Abstract
The COVID-19 pandemic had negative consequences for mental health, yet it is unknown how and to what extent the psychological outcomes of this stressful event are moderated by individual traits. Alexithymia is a risk factor for psychopathology, and thus likely predicted individual differences in resilience or vulnerability to stressful events during the pandemic. This study explored the moderating role of alexithymia in the relationships of pandemic-related stress with anxiety levels and attentional bias. The participants were 103 Taiwanese individuals who completed a survey during the outbreak of the Omicron wave. Additionally, an emotional Stroop task including pandemic-related or neutral stimuli was used to measure attentional bias. Our results demonstrate that pandemic-related stress had a lesser impact on anxiety in individuals with a higher level of alexithymia. Moreover, we found that in individuals with higher exposure to pandemic-related stressors, a higher level of alexithymia indicated less attentional bias toward COVID-19-related information. Thus, it is plausible that individuals with alexithymia tended to avoid pandemic-related information, which could temporarily relieve stressors during the pandemic.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) declared the COVID-19 a pandemic in March 2020; thereafter, dramatic global spread occurred1. Currently, the number of infections and the case fatality rate continue to accumulate2,3. Compared to other countries, Taiwan was relatively resilient to the threat of COVID-19 due to acute awareness of the news about COVID-19 and rapid implementation of approaches to protect public health by the government4,5. However, the Omicron variant wave struck Taiwan in May 2022, and the psychological impacts were profound. Compared to previous waves, the Omicron variants were more contagious6,7, with breakthrough infections occurring even in individuals with multiple vaccine combinations8. With the greater concern over infection during this wave, it is plausible that psychological impacts such as frustration, irritability, burnout, and insomnia would become widespread in response to the prolonged restrictions of social isolation and quarantine practices2. Thus, it is vital to explore the psychological impact of COVID-19 on Taiwanese individuals during this wave.
Compared to the prepandemic period, psychological problems such as depression, sleep disorders, and posttraumatic stress symptoms (PTSS) have been frequently reported in the general population during the pandemic9,10,11,12. Recent studies have suggested that these psychological problems are associated with exposure to COVID-19-related stressors13,14, including social isolation, financial losses, and changes in interpersonal relationships, as well as health-related factors, such as uncertainty about the length of the pandemic process and fears of infection and its consequences9,13,15. These detrimental effects may hinder emotion regulation and the ability to attend to and retrieve information; moreover, pandemic-related restrictions can impact not only short-term but also long-term mental health9. These pandemic-related stressors can lead to psychological and physiological risks, such as anxiety, depression, poor physical condition and disrupted emotional and cognitive functioning13,16,17,18,19,20.
Psychological outcomes of exposure to stressful events are moderated by individual traits21,22,23,24. Reactions to pandemic-related stressors may vary across individuals25. It is plausible that some individuals are more susceptible to stress and more likely to experience mental health problems during lockdown26,27. Thus, identifying individual differences in resilience or vulnerability to stressful events is critical to promote well-being during the pandemic.
Individual traits such as alexithymia have been implicated as a modulator of the psychological outcomes28. Alexithymia is a multifaceted personality trait involving difficulty in identifying and expressing feelings and an externally oriented thinking style29,30; it is associated with stress-related disorders, including anxiety, PTSS and depression31,32,33. According to the stress-alexithymia hypothesis, a lack of emotional awareness in individuals with alexithymia may lead to maladaptive responses when encountering stressors, in turn increasing susceptibility to mental problems34. In support of this, empirical evidence has determined that alexithymia is a transdiagnostic risk factor for psychopathology35,36,37. For instance, research has shown that alexithymia moderates the association between traumatic experiences and PTSS38,39. Increased levels of anxiety have also been reported as a common psychological reaction to the COVID-19 pandemic40,41,42, thus receiving ample attention in psychopathological research. However, these studies have not considered the moderation effects of alexithymia. Considering that stress levels have increased dramatically during the COVID-19 pandemic9, it is important to further explore whether alexithymia moderates the association between COVID-19-related stressors and levels of anxiety.
Recent studies have also highlighted the importance of examining attentional bias in response to elevated levels of stress during COVID-1917,43,44. Specifically, attentional bias is defined as the tendency to pay attention to survival-related information, reflecting greater attentional allocation toward negative information than neutral information45,46,47. Recent studies have indicated that even mere exposure to negative information about COVID-19 (e.g., news or rumors about COVID-19) leads to increased levels of anxiety48. This negative information is distributed through various media platforms, making it impossible to ignore it in daily life. According to evolutionary accounts, negative information is better at capturing attention (i.e., signal detection of potential threats or contamination) and eliciting subsequent physiological and behavioral responses49,50,51. Negative stimuli may convey survival-related information, eliciting a defensive response to minimize the exposure to contamination (e.g., bodily fluids associated with infection or diseases)50,52,53.
Despite the necessity of effective detection of potential threats for survival, there are individual differences in attentional allocation toward threatening information46,47,54. In clinical research, attentional bias toward threat-related information is a robust phenomenon observed in anxious populations45,55,56. For instance, individuals with anxiety disorders showed faster response times toward threat-related stimuli than toward the neutral stimuli, reflecting hypervigilance toward potential harm57,58. Moreover, attentional bias toward threat-related information has been suggested as a crucial pathogenetic indicator for the etiology and maintenance of anxiety disorders58,59. However, this effect is not well established in alexithymia research29. Specifically, there is an unresolved debate regarding attentional bias and whether alexithymia causes disengagement difficulties (i.e., overresponding) or an early avoidance of processing threats29,54,60. Based upon this debate, two main hypotheses have been proposed. The overresponding hypothesis suggests that upon the detection of potential threats, individuals with a higher level of alexithymia may exhibit prolonged attention to unpleasant information versus neutral information29,54. This maintenance of attentional bias may be due to difficulty in regulating top-down attentional allocation for emotionally ambiguous situations, biasing attention in a threat-related manner and selecting negative (or less positive) interpretations of potential threats61. In response to this preattentional evaluation of threats, several studies have reported that individuals with alexithymia demonstrate hypervigilance and unnecessary depletion of attentional resources, resulting in difficulty in disengaging away from the threatening stimuli62,63. Conversely, according to the vigilance–avoidance hypothesis of attentional bias57,64, individuals with alexithymia may demonstrate early facilitation of orienting attention toward potential threats, which initiates their subsequent defensive reactions (i.e., early avoidance) for further processing the negative stimuli. It is proposed that this reflects an immediate defensive approach to downregulate intense subjective experiences65,66. In support of this notion, previous studies found that individuals with alexithymia exhibit less effort (i.e., faster response time) for processing negative information compared to neutral information, which is due to lower allocation of attentional resources toward emotional information67,68,69. Currently, the ecological manifestation of these attentional biases in the presence of real-life stressors has not been elucidated. Given these controversial results, such research is crucial to understand how individual differences in alexithymic traits promote vulnerability or resilience to stressful experiences during the COVID-19 pandemic. Thus, we explored whether alexithymic traits modulate the association between COVID-19-related stressors and attentional bias.
In this cross-sectional study, we aimed to investigate whether alexithymia contributes to vulnerability to anxiety levels in response to stressors related to the COVID-19 pandemic; we focused on the responses of Taiwanese college students to the Omicron wave, and assessments were conducted from May 10 to June 16, 2022. Several studies have investigated the role of alexithymia in the COVID-19 pandemic in both the general population and among health care workers70,71,72,73. Nevertheless, it remains unclear whether alexithymia is a potential risk factor for psychopathology during the COVID-19 pandemic among the college student population. Given that college students are more vulnerable to stress-related symptoms due to their lack of life experience and emotional instability74,75, we hypothesized that COVID-19-related stressors elevate levels of anxiety and that this effect is moderated by alexithymia. Our second objective was to examine attentional bias toward negative information about the COVID-19 pandemic. We proposed that negative information is better at attracting attention and at triggering either disengagement or early avoidance of threats62,68. Negative information may convey critical survival-related information during the pandemic, eliciting reactivity to minimize exposure to infection50,52,53. Thus, we hypothesized that pandemic-related stressors would influence attentional bias to negative information and that this effect would be moderated by alexithymia. This work is anticipated to provide empirical evidence of the role of alexithymia in psychopathological outcomes during the pandemic.
Methods
Participants
A total of 192 students accepted an invitation via social media to complete a battery of self-report questionnaires in an online survey. For inclusion, students had to meet the following inclusion criteria: (1) right-handed, (2) normal or corrected-to-normal vision, (3) normal hearing, and (4) free of psychiatric disorders, neurological diseases, or psychotropic medication use. To control for the influence of anxiety and depressive symptoms28,29,76, the 9-item Patient Health Questionnaire (PHQ-9) and the 7-item generalized anxiety disorder scale (GAD-7) were also conducted to screen for psychiatric disorders. Of these students, 62 students with scores of ten or greater on the PHQ-9 and GAD-7 were excluded77,78,79. Students were contacted again later during the pandemic; at this time, 27 students declined to participate in the experimental session, resulting in a final sample of 103 participants (65 females, Mage = 23.13, SDage = 2.81). Informed consent was obtained from each participant. The informed consent procedures were approved by the Research Ethics Committee of the National Tsing-Hua University. The experimental procedures were carried out in accordance with the Declaration of Helsinki. All participants received reimbursement for their time and participation in the study (approximately 15 USD).
Measures
Levels of alexithymia
The level of self-reported alexithymia was assessed using the Chinese version of the Toronto Alexithymia Scale (TAS-20-TW)80. The TAS-20 consists of 20 items rated on a 5-point Likert scale and features a three-factor structure: (1) difficulty identifying feelings (DIF), (2) difficulty describing feelings (DDF), and (3) externally oriented thinking (EOT). The stability of this factor structure has been confirmed in the Taiwanese population80. On the TAS-20, potential scores range from 20 to 100. Higher scores on this scale indicate a higher level of alexithymia. Regarding reliability, these items had satisfactory internal consistency (Cronbach’s α = 0.85).
Pandemic-related stress
Pandemic-related stress was measured using a 10-item self-report questionnaire adapted from Weissman13. These items mainly examine the extent to which participants’ lives were impacted by the COVID-19 pandemic (e.g., income, personal safety). Participants rate each item on a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”). We utilized the total score (the sum of the 10 items) in the analysis. These items had satisfactory internal consistency (Cronbach’s α = 0.78).
Levels of state anxiety
Levels of state anxiety were measured using the Chinese version of the State-Trait Anxiety Inventory (C-STAI-S)81. In the state anxiety subscale, participants are asked to rate how they feel at the present moment (e.g., “I am tense”). It consists of 20 items rated on a 4-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”). Higher scores indicate higher levels of state anxiety. These items had satisfactory internal consistency (Cronbach’s α = 0.92).
Attentional bias
Attentional bias was measured using the emotional counting Stroop task82,83, which was presented using E-Prime software [version 3.0; Psychology Software Tools (PST)]. Participants took the computerized test in a quiet room. Before the formal test, there were six practice trials with feedback to ensure that participants understood the task; these items involved different stimuli than those used in the formal test. Each participant achieved at least 80% accuracy in each condition in the practice session.
In the emotional counting Stroop task, participants were asked to perform a counting Stroop task preceded by emotional or neutral pictures. The task was categorized into congruent and incongruent conditions, with 60 trials each. For each of these conditions, trials were further divided into two emotional conditions, with 30 pandemic-related trials (e.g., images of pandemic-related objects, scenes of people getting vaccinated or people demonstrating COVID-19-related symptoms, scenes of social distancing behavior or people during lockdown) and 30 neutral trials (e.g., scenes of neutral objects, animals, or people with neutral expressions or in neutral situations). Additionally, 60 trials with either threatening or aversive pictures (e.g., scenes of aversive insects or threatening animals or scenes of people being threatened with weapons) were used as fillers in the congruent and incongruent conditions. Fillers are commonly used to obscure the nature of the task84,85,86,87. In the congruent condition, the number of words was consistent with the word’s meaning, such as ‘‘one’’, ‘‘two’’, ‘‘three’’, or ‘‘four”, but not in the incongruent condition. Participants were required to report the number of words (1–4) on the screen via button pressing, regardless of word meaning. The task consisted of three sessions, lasting approximately 8 min each. Within each testing session, trials were presented in a pseudorandomized order such that no more than three succeeding trials were from the same condition88. Each trial began with a fixation (e.g., white square) for 150 ms, followed by an emotional prime of a neutral, filler, or pandemic-related picture presented for 250 ms. After the emotional primes, an item of the counting Stroop task was presented for 1500 ms. The intertrial intervals (ITIs) were varied randomly among 1000 ms, 1500 ms, and 2000 ms (see Fig. 1). The inclusion of a variable ITI is designed to prevent the carry-over effects of emotional responses82,83,88,89. Moreover, the pseudorandomized presentation of the trials should ensure that any carryover would fall equally on emotional and neutral trials90. In the present study, reaction time (RT) was used as the behavioral index of Stroop performance. Longer response latencies are interpreted as greater interference and higher attentional bias to the emotional content of the presented stimuli91,92,93. Analyses for RT were performed on only correct trials, and we removed outlier RTs more than 2.5 SDs from the mean in each condition for each participant. After removing outliers, the mean RTs were calculated within each condition. In total, 4.19% of observations were excluded. Subsequently, attentional bias was calculated by subtracting the neutral trials’ RT from the pandemic trials’ RT in the incongruent condition82,83.
Stimuli characteristics
As stimuli, 61 pictures were selected from the International Affective Picture System (IAPS)94, and 29 pictures were chosen from the public photo archives95,96,97,98,99; each picture was presented twice in the task, once each in the congruent and incongruent conditions. Pictures were matched for size and brightness. Twenty-nine adults who did not participate in the experiment were asked to rate the emotional characteristics of the stimuli on a 9-point scale, including emotional valence (1 = very unpleasant to 9 = very pleasant) and arousal (1 = very calm to 9 = highly arousing)82,100. Additionally, participants were asked to rate whether the stimuli were associated with COVID-19 on a 9-point scale (1 = not at all to 9 = strongly associated). Pandemic-related pictures had values of 5 or higher on the relatedness scale. Table 1 lists the stimuli characteristics for each condition. Regarding emotional characteristics, valence was significantly lower and arousal was significantly higher for pandemic-related pictures than for neutral pictures (ps < 0.05). Moreover, the selected pandemic-related pictures had a higher pandemic-relatedness score than the neutral pictures (p < 0.05).
Data analysis
All analyses were performed using SPSS version 25.0. First, descriptive statistics and intercorrelations among all variables were calculated. Then, to test the hypotheses, two moderation models were constructed using Hayes PROCESS macro-Model 1101. To examine the first aim of the study, we entered alexithymia as the moderator of the relationship between pandemic-related stress and state anxiety of individuals. To examine the second aim, we entered alexithymia as the moderator of the relationship between pandemic-related stress and attentional bias. In the analysis, both alexithymia and pandemic-related stress were centered to the mean, and the bias-corrected bootstrap 95% confidence interval, based on 5000 bootstrap samples, was calculated to evaluate the conditional effect at different levels of alexithymia101. Using the Johnson–Neyman method, we plotted the conditional effects of these two models.
Results
Descriptive statistics
Descriptive statistics and Pearson’s correlation coefficients among all variables are shown in Table 2.
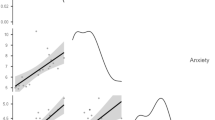
Alexithymia, pandemic-related stress, and state anxiety
As shown in Table 3 (Model 1), three predictors accounted for 21% of the total variance in the outcome, F (3, 99) = 8.96, p < 0.001. Regarding the main effects, the results revealed that greater pandemic-related stress was significantly associated with greater state anxiety, b = 0.31, SE = 0.15, t = 2.09, p < 0.05, and that higher alexithymia levels were significantly associated with greater state anxiety, b = 0.18, SE = 0.09, t = 2.08, p < 0.05. Additionally, the pandemic-related stress × alexithymia interaction was significant, b = − 0.05, SE = 0.01, t = − 3.66, p < 0.001, and ΔR2 = 0.11, indicating that alexithymia moderated the association between pandemic-related stress and state anxiety. The interaction is plotted in Fig. 2A. The conditional effect of pandemic-related stress on state anxiety was calculated at 1 SD below the mean, the mean, and 1 SD above the mean of alexithymia. The results revealed that in participants with lower levels of alexithymia, greater pandemic-related stress caused greater state anxiety, b = 0.82, SE = 0.21, t = 4.00, p < 0.001. However, with increased levels of alexithymia, the effect of pandemic-related stress on state anxiety became weaker. Furthermore, application of the Johnson–Neyman method revealed that the effect of pandemic-related stress on state anxiety was nonsignificant when the alexithymia level of participants was higher than 46.05 (see Fig. 2B).
Alexithymia, pandemic-related stress, and attentional bias
As shown in Table 3 (Model 2), three predictors accounted for 22% of the total variance in the outcome, F (3, 99) = 9.13, p < 0.001. Regarding the main effects, the results revealed that greater pandemic-related stress was significantly associated with greater attentional bias, b = 2.00, SE = 0.46, t = 4.40, p < 0.001, and that higher levels of alexithymia were significantly associated with lower attentional bias, b = − 0.81, SE = 0.27, t = − 2.95, p < 0.01. Additionally, the pandemic-related stress × alexithymia interaction was significant, b = − 0.09, SE = 0.04, t = − 2.06, p < 0.05, and ΔR2 = 0.03, indicating that alexithymia moderated the association between pandemic-related stress and attentional bias. The interaction is plotted in Fig. 3A. The conditional effect of pandemic-related stress on attentional bias was also calculated at 1 SD below the mean, the mean, and 1 SD above the mean of alexithymia. The results revealed that in participants with lower levels of alexithymia, greater pandemic-related stress caused greater attentional bias, b = 2.91, SE = 0.64, t = 4.53, p < 0.001. However, with increased levels of alexithymia, the relationship between pandemic-related stress and attentional bias became weaker. Furthermore, application of the Johnson–Neyman method revealed that the effect of pandemic-related stress on attentional bias was nonsignificant when the alexithymia level of participants was higher than 54.90 (see Fig. 3B).
Discussion
This study aimed to determine whether alexithymia contributed to vulnerability to anxiety levels in response to COVID-19-related stressors among Taiwanese college students during the early phase of the Omicron wave in late spring of 2022. Our results revealed that alexithymia significantly moderated the relationship between pandemic-related stressors and levels of anxiety. Moreover, we found that among individuals with a higher level of alexithymia, exposure to these stressors had a lesser impact on anxiety levels. Our second aim was to explore the cognitive mechanism of attentional bias in response to stressful events during the pandemic. Our results indicate that alexithymia moderated the association between pandemic-related stressors and attentional bias. For individuals with higher alexithymia levels, exposure to the stressors had a smaller impact on attentional bias. Currently, our findings have several theoretical implications in the context of the COVID-19 pandemic.
Our first finding was that the degree of exposure to pandemic-related stressors was associated with anxiety levels and that this relationship was moderated by alexithymia. The stress-alexithymia hypothesis predicts that in individuals with higher levels of alexithymia, higher arousal leads to greater mental problems34. Interestingly, in our cross-sectional study during the Omicron wave of the pandemic, pandemic-related stress had a lesser impact on anxiety among individuals with higher levels of alexithymia. Our results could be interpreted as avoidance of COVID-19-related stressors by alexithymic individuals. According to the accounts of experiential avoidance, alexithymia is considered a learned tendency to use maladaptive coping to deal with severe stress102,103. This tendency in individuals with alexithymia may be related to an unwillingness to tolerate aversive sensations, emotions, thoughts and memories, leading to alterations of the form or frequency with which they confront them33,104. Additionally, this learned tendency is reinforced and maintained as it provides immediate relief and reduced distress in threatening situations33,105,106; however, it is ultimately associated with the accumulation and intensification of unwanted emotions107. Thus, this detrimental effect of temporary relief from stress in individuals with alexithymia may predict the development of psychopathology104,108,109,110. The present results further suggest that alexithymia is a factor moderating mental health outcomes in the context of exposure to pandemic-related stressors, and these early defensive reactions to avoid stress may accumulate unpleasant emotions over time.
Our second finding was that alexithymia moderates the association between exposure to pandemic-related stressors and attentional bias. These findings are consistent with the vigilance-avoidance hypothesis of attentional bias64, which suggests that among individuals with higher exposure to pandemic-related stressors, higher levels of alexithymia indicate less attention toward negative information compared to neutral information (i.e., attentional bias oriented away from threatening information). The attentional bias literature has proposed an underlying mechanism of attentional allocation for individuals with alexithymia111,112. Specifically, decisions regarding coping with unwanted emotions are thought to be determined by appraisals of emotions (i.e., evaluation of whether the emotion is beneficial or detrimental to current goals and thus initiating up- or downregulation of emotions)112,113. With this mechanism, potential threats are detected in a way that buffers the anticipated harm45,55. In the present study, when individuals with alexithymia encountered COVID-19-related stimuli, the defensive pattern of early vigilance followed by avoidance prevented constant contact with threatening information (e.g., increasing numbers of confirmed cases and case fatality rates); thus, negative affect did not interfere with subsequent attentional processing (i.e., less attentional depletion) during the later decision stage. Importantly, early detection of a threat and subsequent shifting of attention away from the threat may provide temporary relief from stressors114,115,116. However, using this defensive mechanism is likely to exacerbate psychopathological problems in the long term117,118. In such a setting, the use of attentional avoidance of threatening information (or less problem-focused coping) makes individuals with alexithymia more vulnerable to increased exposure to pandemic-related stressors over time.
Taken together, the current findings have implications concerning for the mental wellbeing of individuals during the pandemic. Even though the college students in this study were a “low-risk” population (i.e., not predicted to suffer from psychiatric disorders at the early phase of the pandemic), individuals with alexithymia may have used maladaptive coping to downregulate emotions and achieve immediate relief from distress. However, their negative emotions may gradually accumulate during the postpandemic period. Our findings that alexithymia had a moderating role in this stress-symptom relationship may imply that alexithymic traits may identify vulnerable individuals under pandemic conditions. Additionally, this study further found that individuals with alexithymia may give limited attention to essential COVID-19-related information. Therefore, as the pandemic continues, these findings emphasize the importance of implementing policies to alleviate the stress (e.g., by providing support for financial loss, fears of contagion, and social isolation) experienced by young adults. These procedures may help to increase feelings of certainty and control, thus reducing tensions and improving resilience to stress during the pandemic. Moreover, it is plausible that the attentional avoidance of threats may stem from uncertainty; therefore, facilitating the absorption of accurate knowledge about COVID-19 (e.g., symptoms and characteristics of Omicron variants, preventive procedures) and conducting interventions that emphasize improving attentional control (e.g., mindfulness training, attentional bias modification) may potentially eliminate uncertainty119,120,121,122, facilitate the interpretation of threatening information, and enable better coping in the face of environmental threats123.
This study provides an integrated framework for exploring the role of alexithymia in mental health during the COVID-19 pandemic. However, certain limitations should be considered. First, the cross-sectional design means that conclusions regarding how alexithymia modulates the relationship between exposure to stressors and anxiety levels during the pandemic should be interpreted with caution75,124. Future longitudinal studies are needed to further examine whether alexithymia moderates the relationship between the perceived stress of pandemic events and changes in psychological symptoms over time. Second, the use of self-report measures (such as exposure to COVID-19-related stressors, alexithymia, and anxiety level) may lead to report bias; thus, other objective measurements should be considered in the future. Third, although the interpretations of attentional bias are based on a single, well-established measurement that shows consistent association with psychopathology92,125, alternative measurements (e.g., the Posner cueing task, dot-probe task accompanied by the use of eye-tracking technology) should be considered in the future for further validation. Fourth, our findings may not be generalized to the entire population due to the exclusion criterion (i.e., the anxiety and depressive symptoms). Considering that the effects of stress during the pandemic and alexithymia on mental health were found in relatively low-risk students in the current study, it is reasonable to believe that these findings may not be generalizable to populations with higher risk. Fifth, the relationship between attentional bias and mental disorders (i.e., anxiety) may be bidirectional, with anxiety exacerbating attentional bias and attentional bias aggravating anxiety126. Here, we examined whether alexithymic traits elicited attentional bias toward threat-related information. Future studies should further explore whether the maladaptive attentional bias in individuals with alexithymia lead to long-term mental health problems. Finally, recent research has reported that increasing numbers of psychiatric symptoms, such as anxiety and sleep disturbance, developed or persisted after acute COVID-19127. The severity of sleep disturbance was closely linked to high levels of anxiety and stress, reducing quality of life128. Alexithymia may also modulate other mental health issues during the pandemic, such as sleep disturbance and anxiety disorders; hence, further studies should clarify the role of alexithymia in the relationship between pandemic-related stressors and various mental health problems to develop a more comprehensive understanding of the long-term impacts of COVID-19.
In conclusion, pandemic-related stress had a lesser impact on anxiety among individuals with higher levels of alexithymia. Our results support experiential avoidance; in other words, that individuals with alexithymia may avoid unfavorable thoughts and emotions (e.g., stressful experiences). We further demonstrated that among individuals with higher perceived psychological stress, higher levels of alexithymia indicated less attentional bias toward COVID-19-related stimuli. This avoidance may provide immediate relief and decreased levels of anxiety during the COVID-19 pandemic, but this inflexible coping strategy may increase the risk for mental symptoms in reaction to pandemic-related stressors in the long term. Thus, future research should consider the long-term influences of the COVID-19 pandemic on psychopathology.
Data availability
The data and material used and/or analyzed during the current study are available from the corresponding authors (SHL and KTL) on reasonable request.
References
World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 79. https://apps.who.int/iris/handle/10665/331720 (2020).
Sun, T.-K., Chu, L.-C. & Hui, C. The psychological impact and influencing factors during different waves of COVID-19 pandemic on healthcare workers in Central Taiwan. Int. J. Environ. Res. Public Health 19, 10542 (2022).
Wu, Y.-C., Chen, C.-S. & Chan, Y.-J. The outbreak of COVID-19: An overview. J. Chin. Med. Assoc. 83, 217–220 (2020).
Summers, J. et al. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg. Health West. Pac. 4, 100044. https://doi.org/10.1016/j.lanwpc.2020.100044 (2020).
Wang, C. J., Ng, C. Y. & Brook, R. H. Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. JAMA 323, 1341–1342. https://doi.org/10.1001/jama.2020.3151 (2020).
Al-Tawfiq, J. A., Hoang, V.-T., Le Bui, N., Chu, D.-T. & Memish, Z. A. The emergence of the omicron (B.1.1.529) SARS-CoV-2 variant: What is the impact on the continued pandemic?. J. Epidemiol. Glob. Health 12, 143–146 (2022).
Araf, Y. et al. Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. J. Med. Virol. 94, 1825–1832 (2022).
Andrews, N. et al. Covid-19 vaccine effectiveness against the omicron (B.1.1.529) variant. N. Engl. J. Med. 386, 1532–1546 (2022).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 395, 912–920 (2020).
Kang, L. et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 87, 11–17 (2020).
Wang, C. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17, 1729 (2020).
Xiang, Y.-T. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229 (2020).
Weissman, D. G. et al. Contributions of emotion regulation and brain structure and function to adolescent internalizing problems and stress vulnerability during the COVID-19 pandemic: A longitudinal study. Biol. Psychiatry Glob. Open Sci. 1, 272–282 (2021).
Yang, C., Chen, A. & Chen, Y. College students’ stress and health in the COVID-19 pandemic: The role of academic workload, separation from school, and fears of contagion. PLoS ONE 16, e0246676. https://doi.org/10.1371/journal.pone.0246676 (2021).
Cai, H. et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. 26, e924171. https://doi.org/10.12659/msm.924171 (2020).
Bothe, K., Schabus, M., Eigl, E.-S., Kerbl, R. & Hoedlmoser, K. Self-reported changes in sleep patterns and behavior in children and adolescents during COVID-19. Sci. Rep. 12, 20412 (2022).
Cannito, L. et al. Health anxiety and attentional bias toward virus-related stimuli during the COVID-19 pandemic. Sci. Rep. 10, 16476. https://doi.org/10.1038/s41598-020-73599-8 (2020).
Gürsoy, B. K., Çakaloğullari, N. & Üzer, A. The effect of alexithymic characteristics on perceived stress and health anxiety during the COVID-19 pandemic. Eur. Rev. Med. Pharmacol. Sci. 25, 7127–7134 (2021).
Li, X. & Lyu, H. Epidemic risk perception, perceived stress, and mental health during COVID-19 pandemic: A moderated mediating model. Front. Psychol. 11, 563741 (2020).
Mattioli, A. V., Sciomer, S., Maffei, S. & Gallina, S. Lifestyle and stress management in women during COVID-19 pandemic: Impact on cardiovascular risk burden. Am. J. Lifestyle Med. 15, 356–359 (2021).
Carmassi, C. et al. Exploring PTSD in emergency operators of a major University Hospital in Italy: A preliminary report on the role of gender, age, and education. Ann. Gen. Psychiatry 17, 17 (2018).
Xiong, J. et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 277, 55–64 (2020).
Yan, L., Gan, Y., Ding, X., Wu, J. & Duan, H. The relationship between perceived stress and emotional distress during the COVID-19 outbreak: Effects of boredom proneness and coping style. J. Anxiety Disord. 77, 102328 (2021).
Zhou, X. et al. Risk factors of mental illness among adult survivors after the Wenchuan earthquake. Soc. Psychiatry Psychiatr. Epidemiol. 48, 907–915 (2013).
Faye, C., Mcgowan, J. C., Denny, C. A. & David, D. J. Neurobiological mechanisms of stress resilience and implications for the aged population. Curr. Neuropharmacol. 16, 234–270 (2018).
Osório, C., Probert, T., Jones, E., Young, A. H. & Robbins, I. Adapting to stress: Understanding the neurobiology of resilience. Behav. Med. 43, 307–322 (2017).
Vinkers, C. H. et al. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 35, 12–16 (2020).
Preece, D. A. et al. Why is alexithymia a risk factor for affective disorder symptoms? The role of emotion regulation. J. Affect. Disord. 296, 337–341 (2022).
Luminet, O., Nielson, K. A. & Ridout, N. Cognitive-emotional processing in alexithymia: An integrative review. Cogn. Emot. 35, 449–487 (2021).
Taylor, G. J., Bagby, R. M. & Parker, J. D. A. What’s in the name ‘alexithymia’? A commentary on ‘Affective agnosia: Expansion of the alexithymia construct and a new opportunity to integrate and extend Freud’s legacy’. Neurosci. Biobehav. Rev. 68, 1006–1020. https://doi.org/10.1016/j.neubiorev.2016.05.025 (2016).
Bratis, D. et al. Alexithymia and its association with burnout, depression and family support among Greek nursing staff. Hum. Resour. Health 7, 72 (2009).
Zahradnik, M., Stewart, S. H., Marshall, G. N., Schell, T. L. & Jaycox, L. H. Anxiety sensitivity and aspects of alexithymia are independently and uniquely associated with posttraumatic distress. J. Trauma Stress 22, 131–138 (2009).
Zakiei, A. et al. Mediator role of experiential avoidance in relationship of perceived stress and alexithymia with mental health. East. Mediterr. Health J. 23, 335–341 (2017).
Martin, J. B. & Pihl, R. O. The stress-alexithymia hypothesis: Theorectical and empirical considerations. Psychother. Psychosom. 43, 169–176 (1985).
Frewen, P. A. et al. Clinical and neural correlates of alexithymia in posttraumatic stress disorder. J. Abnorm. Psychol. 117, 171–181 (2008).
Marchesi, C., Fontò, S., Balista, C., Cimmino, C. & Maggini, C. Relationship between alexithymia and panic disorder: A longitudinal study to answer an open question. Psychother. Psychosom. 74, 56–60 (2005).
Tolmunen, T., Lehto, S. M., Heliste, M., Kurl, S. & Kauhanen, J. Alexithymia is associated with increased cardiovascular mortality in middle-aged Finnish men. Psychosom. Med. 72, 187–191 (2010).
Park, J. et al. The association between alexithymia and posttraumatic stress symptoms following multiple exposures to traumatic events in North Korean refugees. J. Psychosom. Res. 78, 77–81 (2015).
Ledermann, K. et al. Myocardial infarction-induced acute stress and post-traumatic stress symptoms: The moderating role of an alexithymia trait—Difficulties identifying feelings. Eur. J. Psychotraumatol. 11, 1804119. https://doi.org/10.1080/20008198.2020.1804119 (2020).
Hawes, M. T., Szenczy, A. K., Klein, D. N., Hajcak, G. & Nelson, B. D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 52, 1–9 (2021).
Wong, L. P., Hung, C.-C., Alias, H. & Lee, T.S.-H. Anxiety symptoms and preventive measures during the COVID-19 outbreak in Taiwan. BMC Psychiatry 20, 376. https://doi.org/10.1186/s12888-020-02786-8 (2020).
Deng, J. et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann. N. Y. Acad. Sci. 1486, 90–111 (2021).
Nasiry, S. et al. Psychometric properties of COVID-19 dot-probe task in Iranian adults. Pract. Clin. Psychol. 9, 179–188 (2021).
Somma, F. et al. Further to the left: Stress-induced increase of spatial pseudoneglect during the COVID-19 lockdown. Front. Psychol. 12, 573846. https://doi.org/10.3389/fpsyg.2021.573846 (2021).
Bar-Haim, Y., Lamy, D., Pergamin, L., Bakermans-Kranenburg, M. J. & van Ijzendoorn, M. H. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychol. Bull. 133, 1–24 (2007).
Veerapa, E. et al. Attentional bias towards negative stimuli in healthy individuals and the effects of trait anxiety. Sci. Rep. 10, 11826. https://doi.org/10.1038/s41598-020-68490-5 (2020).
Zhang, D., Liu, Y., Wang, L., Ai, H. & Luo, Y. Mechanisms for attentional modulation by threatening emotions of fear, anger, and disgust. Cogn. Affect. Behav. Neurosci. 17, 198–210 (2017).
Sorokowski, P. et al. Can information about pandemics increase negative attitudes toward foreign groups? A case of COVID-19 outbreak. Sustain. Sci. Pract. Policy 12, 4912. https://doi.org/10.3390/su12124912 (2020).
Chapman, H. A. & Anderson, A. K. Understanding disgust. Ann. N. Y. Acad. Sci. 1251, 62–76 (2012).
Liu, Y., Zhang, D. & Luo, Y. How disgust facilitates avoidance: An ERP study on attention modulation by threats. Soc. Cogn. Affect. Neurosci. 10, 598–604 (2015).
Wheaton, M. G. et al. Danger and disease: Electrocortical responses to threat- and disgust-eliciting images. Int. J. Psychophysiol. 90, 235–239 (2013).
Krusemark, E. A. & Li, W. Do all threats work the same way? Divergent effects of fear and disgust on sensory perception and attention. J. Neurosci. 31, 3429–3434 (2011).
Zimmer, U., Keppel, M.-T., Poglitsch, C. & Ischebeck, A. ERP evidence for spatial attention being directed away from disgusting locations. Psychophysiology 52, 1317–1327 (2015).
Leonidou, C., Constantinou, E., Panteli, M. & Panayiotou, G. Attentional processing of unpleasant stimuli in alexithymia: Early avoidance followed by attention maintenance bias. Cogent Psychol. 9, 2054531. https://doi.org/10.1080/23311908.2022.2054531 (2022).
Cisler, J. M. & Koster, E. H. W. Mechanisms of attentional biases towards threat in anxiety disorders: An integrative review. Clin. Psychol. Rev. 30, 203–216 (2010).
Dudeney, J., Sharpe, L. & Hunt, C. Attentional bias towards threatening stimuli in children with anxiety: A meta-analysis. Clin. Psychol. Rev. 40, 66–75 (2015).
Bradley, B. P., Mogg, K., White, J., Groom, C. & Bono, J. Attentional bias for emotional faces in generalized anxiety disorder. Br. J. Clin. Psychol. 38, 267–278 (1999).
Rinck, M., Reinecke, A., Ellwart, T., Heuer, K. & Becker, E. S. Speeded detection and increased distraction in fear of spiders: Evidence from eye movements. J. Abnorm. Psychol. 114, 235 (2005).
Mogg, K. & Bradley, B. P. A cognitive-motivational analysis of anxiety. Behav. Res. Ther. 36, 809–848 (1998).
Fujiwara, E. Looking at the eyes interferes with facial emotion recognition in alexithymia. J. Abnorm. Psychol. 127, 571–577 (2018).
Bishop, S. J. Neurocognitive mechanisms of anxiety: An integrative account. Trends Cogn. Sci. 11, 307–316 (2007).
Delle-Vigne, D., Kornreich, C., Verbanck, P. & Campanella, S. Subclinical alexithymia modulates early audio-visual perceptive and attentional event-related potentials. Front. Hum. Neurosci. 8, 106. https://doi.org/10.3389/fnhum.2014.00106 (2014).
Hsing, C. K., HofelichMohr, A. J., Brent Stansfield, R. & Preston, S. D. Alexithymia slows performance but preserves spontaneous semantic decoding of negative expressions in the emostroop task. Int. J. Psychol. Res. 6, 56–67 (2013).
Mogg, K., Bradley, B., Miles, F. & Dixon, R. BRIEF REPORT Time course of attentional bias for threat scenes: Testing the vigilance-avoidance hypothesis. Cogn. Emot. 18, 689–700 (2004).
Bokeriia, L. A., Golukhova, E. Z., Polunina, A. G., Davydov, D. M. & Kruglova, M. V. Alexithymia, depression and heart rate in candidates for cardiac surgery. Int. J. Cardiol. 126, 448–449 (2008).
Starita, F., Làdavas, E. & di Pellegrino, G. Reduced anticipation of negative emotional events in alexithymia. Sci. Rep. 6, 27664. https://doi.org/10.1038/srep27664 (2016).
Donges, U. S., Kersting, A. & Suslow, T. Alexithymia and perception of emotional information: A review of experimental psychological findings. Univ. Psychol. 13, 745–756 (2014).
Brandt, L., Pintzinger, N. M. & Tran, U. S. Abnormalities in automatic processing of illness-related stimuli in self-rated alexithymia. PLoS ONE 10, e0129905. https://doi.org/10.1371/journal.pone.0129905 (2015).
Wiebe, A., Kersting, A. & Suslow, T. Deployment of attention to emotional pictures varies as a function of externally-oriented thinking: An eye tracking investigation. J. Behav. Ther. Exp. Psychiatry 55, 1–5 (2017).
La Rosa, V. L., Gori, A., Faraci, P., Vicario, C. M. & Craparo, G. Traumatic distress, alexithymia, dissociation, and risk of addiction during the first wave of COVID-19 in Italy: Results from a cross-sectional online survey on a non-clinical adult sample. Int. J. Ment. Health Addict. 20, 3128–3144 (2022).
Merlo, E. et al. Uncertainty, alexithymia, suppression and vulnerability during the COVID-19 pandemic in Italy. Health Psychol. Rep. 9, 169–179 (2021).
Osimo, S. A., Aiello, M., Gentili, C., Ionta, S. & Cecchetto, C. The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Front. Psychol. 12, 630751. https://doi.org/10.3389/fpsyg.2021.630751 (2021).
Warchoł-Biedermann, K. et al. Dysfunctional coping mediates the relationship between stress and mental health in health-care staff working amid the COVID-19 pandemic. Med. Princ. Pract. 30, 395–400 (2021).
Shu, M. L., Liao, X. Y. & Qin, L. L. Study on the mental health and its influencing factors of college students in Changsha city in the “post-epidemic era”. Chin. J. Health Psychol. CN 11–5257/R. ISSN 2096–4811. https://kns.cnki.net/kcms/detail/11.5257.R.20210524.1555.017.html (2021).
Yang, X., Xu, Y., Tan, R. & Zhou, X. Event centrality and post-traumatic stress symptoms among college students during the COVID-19 pandemic: The roles of attention to negative information, catastrophizing, and rumination. Eur. J. Psychotraumatol. 13, 2078563. https://doi.org/10.1080/20008198.2022.2078563 (2022).
Bagby, R. M., Michael Bagby, R., Parker, J. D. A. & Taylor, G. J. Twenty-five years with the 20-item Toronto Alexithymia scale. J. Psychosom. Res. 131, 109940. https://doi.org/10.1016/j.jpsychores.2020.109940 (2020).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x (2001).
Manea, L., Gilbody, S. & McMillan, D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): A meta-analysis. CMAJ 184, E191–E196. https://doi.org/10.1503/cmaj.110829 (2012).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166, 1092. https://doi.org/10.1001/archinte.166.10.1092 (2006).
Lin, Y. C. & Chan, C. H. A factor analysis of the Taiwan version of the Toronto Alexithymia Scale-20. Taiwan. J. Psychiatry 17, 276–282 (2003).
Wang, K. C. & Chung, F. C. An Investigation of multidimensional factorial validity of the Chinese version of state-trait anxiety inventory. Psychol. Test. 63, 287–313 (2016).
Hart, S. J., Green, S. R., Casp, M. & Belger, A. Emotional priming effects during Stroop task performance. Neuroimage 49, 2662–2670 (2010).
Raschle, N. M. et al. Investigating the neural correlates of emotion–cognition interaction using an affective stroop task. Front. Psychol. 8, 1489. https://doi.org/10.3389/fpsyg.2017.01489 (2017).
Biss, R. K. & Hasher, L. Delighted and distracted: Positive affect increases priming for irrelevant information. Emotion 11, 1474–1478 (2011).
García-Blanco, A., Salmerón, L., Perea, M. & Livianos, L. Attentional biases toward emotional images in the different episodes of bipolar disorder: An eye-tracking study. Psychiatry Res. 215, 628–633 (2014).
Vogt, J., Koster, E. H. W. & De Houwer, J. Safety first: Instrumentality for reaching safety determines attention allocation under threat. Emotion 17, 528–537 (2017).
Zhang, L. et al. Effects of SSRI antidepressants on attentional bias toward emotional scenes in first-episode depressive patients: Evidence from an eye-tracking study. Psychiatry Investig. 17, 871–879 (2020).
Dresler, T. et al. Neural correlates of the emotional Stroop task in panic disorder patients: An event-related fMRI study. J. Psychiatr. Res. 46, 1627–1634 (2012).
Olsavsky, A. K. et al. Amygdala hyperactivation during face emotion processing in unaffected youth at risk for bipolar disorder. J. Am. Acad. Child Adolesc. Psychiatry 51, 294–303 (2012).
Schmidt, S. R. & Saari, B. The emotional memory effect: Differential processing or item distinctiveness?. Mem. Cognit. 35, 1905–1916 (2007).
Coffey, E., Berenbaum, H. & Kerns, J. Brief report. Cogn. Emot. 17, 671–679 (2003).
Mueller, J., Alpers, G. W. & Reim, N. Dissociation of rated emotional valence and Stroop interference in observer-rated alexithymia. J. Psychosom. Res. 61, 261–269 (2006).
Richard-Devantoy, S., Ding, Y., Turecki, G. & Jollant, F. Attentional bias toward suicide-relevant information in suicide attempters: A cross-sectional study and a meta-analysis. J. Affect. Disord. 196, 101–108 (2016).
Lang, P. J., Bradley, M. M. & Cuthbert, B. N. International Affective Picture System (IAPS): Affective Ratings of Pictures and Instruction Manual, Technical Report A-8. (University of Florida, 2008).
Pexels. http://www.pexels.com Accessed May, 2020.
Pixabay. https://pixabay.com/ Accessed May, 2020.
PhotoAC. https://zh-tw.photo-ac.com/ Accessed May, 2020.
Rawpixel. https://www.rawpixel.com/ Accessed May, 2020.
Unsplash. https://unsplash.com/ Accessed May, 2020.
Sass, K. et al. The influence of emotional associations on the neural correlates of semantic priming. Hum. Brain Mapp. 33, 676–694 (2012).
Hayes, A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach (Guilford Publications, 2013).
Celikbas, Z. et al. How are experiential avoidance and cognitive fusion associated with alexithymia?. J. Ration. Emot. Cogn. Behav. Ther. 39, 86–100 (2021).
Panayiotou, G. et al. Do alexithymic individuals avoid their feelings? Experiential avoidance mediates the association between alexithymia, psychosomatic, and depressive symptoms in a community and a clinical sample. Compr. Psychiatry 56, 206–216 (2015).
Venta, A., Sharp, C. & Hart, J. The relation between anxiety disorder and experiential avoidance in inpatient adolescents. Psychol. Assess. 24, 240–248 (2012).
Hayes, S. C. et al. Measuring experiential avoidance: A preliminary test of a working model. Psychol. Rec. 54, 553–578 (2004).
Kashdan, T. B., Barrios, V., Forsyth, J. P. & Steger, M. F. Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behav. Res. Ther. 44, 1301–1320 (2006).
Karekla, M., Forsyth, J. P. & Kelly, M. M. Emotional avoidance and panicogenic responding to a biological challenge procedure. Behav. Ther. 35, 725–746 (2004).
Carvalho, S., Dinis, A., Pinto-Gouveia, J. & Estanqueiro, C. Memories of shame experiences with others and depression symptoms: The mediating role of experiential avoidance. Clin. Psychol. Psychother. 22, 32–44 (2015).
Greene, D., Hasking, P. & Boyes, M. The associations between alexithymia, non-suicidal self-injury, and risky drinking: The moderating roles of experiential avoidance and biological sex. Stress Health 35, 457–467 (2019).
Leonidou, C., Panayiotou, G., Bati, A. & Karekla, M. Coping with psychosomatic symptoms: The buffering role of psychological flexibility and impact on quality of life. J. Health Psychol. 24, 175–187 (2019).
Gross, J. J. Emotion regulation: Current status and future prospects. Psychol Inq. 26, 1–26 (2015).
Preece, D., Becerra, R., Allan, A., Robinson, K. & Dandy, J. Establishing the theoretical components of alexithymia via factor analysis: Introduction and validation of the attention-appraisal model of alexithymia. Pers. Individ. Differ. 119, 341–352 (2017).
Panayiotou, G., Leonidou, C., Constantinou, E. & Michaelides, M. P. Self-awareness in alexithymia and associations with social anxiety. Curr. Psychol. 39, 1600–1609 (2020).
Sheppes, G. & Levin, Z. Emotion regulation choice: Selecting between cognitive regulation strategies to control emotion. Front. Hum. Neurosci. 7, 179. https://doi.org/10.3389/fnhum.2013.00179 (2013).
Davydov, D. M. Alexithymia as a health risk and resilience factor. J. Psychosom. Res. 101, 66–67 (2017).
Panayiotou, G., Panteli, M. & Vlemincx, E. Adaptive and maladaptive emotion processing and regulation, and the case of alexithymia. Cogn. Emot. 35, 488–499 (2021).
Stabbe, O. K., Rolffs, J. L. & Rogge, R. D. Flexibly and/or inflexibly embracing life: Identifying fundamental approaches to life with latent profile analyses on the dimensions of the Hexaflex model. J. Context. Behav. Sci. 12, 106–118 (2019).
Tavakoli, N., Broyles, A., Reid, E. K., RobertSandoval, J. & Correa-Fernández, V. Psychological inflexibility as it relates to stress, worry, generalized anxiety, and somatization in an ethnically diverse sample of college students. J. Context. Behav. Sci. 11, 1–5 (2019).
UC Davis Health. Omicron Variant: What We Know so Far About This COVID-19 Strain. https://health.ucdavis.edu/coronavirus/covid-19-information/omicron-variant (2022).
MacDonald, H. Z. & Olsen, A. The role of attentional control in the relationship between mindfulness and anxiety. Psychol. Rep. 123, 759–780 (2020).
Moore, A., Gruber, T., Derose, J. & Malinowski, P. Regular, brief mindfulness meditation practice improves electrophysiological markers of attentional control. Front. Hum. Neurosci. 6, 18 (2012).
Basanovic, J., Notebaert, L., Grafton, B., Hirsch, C. R. & Clarke, P. J. Attentional control predicts change in bias in response to attentional bias modification. Behav. Res. Ther. 99, 47–56 (2017).
Peters, A., McEwen, B. S. & Friston, K. Uncertainty and stress: Why it causes diseases and how it is mastered by the brain. Prog. Neurobiol. 156, 164–188 (2017).
Ye, Y., Yang, X. & Zhou, X. Attention to negative information and PTSSs during the COVID-19: A moderated mediational model. Curr. Psychol. https://doi.org/10.1007/s12144-022-02877-7 (2022).
Galderisi, S. et al. Alexithymia and cognitive dysfunctions in patients with panic disorder. Psychother. Psychosom. 77, 182–188 (2008).
Van Bockstaele, B. et al. A review of current evidence for the causal impact of attentional bias on fear and anxiety. Psychol. Bull. 140, 682 (2014).
Boiko, D. I. et al. Circadian rhythm disorder and anxiety as mental health complications in post-COVID-19. Environ. Sci. Pollut. Res. 29, 28062–28069 (2022).
Kubota, T., Kuroda, N. & Sone, D. Neuropsychiatric aspects of long COVID: A comprehensive review. Psychiatry Clin. Neurosci. 77, 84–93. https://doi.org/10.1111/pcn.13508 (2023).
Acknowledgements
This research was supported by grants from the Ministry of Science and Technology, Taiwan (MOST 110-2410-H-007-041). For assistance with various aspects of this study, we thank Nai-Wei, Kuo, Yu-Ching, Chen, Wei-Chun, Wang for collecting the data.
Author information
Authors and Affiliations
Contributions
Author contributions included conception and study design (S.H.L.), data collection (S.H.L. and K.T.L.), statistical analysis (K.T.L.), interpretation of results (S.H.L. and K.T.L.), drafting the manuscript work or revising it critically for important intellectual content (S.H.L.) and approval of final version to be published and agreement to be accountable for the integrity and accuracy of all aspects of the work (S.H.L. and K.T.L.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, SH., Lee, KT. The impact of pandemic-related stress on attentional bias and anxiety in alexithymia during the COVID-19 pandemic. Sci Rep 13, 6327 (2023). https://doi.org/10.1038/s41598-023-33326-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-023-33326-5
This article is cited by
-
The relationship of anxiety, benefit finding and academic engagement among Chinese college students in different stages of COVID-19: a repeated cross-sectional pilot study
Current Psychology (2025)
-
Investigating alexithymia, empathy, and resilience in medical students during pandemic era: a cross-sectional study in northern Iran
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2024)
-
A study on the influencing factors of mental health of Chinese garden workers: a cross-sectional study
BMC Public Health (2024)