemminki, A. & Hemminki, K. Population landscape of familial cancer. Sci. Rep. 5, 1–8. https://doi.org/10.1038/srep12891 (2015).
Fogelholm, M., Nuutinen, O., Pasanen, M., Myöhänen, E. & Säätelä, T. Parent–child relationship of physical activity patterns and obesity. Int. J. Obes. 23, 1262–1268. https://doi.org/10.1038/sj.ijo.0801061 (1999).
Hemminki, K. & Li, X. Gender effects in familial cancer. Int. J. Cancer 102, 184–187. https://doi.org/10.1002/ijc.10676 (2002).
Yu, J. & Li, Z. The sex ratio and age of onset features of gastric cancer patients in hereditary diffuse gastric cancer families. Fam. Cancer 10, 573–579. https://doi.org/10.1007/s10689-011-9452-z (2011).
Rebora, P., Lee, M., Czene, K., Valsecchi, M. G. & Reilly, M. High risks of familial chronic lymphatic leukemia for specific relatives: Signposts for genetic discovery?. Leukemia 26, 2419–2421. https://doi.org/10.1038/leu.2012.103 (2012).
Lopes-Ramos, C. M., Quackenbush, J. & DeMeo, D. L. Genome-wide sex and gender differences in cancer. Front. Oncol. https://doi.org/10.3389/fonc.2020.597788 (2020).
Liu, Y., Wang, L. & Zheng, P. X-linked tumor suppressors: Perplexing inheritance, a unique therapeutic opportunity. Trends Genet. 26, 260–265. https://doi.org/10.1016/j.tig.2010.03.004 (2010).
Tricarico, R., Nicolas, E., Hall, M. J. & Golemis, E. A. X- and Y-linked chromatin-modifying genes as regulators of sex-specific cancer incidence and prognosis. Clin. Cancer Res. 26, 5567–5578. https://doi.org/10.1158/1078-0432.ccr-20-1741 (2020).
Kaasinen, E. et al. Nationwide Registry-based analysis of cancer clustering detects strong familial occurrence of kaposi sarcoma. PLoS ONE 8, 55209. https://doi.org/10.1371/journal.pone.0055209 (2013).
Jack, A., Percy, C., Sobin, L., Shanmugarathan, S. & Whelan, S. International Classification of Diseases for Oncology 3rd edn. (World Health Organization, 2000).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems: Tenth Revision 2nd edn. (World Health Organization, 2004).
Matikainen, M. P., Sankila, R., Schleutker, J., Kallioniemi, O.-P. & Pukkala, E. Nationwide cancer family ascertainment using Finnish cancer registry data on family names and places of birth for 35,761 prostate cancer patients. Int. J. Cancer 88, 307–312. https://doi.org/10.1002/1097-0215(20001015)88:2%3C307::aid-ijc25%3E3.0.co;2-7 (2000).
Breslow, N. E. & Day, N. E. Statistical methods in cancer research. Volume II—The design and analysis of cohort studies. IARC Sci. Publ. 82, 1–406 (1987).
Wickham, H. ggplot2: Elegant Graphics for Data Analysis (Springer, 2016).
Leinonen, M. K., Rantanen, M., Pitkäniemi, J. & Malila, N. Coverage and accuracy of myeloproliferative and myelodysplastic neoplasms in the Finnish Cancer Registry. Acta Oncol. 55, 782–786. https://doi.org/10.3109/0284186x.2015.1127416 (2016).
Leinonen, M. K., Miettinen, J., Heikkinen, S., Pitkäniemi, J. & Malila, N. Quality measures of the population-based Finnish Cancer Registry indicate sound data quality for solid malignant tumours. Eur. J. Cancer 77, 31–39. https://doi.org/10.1016/j.ejca.2017.02.017 (2017).
Kotilainen, S. Suomalaisen perheen yhteisen sukunimen lyhyt historia. Kasvatus ja Aika 10, 42–57 (2016).
Ritamies, M. Sinappikylvystä ehkäisypilleriin: Suomalaisen Perhesuunnittelun Historia (Väestöliitto, 2006).
Wakelee, H. A. et al. Lung cancer incidence in never smokers. J. Clin. Oncol. 25, 472–478. https://doi.org/10.1200/jco.2006.07.2983 (2007).
Donner, I. et al. Germline mutations in young non-smoking women with lung adenocarcinoma. Lung Cancer 122, 76–82. https://doi.org/10.1016/j.lungcan.2018.05.027 (2018).
Broms, U., Danielsson, P. & Helakorpi, S. Kohti savutonta Suomea—Tupakoinnin ja Tupakkapolitiikan Muutokset (Terveyden ja hyvinvoinnin laitos, 2012).
Trichopoulos, D., Kalandidi, A., Sparros, L. & Macmahon, B. Lung cancer and passive smoking. Int. J. Cancer 27, 1–4. https://doi.org/10.1002/ijc.2910270102 (1981).
Setia, N. et al. Familial gastric cancers. Oncologist 20, 1365–1377. https://doi.org/10.1634/theoncologist.2015-0205 (2015).
Modlin, I. M., Kidd, M., Latich, I., Zikusoka, M. N. & Shapiro, M. D. Current status of gastrointestinal carcinoids. Gastroenterology 128, 1717–1751. https://doi.org/10.1053/j.gastro.2005.03.038 (2005).
Acknowledgements
The authors thank the Academy of Finland and The Finnish Cancer Society for funding this study. The Finnish Cancer Registry and the Digital and Population Data Service Agency are acknowledged for providing data to us. CSC—IT Center for Science Ltd is acknowledged for providing compute resources. They also thank Alison London and Samantha Martin for proof-reading and editing the language used in this article.
Funding
This work was supported by the Academy of Finland, Finnish Center of Excellence Program 2018–2025 (Grant Number 312041).
Author information
Authors and Affiliations
Contributions
All authors participated in conceptualisation. J.P. and K.S. designed the analysis. M.A., S.H., J.R. and L.J.S. procured data and computational resources. K.S. and L.J.S. curated data. M.A., J.P., J.R., K.S., and L.J.S. carried out formal analysis. L.J.S. drafted figures. L.A.A. and J.P. supervised the project. J.P., K.S., and L.J.S. wrote the original draft, L.A.A., M.A., S.H., J.R. reviewed and edited. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sipilä, L.J., Seppä, K., Aavikko, M. et al. Sex-specific familial aggregation of cancers in Finland. Sci Rep 12, 15126 (2022). https://doi.org/10.1038/s41598-022-19039-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-19039-1