Abstract
Psoriasis, characterized as a chronic relapsing disease with a protracted course, often drives patients to seek relief through Chinese folk remedies (CFR). Nonetheless, the complex compositions of these remedies frequently result in unintended adverse effects, notably various types of heavy metal poisoning. Our study involved an exhaustive collection and analysis of clinical data from psoriasis patients who developed heavy metal poisoning due to CFR usage, admitted to Beijing Chao-Yang Hospital from January 2011 to October 2023. Our analysis identified 44 cases of mercury poisoning, 17 of lead poisoning, 21 of arsenic poisoning, and 4 instances of mixed heavy metal poisoning. The folk remedies used ranged from fumigation and inhalation to skin application and oral administration. Distinct pathogenic characteristics were observed in each poisoning type. After treatment with metal chelating agents, all patients experienced a reduction in heavy metal levels in their bodies, accompanied by varying degrees of symptom alleviation. This study underscores the vital necessity of opting for formal, medically approved treatments for psoriasis, thereby avoiding the hazardous consequences of unregulated folk remedies that may lead to severe heavy metal poisoning.
Similar content being viewed by others
Introduction
Psoriasis, a prevalent chronic inflammatory skin disease, is known for its recurring nature. Characterized by distinctive red, scaly patches on the skin, it not only affects patients’ physical appearance but also imposes a substantial psychological burden1. Globally, the quest for an ideal and effective treatment for psoriasis remains ongoing2. Although there are reports that Chinese herbal formulas, single herbs, and their active components have shown promising prospects in the clinical treatment of psoriasis3,4,5, due to the chronic and often intractable nature of the disease, many patients have not used formal traditional Chinese medicine treatments but instead resorted to Chinese folk remedies (CFR). However, these remedies often contain a complex mix of ingredients with dangerously high levels of heavy metals. Prolonged use can lead to the accumulation of these metals in the body, resulting in severe heavy metal poisoning. A lack of awareness and understanding of heavy metal poisoning among medical professionals can unfortunately lead to misdiagnosis or overlooked diagnosis of this condition. The aim of this article is to conduct a detailed review and analysis of clinical data pertaining to psoriasis patients who experienced heavy metal poisoning.
Methods
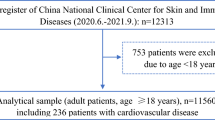
A retrospective study of the psoriasis patients with heavy metal poisoning caused by CFR usage was conducted to provide an exhaustive report on the findings, thereby offering a comprehensive overview of the associated clinical outcomes. These patients were admitted to Beijing Chao-Yang Hospital and diagnosed and treated in accordance with Chinese occupational health standards (GBZ) during the period from January 2011 to October 2023. Patients with occupational exposure to heavy metals or lifestyle exposures other than the use of CFR were excluded. The levels of heavy metals in blood and urinary were tested for all patients. The levels of mercury and arsenic were detected using a fluorescence photometer (atomic fluorescence method), while the lead levels were detected using an atomic absorption spectrophotometer (atomic absorption method). The Research Ethics Board of Beijing Chao-Yang Hospital approved the study and waived the requirement for informed consent (LGH-2022-NO-62). All methods were performed in accordance with the ethical guidelines for human participants.
Results
Study population and CFR usage
Our study encompassed a total of 86 psoriasis patients suffering from heavy metal poisoning, comprising 51 males and 35 females, ranging in age from 17 to 68 years. The breakdown of cases included 44 cases of mercury poisoning, 17 of lead poisoning, 21 of arsenic poisoning, and 4 of mixed heavy metal poisoning (2 of mercury poisoning combined with lead poisoning and 2 of mercury poisoning combined with arsenic poisoning). The methods of using CFR included fumigation and inhalation (FI), skin application (SA), and oral administration (OA), as shown in Table 1. Four patients subjected their used folk remedies to heavy metal testing, revealing the following concentrations: mercury at 17.52 mg/g, mercury at 42.37 mg/g, lead at 9.81 mg/g, and a combination of mercury at 39.24 mg/g and arsenic at 22.47 mg/g.
Clinical symptoms and signs
As shown in Table 2, patients suffering from all three types of heavy metal poisoning—mercury, lead, and arsenic—presented a spectrum of clinical manifestations. These included symptoms of neurasthenia, gastrointestinal disturbances, and peripheral neuropathy. Notably, individuals with mercury poisoning frequently exhibited urinary alterations and edema. Those affected by lead poisoning predominantly experienced severe anemia and abdominal pain. Moreover, arsenic poisoning was markedly characterized by extensive dermatological damage.
Auxiliary examinations
For mercury poisoning, the average blood mercury level was 0.047 mg/L (0.006–0.237 mg/L), well above the normal value of < 0.015 mg/L. Similarly, the average urinary mercury level was significantly elevated at 32.622 μmol/mol Cr (9.994–302.814 μmol/mol Cr), far exceeding the normal value of < 2.250 μmol/mol Cr. In cases of lead poisoning, the average blood lead level was observed at 521 μg/L (281–2031 μg/L), surpassing the normal upper limit of < 400 μg/L. The urinary lead levels also showed an increase, averaging at 4.891 mg/L (0.199–13.050 mg/L), which is considerably higher than the normal value of < 0.070 mg/L. For arsenic poisoning, the average blood arsenic level was found to be 72.6 μg/L (5.6–119.8 μg/L), within a broad normal range of 2.5–190.0 μg/L. The average urinary arsenic was also elevated at 1.288 mg/L (0.159–4.767 mg/L), exceeding the normal value of < 0.100 mg/L.
In 7 cases of mercury poisoning, there was a significant increase in liver enzymes. Alanine Aminotransferase (ALT) levels varied between 57 and 335 U/L, substantially higher than the normal range of 9–50 U/L. Aspartate Aminotransferase (AST) levels also showed a rise, ranging from 42 to 273 U/L, which is above the normal value of 15–40 U/L. Additionally, 2 cases exhibited elevated serum creatinine levels, measuring 115.4 mmol/L and 176.1 mmol/L, respectively. Among 5 cases of lead poisoning, ALT levels ranged from 53 to 406 U/L, and AST levels were found to be between 42 and 299 U/L. In 3 cases of arsenic poisoning, ALT varied from 48 to 133 U/L, and AST ranged from 42 to 126 U/L.
Electromyography in 3 cases of mercury poisoning, 4 cases of lead poisoning, and 1 case of arsenic poisoning showed evidence of conduction nerve damage. Additional findings included proteinuria in 17 cases of mercury poisoning, with 9 cases progressing to nephrotic syndrome characterized by significant proteinuria (3462–5085 mg/days), marked hypoalbuminemia (11.2–26.6 g/L), and hyperlipidemia. Kidney biopsy in 6 cases indicated membranous nephropathy. In lead poisoning, 14 cases showed reduced hemoglobin levels (70–111 g/L), and blood cell analysis in 6 cases revealed basophilic stippling of red cells. Skin pathology in 2 cases of arsenic poisoning was consistent with basal cell carcinoma of the skin.
Treatment and prognosis
For patients with mercury or arsenic poisoning, sodium 2,3-dimercapto-1-propanesulfonate (DMPS) was used for chelation therapy, administered as a 250 mg intramuscular injection once daily. For lead poisoning, calcium disodium edetate (EDTA) chelation therapy was employed, with a 1 g intravenous drip once daily. The chelation therapy regimen involved administering the medication for 3 days, followed by a 4-day break, constituting one treatment course. For patients with both mercury and lead poisoning, both DMPS and calcium disodium EDTA were administered simultaneously. 24-h urinary heavy metal levels were monitored every day during the medication in each course. After several treatment courses, a significant reduction in the patients' body heavy metal content was observed, as shown in Table 3. Except for the dermatological damage in arsenic poisoning patients, which showed no significant improvement, all other symptoms and signs improved or even disappeared.
Discussion
Patients with psoriasis, owing to the persistent characteristics of their ailment, frequently turn to CFR that contain significant levels of heavy metals like mercury, lead, and arsenic6,7,8. The concentration of these heavy metals in Traditional Chinese Medicine is regulated by specific ISO standards (ISO 18664-2015, GB 2762-2017). However, in the cases of four patients highlighted in this article, the levels of heavy metals in their remedies were found to surpass these established standard limits. The application methods for folk remedies primarily included oral administration, followed by fumigation and inhalation and skin application, with some patients even using multiple methods simultaneously. Although the symptoms of psoriasis lesions showed slight improvement in the short term after using these remedies, the underlying mechanism remains unclear. However, long-term use of these remedies can lead to the accumulation of heavy metals in the body, subsequently manifesting symptoms of heavy metal poisoning9.
Heavy metals and their compounds distribute throughout various organs and tissues of the body, where they exhibit a pronounced affinity for sulfhydryl groups. This leads to changes in the activity of sulfhydryl-based enzymes and sulfhydryl-containing receptors, resulting in damage to target organs. These damages present as specific clinical symptoms and signs of poisoning. Different heavy metals exhibit distinct clinical manifestations, and there is individual variability in patients’ toxic responses to these substances. The clinical characteristics of patients with mixed poisoning are a combination of symptoms from multiple heavy metal toxicities.
The significant neurasthenic syndrome symptoms resulting from lead, mercury, and arsenic poisoning are noteworthy. Patients commonly display symptoms like dizziness, headache, insomnia, fatigue, and memory decline, accompanied by anxiety and restlessness10. Gastrointestinal symptoms primarily include nausea, vomiting, a peculiar taste in the mouth, mucosal erosion, and ulceration. Additional symptoms may encompass abdominal pain, diarrhea, and abnormal liver function11. Neurological damage due to these toxic substances often presents as tremors, sensory abnormalities in the limbs, and movement disorders. In more severe cases, patients may suffer from toxic encephalopathy12.
Notably, severe mercury poisoning significantly impacts kidney function, ranging from proteinuria in milder cases to nephrotic syndrome and elevated serum creatinine levels in severe instances13. Among 44 patients with mercury poisoning, 9 showed pronounced lower limb edema and significant proteinuria, suggesting typical nephrotic syndrome14. Pathological examinations in these cases revealed membranous nephropathy15. Most patients with lead poisoning experience varying degrees of anemia and abdominal pain. These symptoms are often misdiagnosed as acute gastroenteritis, intestinal obstruction, or appendicitis16. In some cases, patients undergo exploratory laparotomy to determine the cause of their symptoms, leading to considerable physical harm and financial burden for both the patients and their families. Chronic arsenic accumulation in the skin leads to distinct skin pigmentation and hyperkeratosis in affected individuals17. In severe cases of arsenic poisoning, skin ulcers and even in-situ skin cancer can develop18.
The cases discussed in this article demonstrated that all patients showed significant reductions in urinary heavy metal levels and marked clinical improvement after several courses of treatment19. However, as lead tends to accumulate more in deeper tissues such as muscles and bones, a longer course of treatment is often required to reduce urinary lead levels to normal. Additionally, it was observed that even after normalizing urinary arsenic levels, the skin pigmentation and hyperkeratosis in patients with arsenic poisoning did not show significant improvement. The skin damage caused by arsenic poisoning, similar to psoriasis, requires long-term and regular treatment in dermatology for improvement.
Based on the discussion, it is recommended that psoriasis patients who have been using CFR for extended periods should undergo comprehensive heavy metal testing. This approach is crucial to avoid missing a diagnosis of heavy metal poisoning, which could delay appropriate treatment. Early detection of heavy metal poisoning allows for the immediate cessation of exposure to the toxic source and the initiation of chelation therapy, which generally leads to a favorable prognosis. The issue of heavy metal poisoning caused by CFR warrants societal attention. Patients with psoriasis should be warned against impulsive and indiscriminate medical treatments to avoid the physical harm associated with heavy metal poisoning.
Some limitations of the present study should be mentioned. First, the study is retrospective, and heavy metals poisoning caused by CFR usage may involve a wider variety of toxins and more toxic features that have not been identified. In addition, due to the limited number of cases of various types of heavy metal poisoning, more data is needed for better scientific research.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Griffiths, C. E. M., Armstrong, A. W., Gudjonsson, J. E. & Barker, J. N. W. N. Psoriasis. Lancet 397, 1301–1315 (2021).
Rendon, A. & Schäkel, K. Psoriasis pathogenesis and treatment. Int. J. Mol. Sci. 20, 1475 (2019).
Luo, Y. et al. Chinese herbal medicine for psoriasis: Evidence from 11 high-quality randomized controlled trials. Front. Pharmacol. 11, 599433 (2021).
Li, T. et al. Potential effects and mechanisms of Chinese herbal medicine in the treatment of psoriasis. J. Ethnopharmacol. 294, 115275 (2022).
Yang, X. Y., Cai, W. L., Guo, C. L. & Chen, Q. H. Chinese medicine as supporting therapy for psoriasis: Past, present, and future. Chin. J. Integr. Med. 29, 280–288 (2023).
Mo, T. et al. Mercury poisoning caused by Chinese folk prescription (CFP): A case report and analysis of both CFP and quackery. Med. Baltim. 95, e5162 (2016).
Tang, G., Tu, X. & Feng, P. Lead poisoning caused by traditional Chinese medicine: A Case report and literature review. Tohoku J. Exp. Med. 243, 127–131 (2017).
Zheng, J., Zhang, K., Liu, Y. & Wang, Y. Fatal acute arsenic poisoning by external use of realgar: Case report and 30 years literature retrospective study in China. Forens. Sci. Int. 300, e24–e30 (2019).
Wu, M. L., Deng, J. F., Lin, K. P. & Tsai, W. J. Lead, mercury, and arsenic poisoning due to topical use of traditional Chinese medicines. Am. J. Med. 126, 451–454 (2013).
Qin, A. B., Liu, L., Gao, B. X. & Su, T. A case of chronic mercury poisoning associated nephrotic syndrome, abdominal pain, and neuropsychiatric symptoms. Ren. Fail. 45, 2261553 (2023).
Ibrahim, D., Froberg, B., Wolf, A. & Rusyniak, D. E. Heavy metal poisoning: Clinical presentations and pathophysiology. Clin. Lab. Med. 26, 67–97 (2006).
Krieg, E. F. Jr., Chrislip, D. W. & Brightwell, W. S. A meta-analysis of studies investigating the effects of lead exposure on nerve conduction. Arch. Toxicol. 82, 531–542 (2008).
Orr, S. E. & Bridges, C. C. Chronic kidney disease and exposure to nephrotoxic metals. Int. J. Mol. Sci. 18, 1039 (2017).
Gao, Z. et al. Toxic nephropathy secondary to chronic mercury poisoning: Clinical characteristics and outcomes. Kidney Int. Rep. 7, 1189–1197 (2022).
Doshi, M., Annigeri, R. A., Kowdle, P. C., Subba Rao, B. & Varman, M. Membranous nephropathy due to chronic mercury poisoning from traditional Indian medicines: Report of five cases. Clin. Kidney J. 12, 239–244 (2018).
Tsai, M. T., Huang, S. Y. & Cheng, S. Y. Lead poisoning can be easily misdiagnosed as acute porphyria and nonspecific abdominal pain. Case Rep. Emerg. Med. 2017, 9050713 (2017).
Pathania, Y. S. Mottled pigmentation, palmar keratosis and chronic arsenic poisoning. QJM 114, 265–266 (2021).
Hunt, K. M., Srivastava, R. K., Elmets, C. A. & Athar, M. The mechanistic basis of arsenicosis: Pathogenesis of skin cancer. Cancer Lett. 354, 211–219 (2014).
Bjørklund, G., Mutter, J. & Aaseth, J. Metal chelators and neurotoxicity: Lead, mercury, and arsenic. Arch. Toxicol. 91, 3787–3797 (2017).
Author information
Authors and Affiliations
Contributions
C.X., X.D., X.Z. and N.W. collected the clinical data. C.X. analyzed the data and drafted the manuscript. Q.Y. revised the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xue, C., Du, X., Zhu, X. et al. Heavy metal poisoning caused by Chinese folk remedies in psoriasis patients: a retrospective analysis. Sci Rep 14, 11777 (2024). https://doi.org/10.1038/s41598-024-62653-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-62653-4