Abstract
This study was performed to evaluate the outcome of endovascular intervention therapy for Budd-Chiari syndrome (BCS) and compare recanalization, transjugular intrahepatic portosystemic shunt (TIPS)/direct intrahepatic portosystemic shunt (DIPS), and combined procedure treatment. For the meta-analysis, 71 studies were identified by searching four databases. The individual studies’ samples were used to calculate a confidence interval (CI 95%), and data were pooled using a fixed-effect model and random effect model. The pooled measure and an equal-weighted average rate were calculated in all participant studies. Heterogeneity between the studies was assessed with I2, and T2 tests, and publication bias was estimated using Egger’s regression test. A total of 4,407 BCS patients had undergone an endovascular intervention procedure. The pooled results were 98.9% (95% CI 97.8‒98.9%) for a technical success operation, and 96.9% (95% CI 94.9‒98.9%) for a clinical success operation. The re-intervention rate after the initial intervention procedure was 18.9% (95% CI 14.7‒22.9%), and the survival rates at 1 and 5 years after the initial intervention procedure were 98.9% (95% CI 96.8‒98.9%) and 94.9% (95% CI 92.9‒96.9%), respectively. Patients receiving recanalization treatment (98%) had a better prognosis than those with a combined procedure (95.6%) and TIPS/DIPS treatment (94.5%). The systematic review and meta-analysis further solidify the role of endovascular intervention treatment in BCS as safe and effective. It maintains high technical and clinical success and long-term survival rates. The recanalization treatment had a better prognosis and outcome than the combined procedures and TIPS/DIPS treatment.
Similar content being viewed by others
Introduction
Budd-Chiari syndrome (BCS) is a rare hepatic venous disease. It presents with thrombosis, located anywhere from the hepatic veins (HV) to the suprahepatic of the inferior vena cava (IVC). The result is an outflow obstruction of hepatic veins1,2. The obstruction of BCS is classified as primary or secondary depending on the site of hepatic vein obstruction. The obstruction site can be a thrombus inside the vein or outside the vein due to compression with tumors3. The pathogenesis of BCSs remains unclear, but some known risk factors include myeloproliferative neoplasm, use of oral contraceptive drugs, and coagulation factors4,5. An HV outflow obstruction might cause centrilobular congestion and hepatocyte necrosis. If not treated in time, this can lead to liver cirrhosis, portal hypertension, and ascites. The clinical manifestations of BCS are abdomen pain, hepatomegaly, and ascites6,7. The cause and type of BCS vary by geographical regions; in Western countries, the common cause is HV obstruction, but IVC obstruction is predominate in Eastern countries8,9. Most frequent cause of BCS is thrombophilia, which is detected in more than 84% of patients with BCS10,11. The European Association for the Study of the Liver has recommended a step-wise therapeutic algorithm for BCS. The algorithm depends on treatment response, medical therapy with anticoagulant drugs, angioplasty, stent implantation, thrombolysis, transjugular intrahepatic portosystemic shunt (TIPS), and liver transplantation12. The progressive improvement in radiological intervention therapy in the past two decades has provided a better survival rate for BCS treatment with an intervention procedure than other treatment modalities. Recently, there has been an increase in the number of BCS patients managed with endovascular intervention therapy.
This systematic review and meta-analysis aimed to evaluate the technical and clinical success rates of endovascular intervention operation and re-intervention (including re-occlusion, re-stenosis stent, and shunt dysfunctions). We evaluated the success rates after the initial intervention procedure and the survival rate at 1 and 5 years after the initial intervention procedure. Moreover, this review compares the difference in outcome between recanalization, TIPS/DIPS, and a combined procedure (recanalization and TIPS/DIPS).
Methods
Search strategy
The PubMed, EMBASE, Cochrane Library and Science-Direct databases were searched for relevant published papers. The last search was performed on May 28, 2021. The following search terms were used: Budd-Chiari syndrome, hepatic venous outflow obstruction, hepatic vein stenosis, hepatic vein occlusion, hepatic vein obstruction, supra-hepatic IVC obstruction, membranous obstruction of IVC, endovascular treatment, interventional procedure, transjugular intrahepatic portosystemic shunt (TIPS), direct intrahepatic portosystemic shunt (DIPS), percutaneous transluminal balloon angioplasty(PTBA), percutaneous transluminal angioplasty (PTA) of the hepatic vein, vascular recanalization of the hepatic vein, vascular stent implantation in the hepatic vein, and vascular stent implantation in IVC.
Selection criteria
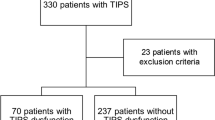
The following criteria were used to determine those studies to include: (1) study had more than ten case participants; (2) retrospective studies, prospective studies, including case series, and case–control studies were eligible; (3) all participants of any age, race, origin with a diagnosis of BCS; (4) full article papers with detailed information and statistical results of intervention treatment; and (5) there were no publication data, publication language or publication status restrictions. Exclusion criteria were: (1) duplicates studies; (2) studies that were not original papers; (3) case reports; (4) comments, (5) essays; (6) abstracts; (7) small case series; (8) not reporting relevant clinical outcomes; (9) lack of detailed results; (10) review articles; (11) less than ten patients; (12) studies unmatched inclusion criteria; (13) studies with missing survival rate, re-intervention rate or clinical success. The study selection process followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guideline flowchart (Fig. 1)13. The PRISMA checklist is provided in (Supplementary Table 1).
Data extraction
The following data were extracted for further analysis: (1) First author, publication year, enrollment period, country, number of BCS patients with endovascular intervention treated, age, gender, site of the obstruction (HV, IVC and combination), type of intervention procedures, technical and clinical success rate, rate of the re-intervention (re-occlusion, re-stenosis stent and dysfunction of shunt), and survival rate at 1 and 5 years.
Quality assessment
Studies were considered higher quality if they fulfilled all the following predetermined criteria: (1) patients were admitted to the hospital; (2) the interval of enrollment and eligibility criteria was recorded; (3) the site of obstruction of BCS patients was reported; and (4) Patients were diagnosed with BCS and treated with endovascular intervention procedures.
HV-angioplasty
When the stiff guide wire was established, a balloon dilator catheter of 12‒15 mm diameter was inserted from the right jugular vein puncture site to the obstructed part of HV/IVC via the guide wire. Next, the balloon catheter was dilated twice, and each dilatation occurred for approximately 40 s. If there was more than 30% residual stenosis on HV venography after balloon dilation then a stent was inserted in the stenosis part of the HV.
IVC-angioplasty
Venography was performed (right femoral vein or right jugular vein) to evaluate the IVC anatomy and obstruction characteristics. Next, a guidewire with a balloon catheter (25‒30 mm) was used to dilate IVC obstructive lesions. A self-expandable metallic stent was used if the IVC narrowed immediately after balloon dilatation or more than 30% residual stenosis on IVC venography after balloon dilation.
Combined HV and IVC angioplasty
Combined HV and IVC stenting were performed in patients having short-segment HV and IVC obstructions.
Recanalization
Recanalization (PTA with or without stent placement) has been used in 31 (43.66%) studies with or without stent placement. In the subgroup, we analyze the technical and clinical success rate of recanalization, re-intervention treatment, and survival rate at 1 and 5 years of recanalization procedure. It was performed with balloon dilation or endovascular stent placement in the stenosis part of HV and IVC.
TIPS/DIPS
TIPS/DIPS were used in 17 (23.94%) studies. In the subgroup, we analyze the technical and clinical success rate of TIPS/DIPS, re-intervention treatment, and survival rate at 1 and 5 years of TIPS/DIPS procedure. This was performed in symptomatic patients with non-recanalization HV obstruction with small collaterals draining into IVC, portal hypertension, refractory ascites, variceal bleeding, and long segment obstruction HV. DIPS usually used in failed TIPS, occluded three major HVs and anomalies of HVs.
Recanalization and TIPS/DIPS (combined procedures)
Recanalization (PTA with or without stent placement) and TIPS/DIPS were used in 23 (32.39%) studies. We analyze the technical and clinical success rate, re-intervention treatment, and survival rate at 1 and 5 years of combined procedures in the subgroup.
Definition
Technical success
Technical success of recanalization was defined as the complete elimination of HV or IVC obstruction and confirmed by venography. Technical success of TIPS was defined as successful placement of artificial stent between the hepatic vein and the portal vein. The stent position was confirmed by angiography, and the contrast medium flowed back into the right atrium smoothly through the intrahepatic shunt.
Clinical success
Clinical success of recanalization, combined procedures, and TIPS/DIPS was defined as an improvement of BCS related-symptoms and liver function after a technical success within day one to 90 days.
Statistical analysis
The individual studies’ sample sizes were used to calculate a confidence interval (CI: 95%). The pooled measure and an equal weighted average rate were calculated in all participant studies. The data were pooled using a fixed effect model and random effect model. Heterogeneity between studies was assessed with the I2 and T2 tests (I2 > 50% or P ≤ 0.10 was considered statistically significant heterogeneity). Publication bias was estimated using Egger’s regression asymmetry test (P ≤ 0.05 represented statistically significant publication bias). Subgroup analyses were performed according to the continent of objectives. Statistical analyses were carried out using the R-version 3.5.3 software.
Results
Study characteristics
Overall, a total of 536 papers were identified in four databases. Among them, 71 original articles9,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83 were eligible for systematic review and meta-analysis (Fig. 1). The general characteristics of the included studies are listed in Table 1. All included studies were published between 1995 and 2019. Among them, 33 (46.4%) were published between 2015 and 2019, and four (5.6%) before 2000. Most of the papers were published after 2010. Thirty-five (50%) studies were conducted in China, ten (14.2%) studies in India, four studies in the UK, three studies in Germany and Egypt, and two studies each in the USA, Italy, Netherland, and Turkey (Table 1).
A total of 4407 patients underwent endovascular intervention procedures. Among them, 98.9% of patients were considered technical successes and 96.9% achieved clinical improvement. The site of obstruction was documented in 53 (75.7%) studies, including 42.25% in HV, 30.98% in the IVC, and 26.76% in combined (HV and IVC) (Table 1). In subgroup analysis, recanalization was used in 31(43.66%) studies, combined procedures (recanalization and TIPS) in 23 (32.39%) studies, and TIPS in 17 (23.94%) studies (Table 1).
Study quality assessment
Patients were consecutively admitted in 57 (80.28%) studies9,12,14,15,16,17,18,19,20,21,22,23,24,25,28,30,31,32,33,34,35,36,37,38,39,41,42,43,44,45,47,48,49,50,51,52,53,54,55,56,57,59,64,66,68,70,71,72,73,74,75,78,79,80,81,82,83. Fifty one (71.83%) studies were considered to be of high-quality9,12,14,16,17,18,19,21,22,23,25,26,31,32,33,34,39,41,42,43,45,46,47,49,50,51,52,53,54,55,56,58,59,61,62,63,64,66,67,68,70,71,72,73,74,75,78,79,80,81,82,83 and six (8.45%) studies were of poor-quality13,15,29,65,76,77. The site of obstruction was clearly reported in 53 (75.7%) studies (Table 1). The interval of enrollment and eligibility criteria were recorded in all included studies. All patients were diagnosed with BCS and treated with endovascular intervention procedures.
The technical success rate of endovascular intervention procedures
The technical success rate of all individual studies is shown in Fig. 2.The pooled result of total technical success procedures was 98.9% (95% CI 97.8‒98.9%), with statistically significant heterogeneity among studies (I2 = 54%, P < 0.01). The pooled results of the recanalization, combined procedures, and TIPS subgroups were 97.9% (95% CI 96.8‒98.9%), 98.9% (95% CI 97.9‒99.9%), and 99.8% (95% CI 97.9‒99.9%), respectively.
The clinical success rate of endovascular intervention treatment
The clinical success rates of all cases of BCS are shown in Fig. 3. The pooled result of the total patients with a clinical success rate was 96.9% (95% CI 94.9‒98.9%), with statistically significant heterogeneity among studies (I2 = 83%, P < 0.01). The pooled results of the recanalization, combined procedures, and TIPS subgroups were 97.9% (95% CI 95.9‒99.9%), 95.6% (95% CI 92.7‒98.9%), and 94.0% (95% CI 88.5‒98.8%), respectively.
The rate of re-intervention at 5 years after initial intervention treatment
The vascular re-occlusion, stent stenosis, and shunt dysfunction at 5 years after initial endovascular intervention procedures of BCS are shown in Fig. 4. The pooled result of total re-intervention was 18.9% (95% CI: 14.7‒16.9%), with statistically significant heterogeneity among studies (I2 = 90%, P < 0.01). The pooled results of the recanalization, combined procedures, and TIPS subgroups were 10.8% (95% 7.5‒13.8%), 17.9% (95% CI 10.9‒24.9%), and 42.9% (95% CI 29.9‒56.8%), respectively.
The survival rate at 1 and 5 years after endovascular intervention procedures
The survival rate of endovascular intervention therapy of BCS patients at 1 and 5 years after initial intervention procedures are shown in Figs. 5 and 6. The pooled result of the total survival rate at 1 year was 98.9% (95% CI 96.8‒98.9%), with statistically significant heterogeneity among studies (I2 = 60%, P < 0.01). The pooled results of the recanalization, combined procedures, and TIPS subgroups were 99.9% (95% CI 98.9‒99.9%), 96.9% (95% CI 94.8‒97.9%), and 94.9% (95% CI 91.9‒96.7%), respectively. Similarly, the pooled result of the total survival rate at 5 years was 94.9% (95% CI: 92.5‒96.9%), with statistically significant heterogeneity among studies (I2 = 77%, P < 0.01). The pooled results of the recanalization, TIPS, and combined procedures subgroups were 97.9% (95% CI 94.8‒98.9%), 88.9% (95% CI 84.9‒91.9%), and 93.9% (95% CI 90.9‒95.9%), respectively.
Publication bias
The results of publication bias in the studies evaluated with Egger’s test. The publication bias for the technical success rate of endovascular intervention procedures (P = 0.0335), clinical success (P = 0.5567), re-intervention (P = 0.08108), the survival rate in one year (P = 0.01549) and the survival rate at five years (P = 0.8909). Although the P value of technical success and survival rate at 1 year was statistically significant.
Discussion
This extensive study evaluates and updates the clinical efficacy and long-term outcome of endovascular therapy in BCS patients and compares recanalization, TIPS/DIPS, and combined procedures. The technical and clinical success rates were 98.9% and 96.9%. After the initial endovascular treatment, the re-intervention rate was 18.9%, and the survival rates at 1 and 5 years after the initial endovascular treatment were 97.9% and 94.9%, respectively. The findings indicate that endovascular intervention treatment is safe, effective, and provides long term survival rates in patients with BCS.
Most of the studies were conducted in Asian countries, half of the study sample was from China (50%), and 45.7% of the study sample was published from 2015 to 2019. Most of the patients were treated with endovascular recanalization with or without stent placement. The subgroups’ pooled result showed that the re-intervention treatment rate was high in TIPS/DIPS, the technical success rate higher in combined procedures, and the clinical success rate and the survival rate at 1 and 5 years were higher with recanalization. It was interesting to find that the most common obstruction site was HV in the Asian countries. Also, most Asian studies reported the most common obstruction sites IVC and combined (HV and IVC)48,84,85. However, some studies have reported HV obstruction as the most common cause of BCS in the Asian population27,86.
BCS can be classified according to etiology (primary and secondary), site of obstruction (HV, IVC, and combined HV + IVC), the manifestation of the disease (fulminant or non-fulminant), and duration of the disease (acute, subacute or chronic)2. The clinical presentation is highly variable but may be categorized as acute/fulminant hepatic failure, as subacute without evidence of cirrhosis and as chronic with evidence of portal hypertension and cirrhosis87. In this meta-analysis, we found most of the studies were treated according to the site of obstruction (42.25% in HV, 30.98% in the IVC, and 26.76% in combined HV + IVC). Recanalization and TIPS treatments for BCS depend on the anatomical site and the extent of obstruction and liver function58. HV recanalization and TIPS have become the main treatment for HV-type BCS 16,33,38.
BCS is a rare disorder and therefore management guidelines are based on the retrospective case series, expert opinion and clinical presentation75,88,89,90, due to the lack of randomized controlled trials study9. BCS is more prevalent in developing countries such as, China, India, Nepal and South Africa. In contrast, the most common cause is membranous obstruction, an underlying thrombotic disorder that has been in only a few patients28, where the treatment choice is recanalization. However, only 29–41% of Western patients have membranous or segment obstruction41,91, and pure hepatic vein thrombosis accounts for more than half of BCS cases92. In contrast, recanalization is not applicable in most Western patients with BCS, and TIPS is a preferable treatment41.
Membranous obstruction of IVC is a common cause of hepatic venous outflow obstruction, which has short web narrowing to a long segmental occlusion with or without narrowing of hepatic vein46,93. In the West, HV thrombosis is the most common cause, while in Asian countries isolated IVC membranous webs are more common84,85, and two-thirds of IVC obstructions are due to membranous or segment obstruction. The long-term treatment outcome of endovascular intervention treatment was better for membranous obstruction of IVC rather than segmental obstruction of IVC. PTA alone could be the optimal treatment for membranous obstruction and stenting should be more strongly recommended for a segment of obstruction of IVC30.
The thrombophilic factors are responsible to development of BCS, which is detected in up to 84% of BCS patients10,11. The most common thrombophilic factors are myeloproliferative disease and factor V linden11. In over 25% of BCS cause more than one thrombophilic state may be present with BCS patients94. Most inherited thrombophilias result increased thrombosis due to an impaired neutralization of thrombin or failure to control of generation of thrombin95. Data show that prothrombotic disorders are not common in china as a cause of unknown factors in Chinese BCS patients96. The thrombophilia is more commonly found in western BCS patient than Chinese BCS patients97.
HV recanalization was performed in patients with short-segment HV obstruction (< 3 cm), and stenting was performed in long segment HV occlusion (> 3 cm) with large collateral vein drainage36. HV recanalization is usually difficult for BCS patients with segmental obstruction, whereas TIPS placement has been widely used for BCS patients who fail to HV recanalization41,98. In patients with compensatory but obstruction accessory hepatic vein (AHV), Fu et al.22 reported that recanalization of the AHV is a simple, safe, and effective treatment option for long segmental obstruction of the HV. However, TIPS is often the treatment choice for long segmental obstruction of HV41,76.
In Western countries, where HV extensive thrombosis is more common mostly due to myeloproliferative neoplasm92,99, TIPS placement is used to treat most patients. In Asia, where HV obstruction is mostly due to membranous webs84, recanalization (PTA and stenting) is a more common treatment. In this extensive meta-analysis, TIPS placement was more used in Western countries than Asian countries, and membranous webs had better outcomes than extensive thrombosis.
The step-wise therapeutic algorithm of BCS includes medical therapy with anticoagulant drugs and thrombolysis—recanalization with or without stent placement—TIPS/DIPS and liver transplantation45,100. However, due to poor long-term medical therapy outcomes, most of the studies used recanalization with or without stent placement as the first-line treatment for BCS14,15,22,26,35,59,80. Moreover, TIPS was used in circumstances of failed recanalization, refractory ascites, portal hypertension, variceal bleeding, and long segment obstruction or diffused obstruction of the HV21,24,41,43,52.
Recanalization is a physiological procedure that maintains the natural blood flow in HV/IVC33,36,41. It can minimize the risk of hepatic encephalopathy, and remains a first-line treatment option for BCS patients35,61. However, TIPS has less portal vein blood perfusion in the liver than recanalization and a high risk of hepatic encephalopathy due to the formation of a blood ammonia level and impaired liver function after shunt placement19. The secondary patency of recanalization with angioplasty + stent (79% and 92%) was higher than recanalization with only angioplasty (64% and 69%) at 1 and 5 years49. The treatment of BCS with an expandable metallic stent was introduced to decreasing the re-stenosis rate after angioplasty101. This study found that most studies adopted recanalization (44.28%) as a first-line treatment because it is a relatively simple and quick procedure. Also, the risk of hepatic encephalopathy after recanalization is lower than TIPS/DIPS. TIPS/DIPS has only been applied as an alternative treatment option for selective cases of BCS, but it may have a high risk of complication after shunt implantation49,102. However, several previous studies have reported the high patency rate and long-term outcome of TIPS/DIPS for BCS43,75,103,104,105,106. Liver transplantation is a second surgical option for BCS when a rapidly progressive liver failure occurs before or after TIPS107,108.
In this meta-analysis, we found that the survival of recanalization and TIPS were 99.9% and 94.9% at 1 year and 97.9% and 87.9% at 5 years, respectively. The survival of patients in this study seems comparable to that of a previous meta-analysis Zhang et al.109, which showed the survival of recanalization and TIPS were 95.9% and 87.3% at 1 year and 88.6% and 72.1% at 5 years, respectively. Tripathi et al.’s49 retrospective study showed the survival of recanalization and TIPS were 97% and 88% at 1 year, 89% and 79% at 5 years, and 85% and 73% at 10 years, respectively. Garcia-pagan et al.75 reported that the survival of TIPS with liver transplantation at 1and 5 years were 88% and 78%, respectively. Mentha et al.110 reported that survival of liver transplantation for BCS at 1, 5, and 10 years were 76%, 71%, and 68%, respectively. Nonetheless, our meta-analysis results indicate a progressive improvement in survival rate with endovascular therapy for BCS treatment.
Our results show that recanalization therapy had a better prognosis than TIPS therapy. Similarly, the prognosis of recanalization was shown by previous meta-analyses109. Mukund et al.82 reported that BCS patients treated with recanalization have improved biochemical profile and overall outcome relative to DIPS treatment. However, the survival and clinical improvement were similar in both groups, and Tripathi et al.49 also reported no significant difference in the results of patients treated with recanalization and TIPS.
Recently, endovascular intervention treatment has emerged as an advanced therapeutic option for BCS patients. The TIPS/DIPS procedures have rapidly replaced the traditional surgical shunt due to minimal invasiveness, less blood loss, low infection rate, quick recovery, shorter hospital stay, and increased long-term survival rate9,24. The technical success rate of TIPS in BCS has been reported to be between 75 and 100%. Shunt dysfunction at 5 years ranges between 40 and 75%, and the survival rate at 1 and 5 years after the initial intervention treatment was 85% and 75%, respectively16,24,74,111,112. It was found that the TIPS/DIPS technical success rate was 98.9%, while shunt dysfunction was 42.9%, and the survival rates at 1 and 5 years were 94.9% and 87.9%, respectively.
The development of new techniques and improvements in radiological intervention has established endovascular intervention therapy as a treatment of choice for BCS patients. This method provides an effective treatment modality for BCS patients and prevents progression to life threatening conditions, such as portal hypertension and other related complications47,113.
In this updated analysis, most of the included study was original articles published after 2010. The survival rates at 1 and 5 years were 97.9% and 94.9%, the success rate of operation was 98.9%, and the re-intervention episode was 18.9%. Similarly, the survival rates of recanalization, combined procedures, and TIPS/DIPS in BCS at 1 and 5 years were 99.9%, 96.9%, and 94.9% and 97.9%, 93.9%, and 87.9%, respectively. Publication bias of technical success (P = 0.0335), clinical success (P = 0.5567), re-intervention (P = 0.08108), the survival rate at 1 year (P = 0.01549) and survival rates at 5 years (P = 0.8909) were observed. The patients with recanalization treatment had a better prognosis and outcome than the combined procedures and TIPS/DIPS treatment. Additionally, the clinical success rate, shunt dysfunction rate, combined procedures, and obstruction site were analyzed. Overall, comparatively the statistical results are progressively more favorable than the previous study109.
Despite the latest update on the role of endovascular intervention therapy for BCS, the present study has several limitations: First, studies on endovascular intervention therapy for BCS worldwide are limited. Retrievable articles were available between 1995 and 2019. Most of the relevant studies were published between 2015 and 2019 and only four studies were published before 2000. Second, some articles were excluded during the selection because of a lack of information about re-intervention and long-term survival rates. Third, there was an unequal distribution based on studies conducted in different geographical regions. Most of the study samples were from Asian and European countries; the African and American data were scarce. Also, some studies were excluded due to low study quality.
Conclusion
The systematic review and meta-analysis findings further solidify the role of endovascular intervention treatment in BCS as safe and effective. It maintains high technical and clinical success, and long-term survival rates. The recanalization treatment had a better prognosis and outcome than the combined procedures and TIPS/DIPS treatment. The endovascular intervention procedures are the preferred first-line treatment in selected patients with BCS. However, randomized controlled multidisciplinary centers studies are needed to further evaluation.
Data availability
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to legal restrictions.
References
Valla, D. C. Primary Budd-Chiari syndrome. J. Hepatol. 50(1), 195–203. https://doi.org/10.1016/j.jhep.2008.10.007 (2009).
Janssen, H. L. et al. Budd-Chiari syndrome: A review by an expert panel. J. Hepatol. 38(3), 364–371. https://doi.org/10.1016/s0168-8278(02)00434-8 (2003).
Plessier, A. & Valla, D. C. Budd-Chiari syndrome. Semin. Liver Dis. 28(3), 259–269. https://doi.org/10.1055/s-0028-1085094 (2008).
Riva, N., Donadini, M. P., Dentali, F., Squizzato, A. & Ageno, W. Clinical approach to splanchnic vein thrombosis: risk factors and treatment. Thromb. Res. 130(Suppl 1), S1-3. https://doi.org/10.1016/j.thromres.2012.08.259 (2012).
Shetty, S. & Ghosh, K. Thrombophilic dimension of Budd chiari syndrome and portal venous thrombosis–a concise review. Thromb. Res. 127(6), 505–512. https://doi.org/10.1016/j.thromres.2010.09.019 (2011).
Menon, K. V., Shah, V. & Kamath, P. S. The Budd-Chiari syndrome. N. Engl. J. Med. 350(6), 578–585. https://doi.org/10.1056/NEJMra020282 (2004).
Orloff, M. J., Daily, P. O., Orloff, S. L., Girard, B. & Orloff, M. S. A 27-year experience with surgical treatment of Budd-Chiari syndrome. Ann. Surg. 232(3), 340–352. https://doi.org/10.1097/00000658-200009000-00006 (2000).
Qi, X. & Han, G. Images in clinical medicine: Abdominal-wall varices in the Budd-Chiari syndrome. N. Engl. J. Med. 370(19), 1829. https://doi.org/10.1056/NEJMicm1308567 (2014).
Darwish Murad, S. et al. Etiology, management, and outcome of the Budd-Chiari syndrome. Ann. Intern. Med. 151(3), 167–175. https://doi.org/10.7326/0003-4819-151-3-200908040-00004 (2009).
Mohanty, D., Shetty, S., Ghosh, K., Pawar, A. & Abraham, P. Hereditary thrombophilia as a cause of Budd-Chiari syndrome: A study from Western India. Hepatology 34(4 Pt 1), 666–670. https://doi.org/10.1053/jhep.2001.27948 (2001).
Smalberg, J. H. et al. Myeloproliferative neoplasms in Budd-Chiari syndrome and portal vein thrombosis: A meta-analysis. Blood 120(25), 4921–4928. https://doi.org/10.1182/blood-2011-09-376517 (2012).
Liver EAftSot. EASL clinical practice guidelines: Vascular diseases of the liver. J. Hepatol. 64(1), 179 (2016).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 339, b2700. https://doi.org/10.1136/bmj.b2700 (2009).
Ding, P. X. et al. An individualised strategy and long-term outcomes of endovascular treatment of Budd-Chiari syndrome complicated by inferior vena cava thrombosis. Eur. J. Vasc. Endovasc. Surg. 55(4), 545–553. https://doi.org/10.1016/j.ejvs.2017.12.016 (2018).
Nagral, A., Hasija, R. P., Marar, S. & Nabi, F. Budd-Chiari syndrome in children: Experience with therapeutic radiological intervention. J. Pediatr. Gastroenterol. Nutr. 50(1), 74–78. https://doi.org/10.1097/MPG.0b013e3181aecb63 (2010).
Rössle, M. et al. The Budd-Chiari syndrome: Outcome after treatment with the transjugular intrahepatic portosystemic shunt. Surgery. 135(4), 394–403 (2004).
Blum, U. et al. Budd-Chiari syndrome: Technical, hemodynamic, and clinical results of treatment with transjugular intrahepatic portosystemic shunt. Radiology 197(3), 805–811 (1995).
Pavri, T. M., Herbst, A., Reddy, R. & Forde, K. A. Budd-Chiari syndrome: A single-center experience. World J. Gastroenterol. 20(43), 16236–16244. https://doi.org/10.3748/wjg.v20.i43.16236 (2014).
Xu, K. et al. Budd-Chiari syndrome caused by obstruction of the hepatic inferior vena cava: Immediate and 2-year treatment results of transluminal angioplasty and metallic stent placement. Cardiovasc. Interven. Radiol. 19(1), 32–36 (1996).
Kathuria, R., Srivastava, A., Yachha, S. K., Poddar, U. & Baijal, S. S. Budd-Chiari syndrome in children: Clinical features, percutaneous radiological intervention, and outcome. Eur. J. Gastroenterol. Hepatol. 26(9), 1030–1038 (2014).
Khuroo, M. S. et al. Budd-Chiari syndrome: Long-term effect on outcome with transjugular intrahepatic portosystemic shunt. J. Gastroenterol. Hepatol. 20(10), 1494–1502 (2005).
Fu, Y. F., Xu, H., Zhang, K., Zhang, Q. Q. & Wei, N. Accessory hepatic vein recanalization for treatment of Budd-Chiari syndrome due to long-segment obstruction of the hepatic vein: Initial clinical experience. Diagn. Interv. Radiol. 21(2), 148–153. https://doi.org/10.5152/dir.2014.14128 (2015).
Jagtap, N. et al. Budd-Chiari syndrome: Outcomes of endovascular intervention: A single-center experience. Indian J. Gastroenterol. 36(3), 209–216 (2017).
Zahn, A. et al. Budd-Chiari Syndrome: Long term success via hepatic decompression using transjugular intrahepatic porto-systemic shunt. BMC Gastroenterol. 10(1), 25. https://doi.org/10.1186/1471-230X-10-25 (2010).
Zhou, P.-L., Wu, G., Han, X.-W., Yan, L. & Zhang, W.-G. Budd-Chiari syndrome with upper gastrointestinal hemorrhage: Characteristic and long-term outcomes of endovascular treatment. Vascular. 25(6), 642–648 (2017).
Yang, F. et al. Catheter aspiration with recanalization for Budd-Chiari syndrome with inferior vena cava thrombosis. Surg. Laparosc. Endosc Percutan. Tech. 29(4), 304–307 (2019).
Amarapurkar, D. N., Punamiya, S. J. & Patel, N. D. Changing spectrum of Budd-Chiari syndrome in India with special reference to non-surgical treatment. World J. Gastroenterol. 14(2), 278–285. https://doi.org/10.3748/wjg.14.278 (2008).
Cheng, D. et al. Clinical features and etiology of Budd-Chiari syndrome in Chinese patients: A single-center study. J. Gastroenterol. Hepatol. 28(6), 1061–1067. https://doi.org/10.1111/jgh.12140 (2013).
Fu, Y.-F. et al. Combined thrombus aspiration and recanalization in treating Budd-Chiari syndrome with inferior vena cava thrombosis. Radiol. Med. 120(12), 1094–1099 (2015).
Huang, Q. et al. Comparison of long-term outcomes of endovascular management for membranous and segmental inferior vena cava obstruction in patients with primary Budd-Chiari syndrome. Circ. Cardiovasc. Interv. 9(3), e003104. https://doi.org/10.1161/circinterventions.115.003104 (2016).
Mishra, T. K., Routray, S. N., Behera, M., Patnaik, U. K. & Satapathy, C. Percutaneous balloon angioplasty of membranous obstruction of the inferior vena cava. Indian Heart J. 55(4), 362–364 (2003).
Mo, A. et al. Early radiological intervention and haematology screening is associated with excellent outcomes in Budd-Chiari syndrome. Intern. Med. J. 47(12), 1361–1367 (2017).
Zhang, B. et al. Effects of percutaneous transhepatic interventional treatment for symptomatic Budd-Chiari syndrome secondary to hepatic venous obstruction. J. Vasc. Surg. Venous Lymphat. Disord. 1(4), 392–399. https://doi.org/10.1016/j.jvsv.2013.05.008 (2013).
Meng, X. et al. Endovascular management of Budd-Chiari syndrome with inferior vena cava thrombosis: A 14-year single-center retrospective report of 55 patients. J. Vasc. Interven. Radiol. JVIR. 27(10), 1592–1603. https://doi.org/10.1016/j.jvir.2016.04.019 (2016).
Chen, Z. K., Fan, J., Cao, C. & Li, Y. Endovascular treatment for hepatic vein-type Budd-Chiari syndrome: Effectiveness and long-term outcome. Radiol. Med. 123(10), 799–807. https://doi.org/10.1007/s11547-018-0907-2 (2018).
Rathod, K. et al. Endovascular treatment of Budd-Chiari syndrome: Single center experience. J. Gastroenterol. Hepatol. 32(1), 237–243. https://doi.org/10.1111/jgh.13456 (2017).
Sang, H.-F. & Li, X.-Q. Endovascular treatment of Budd-Chiari syndrome with hepatic vein obstruction in China. J. Laparoendosc. Adv. Surg. Tech. 24(12), 846–851. https://doi.org/10.1089/lap.2014.0095 (2014).
Rosenqvist, K. et al. Endovascular treatment of symptomatic Budd-Chiari syndrome: In favour of early transjugular intrahepatic portosystemic shunt. Eur. J. Gastroenterol. Hepatol. 28(6), 656–660. https://doi.org/10.1097/meg.0000000000000621 (2016).
Bi, Y. et al. Excellent long-term outcomes of endovascular treatment in Budd-Chiari syndrome with hepatic veins involvement: A STROBE-compliant article. Medicine 97(43), e12944. https://doi.org/10.1097/md.0000000000012944 (2018).
Al-warraky, M., Tharwa, E., Kohla, M., Aljaky, M. A. & Aziz, A. Evaluation of different radiological interventional treatments of Budd-Chiari syndrome. Egypt. J. Radiol. Nucl. Med. 46(4), 1011–1020. https://doi.org/10.1016/j.ejrnm.2015.07.003 (2015).
Eapen, C. E. et al. Favourable medium term outcome following hepatic vein recanalisation and/or transjugular intrahepatic portosystemic shunt for Budd Chiari syndrome. Gut 55(6), 878–884. https://doi.org/10.1136/gut.2005.071423 (2006).
Li, T. et al. Feasibility and midterm outcomes of percutaneous transhepatic balloon angioplasty for symptomatic Budd-Chiari syndrome secondary to hepatic venous obstruction. J. Vasc. Surg. 50(5), 1079–1084. https://doi.org/10.1016/j.jvs.2009.06.049 (2009).
Tripathi, D. et al. Good clinical outcomes following transjugular intrahepatic portosystemic stent-shunts in Budd-Chiari syndrome. Aliment. Pharmacol. Ther. 39(8), 864–872. https://doi.org/10.1111/apt.12668 (2014).
Fan, X. et al. Good clinical outcomes in Budd-Chiari syndrome with hepatic vein occlusion. Dig. Dis. Sci. 61(10), 3054–3060. https://doi.org/10.1007/s10620-016-4208-0 (2016).
Seijo, S. et al. Good long-term outcome of Budd-Chiari syndrome with a step-wise management. Hepatology 57(5), 1962–1968. https://doi.org/10.1002/hep.26306 (2013).
Srinivas, B. C., Dattatreya, P. V., Srinivasa, K. H. & Prabhavathi, M. C. N. Inferior vena cava obstruction: Long-term results of endovascular management. Indian Heart J. 64(2), 162–169. https://doi.org/10.1016/s0019-4832(12)60054-6 (2012).
Qiao, T. et al. Interventional endovascular treatment for Budd-Chiari syndrome with long-term follow-up. Swiss Med. Wkly. 135(21–22), 318–326 (2005).
Cheng, D.-L. et al. Interventional treatment strategy for primary Budd-Chiari syndrome with both inferior vena cava and hepatic vein involvement: Patients from two centers in China. Cardiovasc. Interven. Radiol. 42(9), 1311–1321. https://doi.org/10.1007/s00270-019-02267-w (2019).
Tripathi, D. et al. Long-term outcomes following percutaneous hepatic vein recanalization for Budd-Chiari syndrome. Liver Int. 37(1), 111–120. https://doi.org/10.1111/liv.13180 (2017).
Sonavane, A. D., Amarapurkar, D. N., Rathod, K. R. & Punamiya, S. J. Long term survival of patients undergoing TIPS in Budd-Chiari syndrome. J. Clin. Exp. Hepatol. 9(1), 56–61. https://doi.org/10.1016/j.jceh.2018.02.008 (2019).
Zhang, C. Q. et al. Long-term effect of stent placement in 115 patients with Budd-Chiari syndrome. World J Gastroenterol. 9(11), 2587–2591. https://doi.org/10.3748/wjg.v9.i11.2587 (2003).
Hayek, G. et al. Long-term outcome and analysis of dysfunction of transjugular intrahepatic portosystemic shunt placement in chronic primary Budd-Chiari syndrome. Radiology 283(1), 280–292. https://doi.org/10.1148/radiol.2016152641 (2017).
Bi, Y., Chen, H., Ding, P., Ren, J. & Han, X. Long-term outcome of recoverable stents for Budd-Chiari syndrome complicated with inferior vena cava thrombosis. Sci. Rep. 8(1), 7393. https://doi.org/10.1038/s41598-018-25876-w (2018).
Bi, Y. et al. Long-term outcomes of endoluminal sharp recanalization of occluded inferior vena cava in Budd-Chiari syndrome. J. Laparoendosc. Adv. Surg. Techol. A. 29(3), 309–315. https://doi.org/10.1089/lap.2018.0385 (2019).
Ding, P. X. et al. Long-term outcomes of individualized treatment strategy in treatment of type I Budd-Chiari syndrome in 456 patients. Liver Int. 39(8), 1577–1586. https://doi.org/10.1111/liv.14114 (2019).
Shalimar, S. R. et al. Long-term outcomes of transjugular intrahepatic portosystemic shunt in Indian patients with Budd-Chiari syndrome. Eur. J. Gastroenterol. Hepatol. 29(10), 1174–1182. https://doi.org/10.1097/meg.0000000000000945 (2017).
Ding, P. X. et al. Long-term safety and outcome of percutaneous transhepatic venous balloon angioplasty for Budd-Chiari syndrome. J. Gastroenterol. Hepatol. 31(1), 222–228. https://doi.org/10.1111/jgh.13025 (2016).
DarwishMurad, S. et al. Long-term outcome of a covered vs uncovered transjugular intrahepatic portosystemic shunt in Budd-Chiari syndrome. Liver Int. 28(2), 249–256. https://doi.org/10.1111/j.1478-3231.2007.01649.x (2008).
Fu, Y. et al. Necessity and indications of invasive treatment for Budd-Chiari syndrome. Hepatob. Pancreat. Dis. Int. HBPD INT. 10(3), 254–260. https://doi.org/10.1016/s1499-3872(11)60042-8 (2011).
Eldorry, A. et al. Outcome of non surgical hepatic decompression procedures in Egyptian patients with Budd-Chiari. World J. Gastroenterol. 17(7), 906–913. https://doi.org/10.3748/wjg.v17.i7.906 (2011).
Cheng, D. L. et al. Outcomes of endovascular interventional therapy for primary Budd-Chiari syndrome caused by hepatic venous obstruction. Exp. Ther. Med. 16(5), 4141–4149. https://doi.org/10.3892/etm.2018.6708 (2018).
Yu, C. et al. Effectiveness and postoperative prognosis of using preopening and staged percutaneous transluminal angioplasty of the inferior vena cava in treating Budd-Chiari syndrome accompanied with inferior vena cava thrombosis. Ann. Vasc. Surg. 60, 52–60. https://doi.org/10.1016/j.avsg.2019.03.037 (2019).
Wu, T. et al. Percutaneous balloon angioplasty of inferior vena cava in Budd-Chiari syndrome-R1. Int. J. Cardiol. 83(2), 175–178. https://doi.org/10.1016/s0167-5273(02)00037-2 (2002).
Han, G. et al. Percutaneous recanalization for Budd-Chiari syndrome: An 11-year retrospective study on patency and survival in 177 Chinese patients from a single center. Radiology 266(2), 657–667. https://doi.org/10.1148/radiol.12120856 (2013).
Fu, Y. F. et al. Percutaneous recanalization for combined-type Budd-Chiari syndrome: Strategy and long-term outcome. Abdom. Imaging. 40(8), 3240–3247. https://doi.org/10.1007/s00261-015-0496-7 (2015).
Cui, Y.-F., Fu, Y.-F., Li, D.-C. & Xu, H. Percutaneous recanalization for hepatic vein-type Budd-Chiari syndrome: Long-term patency and survival. Hep. Intl. 10(2), 363–369. https://doi.org/10.1007/s12072-015-9676-3 (2016).
Boyvat, F., Harman, A., Ozyer, U., Aytekin, C. & Arat, Z. Percutaneous sonographic guidance for TIPS in Budd-Chiari syndrome: Direct simultaneous puncture of the portal vein and inferior vena cava. AJR Am. J. Roentgenol. 191(2), 560–564. https://doi.org/10.2214/ajr.07.3496 (2008).
Kucukay, F., Akdogan, M., Bostanci, E. B., Ulus, A. T. & Kucukay, M. B. Percutaneous transluminal angioplasty for complete membranous obstruction of suprahepatic inferior vena cava: Long-term results. Cardiovasc. Intervent. Radiol. 39(10), 1392–1399. https://doi.org/10.1007/s00270-016-1394-2 (2016).
Lee, B. B. et al. Primary Budd-Chiari syndrome: Outcome of endovascular management for suprahepatic venous obstruction. J. Vasc. Surg. 43(1), 101–108. https://doi.org/10.1016/j.jvs.2005.09.003 (2006).
Griffith, J. F. et al. Radiological intervention in Budd-Chiari syndrome: techniques and outcome in 18 patients. Clin. Radiol. 51(11), 775–784. https://doi.org/10.1016/s0009-9260(96)80005-5 (1996).
Cui, Y. F., Fu, Y. F., Wei, N., Zhu, H. C. & Xu, H. Retrograde puncture assisted hepatic vein recanalization in treating Budd-Chiari syndrome with segmental obstruction of hepatic vein. Radiol. Med. 120(12), 1184–1189. https://doi.org/10.1007/s11547-015-0557-6 (2015).
Yang, X. L., Cheng, T. O. & Chen, C. R. Successful treatment by percutaneous balloon angioplasty of Budd-Chiari syndrome caused by membranous obstruction of inferior vena cava: 8-year follow-up study. J. Am. Coll. Cardiol. 28(7), 1720–1724. https://doi.org/10.1016/s0735-1097(96)00385-3 (1996).
Xue, H., Li, Y. C., Shakya, P., Palikhe, M. & Jha, R. K. The role of intravascular intervention in the management of Budd-Chiari syndrome. Dig. Dis. Sci. 55(9), 2659–2663. https://doi.org/10.1007/s10620-009-1087-7 (2010).
Molmenti, E. P. et al. The utility of TIPS in the management of Budd-Chiari syndrome. Ann. Surg. 241(6), 978–981. https://doi.org/10.1097/01.sla.0000164180.77824.12 (2005) (Discussion 982–983).
Garcia-Pagán, J. C. et al. TIPS for Budd-Chiari syndrome: Long-term results and prognostics factors in 124 patients. Gastroenterology 135(3), 808–815. https://doi.org/10.1053/j.gastro.2008.05.051 (2008).
Neumann, A. B. et al. Treatment of Budd-Chiari syndrome with a focus on transjugular intrahepatic portosystemic shunt. World J. Hepatol. 5(1), 38–42. https://doi.org/10.4254/wjh.v5.i1.38 (2013).
Wang, R. et al. Treatment of Budd-Chiari syndrome with inferior vena cava thrombosis. Exp. Ther. Med. 5(4), 1254–1258. https://doi.org/10.3892/etm.2013.961 (2013).
Corso, R., Intotero, M., Solcia, M., Castoldi, M. C. & Rampoldi, A. Treatment of Budd-Chiari syndrome with transjugular intrahepatic portosystemic shunt (TIPS). Radiol. Med. 113(5), 727. https://doi.org/10.1007/s11547-008-0288-z (2008).
Ding, P. X. et al. Treatment of Budd-Chiari syndrome with urokinase following predilation in patients with old inferior vena cava thrombosis. Radiol. Med. 116(1), 56–60. https://doi.org/10.1007/s11547-010-0600-6 (2011).
Fu, Y. F. et al. Use of accessory hepatic vein intervention in the treatment of Budd-Chiari syndrome. Cardiovasc. Intervent. Radiol. 38(6), 1508–1514. https://doi.org/10.1007/s00270-015-1105-4 (2015).
Fitsiori, K. et al. Transjugular intrahepatic portosystemic shunt for the treatment of Budd-Chiari syndrome patients: results from a single center. Cardiovasc. Intervent. Radiol. 37(3), 691–697. https://doi.org/10.1007/s00270-013-0697-9 (2014).
Mukund, A., Mittal, K., Mondal, A. & Sarin, S. K. Anatomic recanalization of hepatic vein and inferior vena cava versus direct intrahepatic portosystemic shunt creation in Budd-Chiari syndrome: Overall outcome and midterm transplant-free survival. J. Vasc. Interv. Radiol. 29(6), 790–799. https://doi.org/10.1016/j.jvir.2018.01.781 (2018).
Shaker, M. et al. Outcome of transjugular intrahepatic portosystemic shunt in Budd-Chiari syndrome: Long-term outcomes of 118 patients; A single-center experience. Arab J. Interven. Radiol. 2(02), 75–81 (2018).
Okuda, H. et al. Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J. Hepatol. 22(1), 1–9. https://doi.org/10.1016/0168-8278(95)80252-5 (1995).
Okuda, K. Inferior vena cava thrombosis at its hepatic portion (obliterative hepatocavopathy). Semin. Liver Dis. 22(1), 15–26. https://doi.org/10.1055/s-2002-23203 (2002).
Kohli, V. et al. Management of hepatic venous outflow obstruction. Lancet 342(8873), 718–722. https://doi.org/10.1016/0140-6736(93)91712-u (1993).
Zahn, A. et al. Budd-Chiari syndrome: Long term success via hepatic decompression using transjugular intrahepatic porto-systemic shunt. BMC Gastroenterol. 10, 25. https://doi.org/10.1186/1471-230x-10-25 (2010).
DeLeve, L. D., Valla, D. C. & Garcia-Tsao, G. Vascular disorders of the liver. Hepatology 49(5), 1729–1764. https://doi.org/10.1002/hep.22772 (2009).
de Franchis, R. Revising consensus in portal hypertension: Report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J. Hepatol. 53(4), 762–768. https://doi.org/10.1016/j.jhep.2010.06.004 (2010).
Klein, A. S. Management of Budd-Chiari syndrome. Liver Transpl. 12(11 Suppl 2), S23–S28. https://doi.org/10.1002/lt.20941 (2006).
Valla, D. et al. Hepatic venous outflow block caused by short-length hepatic vein stenoses. Hepatology 25(4), 814–819. https://doi.org/10.1002/hep.510250405 (1997).
Darwish Murad, S. et al. Determinants of survival and the effect of portosystemic shunting in patients with Budd-Chiari syndrome. Hepatology 39(2), 500–508. https://doi.org/10.1002/hep.20064 (2004).
Kandpal, H., Sharma, R., Gamangatti, S., Srivastava, D. N. & Vashisht, S. Imaging the inferior vena cava: a road less traveled. Radiographics 28(3), 669–689. https://doi.org/10.1148/rg.283075101 (2008).
Denninger, M. H. et al. Cause of portal or hepatic venous thrombosis in adults: The role of multiple concurrent factors. Hepatology 31(3), 587–591. https://doi.org/10.1002/hep.510310307 (2000).
Seligsohn, U. & Lubetsky, A. Genetic susceptibility to venous thrombosis. N. Engl. J. Med. 344(16), 1222–1231. https://doi.org/10.1056/nejm200104193441607 (2001).
Dang, X., Li, L. & Xu, P. Research status of Budd-Chiari syndrome in China. Int. J. Clin. Exp. Med. 7(12), 4646 (2014).
Qi, X. et al. Thrombotic risk factors in Chinese Budd-Chiari syndrome patients. Thromb. Haemost. 109(05), 878–884 (2013).
Miraglia, R., Maruzzelli, L. & Luca, A. Recanalization of occlusive transjugular intrahepatic portosystemic shunts inaccessible to the standard transvenous approach. Diagn. Interv. Radiol. 19(1), 61–65. https://doi.org/10.4261/1305-3825.Dir.5541-12.1 (2013).
Qi, X. et al. Meta-analysis: the significance of screening for JAK2V617F mutation in Budd-Chiari syndrome and portal venous system thrombosis. Aliment Pharmacol. Ther. 33(10), 1087–1103. https://doi.org/10.1111/j.1365-2036.2011.04627.x (2011).
EASL Clinical Practice Guidelines. Vascular diseases of the liver. J. Hepatol. 64(1), 179–202. https://doi.org/10.1016/j.jhep.2015.07.040 (2016).
Charnsangavej, C. et al. Stenosis of the vena cava: Preliminary assessment of treatment with expandable metallic stents. Radiology 161(2), 295–298. https://doi.org/10.1148/radiology.161.2.3763891 (1986).
Zhang, W. et al. Budd-Chiari syndrome in China: A 30-year retrospective study on survival from a single center. World J. Gastroenterol. 24(10), 1134–1143. https://doi.org/10.3748/wjg.v24.i10.1134 (2018).
He, F. L. et al. Transjugular intrahepatic portosystemic shunt for severe jaundice in patients with acute Budd-Chiari syndrome. World J. Gastroenterol. 21(8), 2413–2418. https://doi.org/10.3748/wjg.v21.i8.2413 (2015).
Qi, X. et al. Transjugular intrahepatic portosystemic shunt for Budd-Chiari syndrome: Techniques, indications and results on 51 Chinese patients from a single centre. Liver Int. 34(8), 1164–1175. https://doi.org/10.1111/liv.12355 (2014).
Hernández-Guerra, M. et al. PTFE-covered stents improve TIPS patency in Budd-Chiari syndrome. Hepatology 40(5), 1197–1202. https://doi.org/10.1002/hep.20436 (2004).
Gandini, R., Konda, D. & Simonetti, G. Transjugular intrahepatic portosystemic shunt patency and clinical outcome in patients with Budd-Chiari syndrome: Covered versus uncovered stents. Radiology 241(1), 298–305. https://doi.org/10.1148/radiol.2411050347 (2006).
Hemming, A. W. et al. Treatment of Budd-Chiari syndrome with portosystemic shunt or liver transplantation. Am. J. Surg. 171(1), 176–180. https://doi.org/10.1016/s0002-9610(99)80095-6 (1996) (Discussion 180–181).
Rao, A. R. et al. Orthotopic liver transplantation for treatment of patients with Budd-Chiari syndrome: A Singe-center experience. Transpl. Proc. 32(7), 2206–2207. https://doi.org/10.1016/s0041-1345(00)01636-5 (2000).
Zhang, F., Wang, C. & Li, Y. The outcomes of interventional treatment for Budd-Chiari syndrome: Systematic review and meta-analysis. Abdom. Imaging. 40(3), 601–608. https://doi.org/10.1007/s00261-014-0240-8 (2015).
Mentha, G. et al. Liver transplantation for Budd-Chiari syndrome: A European study on 248 patients from 51 centres. J. Hepatol. 44(3), 520–528. https://doi.org/10.1016/j.jhep.2005.12.002 (2006).
Rogopoulos, A., Gavelli, A., Sakai, H., McNamara, M. & Huguet, C. Transjugular intrahepatic portosystemic shunt for Budd-Chiari syndrome after failure of surgical shunting. Arch. Surg. 130(2), 227–228. https://doi.org/10.1001/archsurg.1995.01430020117024 (1995).
Mancuso, A. et al. TIPS for acute and chronic Budd-Chiari syndrome: A single-centre experience. J. Hepatol. 38(6), 751–754. https://doi.org/10.1016/s0168-8278(03)00118-1 (2003).
Carbonell, N. et al. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology 40(3), 652–659. https://doi.org/10.1002/hep.20339 (2004).
Garcia-Pagan, J. C. et al. TIPS for Budd-Chiari syndrome: Long-term results and prognostics factors in 124 patients. Gastroenterology 135(3), 808–815. https://doi.org/10.1053/j.gastro.2008.05.051 (2008).
Januszewicz, M. et al. Transjugular Intrahepatic Portosystemic Shunt in patients after orthotopic liver transplantation (OLTx) due to life threatening gastrointestinal hemorrhage: A single-center experience based on three cases and literature review. Pol. Przegl. Chir. 91(2), 38–44. https://doi.org/10.5604/01.3001.0012.7791 (2018).
Author information
Authors and Affiliations
Contributions
G.M., and X.Z., retrieved of all data and analyzed data, interpretation of data, wrote manuscript and final approval; X.H., and D.J., conception and designed of the study, supervised the work, draft manuscript, critical revision and final approval; G.P., interpretation data and revised manuscript and final approval; Y.L. and S.P., revised manuscript and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mukhiya, G., Zhou, X., Han, X. et al. Evaluation of outcome from endovascular therapy for Budd-Chiari syndrome: a systematic review and meta-analysis. Sci Rep 12, 16166 (2022). https://doi.org/10.1038/s41598-022-20399-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-20399-x
This article is cited by
-
Comparison of direct intrahepatic portosystemic shunt and other major radiological interventions in patients with Budd-Chiari syndrome
Indian Journal of Gastroenterology (2025)
-
Letter to Editor re:Comparison of DIPSS and other interventions in Budd-Chiari syndrome
Indian Journal of Gastroenterology (2025)
-
Interventions in Budd-Chiari syndrome: an updated review
Abdominal Radiology (2024)