Abstract
As a hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase inhibitor, Fluvastatin (FLV) is used for reducing low-density lipoprotein (LDL) cholesterol as well as to prevent cardiovascular problems. FLV showed cell line cytotoxicity and antitumor effect. Melittin (MEL) exhibits antineoplastic activity and is known to be promising as a therapeutic option for cancer patients. The aim of this work was to investigate the combination of FLV with MEL loaded hybrid formula of phospholipid (PL) with alpha lipoic acid (ALA) nanoparticles to maximize anticancer tendencies. This study examines the optimization of the prepared formulation in order to minimize nanoparticles size and maximize zeta potential to potentiate cytotoxic potentialities in colon cancer cells (Caco2), cell viability, cell cycle analysis and annexin V were tested. In addition to biological markers as P53, Bax, bcl2 and Caspase 3 evaluation The combination involving FLV PL ALA MEL showed enhanced cytotoxic potentiality (IC50 = 9.242 ± 0.35 µg/mL), about twofold lower, compared to the raw FLV (IC50 = 21.74 ± 0.82 µg/mL). According to studies analyzing cell cycle, optimized FLV PL ALA MEL was found to inhibit Caco2 colon cancer cells more significantly than other therapeutic treatments, wherein a higher number of cells were found to accumulate over G2/M and pre-G1 phases, whereas G0/G1/S phases witnessed the accumulation of a lower number of cells. The optimized formulation may pave the way for a novel and more efficacious treatment for colon cancer.
Similar content being viewed by others
Introduction
Colon cancer is known to affect people of all ages but generally impacts older individuals, commencing in the colon (large intestine). It usually begins as small and noncancerous cell clusters referred to as polyps forming inside the large intestine1,2,3, which, however, can turn cancerous over time. These polyps may be small and asymptomatic, which is why doctors advise people to undergo screening tests on a regular basis to get rid of polyps before they become cancerous4,5,6. Treatment options for colon cancer include drugs, radiation therapies, chemotherapy, immunotherapy, surgery, as well as targeted therapies. Another name for colon cancer is colorectal cancer, which is since it is used to denote cancers of the rectum (which is where it begins) and colon7,8. The first statin, Fluvastatin (FLV), is one of the synthetic origin statins9,10. Statins are characterized by a characteristic pharmacophore group either being a lactone ring as a pro-drug or a long chain carboxylic acid as an active form, responsible for the inhibiting activity, and a ring system moiety that is different for each type11. Alpha-Lipoic acid (ALA), a naturally occurring disulfide molecule, is a powerful antioxidant that reportedly exerts beneficial effects in patients with advanced cancer by reducing the level of reactive oxygen species and increasing glutathione peroxidase activity12,13. After the Food and Drug Administration (FDA) gave its approval FLV has primarily been utilized for preventing/treating cardiovascular ailments as well as for maintaining blood low-density lipoprotein (LDL) cholesterol14,15. However, the pathological situations of heart attack and coronary heart disease (CHD) cannot be cured by such drugs; at best, the drugs can prevent the recurrence or aggravation of symptoms in individuals who are prone to getting diagnosed with these diseases. However, statins, in particular, FLV, have been recommended as an option to treat various colon cancer types16,17,18,19. Notably, the primary use of FLV relates to treating coronary artery disease and dyslipidemia20. Moreover, FLV is associated with toxic and antineoplastic impacts across various experimental cancer models10,14,21.
Comprising 26 amino acids, a water-soluble, small-sized cationic peptide Melittin (MEL) constitutes a key element of Apis mellifera or honeybee venom22,23,24. While several studies have examined the peptide’s anticancer activity in vitro as well as in vivo trials, the clinical usage remains contentious owing to its hemolytic activity and cytotoxicity at significant dosages. Given that MEL can also impart anti-inflammatory/antiviral/antibacterial attributes25,26, optimized formulation development where MEL is used in conjunction with antineoplastic drugs has been shown to assume significance.
This work aimed at probing FLV’s pro-apoptotic and cytotoxic efficacy on cells of colon cancer in humans following its formulation to nanoparticles of ALA encompassed using (that is, in a nanoform) MEL. The cell line denotes an adequate system for investigating the resistance of drugs and the potential toxicity of statins in isolation or when they are used alongside antineoplastic drugs. To have FLV PL ALA MEL NPs prepared and optimized, a factorial design of Box Behnken was employed. This optimized formula comprising FLV’s sub-toxic concentration was investigated in human Caco2 cells to determine inhibitory concentration (IC50) values, apoptosis, mitochondrial membrane potential (MMP), and BCL-2/BAX proteins.
Materials and methods
FLV was received as a gift from the Egyptian International Pharmaceutical Industries Company (EIPICO) (10th of Ramadan city, Egypt). On the other hand, both ALA as well as MEL were derived from the USA-based Sigma-Aldrich Inc. meanwhile, Phospholipon® 90H was received as a gift from Ludwigshafen, Germany-based Lipoid GmbH. Caco2 colon cancer cells and EA.hy926 human endothelial cells were from the Egypt-based VACSERA cell culture originally procured from the US-based ATCC located in Manassas, VA.
Experimental design
Response surface design, specifically three-factor Box Behnken, was employed for optimizing FLV- PL-ALA-MEL nanoformula. PL, ALA, and MEL amounts in mg (designated as X1, X2, and X3, respectively). Size (nm, Y1) and zeta potential (mV, Y2) were the response parameters (Table 1). Based on the implemented design, 15 experimental runs listed in Table 2 were generated by Design-Expert software (Version 12; Stat-Ease Inc., Minneapolis, MN, USA). Selection of the optimal polynomial model for each response was computed by the software. The goodness of the fit of responses to the models was assessed by diagnostic plots27.
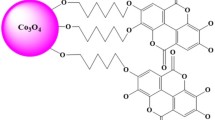
Preparation of FLV-PL-ALA-MEL
FLV-PL-ALA-MEL nanoparticles were prepared as elucidated previously. FLV (30 mg) and Phospholipon® 90H in weights were dissolved in methanol/chloroform (1:1) (20 mL). The solution was then evaporated to obtain a thin film layer. The thin film layer was further dried in a vacuum oven for 48 h at 35 °C. The dried film layer was hydrated in an aqueous solution containing the specified MEL amounts. The formed FLV- PL-ALA-MEL nanoformula were then stored at a temperature of 4 °C in an airtight glass container until use in future.
FLV-PL-ALA-MEL size and zeta potential were determined using an instrument (bought from the UK-based Malvern) utilized for measuring the size of nanoparticles. The results were mentioned in accordance with five determinations: laser wavelength, scattering angle, temperature, medium refractive index, and viscosity.
Optimization of FLV-PL-ALA-MEL nanoformula
The desirability function amalgamating both responses was calculated to forecast the investigated factors’ optimum levels. The objective behind this approach was to minimize the nanoparticle size while increasing the absolute zeta potential to the maximum possible level, as shown in Table 1.
Optimized FLV-PL-ALA-MEL entrapment efficiency %
FLV entrapment in FLV-PL-ALA-MEL nanoformula was estimated using Eq. (1). FLV was analyzed by HPLC as previously reported28.
Optimized FLV-PL-ALA-MEL nanoformula’ cytotoxicity
Caco2 colon cancer cells were cultured as described elsewhere8. Thereafter, Caco2 cells’ IC50 values were measured using the plain formula, FLV raw or FLV-PL-ALA-MEL for a period of 48 h by metabolizing MTT to a formazan salt elucidated previously29, albeit after making slight changes. After being seeded in a culture plate (96-well tissue), the incubation of Caco2 cells took place in an environment that was humidified (temperature of 37 °C and 5% CO2) to make sure the cells were attached completely. The 48-h cell treatment was followed by the application of MTT protocol. A Spark® multimode microplate reader was used to read the absorbance in all wells. This was followed by the calculation of IC50 concerning all experimental conditions on the basis of the curves obtained after deducing cell viability variation (percentage) as a measure of growing concentrations (0.39, 1.56, 6.26, 25, and 100 µg) of the aforementioned plain formula. The noncancerous EA.hy926 endothelial cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) and were then treated in the same way as mentioned for Caco2 colon cancer cells.
Analysis of cell cycle
As previously explained, flow cytometry was used to analyze Caco2 cell cycle within the experimental conditions30,31. The already-seeded Caco2 cells (3 × 105 cells/well) were treated using the plain formula, FLV-PL-ALA-MEL, FLV raw for 24 h and untreated ones were considered as control. When the treatment ended, the cells were separated via centrifugation, had them fixed using ethanol (70% cold) repeated the procedure of centrifugation, washed them, and eventually stained them. Finally, FACS Calibur flow cytometer was used to analyze all samples.
Annexin V-FITC apoptotic activity
The dual staining approach was employed for examining how the various experimental scenarios impacted Caco2 cells for late/early-stage apoptotic percentages32. For this purpose, the Annexin V-FITC Apoptosis Kit was used relying on the manufacturer protocol, which made it possible to identify apoptosis and distinguish apoptosis from necrosis-induced cell death. In this study, the capability of propidium iodide for entering only dead or damaged cells was utilized to ascertain both cell death types.
RT-PCR for estimation of Bcl-2, Bax, p53, caspase 3, NF-kB and TNF-α
The Caco2 cells were treated with plain formula, FLV raw, and FLV-PL-ALA-MEL and incubated with IC50 concentration of samples. After the 24-h treatment, BCL-2 and BAX proteins were quantitatively determined. For this purpose, the Zymed® Bcl-2 ELISA Kit and Human BAX ELISA kit were procured, based on the instructions given by the manufacturers33,34,35. As mentioned previously, untreated cells were considered to be a control. Primers were designed by using Gene Runner software. Samples were normalized with β actin.
Western blot for protein expression of Bcl-2, Bax, Caspase 3, and p 53
Western blot of cellular proteins collected from cells treated with plain formula, FLV raw, and FLV-PL-ALA-MEL was carried out as previously reported36,37. The target proteins’ band intensities were normalized versus β-actin’s band intensity (ChemiDoc™ MP imager, Bio-Rad Inc.).
Mitochondrial membrane potential (MMP)
As previously explicated, we tracked the MMP occurring at the previously-seeded Caco2 cells (density 5 × 103 was incubated for 24 h that were exposed to the plain formula, FLV raw and FLV-PL-ALA-MEL for a period of 24 h, MitoProbe™ TMRM Assay Kit was used and cells were observed using FACS Caliber, BD Bioscience flow cytometer8. For this purpose, as well, untreated cells was considered to be a control.
Statistical analysis
For Caco2 cells as well as cell-free experiments, the IBM SPSS® statistical or (Version 8) Graphpad Prism software were used. To facilitate more than one comparison, this study employed ANOVA (one-way/two-way) as well as the post hoc Tukey test. We reported all experiments as follows: means ± standard deviation (SD) comprising a minimum of four distinct experiments and set statistical significance at p-values < 0.05.
Results
Experimental design
Size and zeta potential Fit statistical analysis results are summarized in Table 3. Based on the highest R2 and lowest PRESS, the observed size and zeta potential fitted the linear and two-factor interaction (2FI) models, respectively. The adjusted R2 and the predicted R2 for both responses coincide well with difference of less than 0.2. Accordingly, the selected models could be successfully utilized for exploring the design space.
Diagnostic plots, illustrated in Figs. 1 and 2, assessing the selected models’ goodness of fit. Figures 1A and 2A, exhibited appropriate linearity indicating the normal distribution of residuals, thus the absence of need for transformation. The colored points in the externally studentized residuals vs. predicted responses, Figs. 1B and 2B, were scattered randomly within the limits highlighting that no fixed error exists. Randomly scattered points in residual vs. run plots, Figs. 1C and 2C, indicate that no lurking variable influenced either response. Furthermore, predicted versus actual values of both responses’ plots, Figs. 1D and 2D, showed a depicted good analogy between both values as evidenced by the highly linear observed pattern38,39.
Investigated variables influence on responses
ANOVA for size confirmed the significance of the linear model as evidenced by the F-value of 224.45 (P < 0.0001). The lack of fit F-value of 9.09 (P = 0.1030) shows a non-significant lack of fit; thus, fitting of the measured size to the recommended model is ensured. The equation demonstrating the linear model in terms of coded factor was generated by the software as follows:
The analysis showed that all the linear terms representing the three studied variables had a significant effect on size (P < 0.0001, 0.0002 and 0.0049 for X1, X2, and X3, respectively). Figure 3A shows the impact of the studied factors on size, while Fig. 3B–D showing the interaction between them. It was evident that the size significantly increases with increasing either PL or ALA amounts, while decreases with increasing Mel concentration; this finding is supported by the positive sign of X1 and X2 coefficients, in addition to the negative sign of X3. As per the lowest P value and the highest coefficient of the corresponding equation term, it is evident that the PL amount exhibited the most significant effect on the size compared to the other two factors.
Regarding zeta potential, ANOVA confirmed the significance of the two-factor (2FI) interaction model as depicted by the corresponding F-value of 64.94 (P < 0.0001). The lack of fit F-value of 4.43 (P = 0.1957) reflects non-significant lack of fit; thus, the fitting of zeta potential values to the proposed model is confirmed. The software was employed to develop the equation demonstrating the 2FI model for the zeta potential in terms of coded factor as follows:
All the linear terms representing the investigated variables had a significant effect on zeta potential (P < 0.0001 for X1 and X3, respectively, and P = 0.0164 for X2). In addition the interaction term X2X3 representing the interaction between ALA and MEL amounts was significant at the 95% level of significance. Figure 4A illustrates the perturbation graph demonstrating the main effects of the studied factors on the zeta potential, while Fig. 4B–D represents the 2D- contour plots showing the interactions between them. The illustration shows that the zeta potential significantly increases at higher PL and ALA amounts, while decreases with higher MEL amounts. This finding is supported by the signs of the corresponding terms in the coded gebnerated eqauation.
Optimization of FLV-PL-ALA-MEL nanoformula
Desirability function was utilized for predicting the optimal FLV-PL-ALA-MEL nanoparticles according to the predetermined goals for the responses. The optimized levels that could yield a formulation with minimized size and maximized zeta potential when combined together are listed in Table 4. The predicted formulation is expected to achieve the desired goals with desirability of 0.704.The measured responses were in good agreement with the predicted values as depicted by the relatively low percentage error, thereof, emphasizing the adequate utility of the design and the validity of the optimization process.
Optimized FLV-PL-ALA-MEL entrapment efficiency %
The prepared Optimized FLV-PL-ALA-MEL showed FLV entrapment of 71.4 ± 5.8%.
Cytotoxic activity within Caco2 cells
After obtaining the optimized formula, our next objective was to examine both pharmacological activities as well as the potentiality of toxicity of Caco2 cells’ treatment using the optimized formula for 24 h. According to the findings derived from the MTT assay, it was observed that the least toxic potential denoted by the highest IC50 value was associated with the plain formula, this is illustrated in Fig. 5A–C. FLV PL ALA MEL showed enhanced cytotoxic potentiality with IC50 value of 9.242 ± 0.35 µg/mL compared with IC50 vlues of 21.74 ± 0.82 and 81.91 ± 3.08 for raw FLV and plain formula, respectively. The cytotoxicity efficacy of all treatments has been reduced when investigated in EA.hy926 non-cancerous endothelial cells (Fig. 5D–F). All preparations exhibited IC50 values greater than 70 µg/mL against EA.hy926 endothelial cells.
Inhibition of Caco2 cell proliferation
The impact of plain formula, FLV raw, FLV PL ALA MEL over the phases of Caco2 cell cycle can be seen in Fig. 6. The phase-wise % values for untreated Caco2 cells (control) were 1.47 ± 0.06% for pre-G1, 46.57 ± 0.86% for G0/G1, 41.18 ± 0.83% for S, and 12.25 ± 0.23% for G2-M. It is notable that the optimized FLV-PL-ALA-MEL nanoformula treatment led to significant changes in cell cycles concerning pre-G, S, as well as G2-M when compared with untreated cells of Caco2. The optimized FLV-PL-ALA-MEL nanoformula treatment did reduce Caco2 cell proliferation to a greater extent when compared with all treatments in the study (control, plain formula and FLV raw).
The effect of the FLV-PL-ALA-MEL over the phases of Caco2 cell cycle. With a view to making more than one comparison, we used the Tukey post hoc test. *Significantly different versus control (p < 0.05). #Significantly different versus Plain formula (p < 0.05). $Significantly different versus FLV-R (p < 0.05). (a) control, (b) Plain formula, (c) FLV and (d) FLV-PL-ALA-MEL.
Apoptotic activity
This study examined how various treatments impacted the Caco2 cells’ percentage going through apoptosis to illuminate the improved FLV-PL-ALA MEL antiproliferative effect and to determine whether pro-apoptotic activities were also observed. Figure 7 shows that treatment involving the optimized FLV-PL-ALA MEL formula led to a significant change in Caco2 cell percentage in both early and late apoptotic and necrosis stages when compared with the investigated Plain formula and untreated control (Fig. 7). Expectedly and as depicted in Fig. 7, the decision to use the optimized formula to treat Caco2 cells led to a significant increase in cell population percentage within necrosis (8.12 ± 0.22%; p < 0.05), early (1.99 ± 0.07%; p < 0.05)/late (16.40 ± 0.37%; p < 0.05) apoptosis stages, as well as total (necrosis + apoptosis) (26.5 ± 0.2%) when compared with other conditions of the experiment as shown in (Fig. 7). This demonstrates FLV’s enhanced pro-apoptotic attribute after combining MEL and ALA in the formula.
The effect of plain formula, FLV raw and FLV-PL-ALA MEL treatments, on apoptotic/necrotic Caco2 cells. Early refers to the early phase (apoptotic) while late denotes the late phase. On the other hand, total denotes the combination of necrosis and apoptosis. With a view to making more than one comparison, we used the Tukey post hoc test. *Significantly different versus control (p < 0.05). #Significantly different versus Plain formula (p < 0.05). $Significantly different versus FLV raw.
FLV PL ALA MEL modulating BAX, BCL-2, caspase 3 and P53 protein levels
BAX, BCL-2, caspase 3 and P53 protein concentration modulation within Caco2 cells ascertained by varying experimental scenarios is shown in Fig. 8. Caco2 treatment with optimized FLV-PL-ALA MEL increased the expression level of Bax, caspase-3, and p53 and hence caused apoptosis (Fig. 8A,C,D). While, treatment of Caco2 with optimized FLV-PL-ALA MEL reduced the expression of antiapoptotic protein Bcl-2 and thus, confirmed the apoptotic and anti-cancer activity when compared with control and other treatments as shown in Fig. 8B. The optimized FLV-PL-ALA MEL showed 4.457 ± 0.09, 0.281 ± 0.01, 5.59 ± 0.18 and 7.32 ± 0.19 fold change (normalized to β-actin) of BAX, BCL2, Caspase 3 and P53, respectively.
Expression of apoptotic markers (A) Bax, (B) Bcl-2 (C) caspase-3, and (D). p53 within Caco2 cells. Data denote the mean of four independent experiments ± SD. With a view to making more than one comparison, we used the Tukey post hoc test. #Significantly different versus plain formula (p < 0.05). *Significantly different versus control (p < 0.05). $Significantly different versus FLV-R (p < 0.05).
Expression of TNF-α and NF-kB
In the present study for investigation of TNF-α and NF-kB levels, Fig. 9 shows that treatment of Caco2 cells with the optimized FLV-PL-ALA MEL, a significant (p < 0.05) increase in the expression of TNF-α (Fig. 9A) and significant (p < 0.05) reduction in the expression of activated NF-kB (Fig. 9B) when compared with plain formula and FLV raw. The optimized FLV-PL-ALA MEL showed 1.693 ± 0.06 and 0.552 ± 0.01 fold change (normalized to β-actin) of TNF-α and NF-kB, respectively.
Modulation of treatments using the plain formula, FLV-raw and FLV-PL-ALA-MEL over Expression level of inflammatory markers (A) TNF-α and (B) NF-kB. Data denote the mean of four independent experiments ± SD. To make several comparisons, we used the Tukey post hoc test. *Significantly different versus control (p < 0.05). #Significantly different versus plain formula (p < 0.05). $Significantly different versus FLV raw (P < 0.05).
Western blot for protein expression of Bcl-2, Bax, Caspase 3, and p 53
The data for Bcl-2, Bax, Caspase 3, and p 53 expression showed significant (p < 0.05) increase in p 53 and Caspase 3 expression of FLV-PL-ALA-MEL over compared to control, plain formula, and FLV-raw groups (Fig. 10A,B). Original scans and gel picture are available as supplementary data (S1, S2). FLV-PL-ALA-MEL also showed significant (p < 0.05) increase in the expression BAX over control and plain formula groups. On the other hand, FLV-PL-ALA-MEL showed significant (p < 0.05) reduction of Bcl2 expression compared to the other investigated groups.
Bcl-2, Bax, Caspase 3, and p 53 proteins expression, Western blots (A) and histogram (B) for the groups (I) control (II) plain formula, (III) FLV and (IV) FLV-PL-ALA-MEL. *Significantly different versus control (p < 0.05). #Significantly different versus plain formula (p < 0.05). $Significantly different versus FLV raw (P < 0.05).
Mitochondrial membrane potential study
With a view to investigating whether or not the pro-apoptotic, as well as antiproliferative FLV-PL-ALA-MEL activities, induced alterations on MMP, an assessment, was carried out of the percentage variation with respect to MMP caused by varying treatments when compared with control cells. It was interesting to note that the optimized FLV-PL-ALA-MEL could make noticeable changes in MMP when compared with control and plain formula cells (Fig. 11).
The effect of optimized FLV-PL-ALA MEL on Caco2 cells’ MMP variation. Normationalization of values took place with respect to untreated (control) Caco2 cells and expressed as variation percentage. Data denote the mean of four independent experiments ± SD. To make several comparisons, we used the Tukey post hoc test. *Significantly different versus control (p < 0.05). #Significantly different versus Plain formula (p < 0.05).
Discussion
Approved by the FDA, FLV has the capability of curtailing HMG-CoA reductase, which is why it is prescribed to prevent cardiovascular problems and also for lowering LDL/total cholesterol levels9,40. Along with MEL, it is capable of exerting toxic as well as antineoplastic impacts against varied cancer treatment-related experimental models23,41,42,43,44,45. For this reason, it is believed to hold promise as a therapeutic option to treat cancer patient. MEL is a 26 amino acid cationic polypeptide resulting from bee venom that have potent anticancer activity. MEL limited in vivo application is its hemolytic effect as previously reported46. However, MEL has been the focus of anticancer preclinical studies according to its lytic activities in several types of tumors47. Previous report revealed that MEL nanoparticles markedly inhibited tumor growth ability48. Nevertheless, FLV and MEL usage is not impervious to adverse side effects particularly when the dose of MEL is high49,50. This underscores the necessity to develop an optimized formulation comprising combination of active ingredients to synergistically perform anticancer activities and find application in future clinical trials.
The endeavor of the experimental design, as well as the optimization process, was to understand the manner in which the variables affected the investigated responses while optimizing their levels to accomplish the objectives of this study. The size of a particle assumes importance in the context of this study. The findings of our study show that the size increases when there is an increase in all the studied factors. The enhanced interactions of negatively charged components FLV, PL and ALA with MEL possibly increasing the conjugate’s size. Notably, the values of zeta potential have a direct correlation with MEL because of the latter’s cationic nature that constitutes a key element of honeybee venom peptide devoid of negative charges but comprises six positive charges51.
After obtaining the optimized formula, in vitro experiments was conducted wherein tested the ability of the optimized formula FLV-PL-ALA-MEL to enhance the antineoplastic activity against Caco2 cells, representing a robust experimental model to examine statins’ toxic potentiality either in isolation or when used alongside with other active ingredients. The enhanced therapeutic potentiality of FLV-PL-ALA-MEL is first indicated in the data as shown by Fig. 5, concerning values of IC50 used for assessing anticancer agents’ toxic potentiality and antiproliferative activities. For example, it was found that the aforementioned FLV-PL-ALA-MEL value was considerably lower when compared to the plain formula or FLV raw. Importantly, the symbiotic cytotoxic impact derived by combining MEL and FLV assumes great significance from varied standpoints. Despite the fact that statins continue to be used extensively for traditional as well as non-traditional therapies to treat cancer52,53, MEL’s utilization within clinical practices, despite its perceived efficacy in treating cancer does give rise to several questions because of the non-specific cytotoxicity associated with it together with its hemolytic activity, especially when the dosage prescribed of this drug is on the higher side23,54. For this reason, it becomes necessary to explore novel formulations and harmonize the two drugs’ antineoplastic activities augmentation in a formula that is properly optimized. Doing so significantly enhances the scope for boosting the therapeutic properties of FLV while simultaneously lowring the number of its side effects.
Further evidence of the above-mentioned optimized formulation's anticancer attributes, when compared with other experimental scenarios, was seen after investigating how the varied treatments affected the phases of the Caco2 cell cycle (Fig. 6). The figure shows that this optimized treatment was indeed able to effectively reduce Caco2 cells’ proliferation. This was demonstrated by a decline in the transition from G1 to S and also by curtailing the G2-M phase transition. The strength of these impacts could be predicated on FLV’s ability for inhibiting cancer’s proliferation with augmenting effect of MEL24,55.
Screening of apoptotic activity is vital in the development of anticancer agents. It is also useful in the evaluation of drug delivery systems. This study examined how various treatments impacted the Caco2 cells’ percentage going through necrosis or apoptosis to illuminate the improved FLV-PL-ALA-MEL antiproliferative effect and to determine whether pro-apoptotic activities were also observed. The expression level of pro and antiapoptotic signifies the rate of apoptosis. This study also examined the formulation’s pronecrotic and pro-apoptotic effects. The findings with regard to the alterations observed in Caco2 cells’ antiproliferative activity and cytotoxicity under the conditions created in this study’s experiments showed that FLV-PL-ALA-MEL did considerably enhance the cell population percentage in necrosis as well as late apoptosis phases, as well as the overall cell death when compared with the plain formula or FLV raw (Fig. 7). Interestingly, the findings of this study are in alignment with those of prior studies that exemplified FLV’s capability to induce apoptosis across varied non-neoplastic types of cells9,40,55. At the same time, the pro-apoptotic activity of FLV gets implemented at extremely low concentrations because of its nano-formulation and with MEL. This is evidenced by the drug’s extremely low levels of activity. These findings were also augmented by the above-mentioned synergistic formula’s capability of modulating BAX, Caspase 3, P53 as well as BCL-2 protein levels (Fig. 8) within the Caco2 cells. BAX protein expression pertains to events of pro-apoptosis56. On the other hand, BCL-2 protein pertains to antiapoptotic events56,57,58. BAX protein concentration modulation within Caco2 cells ascertained by varying experimental scenarios is shown in Fig. 8. The increased ratio of BAX/BCL-2 ratio agrees with the observations of a prior study that demonstrated FLV’s ability to successfully cause lymphoma cells’ death by increasing pro-apoptotic members’ activation and the simultaneous inhibition of BCL-259. The optimized formula FLV-PL-ALA-MEL showed significant (p < 0.05) increase in levels of TNF-α and reduction in NF-kB (Fig. 9). NF-kB is a transcription factor that once activated, regulates the transcription of various proinflammatory cytokines such as TNF-α60,61. Furthermore, the proapotptotic activity of FLV-PL-ALA-MEL has been confirmed using Western plot technique that indicated enhanced protein expression of Bax, caspase 3 and P53 as well as reduced expression of Bcl2 (Fig. 10). The optimized formula FLV-PL-ALA-MEL exhibit ability to cause noticeable alterations in Caco2 cells’ MMP when compared with plain formula and untreated cells (Fig. 11). As a matter of fact, it was found that MEL treatment could only considerably reduce the percentage of MMP. However, this may be contingent on the peptide structure of MEL as well as its cationic attributes. Of the various ways to regulate Caco2 cells’ proliferative status, it has been found that the optimized formula is able to implement its anticancer impact effectively via the promulgation of pro- necrotic and apoptotic phenomena as well as MMP modulation.
From these findings, it can be inferred that the antineoplastic drugs can be combined with various natural ingredients to emerge as a potent anticancer contributor. Taking into consideration the physicochemical attributes of the optimized formula FLV PL ALA MEL used in this study, it can be seen that the nano-conjugates are able to efficiently improve the cytotoxicity of FLV. However, in order to better understand the formulation’s pharmacokinetic profile in colon cancer in animal models, it is necessary to conduct more studies in the future.
Conclusions
This study employed experimental designs for response surface methodology (Box–Behnken designs) to prepare FLV-PL-ALA-MEL and their concomitant optimization. In this process, the particle size was minimized. On the other hand, the zeta potential was maximized. According to the in vitro research conducted in cells of Caco2 colon cancer, reduced IC50 (thus implying increased toxicity) and the potentiality for antiproliferation of cancer cells was observed by the impact of the optimized FLV-PL-ALA-MEL formula. This optimized formula can be said to hold promise as it may signify a new mechanism to develop more efficacious and precise antineoplastic therapies that could then emerge as an effective option in treating colon cancer.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Change history
13 November 2024
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1038/s41598-024-78897-z
References
Ukomadu, C. & Dutta, A. p21-dependent inhibition of colon cancer cell growth by mevastatin is independent of inhibition of G1 cyclin-dependent kinases. J. Biol. Chem. 278, 43586–43594 (2003).
Shon, Y. H. & Nam, K. S. Chemopreventive effect of protein extract of Asterina pectinifera in HT-29 human colon adenocarcinoma cells. Arch. Pharm. Res. 29, 209–212 (2006).
Alhakamy, N. A. et al. Chitosan-based microparticles enhance ellagic acid’s colon targeting and proapoptotic activity. Pharmaceutics 12, 1–14 (2020).
Jain, S. K. & Jain, A. Target-specific drug release to the colon. Expert Opin. Drug Deliv. 5, 483–498 (2008).
Aiello, P. et al. Medicinal plants in the prevention and treatment of colon cancer. Oxid. Med. Cell. Longev. 2019, 2075614 (2019).
Reddy, B. S. Diet and colon cancer: Evidence from human and animal model studies. in Diet, Nutrition, and Cancer: A Critical Evaluation 47–66 (CRC Press, 2018). https://doi.org/10.1201/9781351071406-4.
Shirin, H. et al. Lovastatin augments sulindac-induced apoptosis in colon cancer cells and potentiates chemopreventive effects of sulindac. Gastroenterology 117, 838–847 (1999).
Alhakamy, N. A. et al. Piceatannol-loaded emulsomes exhibit enhanced cytostatic and apoptotic activities in colon cancer cells. Antioxidants 9, 419 (2020).
Fahmy, U. A. Augmentation of fluvastatin cytotoxicity against prostate carcinoma PC3 cell line utilizing alpha lipoic-ellagic acid nanostructured lipid carrier formula. AAPS PharmSciTech 19, 3454–3461 (2018).
Alhakamy, N. A. et al. Fluvastatin-Loaded Emulsomes Exhibit Improved Cytotoxic and Apoptosis in Prostate Cancer Cells. AAPS PharmSciTech 22, (2021).
Gazzerro, P. et al. Pharmacological actions of statins: A critical appraisal in the management of cancer. Pharmacol. Rev. 64, 102–146 (2012).
Shay, K. P., Moreau, R. F., Smith, E. J., Smith, A. R. & Hagen, T. M. Alpha-lipoic acid as a dietary supplement: Molecular mechanisms and therapeutic potential. Biochim. Biophys. Acta Gen. Subj. 1790, 1149–1160 (2009).
Dozio, E. et al. The natural antioxidant alpha-lipoic acid induces p27Kip1-dependent cell cycle arrest and apoptosis in MCF-7 human breast cancer cells. Eur. J. Pharmacol. 641, 29–34 (2010).
Aldawsari, H. M. et al. Development of a fluvastatin-loaded self-nanoemulsifying system to maximize therapeutic efficacy in human colorectal carcinoma cells. J. Drug Deliv. Sci. Technol. 46, 7–13 (2018).
El-Helw, A.-R. M. A.-R. M. & Fahmy, U. A. Improvement of fluvastatin bioavailability by loading on nanostructured lipid carriers. Int. J. Nanomed. 10, 5797–5804 (2015).
Graaf, M. R., Richel, D. J., van Noorden, C. J. F. & Guchelaar, H. J. Effects of statins and farnesyltransferase inhibitors on the development and progression of cancer. Cancer Treat. Rev. 30, 609–641 (2004).
Demierre, M. F., Higgins, P. D. R., Gruber, S. B., Hawk, E. & Lippman, S. M. Statins and cancer prevention. Nat. Rev. Cancer 5, 930–942 (2005).
Campbell, M. J. et al. Breast cancer growth prevention by statins. Cancer Res. 66, 8707–8714 (2006).
Brown, A. J. Cholesterol, statins and cancer. Clin. Exp. Pharmacol. Physiol. 34, 135–141 (2007).
Chan, K. K. W., Oza, A. M. & Siu, L. L. The statins as anticancer agents. Clin. Cancer Res. 9, 10–19 (2003).
Carlin, C. M., Peacock, A. J. & Welsh, D. J. Fluvastatin inhibits hypoxic proliferation and p38 MAPK activity in pulmonary artery fibroblasts. Am. J. Respir. Cell Mol. Biol. 37, 447–456 (2007).
Al-Rabia, M. W. et al. Repurposing of sitagliptin-melittin optimized nanoformula against sars-cov-2: Antiviral screening and molecular docking studies. Pharmaceutics 13, 1–21 (2021).
Gajski, G. & Garaj-Vrhovac, V. Melittin: A lytic peptide with anticancer properties. Environ. Toxicol. Pharmacol. 36, 697–705 (2013).
Kong, G. M. et al. Melittin induces human gastric cancer cell apoptosis via activation of mitochondrial pathway. World J. Gastroenterol. 22, 3186–3195 (2016).
Liu, S. et al. Melittin prevents liver cancer cell metastasis through inhibition of the Rac1-dependent pathway. Hepatology 47, 1964–1973 (2008).
Mahmoudi, H., Alikhani, M. Y. & Imani Fooladi, A. A. Synergistic antimicrobial activity of melittin with clindamycin on the expression of encoding exfoliative toxin in Staphylococcus aureus. Toxicon 183, 11–19 (2020).
Al-Rabia, M. W. et al. Boosting curcumin activity against human prostatic cancer PC3 cells by utilizing scorpion venom conjugated phytosomes as promising functionalized nanovesicles. Drug Deliv. 29, 807–820 (2022).
Gomes, F. P. et al. Development and validation of stability-indicating hplc methods for quantitative determination of pravastatin, fluvastatin, atorvastatin, and rosuvastatin in pharmaceuticals. Anal. Lett. 42, 1784–1804 (2009).
Fahmy, U. A., L. Alaofi, A., Awan, Z. A., Alqarni, H. M. & Alhakamy, N. A. Optimization of thymoquinone-loaded coconut oil nanostructured lipid carriers for the management of ethanol-induced ulcer. AAPS PharmSciTech 21, 1–10 (2020).
Alhakamy, N. A. et al. Encapsulation of lovastatin in zein nanoparticles exhibits enhanced apoptotic activity in HepG2 Cells. Int. J. Mol. Sci. 20, E5788 (2019).
Fahmy, U. A. et al. The encapsulation of febuxostat into emulsomes strongly enhances the cytotoxic potential of the drug on HCT 116 colon cancer cells. Pharmaceutics 12, 1–17 (2020).
Van Engeland, M., Nieland, L. J. W., Ramaekers, F. C. S., Schutte, B. & Reutelingsperger, C. P. M. Annexin V-affinity assay: A review on an apoptosis detection system based on phosphatidylserine exposure. Cytometry 31, 1–9 (1998).
Naseri, M. H. et al. Up regulation of Bax and down regulation of Bcl2 during 3-NC mediated apoptosis in human cancer cells. Cancer Cell Int. 15, 55 (2015).
Chipuk, J. E. et al. Direct activation of Bax by p53 mediates mitochondrial membrane permeabilization and apoptosis. Science (80-. ). 303, 1010–1014 (2004).
Liu, Q. S. et al. Ellagic acid protects against neuron damage in ischemic stroke through regulating the ratio of Bcl-2/Bax expression. Appl. Physiol. Nutr. Metab. 42, 855–860 (2017).
Mahmood, T. & Yang, P. C. Western blot: Technique, theory, and trouble shooting. N. Am. J. Med. Sci. 4, 429–434 (2012).
Eid, B. G. et al. Melittin and diclofenac synergistically promote wound healing in a pathway involving TGF-β1. Pharmacol. Res. 175, (2022).
Ahmed, O. A. A. et al. Optimized vinpocetine-loaded vitamin E D-α-tocopherol polyethylene glycol 1000 succinate-alpha lipoic acid micelles as a potential transdermal drug delivery system: In vitro and ex vivo studies. Int. J. Nanomed. 14, 33–43 (2018).
Badr-Eldin, S. M. et al. Optimized semisolid self-nanoemulsifying system based on glyceryl behenate: A potential nanoplatform for enhancing antitumor activity of raloxifene hydrochloride in MCF-7 human breast cancer cells. Int. J. Pharm. 600, 120493 (2021).
Ali, N. et al. Fluvastatin interferes with hepatitis C virus replication via microtubule bundling and a doublecortin-like kinase-mediated mechanism. PLoS ONE 8, 1–10 (2013).
Elsayed, M. et al. Synergistic antiproliferative effects of zoledronic acid and fluvastatin on human pancreatic cancer cell lines: An in Vitro study. Biol. Pharm. Bull. 39, 1238–1246 (2016).
Zhang, W., Wu, J., Zhou, L., Xie, H.-Y. & Zheng, S.-S. Fluvastatin, a lipophilic statin, induces apoptosis in human hepatocellular carcinoma cells through mitochondria-operated pathway. Indian J. Exp. Biol. 48, 1167–1174 (2010).
Bocci, G. et al. Fluvastatin synergistically enhances the antiproliferative effect of gemcitabine in human pancreatic cancer MIAPaCa-2 cells. Br. J. Cancer 93, 319–330 (2005).
Chang, S. N., Kim, H. J. & Lee, K. C. Melittin, a major polypeptide of bee venom, increases radiosensitivity of breast cancer in vitro and in vivo. Int. J. Radiat. Oncol. 108, e527 (2020).
Lee, C. et al. Targeting of M2-like tumor-associated macrophages with a melittin-based pro-apoptotic peptide. J. Immunother. Cancer 7, 147 (2019).
Jin, H. et al. Tumor ablation and therapeutic immunity induction by an injectable peptide hydrogel. ACS Nano 12, 3295–3310 (2018).
Zhou, J. et al. Delivery strategies for melittin-based cancer therapy. ACS Appl. Mater. Interfaces 13, 17158–17173 (2021).
Yu, X. et al. Melittin-lipid nanoparticles target to lymph nodes and elicit a systemic anti-tumor immune response. Nat. Commun. 11, (2020).
Rady, I., Siddiqui, I. A., Rady, M. & Mukhtar, H. Melittin, a major peptide component of bee venom, and its conjugates in cancer therapy. Cancer Lett. 402, 16–31 (2017).
Mascitelli, L. & Pezzetta, F. Fluvastatin and cancer: Letter [1]. Int. J. Clin. Pract. 61, 168 (2007).
El-Aarag, B., Magdy, M., AlAjmi, M. F., Khalifa, S. A. M. & El-Seedi, H. R. Melittin exerts beneficial effects on paraquat-induced lung injuries in mice by modifying oxidative stress and apoptosis. Molecules 24, (2019).
Hardie, C., Jung, Y. & Jameson, M. Effect of statin and aspirin use on toxicity and pathological complete response rate of neo-adjuvant chemoradiation for rectal cancer. Asia. Pac. J. Clin. Oncol. 12, 167–173 (2016).
Browning, D. R. L. & Martin, R. M. Statins and risk of cancer: A systematic review and metaanalysis. Int. J. Cancer 120, 833–843 (2007).
Dempsey, C. E. The actions of melittin on membranes. BBA Rev. Biomembranes 1031, 143–161 (1990).
Badr-Eldin, S. M. et al. Cytotoxic and pro-apoptotic effects of a sub-toxic concentration of fluvastatin on OVCAR3 ovarian cancer cells after its optimized formulation to melittin nano-conjugates. Front. Pharmacol. 11, 642171 (2021).
Wong, R. S. Y. Apoptosis in cancer: From pathogenesis to treatment. J. Exp. Clin. Cancer Res. 30, 87 (2011).
Marie Hardwick, J. & Soane, L. Multiple functions of BCL-2 family proteins. Cold Spring Harb. Perspect. Biol. 5, (2013).
Tsujimoto, Y. Role of Bcl-2 family proteins in apoptosis: Apoptosomes or mitochondria?. Genes Cells 3, 697–707 (1998).
Qi, X. F. et al. HMG-CoA reductase inhibitors induce apoptosis of lymphoma cells by promoting ROS generation and regulating Akt, Erk and p38 signals via suppression of mevalonate pathway. Cell Death Dis. 4, e518 (2013).
Zhang, H. & Sun, S. C. NF-ΚB in inflammation and renal diseases. Cell Biosci. 5, 1–12 (2015).
Liu, T., Zhang, L., Joo, D. & Sun, S. C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2, 17023 (2017).
Acknowledgements
This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, Saudi Arabia, has funded this project under grant no. (RG-14-166-42). The authors, therefore, acknowledge with thanks DSR for technical and financial support.
Author information
Authors and Affiliations
Contributions
Conceptualization, N.A.,U.F. and M.W.; methodology,M.A.S., M.A.,O.A., W.Y.; software, M.A., M.A.S.; validation, W.Y., M.A.S. and M.W.; formal analysis, W.Y.; investigation, W.Y.; resources,S.B.M, H.M., N.A.; data curation, O.F.,N.A.; writing—original draft preparation,O.F., A.A., B.M., W.Y.; writing—review and editing, H.A., W.Y.; visualization H.M, S.M.; supervision, N.A..; project administration, M.A.,N.A.; funding acquisition, M.A.S. ,N.A.. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41598-024-78897-z
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alfaleh, M.A., Fahmy, O., Al-Rabia, M.W. et al. RETRACTED ARTICLE: Hybrid nanoparticulate system of Fluvastatin loaded phospholipid, alpha lipoic acid and melittin for the management of colon cancer. Sci Rep 12, 19446 (2022). https://doi.org/10.1038/s41598-022-24151-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-24151-3