Abstract
COVID-19 can increase the long-term risk of multiorgan dysfunction. Few studies investigated the long-term risk in Asian populations or investigated the association between viral load and long-term risk. We aimed to investigate the post-discharge rates of hospitalization and association with baseline viral load in all patients with COVID-19 in Hong Kong. This was a population-based cohort study included all patients with a positive RT-PCR test for SARS-CoV-2 in Hong Kong between January 1st 2020 and August 30th 2020, routinely admitted to public health care facilities for isolation and treatment. Viral Ct values were available in 3433 (85%) of patients. Outcomes of interest included death, cause-specific hospitalizations, and initiation of medication from the Hospital Authority's territory-wide electronic health records from the Clinical Data Analysis and Reporting System. In total, 4054 people in Hong Kong tested positive for COVID-19 and were admitted to a public health care facility, of whom 167 (4.1%) were admitted to ICU. During a median follow-up time of 251 (interquartile range 240–279) days, 408 (11.9%) were hospitalized for any reason and 16 (0.5%) patients died. After discharge, patients were most often readmitted for respiratory reasons, followed by gastro-intestinal reasons. A higher viral load (lower RT-PCR Ct values) was associated with a higher likelihood of death (Hazard ratio [HR] 5.86, 95% Confidence interval [CI] 2.57–13.33), hospitalization (HR 1.22, 95%CI 1.08–1.39) or hospitalization for cardiovascular disease (HR 12.78, 95%CI 3.67–44.48). Patients with higher viral loads more likely started ACE-inhibitors (HR 1.37, 95%CI 1.12–1.68) and non-opioid analgesics (HR 1.01, 95%CI 1.01–1.23). In a relatively mild COVID-19 population from Hong Kong, the post-acute risk of complications was substantial. Our results highlight that higher viral load predict post-acute complications in patients with relatively mild disease.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for causing coronavirus disease 2019 (COVID-19), has directly or indirectly affected the global population and caused a total of 2.9 million deaths to date. In the early stages of the pandemic, research and health services have predominantly focused on the immediate direct (through infection) and indirect (changes in behaviours and effect on health systems) effects of the virus1.
While COVID-19 predominantly manifests as respiratory disease, there is increasing evidence of other organ involvement, including the heart2. A prospective cohort study of 201 young low-risk individuals showed that almost 70% of participants had ongoing impairment of multiple organ systems3. In Wuhan, a sample of 1733 patients were followed up after discharge and reported mainly muscle fatigue and lethargy4.
Viral load measurements from nasopharyngeal swabs indicate active viral replication5,6. Previous studies indicated that higher SARS-CoV-2 viral loads at presentation were independently associated with in-hospital mortality, or intubation5,6,7,8,9. Furthermore, a higher viral load is associated with an increased risk of post-COVID-19 syndrome10. A previous systematic review found that respiratory virus real-time polymerase chain reaction cycle threshold (ct) values are associated with disease severity and outcomes11. However, few studies investigated the association between SARS-CoV-2 viral loads at presentation and long-term outcomes or hospitalization in mild populations. Therefore, we studied the association of SARS-CoV-2 viral load with long-term outcomes in patients with COVID-19 in Hong Kong.
Methods
Data source
COVID-19 patients were identified using the Clinical Data Analysis and Reporting System (CDARS). CDARS is an electronic healthcare database developed by the Hospital Authority. The Hospital Authority is a statutory body that manages all public hospitals and public clinics in Hong Kong, covering over 80% of Hong Kong’s population. In Hong Kong, all people testing positive for COVID-19 are admitted to hospital for isolation. Therefore, the included study population in CDARS represent all patients with proven COVID-19, regardless of disease severity. Electronic patient records include demographics, diagnoses date and disease coding, hospital admission and discharge dates, drug prescriptions and dispensing records, laboratory test results, and date of registered death for research and audit purposes. All patients were anonymised in this system, thus sensitive information such as name and ID were not accessible. The coding accuracy of CDARS has been well-validated and published previously12,13,14,15,16,17.
The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (reference number: UW 21-436) and the need for informed consent was waived by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. This study was conducted under the principles of the Declaration of Helsinki.
Study design and patients selection
This is a population-based retrospective cohort study. COVID patients were identified based on a positive SARS-CoV-2 RT-PCR test or disease classification (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code: 079.89, 480.8, 519.8) between January 1, 2020, and August 31, 2020. Patients who tested positive on ART, but negative on RT-PCR were excluded. Demographic information, date of the first positive lab result, baseline medication, baseline comorbidities, baseline laboratory result, admission date and principal diagnosis during follow up, and other clinical information were extracted from CDARS.
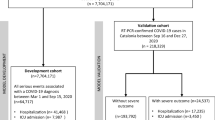
The index date was defined as the first date of positive PCR test. Follow-up started from the date of discharge until the occurrence of outcome, death, or study end (2021-04-13). Patients aged < 18 years at the index date or who died during hospitalisation were excluded.
Outcome
The main outcome of this study were all-cause mortality and all-cause re-hospitalisation after COVID discharge. Secondary outcomes included cause specific hospitalizations and new-onset medication use. Cause specific hospitalizations included hospitalization for respiratory reasons, gastro-intestinal reasons, mental/psychiatric reasons and cardiovascular reasons. Supplementary Table 1 shows details on the ICD codes used for each outcome. New onset medication use included angiotensin receptor blocker (ARB), beta-blockers (BBs), calcium channel blockers (CCBs), statins, anti-depressants, aspirin and non-steroidal anti-inflammatory drugs (NSAIDs). Supplementary Table 2 provides a detailed overview of the coding used to identify medications.
Statistical analysis
Baseline characteristics of all included patients were presented. Mean and standard deviation (SD) were used to present continuous variables, frequencies and percentages were used to present categorical variables. Normality of continuous variables was evaluated by visualizing histograms and inspecting the distribution. The incidence was presented as the rate per 100 person-year with the 95% confidence interval. We modelled the association of baseline viral load (CT values) as continuous variables with the risk of death, total- and cause-specific hospitalizations using restricted cubic splines and Cox regression analyses. We fitted models with 2–5 knots and chose the optimal number of knots for each spline using the Akaike Information Criterion. (AIC). Because we found a non-linear increase in risk with lower CT values for most outcomes, we dichotomized the CT values based on a cut-off point identified from the restricted cubic splines. To account for factors associated with higher viral loads, we weighed the hazards by balancing weights calculated from the propensity scores using the CBPS package18,19. We dichotomized the CT values according to the median and calculated propensity scores using the dichotomized CT values as the dependent variable. Supplementary Table 3 provides a full list of variables used for weighting, including age, sex, medical history, baseline medication and intensive care unit (ICU) stay. Variables for the multivariable models were included based on clinical relevance and data availability. All analyses were performed using R, version 4.0.5 (2021-03-31) and a two-sided P value of < 0.05 was considered statistically significant.
Results
Baseline characteristics
Figure 1 depicts the consort diagram on patient inclusion. A total of 4,602 patients with COVID-19 were identified in CDARS between 1 Jan 2020 to 31 Aug 2020. Patients aged < 18 years (n = 440) and who died before discharge (n = 108) were excluded. Out of the remaining 4054 patients, 3433 (85%) patients had CT values.
Table 1 shows the baseline characteristics of the 4054 patients with COVID-19 discharged alive. The median age was 47 (interquartile range [IQR] 32–60) years and 49.2% (n = 1995) were men. Most patients had a low prevalence of comorbidities. Diabetes was the most common comorbidity, followed by a history of ischemic heart disease. Calcium channel blockers (CCBs) and statins were the most common medication at baseline. 4.1% of patients were admitted to ICU. The median ICU stay was 9 (IQR 5–15) days.
Outcomes and association with viral load
Table 2 shows the event rates of patients discharged alive. During a median follow up of 251 (IQR 240–279) days, 16 patients died, and 408 patients were rehospitalized. The incidence rate of death was 0.47 (95% confidence interval [CI] 0.27–0.764) per 100 patient years (py) and 11.88 (95% CI 10.76–13.1) per 100 py for hospitalization for any reason. The most common reason for rehospitalization was respiratory, followed by gastro-intestinal, mental and cardiovascular reasons.
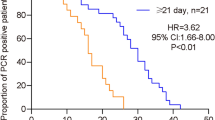
Figure 2 depicts the restricted cubic splines for the association of CT values at presentation with death, total- and cause-specific hospitalization. We found a non-linear association of higher of lower CT values with a higher relative risk of death, total hospitalization and cardiovascular hospitalization (P < 0.001 for all), but not for mental, respiratory and GI hospitalizations. The risk for death, total and CV and respiratory hospitalizations decreased linearly until 20 repeats, after which the relative risk fell to 1.
Table 3 shows results of the association between dichotomized CT values (< 20 repeats versus ≥ 20 repeats) and the different outcomes, weighed for probability weights using propensity scores. We observed that patients with high viral loads (< 20 CT repeats) were at a higher risk for death, total hospitalization, and CV hospitalization than those with lower viral loads (≥ 20 CT repeats). Patients with high viral loads more likely started ACE-inhibitors than patients with lower viral loads (≥ 20 repeats).
Discussion
In our study, we found that post-discharge rehospitalization for patients with COVID-19 in Hong Kong were common. Higher SARS-CoV-2 viral loads at admission were associated with an increased likelihood of post-discharge death or rehospitalization, particularly for myocardial infarction or stroke, independent of initial ICU stay. Early risk stratification for long-term dismal outcomes after COVID-19 infection remains a challenge. Our results suggest that patients with higher viral loads at admission might benefit from close follow-up, early initiation of treatment and a holistic and multidisciplinary long-term care plan.
In Hong Kong, one in ten patients with COVID-19 were rehospitalized during a median follow-up of 251 days. In the United Kingdom, over a third of patients admitted for COVID-19 were readmitted and more than 1 in 10 died after discharge20. Strict lockdown measures and quarantine orders in Hong Kong have kept COVID-19 numbers lower in Hong Kong than most other countries21. Therefore, all COVID-19 patients in Hong Kong who test positive on RT-PCR, are isolated in hospitals or community facilities. The CDARs data represents all patients with COVID-19 in Hong Kong registered with the Hospital Authority, which includes a substantial number of asymptomatic individuals. This explains the lower numbers of post-discharge death and rehospitalization in Hong Kong than the UK. However, in a large study from the Veterans Health Administration among 73,435 uses with COVID-19 who were not hospitalized and survived the first 30 days after diagnosis, the risk of long-term rehospitalization and death was still higher than matched negative-controls, particularly for respiratory signs and symptoms and incident hypertension22.
Various studies indicated that higher SARS-CoV-2 viral loads at presentation was independently associated with in-hospital mortality, or intubation5,6,7,8,9. Respiratory and plasma viral loads of SARS-CoV-2 predicted the risk of in-hospital death, predominantly due to pneumonia5. This was confirmed in a 3,014 patients hospitalized in 3 large New York City hospitals6. All of these previous studies5,6,7,8,9 were performed in countries with a more significant burden of the epidemic and consequently higher admission threshold than Hong Kong and did not include long-term outcome. The current study is unique, due to its large representative sample size, inclusion of long-term outcomes and many asymptomatic patients. To our knowledge, we are the first to report on the association of viral load and long-term outcomes in patients with COVID-19.
We found that higher viral loads (lower CT-values) independently predicted death, total rehospitalization and rehospitalization for stroke or myocardial infarction, independent of ICU stay. In a previous study from the United States22, patients discharged after hospitalization for COVID-19 had an increased risk of CV conditions after discharge22. Similar results were observed in the United Kingdom in patients after discharge for hospitalization with more severe COVID-1920. A recent study in Sweden confirmed the increased risk of incident stroke and myocardial infarction in patients who recovered from COVID-1923. In our study, a higher viral load was associated with an increased risk of hospitalization for myocardial infarction, chest pain, and stroke. We also found that higher viral loads were associated with an increased risk of incident ACEi use. However, these associations were non-linear, such that the risk for death, hospitalization and medication use decreased linearly until 20 repeats, after which the relative risk remained stable at 1. Literature on cut-off values for CT repeats is not conclusive9, but many studies considered a viral load < 25 CT values as high9. Patients with a high viral load commonly also have more severe disease5,6,7,8,9. However, we did not find a significant interaction between viral load and ICU stay for any of the outcomes.
A discussion on the potential mechanisms of the association between higher viral loads and increased myocardial infarction and stroke risk is warranted. COVID-19 infection creates a pro-thrombotic state24. Several previous publications suggested that this prothrombotic phenotype might be mediated by ACE225,26. SARS-CoV2 enters the host cell by binding to ACE2, similar to other Corona viruses25, leading to enhanced shedding of ACE2 and release of soluble protein. Decreased ACE2 activity is potentially thrombogenic through angiotensin-2 activity and plasminogen activator inhibitor-1 expression27. Increased ACE2 plasma levels, potentially reflecting excess shedding, were associated with an increased risk of myocardial infarction and stroke in the PURE study28. Our study suggests that increased viral loads in patients with COVID-19 are associated with an increased risk of myocardial infarction and stroke, potentially mediated through reduced ACE2 activity. The results of our study might have several important clinical implications. First, our results suggest that viral load should not only be used for increased risk stratification but might also be a good indicator for the risk of long-term outcomes. Second, in the post-vaccination era, more patients will have milder disease. Therefore, future studies should investigate whether COVID. While our results indicate the association between COVID-19 viral load and long-term clinical outcomes, future prospective studies, including those accounting for vaccination, should confirm our findings-19 that viral loads are related to long-term risk in those with milder disease post-vaccination.
Limitations
The strength of our study was the inclusion of all patients with COVID-19 in Hong Kong, from a real-world cohort with a wide spectrum of disease severity. A limitation of the current analyses is that viral load measurements were missing in 16% of patients. Ascertainment bias might have affected the reliability of the study due to inaccurate entry of certain diagnosis codes for comorbidities, namely DM, and hypertension. Socioeconomic status was not available for many of the patients. However, because all patients with COVID-19 were mandated to be hospitalized, this will likely not have influenced our results. Finally, some patients might have had laboratory tests performed outside of the public hospitals. Patient-reported outcome measurements (PROMs) and cognitive status measurements were not available for this study, which can provide valuable insights into patient outcomes29. It is unclear how results from Hong Kong validate in other geographic regions. Unfortunately, costing variables were not available for this paper and not included in the analyses.
Conclusion
In Hong Kong, rehospitalization after discharge for COVID-19 infection was common, especially for respiratory and gastro-intestinal reasons. A higher viral load at diagnosis is an independent risk factor for death, all-cause rehospitalization and CV rehospitalization, particularly in patients with CT values < 20. Our results can inform global discussion on the post-acute manifestations of COVID-19 and risk stratification of patients based on their viral load.
Data availability
The datasets used in the main manuscript or additional supporting files during the current study are available from the corresponding author at reasonable request.
References
Banerjee, A. et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: A population-based cohort study. Lancet 395(10238), 1715–1725. https://doi.org/10.1016/S0140-6736(20)30854-0 (2020).
Abbasi, J. Researchers investigate what COVID-19 does to the heart. JAMA 325(9), 808–811. https://doi.org/10.1001/jama.2021.0107 (2021).
Dennis, A., Wamil, M., Kapur. S. et al. Multi-organ impairment in low-risk individuals with long COVID. medRxiv. https://doi.org/10.1101/2020.10.14.20212555.
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 397(10270), 220–232. https://doi.org/10.1016/S0140-6736(20)32656-8 (2021).
Fajnzylber, J. et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nat. Commun. 11(1), 1–9. https://doi.org/10.1038/s41467-020-19057-5 (2020).
Westblade, L. F. et al. SARS-CoV-2 viral load predicts mortality in patients with and without cancer who are hospitalized with COVID-19. Cancer Cell 38(5), 661-671.e2. https://doi.org/10.1016/j.ccell.2020.09.007 (2020).
El Zein, S. et al. SARS-CoV-2 infection: Initial viral load (iVL) predicts severity of illness/outcome, and declining trend of iVL in hospitalized patients corresponds with slowing of the pandemic. PLoS One 16(9), e0255981. https://doi.org/10.1371/journal.pone.0255981 (2021).
Pujadas, E. et al. SARS-CoV-2 viral load predicts COVID-19 mortality. Lancet Respir. Med. 8(9), e70. https://doi.org/10.1016/S2213-2600(20)30354-4 (2020).
Rao, S. N., Manissero, D., Steele, V. R. & Pareja, J. A narrative systematic review of the clinical utility of cycle threshold values in the context of COVID-19. Infect. Dis. Ther. 9(3), 573–586. https://doi.org/10.1007/s40121-020-00324-3 (2020).
Girón Pérez, D. A. et al. Post-COVID-19 syndrome in outpatients and its association with viral load. Int. J. Environ. Res. Public Health 19(22), 15145. https://doi.org/10.3390/IJERPH192215145 (2022).
Bouzid, D. et al. Systematic review on the association between respiratory virus real-time PCR cycle threshold values and clinical presentation or outcomes. J. Antimicrob. Chemother. 76(Suppl 3), III33–III49. https://doi.org/10.1093/JAC/DKAB246 (2021).
Lui, G. C. Y. et al. Significantly lower case-fatality ratio of coronavirus disease 2019 (COVID-19) than severe acute respiratory syndrome (SARS) in Hong Kong-a territory-wide cohort study. Clin. Infect. Dis. 72(10), e466–e475. https://doi.org/10.1093/cid/ciaa1187 (2021).
Yip, T. C. F. et al. Liver injury is independently associated with adverse clinical outcomes in patients with COVID-19. Gut 70(4), 733–742. https://doi.org/10.1136/gutjnl-2020-321726 (2021).
Zhou, J. et al. Development of a multivariable prediction model for severe COVID-19 disease: A population-based study from Hong Kong. NPJ Digit. Med. 4(1), 66. https://doi.org/10.1038/s41746-021-00433-4 (2021).
Zhou, J. et al. Anticoagulant or antiplatelet use and severe COVID-19 disease: A propensity score-matched territory-wide study. Pharmacol. Res. 165, 105473. https://doi.org/10.1016/j.phrs.2021.105473 (2021).
Zhou, J. et al. Interaction effects between angiotensin-converting enzyme inhibitors or angiotensin receptor blockers and steroid or antiviral therapies in COVID-19: A population-based study. J. Med. Virol. 93(5), 2635–2641. https://doi.org/10.1002/jmv.26904 (2021).
Zhou, J. et al. Proton pump inhibitor or famotidine use and severe COVID-19 disease: A propensity score-matched territory-wide study. Gut 70(10), 2012–2013. https://doi.org/10.1136/gutjnl-2020-323668 (2021).
Imai, K. & Ratkovic, M. Covariate balancing propensity score. J. R. Stat. Soc. Ser. B Stat. Methodol. 76(1), 243–263. https://doi.org/10.1111/rssb.12027 (2014).
Ning, Y., Sida, P. & Imai, K. Robust estimation of causal effects via a high-dimensional covariate balancing propensity score. Biometrika 107(3), 533–554. https://doi.org/10.1093/biomet/asaa020 (2020).
Ayoubkhani, D. et al. Post-covid syndrome in individuals admitted to hospital with covid-19: Retrospective cohort study. BMJ 372, n693. https://doi.org/10.1136/bmj.n693 (2021).
Cowling, B. J. et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 5(5), e279–e288. https://doi.org/10.1016/S2468-2667(20)30090-6 (2020).
Al-Aly, Z., Xie, Y. & Bowe, B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 594(7862), 259–264. https://doi.org/10.1038/s41586-021-03553-9 (2021).
Katsoularis, I., Fonseca-Rodríguez, O., Farrington, P., Lindmark, K. & Fors Connolly, A. M. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: A self-controlled case series and matched cohort study. Lancet 398(10300), 599–607. https://doi.org/10.1016/S0140-6736(21)00896-5 (2021).
Bikdeli, B. et al. COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 75(23), 2950–2973. https://doi.org/10.1016/J.JACC.2020.04.031 (2020).
Gue, Y. X. & Gorog, D. A. Reduction in ACE2 may mediate the prothrombotic phenotype in COVID-19. Eur. Heart J. 41(33), 3198–3199. https://doi.org/10.1093/eurheartj/ehaa534 (2020).
Lupi, L., Adamo, M., Inciardi, R. M. & Metra, M. ACE2 down-regulation may contribute to the increased thrombotic risk in COVID-19. Eur. Heart J. 41(33), 3200. https://doi.org/10.1093/eurheartj/ehaa583 (2020).
Dielis, A. W. J. H. et al. The prothrombotic paradox of hypertension. Hypertension 46(6), 1236–1242. https://doi.org/10.1161/01.hyp.0000193538.20705.23 (2005).
Narula, S. et al. Plasma ACE2 and risk of death or cardiometabolic diseases: A case-cohort analysis. Lancet 396(10256), 968–976. https://doi.org/10.1016/S0140-6736(20)31964-4 (2020).
Seligman, W. H. et al. Which outcomes are most important to measure in patients with COVID-19 and how and when should these be measured? Development of an international standard set of outcomes measures for clinical use in patients with COVID-19: A report of the International Consortium for Health Outcomes Measurement (ICHOM) COVID-19 Working Group. BMJ Open 11(11), e051065. https://doi.org/10.1136/BMJOPEN-2021-051065 (2021).
Author information
Authors and Affiliations
Contributions
J.T., M.W., W.O., C.S.P., K.H.Y. conceived the study and wrote the main manuscript. J.T., M.W. performed analyses. All authors reviewed the manuscript and made critical revisions.
Corresponding authors
Ethics declarations
Competing interests
JT is supported by the National University of Singapore Start-up grant, the tier 1 grant from the ministry of education and the CS-IRG New Investigator Grant from the National Medical Research Council; has received consulting or speaker fees from Daiichi-Sankyo, Boehringer Ingelheim, Roche diagnostics and Us2.ai, owns patent US-10702247-B2 unrelated to the present work. All other authors have nothing to disclosure.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tromp, J., Wong, M., Ouwerkerk, W. et al. The association between baseline viral load and long-term risk in patients with COVID-19 in Hong Kong: a territory-wide study. Sci Rep 14, 30644 (2024). https://doi.org/10.1038/s41598-024-65764-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65764-0
This article is cited by
-
Anti-spike Antibody Response to Natural SARS-CoV-2 Infection
Bratislava Medical Journal (2025)