Abstract
The current research focuses on the effects of nutritional supplementation and exercise on dialysis patients, but whether physical activity (PA) can reduce the risk of adverse outcomes for patients with different nutritional status is not clear. The maintenance hemodialysis (MHD) patients were recruited from April 2021 to April 2022. The information of PA was obtained from the international physical activity questionnaire (IPAQ). The outcomes were cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor and all-cause death. We used COX proportional risk model to estimate the association between PA and the outcomes of MHD patients. Patients are classified into two groups based on geriatric nutritional risk index (GNRI) and classified by age, and we used COX proportional risk model to estimate the association of PA and outcomes in subgroups. The isotemporal substitution model (ISM) was used to estimate the effects of replacing light physical activity (LPA) with moderate physical activity (MPA) or vigorous physical activity (VPA) on risk of cardiovascular events, tumors, and all-cause death in different subgroups. The effects of PA on ankle-brachial index (ABI) and body fat content were analyzed in different IPAQ groups. A total of 241 maintenance hemodialysis patients were included, 105 peoples developed cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor and all-cause death (43.6%). The median follow-up time was 12 months. MPA reduced the risk of outcome in MHD patients or high GNRI patients (40% vs 39%).In MHD patients who was under 65 years with high GNRI, MPA reduced cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor and all-cause death by 55%.PA reduced the risk of cardiovascular event by 65%, but did not reduce the risk of tumor or all-cause death. Replacing LPA with VPA did not improve clinical outcomes. It actually increases the risk of heart failure 0.4%. MPA reduced the risk of cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor, all-cause death in MHD patients under 65 years, while VPA had no health benefit.
Trial registration: ChiCTR210050998.
Similar content being viewed by others
Introduction
There’s approximately 82 million adults in China suffered from chronic kidney disease (CKD) between 2018 and 20191. It is estimated that the total number of people undergoing hemodialysis in China will reach 870,000 by 20252. In recent years, with the rapid development of hemodialysis technology, the life of maintenance hemodialysis (MHD) patients has been extended, but the problems such as malnutrition, low quality of life, and decreased physical function have also emerged.
Physical activity (PA) can improve the prognosis of maintenance hemodialysis patients. Participation in physical activity is associated with a reduced risk of mortality in hemodialysis patients, with a significant decrease in mortality rate among patients who engage in at least 4000 steps3. Notably, in addition to the dialysis interval, intradialytic exercise may prevent intradialytic hypertension, although its intensity was relatively low level4,5. More importantly, the physical activity still exhibit lasting effects even after termination, alleviating the degradation of mobility within 36 months6. However, the level of physical activity decreases with the progression of kidney disease, factors such as age, gender, hemoglobin levels, and cardiovascular fitness contribute to lower physical activity levels, particularly in older individuals, females, and those with diminished hemoglobin and cardiovascular fitness7.
Nutrition and Physical activity, as modifiable factors in maintenance hemodialysis, have always been the research direction of many teams. However, current investigations focuses on nutritional therapy supplementation and the impact of physical activity on dialysis patients, without exploring whether physical activity can benefit under different nutritional states. Therefore, we established a multicenter cohort of maintenance hemodialysis patients to explore whether physical activity can improve cardiovascular events, tumors and all-cause mortality in maintenance hemodialysis patients under different nutritional status.
Results
Baseline characteristics of the study population
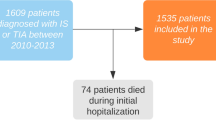
A total of 241 maintenance hemodialysis patients were enrolled, with an average age of 57 years old. 105 patients experienced major adverse cardiovascular events, including cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor or all-cause mortality, with an incidence rate of 43.6%. The median follow-up period for the cohort was 12 months.
It was observed that the population with low GNRI exhibited significantly lower levels of weight, Body Mass Index (BMI), Total Protein (TP), Albumin (ALB), Total bilirubin (TBIL), Direct Bilirubin (DBIL), Blood urea nitrogen (BUN), Creatinine (Cr), uric acid (UA), potassium (K), Calcium (Ca), Phosphorus (P), and aging than the population with high GNRI (P < 0.05). Additionally, the fasting blood glucose (FBG), serum chlorine (Cl), prevalence of diabetes and coronary heart disease was higher in the low GNRI group compared to the high GNRI group (P < 0.05). Although the physical activity, measured in METs, was higher in the high GNRI group, but this difference did not reach statistical significance (P < 0.05) (Table 1).
The relationship between physical activity levels and major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure, all-cause mortality and incidence of tumors in maintenance hemodialysis patients with different nutritional states
In our observed population, we observed that moderate physical activity volume resulted in a 40% reduction in the risk of cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor, all-cause mortality in maintenance hemodialysis patients when compared to those with low physical activity volume (HR: 0.60, 95% CI 0.4–0.92). However, high physical activity volume did not reduce the risk of outcome events in hemodialysis patients (Table 2).
When stratifying the population based on GNRI and age, among those in the high GNRI group who were under 65 years old, moderate physical activity volume significantly lowered the risk of adverse outcomes by 55% compared to low physical activity volume (HR: 0.45, 95% CI: 0.26–0.79). After adjusting for gender, moderate physical activity volume can still reduce the risk of adverse outcomes by 55% (HR: 0.41, 95% CI: 0.26–0.78). After further adjusting for indicators such as primary disease, dialysis duration, Hb, P, PTH, Cr, moderate physical activity volume still benefit (HR: 0.38, 95% CI: 0.20–0.75). The high physical activity volume maybe do not exhibit a significant reduction in the risk of adverse outcomes in this subgroup due to the small number of people. Conversely, in the low GNRI group, irrespective of age, neither moderate nor high physical activity volume did not appear to show a significant improvement in patient outcomes compared to those with low physical activity (Table 2).
The independent relationship between physical activity and major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure, all-cause mortality and incidence of tumors
In comparison to individuals with low physical activity volume, engaging in moderate physical activity volume demonstrated a substantial risk reduction in adverse cardiovascular events among MHD patients. The risk was lowered by 70%, with a HR of 0.30 and a 95% CI of 0.14–0.65. Furthermore, the risk of stroke was notably decreased by 80% with a HR of 0.2 and a 95% CI of 0.05–0.79. However, it's noteworthy that high physical activity volume did not show a significant risk reduction in outcome events for MHD patients. Moreover, when comparing individuals with low physical activity volume, both moderate and high levels of physical activity volume did not exhibit a reduction in the risk of tumor occurrence and all-cause mortality in MHD patients (Table 3).
Stratified analysis of the relationship between physical activity and major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure, all-cause mortality and incidence of tumors
In the analysis of the relationship between physical activity and adverse health outcomes in maintenance hemodialysis patients, various factors such as gender, BMI, smoking, drinking, diabetes, coronary heart disease, hypertension and dialysis duration were considered. The overarching observation is that these factors did not exert a significant influence on the overall risk of physical activity in relation to major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure, all-cause mortality and incidence of tumors in these patients.
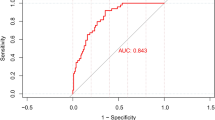
However, when conducting subgroup analysis of outcomes, we found that moderate physical activity volume can reduce cardiovascular events in patients with hypertension. In terms of all-cause mortality, individuals who do not drink alcohol may benefit from moderate physical activity volume (Fig. 1). Due to the relatively low incidence of tumors, we did not conduct further stratified analysis.
The relationship between MPA or VPA replacing LPA and adverse outcomes
In our study, we investigated the impact of replacing 60 min of LPA with either 60 min of MPA or VPA on clinical outcomes, including cardiovascular events, tumors and all-cause mortality. The results indicated that such substitutions did not lead to a reduction in the risk of adverse clinical outcomes for patients. In subgroup analysis, the risk of all-cause mortality, cardiovascular events, stroke and myocardial infarction did not decrease in patients (P < 0.05). When replacing 60 min of LPA with 60 min of MPA, the risk of heart failure increased by 0.4% (HR: 1.004, 95% 1.000–1.007). In the population with VPA, there was no occurrence of atrial fibrillation and tumors, so no analysis was conducted.
In patients with a high GNRI and under the age of 65, substituting 60 min of LPA with either moderate or VPA did not result in a reduction in the risk of clinical outcomes. Subgroup analyses within this population revealed that the risk of all-cause mortality, cardiovascular events, heart failure and atrial fibrillation did not decrease. However, it is noteworthy that the risk of stroke increased by 0.9% (HR: 1.009, 95% CI: 1.000–1.018) and 1% (HR: 1.010, 95% CI: 1.002–1.018) for MPA and VPA, respectively (Table 4).
The effects of physical activity on arterial stiffness and body composition
In assessing the impact of physical activity on arterial stiffness and body composition in patients under the age of 65 with good nutritional status, we categorized them into three groups based on their physical activity levels. Our analysis revealed noteworthy findings in both arterial stiffness and body composition. Regarding arterial stiffness, the left lower limb ABI in the moderate physical activity group exhibited a numerical decrease compared to the other two groups; however, this difference did not achieve statistical significance (Table 5).
In terms of human body composition, the left upper limb fat content, right upper limb fat content, trunk fat content, and right lower limb fat content between the low, medium, and high groups were statistically significant (P < 0.05). Patients who engage in moderate physical activity have lower left upper limb fat content, right upper limb fat content, trunk fat content, and right lower limb fat content than the other two groups. Although there was no statistically significant difference in total body fat content and left lower limb fat content compared to the other two groups, the values were significantly lower than the other two groups (Table 5).
Discussion
This study found that moderate physical activity volume can reduce the risk of cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor, all-cause mortality in maintenance hemodialysis patients under the age of 65 with low risk of malnutrition. However, in subgroup analysis, while moderate physical activity volume showed a risk reduction for cardiovascular events (cardiovascular death, myocardial infarction, stroke, heart failure and atrial fibrillation), it did not affect tumor occurrence or all-cause mortality. Notably, substituting LPA with MPA or VPA did not yield improved clinical outcomes.
GNRI is an indicator evaluated based on serum albumin levels and BMI8. The previous studies have shown that GNRI is the most accurate indicator for identifying nutritional risk in hemodialysis patients, with a critical value of 92 that can clinically identify malnutrition patients undergoing hemodialysis9,10. GNRI has advantages in predicting all-cause mortality and cardiovascular mortality11. Therefore, based on the results of previous studies, we divided maintenance hemodialysis patients into two groups: the high-risk group for malnutrition (GNRI < 92) and the low-risk group for malnutrition (GNRI ≥ 92).
Diabetic nephropathy has become the main cause of chronic kidney disease. Our baseline data showed that the prevalence of diabetic nephropathy was diverse in different nutritional status (Table 1). Compared with non-diabetic nephropathy patients, diabetic nephropathy patients have poorer nutritional status, more comorbidities, and a higher risk of death or cardiovascular events12,13. Therefore, we adjusted the primary disease in model 2 to exclude the effect of diabetes.
Physical activity emerges as a pivotal factor in preserving health and impeding disease progression across diverse populations, encompassing end-stage renal disease (ESRD) patients undergoing hemodialysis treatment14. Even mild physical activity demonstrates a negative correlation with the mortality risk in individuals with kidney disease. Notably, regular physical activity proves advantageous at all stages of kidney disease, contributing to enhancements in physical health, muscle strength, and health-related quality of life15,16,17,18. High-intensity physical activity aligns with favorable outcomes across various health-related quality of life metrics, encompassing frailty, disability, and fatigue19.
Our study found that moderate physical activity volume can reduce the risk of clinical outcomes such as cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor and all-cause death in maintenance hemodialysis patients. High physical activity volume cannot improve the clinical outcomes of dialysis patients, consistent with the results of other studies. However, when stratifying by nutritional status, we observed a positive association between moderate physical activity volume and improved clinical outcomes among patients with a high GNRI. Conversely, in the low GNRI group, engaging in moderate to high physical activity volume did not confer health benefits. This disparity could be attributed to the diminished nutritional status, reduced physical activity capacity, and suboptimal physical function in patients with a low GNRI. Moreover, considering the susceptibility of maintenance hemodialysis patients to cardiovascular and cerebrovascular events during high-intensity physical activity, our findings suggest that moderate physical activity volume might be the most suitable regimen for this patient population.
In the age stratification of patients with a high GNRI patients, we can see that those aged over 65 exhibited lower levels of various biomarkers such as Hb, WBC, ALB, Cr, TG, P, and MET compared to individuals under 65. Concurrently, the incidence of coronary heart disease was notably higher among the over65 group. These findings strongly suggest that elderly individuals above 65 years old tend to have compromised nutritional statuses and a higher prevalence of cardiovascular and cerebrovascular conditions, predisposing them to cardiovascular and cerebrovascular events. Moreover, the presence of severe underlying health conditions imposes limitations on physical activity in this age group. Although our statistical analysis did not show a reduction in tumor incidence with increased physical activity in maintenance hemodialysis patients over a median follow-up period of 1 year, it's important to note that the onset of tumors might necessitate a longer observation period for more definitive conclusions.
A cross-sectional study showed that replacing one hour of sedentary behavior with moderate intensity physical activity can reduce the incidence of chronic kidney disease by 3–4%. Additionally, even a slight increment in moderate intensity physical activity (10 min/day) appears to help maintain skeletal muscle strength in in patients with chronic kidney disease19,20,21. However, our recent study results revealed that replacing LPA with 60 min of MPA or VPA did not demonstrate significant benefits in terms of cardiovascular mortality, myocardial infarction, stroke, heart failure, atrial fibrillation, tumor incidence, all-cause mortality. This discrepancy could be attributed to our isotemporal replacement model's replacement of LPA rather than sedentary behavior, as observed in other studies, suggesting that the advantageous effects of physical activity might be specifically linked to replacing sedentary behaviors.
In terms of physical activity type, a combination of aerobic activities and resistance training stands out as the preferred regimen for enhancing outcomes in 6-min walking tests, as well as for effectively managing systolic and diastolic blood pressure. Concerning the adequacy of dialysis and the health-related quality of life, no exercise protocol or intensity demonstrated superiority over a placebo22. The recommended practice involves at least 30 min of low-to-moderate intensity physical activity, encompassing aerobic exercises such as walking, jogging, swimming, and other health-promoting activities, as well as resistance training incorporating dumbbells, resistance bands and knee extension exercises. This regimen is advised within the initial 2 h of either dialysis or non-dialysis treatments23. Our survey questionnaire shows that the majority of dialysis patients engage in LPA such as walking, and unfortunately, it is not possible to analyze the physical activity patterns.
The amelioration of physical activity and its impact on the prognosis of CKD patients predominantly correlates with the reduction of fat content and enhancement of skeletal muscle mass24. Our research indicates no statistically significant variance in the quality of skeletal muscle and skeletal muscle mass index. However, patients with moderate physical activity volume exhibit the lowest fat content, particularly in subcutaneous fat, and possess a superior quality index. Consequently, we postulate that adipose tissue serves as a pro-inflammatory risk factor for the progression of cardiovascular disease in dialysis patients. Physical activity, as per our findings, holds the potential to ameliorate the pro-inflammatory metabolic environment of patients25, leading to substantial benefits.
The IPAQ short form tends to overestimate the amount of physical activity reported compared to an objective device. In most studies the IPAQ short form overestimated physical activity level by 36–173% and IPAQ data depends on patients’ comprehension level26, In order to implement this questionnaire in MHD patients, we conducted face-to-face visits in the process of complete the questionnaire. In order to improve the accuracy of the questionnaire, we provided additional detail of the types of activities MHD patients may do. This may improve their ability to recall their activity over the course of a seven-day period; a problem highlighted by Prince et al.27, within their review of self-report validation studies.
However, it's crucial to acknowledge the limitations of this study. The sample size is relatively small, encompassing only 241 individuals, and the follow-up duration is short, with a median follow-up time of merely 12 months. To ensure more robust and stable results, there is a necessity to expand the sample size and extend the follow-up duration. Meanwhile, the PA of the participants was obtained from the IPAQ based on the patients' recall of their activities within a week, which carried a certain degree of subjectivity or error. It would be more accurate to obtain the information on PA by using the data collected by wearable devices such as accelerometers.
This study explore the association between physical activity and adverse cardiovascular events (cardiovascular death, myocardial infarction, stroke, heart failure, atrial fibrillation), tumor, all-cause death in maintenance hemodialysis patients with varying nutritional status. The findings indicate that moderate physical activity volume has a positive impact on clinical outcomes, particularly in high GNRI patients under the age of 65. It provides substantive recommendations for clinical practice, enabling interventions to be tailored more precisely to meet the specific needs of different patient populations. The study provides substantial guidance for healthcare, especially for maintenance hemodialysis patients. The doctors can take physical activity recommendations into account in their treatment regimen, especially for younger patients with high GNRI.
Methods
Study design and participants
This is a prospective observational cohort study. This study recruited 241 maintenance hemodialysis patients who underwent regular follow-up in three hospitals in Tianjin and Inner Mongolia from April 2021 to April 2022. The inclusion and exclusion criteria were strictly adhered to in order to ensure the robustness and relevance of the study population.
Inclusion criteria: (1) Regular maintenance hemodialysis patients, with a dialysis frequency of ≥ 3 times/week, a dialysis duration of 4 h/time, and dialysis duration ≥ 3 months; (2) Age ≥ 18 years old; (3) Clear awareness, able to cooperate with doctors for physical examinations and questionnaire surveys, and able to communicate normally with medical staff or family members. Exclusion criteria: (1) Simultaneously performing hemodialysis and peritoneal dialysis; (2) Recent occurrences (within the last three months) of acute infectious diseases, acute cardiovascular and cerebrovascular diseases, massive gastrointestinal bleeding, trauma, surgery, etc. in the last 3 months; (3) A history of kidney transplantation and is currently receiving immunosuppressive therapy; (4) Merge malignant tumors, hematological disorders, and mental disorders; (5) Currently in pregnancy, lactation, or with a recent pregnancy plan; (6) Cognitive or behavioral disorders, unclear consciousness, lack of cooperation or refusal to investigate.
This study was approved by the Ethics Committee of Chu Hsien-I Memorial Hospital of Tianjin Medical University (No. ZHYJNYYhMEC2021-19), and it was registered as a clinical trial with the identifier ChiCTR210050998. All participants signed informed consent. The research have been performed in accordance with the Declaration of Helsinki.
Assessment of physical activity and nutritional status
The questions on physical activity were adapted from the IPAQ short form, a validated survey instrument28. The questions simply divided PA into three types based on the intensity: light PA (LPA), moderate PA (MPA), and vigorous PA (VPA). Vigorous physical activities refer to activities that take hard physical effort and make you breathe much harder than normal, such as heavy lifting, digging, aerobics, or fast bicycling. Moderate activities refer to activities that take moderate physical effort and make you breathe somewhat harder than normal, such as carrying light loads, bicycling at a regular pace, or doubles tennis. The IPAQ assigned 3.3 Metabolic equivalents (METs) to LPA, 4.0 METs to MPA, and 8.0 METs to VPA. The number of days per week for each level of PA was multiplied by the number of minutes spent per day to calculate PA volume. The participants were divided into three groups (low, moderate, and high) based on PA volume and weekly frequency and time29 (Supplementary information).
The calculation formula for GNRI is as follows:
In previous research, it has been established that a Geriatric Nutritional Risk Index (GNRI) threshold of 92 is effective in identifying malnutrition, particularly in hemodialysis patients30,31,32. Therefore, we used a GNRI threshold of 92 to divide patients into a high GNRI group, indicating a lower risk of malnutrition (GNRI≥ 92) and a low GNRI group, indicating a higher risk of malnutrition (GNRI< 92).
Covariates
Collect demographic characteristics (including age, gender, date of birth, etc.), lifestyle habits (including alcohol consumption, smoking, etc.), history of primary and previous diseases (including hypertension, coronary heart disease, arrhythmia, stroke), and medication history of hemodialysis patients enrolled in the study. Drinking status was classified as never or current, and the same categorization was used for smoking status. Physical examination is conducted by professional doctors according to standards, collecting information such as height, weight, systolic blood pressure and diastolic blood pressure. The laboratory examination requires patients to collect blood before the second dialysis of every week. The laboratory examination covariates included blood routine, triglyceride (TG), total cholesterol (TC), high-density lipoprotein–cholesterol (HDL_C), low-density lipoprotein–cholesterol (LDL_C), blood urea nitrogen, uric acid, creatinine, estimated glomerular filtration rate (eGFR), Total Protein, Albumin, total bilirubin, direct bilirubin, alanine aminotransferase (ALT), alanine transaminase(AST) and fasting blood glucose, serum potassium, serum sodium (Na), serum chlorine, serum calcium, serum phosphorus, parathyroid hormone (PTH), serum ferritin, iron ions (Fe), and so on. The measurement time for human body composition analysis is fixed on the patient’s dialysis day before dialysis. The ankle brachial index (ABI) is measured by the Beijing Yueqi Arteriosclerosis Tester VBP-9 series.
Outcome assessment
Maintenance hemodialysis patients were treated with dialysis three times a week and followed up every 3 months. The primary outcomes of this study were all-cause mortality, major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure and incidence of tumors. The participants were followed-up with from inclusion until the incidence of all-cause mortality, major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure, tumors, or the end of the follow-up (August 31, 2022).
Statistical analysis
Baseline characteristics were compared by the GNRI using analysis of variance or Kruskal–Wallis test for continuous variables and Pearson chi-square test for categorical variables. We used Cox proportional hazard models to investigate the relationship physical activity and all-cause mortality, major adverse cardiovascular events, atrial fibrillation, hospitalization due to heart failure, and incidence of tumorsin maintenance hemodialysis patients with different nutritional status. And adjust for confounding factors. Stratified analysis was conducted based on the baseline characteristics such as gender, BMI, smoking, alcohol consumption, dialysis age, and comorbidities.
The isotemporal substitution model (ISM) was used to estimate the effects of replacing LPA with MPA or VPA on the risk of the outcome events of CKD. Compared with conventional regression modelling, ISM can provide a more accurate estimation of the potential effects of different activities. The ISM analyses make a more realistic assumption that an increase in one behaviour will be accompanied by a decrease of equivalent duration (isotemporal) in another behaviour while total time in all behaviours is kept constant33.
All statistical analyses were performed using STATA17.0 and R4.2.1 software. Two-tailed P values lower than 0.05 were considered statistically significant.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Chu Hsien-I Memorial Hospital of Tianjin Medical University (No. ZHYJNYYhMEC2021-19), and it was registered as a clinical trial with the identifier ChiCTR210050998.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Wang, L. et al. Prevalence of chronic kidney disease in China: Results from the Sixth China Chronic Disease and Risk Factor Surveillance. JAMA Intern. Med. 183(4), 298–310 (2023).
Yang, C. et al. Estimation of prevalence of kidney disease treated with dialysis in China: A study of insurance claims data. Am. J. Kidney Dis. 77(6), 889-897.e1 (2021).
Matsuzawa, R. et al. Physical activity dose for hemodialysis patients: Where to begin? Results from a prospective cohort study. J. Ren. Nutr. 28(1), 45–53 (2018).
Graham-Brown, M. P. M. et al. Design and methods of CYCLE-HD: improving cardiovascular health in patients with end stage renal disease using a structured programme of exercise: A randomised control trial. BMC Nephrol. 17(1), 69 (2016).
Ookawara, S. et al. Blood volume changes induced by low-intensity intradialytic exercise in long-term hemodialysis patients. ASAIO J. 62(2), 190–196 (2016).
F. Manfredini, G. D'arrigo, N. Lamberti, C. Torino, G. Tripepi, F. Mallamaci, C. Zoccali (2022) The legacy effect of a home walking exercise program in kidney failure patients on dialysis. Nephrol. Dial. Transplant. gfac147.
Wilkinson, T. J. et al. Prevalence and correlates of physical activity across kidney disease stages: An observational multicentre study. Nephrol. Dial Transpl. 36(4), 641–649 (2021).
Naito, T. et al. Synergistic effects of the geriatric nutritional risk index and the modifified creatinine index for predicting mortality in patients on hemodialysis. Nutrients 14(12), 2398 (2022).
Yajima, T., Yajima, K. & Arao, M. Combined evaluation of geriatric nutritional risk index and modified creatinine index for predicting mortality in patients on hemodialysis. Nutrients 14(4), 752 (2022).
Panichi, V. et al. Geriatric nutritional risk index is a strong predictor of mortality in hemodialysis patients: Data from the Riscavid cohort. J. Nephrol. 27(2), 193–201 (2014).
Yamada, S. et al. Geriatric nutritional risk index (GNRI) and creatinine index equally predict the risk of mortality in hemodialysis patients: J-DOPPS. Sci. Rep. 10(1), 5756 (2020).
Al-Ghamdi, S. M. G. et al. Diabetes prevalence, treatment, control, and outcomes among hemodialysis patients in the gulf cooperation council countries. Kidney Int. Rep. 7(5), 1093–1102. https://doi.org/10.1016/j.ekir.2022.02.012 (2022).
Hoppe, K. et al. Can overnutrition lead to wasting? The paradox of diabetes mellitus in end-stage renal disease treated with maintenance hemodialysis. Nutrients. 14(2), 247. https://doi.org/10.3390/nu14020247 (2022).
Yamamoto, S. et al. Utility of regular management of physical activity and physical function in hemodialysis patients. Kidney Blood Press Res. 43, 1505–1515 (2018).
Beddhu, S., Wei, G., Marcus, R. L., Chonchol, M. & Greene, T. Light-intensity physical activities and mortality in the United States general population and CKD subpopulation. Clin. J. Am. Soc. Nephrol. 10, 1145–1153 (2015).
Barcellos, F. C., Santos, I. S., Umpierre, D., Bohlke, M. & Hallal, P. C. Effffects of exercise in the whole spectrum of chronic kidney disease: A systematic review. ClinKidney J. 8, 753–765 (2015).
Tentori, F. et al. Physical exercise among participants in the Dialysis Outcomes and Practice Patterns Study (DOPPS): Correlates and associated outcomes. Nephrol. Dial Transpl. 25(9), 3050–3062 (2010).
Suzuki, Y. et al. Physical activity and its trajectory over time and clinical outcomes in hemodialysis patients. Int. Urol. Nephrol. 54(8), 2065–2074 (2022).
Zhang, F., Wang, H., Wang, W. & Zhang, H. The role of physical activity and mortality in hemodialysis patients: A review. Front. Public Health 17(10), 818921 (2022).
Wang, Y., Nie, J., Ferrari, G., Rey-Lopez, J. P. & Rezende, L. F. M. Association of physical activity intensity with mortality: A national cohort study of 403,681 US adults. JAMA Intern. Med. 181(2), 203–211 (2021).
Yoshioka, M. et al. Replacing sedentary time for physical activity on bone density in patients with chronic kidney disease. J. Bone Miner. Metab. 39(6), 1091–1100 (2021).
Song, Y. et al. The optimal exercise modality and intensity for hemodialysis patients incorporating Bayesian network meta-analysis and systematic review. Front. Physiol. 13, 945465 (2022).
Y. Li, X. Wang, Z. Pei. Advances in exercise therapy in hemodialysis: A systematic review. Mini Rev. Med. Chem. (2022).
N.M. Chu, J. Hong, O. Harasemiw, X. Chen, K.J. Fowler, I. Dasgupta, C. Bohm, D.L. Segev, M.A. McAdams-DeMarco (2022) Global Renal Exercise Network. Chronic kidney disease, physical activity and cognitive function in older adults-results from the National Health and Nutrition Examination Survey (2011–2014). Nephrol. Dial Transpl. 37(11), 2180–2189.
Zelle, D. M. et al. Physical inactivity: A risk factor and target for intervention in renal care. Nat. Rev. Nephrol. 13(3), 152–168 (2017).
Lee, P. H., Macfarlane, D. J., Lam, T. H. & Stewart, S. M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 8, 115. https://doi.org/10.1186/1479-5868-8-115 (2011).
Prince, S. A. et al. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 5, 56–60. https://doi.org/10.1186/1479-5868-5-56 (2008).
Craig, C. L. et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
Fan, M., Lyu, J. & He, P. Chinese guidelines for data processing and analysis concerning the International Physical Activity Questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi. 35(8), 961–964 (2014).
Chen, J. et al. Comparison of three nutritional screening tools for predicting mortality in maintenance hemodialysis patients. Nutrition. 67–68, 110532 (2019).
Takahashi, H. et al. Geriatric nutritional risk index accurately predicts cardiovascular mortality in incident hemodialysis patients. J. Cardiol. 64(1), 32–36 (2014).
J. Xiong, M. Wang, J. Wang, K. Yang, Y. Shi, J. Zhang, B. Zhang, L. Zhang, J. Zhao (2020) Chinese Cohort Study of Chronic Kidney Disease (C-STRIDE). Geriatric nutrition risk index is associated with renal progression, cardiovascular events and all-cause mortality in chronic kidney disease. J. Nephrol. 33(4), 783–793.
Cao, Z. et al. Associations of sedentary time and physical activity with adverse health conditions: Outcome-wide analyses using isotemporal substitution model. EClinicalMedicine 28(48), 101424 (2022).
Acknowledgements
We gratefully acknowledge the participants of the research.
Funding
This research was funded by First Level Leading Talent Project of "123 Climbing Plan" for Clinical Talents of Tianjin Medical University, "Tianjin Medical Talents" project, the second batch of high-level talents selection project in health industry in Tianjin (No. TJSJMYXYC-D2-014), Key Project of Natural Science Foundation of Tianjin (No.22JCZDJC00590), Scientific Research Funding of Tianjin Medical University Chu Hsien-I Memorial Hospital (No. ZXY-ZDSYSZD-1), Tianjin Science and Technology Major Special Project and Engineering Public Health Science and Technology Major Special Project (No. 21ZXGWSY00100), Tianjin Key Medical Discipline (Specialty) Construct Project (No. TJYXZDXK-032A), China International Medical Foundation (No. Z-2017-26-1902-5).
Author information
Authors and Affiliations
Contributions
Conceptualization, Hongyan Liu; Formal analysis, Hongyan Liu; Funding acquisition, Pei Yu; Methodology, Hongyan Liu and Yao Lin; Project administration, Pei Yu; Software, Hongyan Liu; Supervision, Pei Yu; Validation, Yao Lin; Writing–original draft, Hongyan Liu; Writing – review & editing, Hongyan Liu.All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, H., Chen, Y., Feng, T. et al. The association between physical activity and cardiovascular events, tumors and all-cause mortality in patients with maintenance hemodialysis with different nutritional status. Sci Rep 14, 16924 (2024). https://doi.org/10.1038/s41598-024-67707-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67707-1