Abstract
In this retrospective cohort study the survival rate, clinical parameters, patient satisfaction with aesthetics and oral health-related quality of life of 3D printed temporary crowns were evaluated. Temporary crowns were 3D printed with a Form3B out of Permanent Crown Resin (Formlabs GmbH). Anonymized data for the restorations’ survival (in-situ) was evaluated retrospectively for 98 temporary crowns of 63 patients fabricated within 19 months. Among these restorations, further analysis was conducted for 42 temporary crowns of 24 patients regarding clinical parameters (modified USPHS criteria), patient satisfaction with aesthetics and impact on oral health-related quality of life (OHRQoL) (OHIP 14). Descriptive statistical analysis (significance level of α = 0.05) included a Kaplan–Meier curve for survival analysis, a Kolmogorov–Smirnov test for USPHS, aesthetics and OHIP data, followed by a Wilcoxon test for USPHS and OHIP data and Chi-squared test for aesthetics data. Cronbach’s alpha was calculated for OHIP data. The average observation period for survival analysis was 256 days. The survival rate was satisfactory at 98% and n = 2 catastrophic failures (i.e. fracture) occurred. Total OHIP scores, with good reliabilities, improved from 6.63 to 2.21 significantly (p = 0.005) and patient satisfaction with aesthetics (p < 0.001) as well. Clinical analysis with modified USPHS criteria revealed encouraging results.
Similar content being viewed by others
Introduction
Crowns are an established restorative method with the availability of various restorative materials. Due to computer assistance, computer-aided-design (CAD) / computer-aided-manufacturing (CAM) represents a development that enables further options1. CAM includes subtractive (s-CAM) and additive (a-CAM) manufacturing of materials such as ceramics, alloys or resins. S-CAM is considered the gold standard within its limitations2.
3D printing, representing an a-CAM method, is a novel production method and can be utilized to produce resin-based products such as crowns, bridges, bite splints or prothesis. While some materials enable a permanent intraoral use or restoration, other materials are approved for a temporal intraoral use only. Generally, materials require an approvement as legitimated for intraoral use. Overall, there is an increasing popularity of 3D printing in dentistry, however, limited information on clinical performance is available3. Clinical outcomes of resin-based crowns fabricated with s-CAM have been reported4 and survival rates of 100% after 6 months5 and 87.9% after 3 years6 were observed. However, limited data is available for the survival rate and clinical performance of a-CAM restorations.
Permanent Crown Resin (Formlabs GmbH, Berlin, Germany) is a material for additive manufacturing of 3D printed biocompatible crowns for permanent use. It can be utilized to produce single crowns, onlays, inlays and veneers with unlimited residual duration. Formlabs states that Permanent Crown Resin restorations are accurate with precise fitment and low tendency of aging effects. Temporary crowns are utilized for teeth with unclear prognosis, such as severe attachment loss or defects, and represent a crucial step in pre-prosthetic treatments.
The aims of this retrospective cohort study were to evaluate the survival of 3D printed temporary crowns and analyze their clinical parameters, satisfaction with aesthetics and impact on oral health-related quality of life (OHRQoL).
The null hypothesis was that 3D printed temporary crowns fabricated out of Permanent Crown Resin perform poorly compared to resin-based s-CAM restorations (data obtained from literature) regarding their technical survival.
Materials and methods
This retrospective cohort study has been approved by the Institutional Review Board (University of Würzburg, Germany) and usage of anonymized data of the Department of Prosthodontics of the University of Würzburg for the observation period from 01 December 2021 to 30 June 2023 was granted on 11 July 2023 (20230710 01). All methods were performed in accordance with the named guidelines, regulations and Declaration of Helsinki.
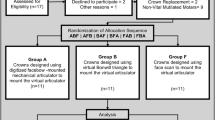
Study design
Patients from the Department of Prosthodontics of the University of Würzburg with 3D printed temporary crowns out of Permanent Crown Resin between 01 December 2021 and 30 June 2023 were included in this study – overall 63 patients with a total of 98 temporary crowns. All types of teeth were included. There were no exclusion criteria upon tooth location, endodontic status, attachment level or patients’ temporomandibular disorder and bruxism. A prosthetic preparation for a crown with a chamfer type of finish line was performed on all teeth, under the premise of a defect oriented preparation, i.e., surpassing build-up fillings where existing.
Survival was defined by the in-situ criterion. A catastrophic failure was defined by a technical defect, i.e., chipping or fracture, which required a new restoration. All other complications were, if documented, recorded, e.g., biological complication of the tooth, removal of the temporary crown for replacement with a permanent crown or cementation failure.
Among the 98 temporary crowns, further analysis was conducted for 42 temporary crowns of 24 patients. These 42 restorations were provided in predoctoral courses and reevaluated at recalls, supervised by experienced dentists under a standardized protocol. Within the predoctoral courses a thorough documentation was conducted, enabling the further analysis for these 42 restorations. Analysis of clinical parameters was enabled via modified USPHS criteria (Table 1), providing descriptives for an evaluation with “alpha”, “bravo”, “charlie” or “delta”. Patient satisfaction with aesthetics and OHRQoL were recorded at baseline before treatment and at recall sessions. For estimating patient satisfaction with aesthetics, the Wong-Baker FACES scale was utilized, a scale with six faces spanning from a happy face to a crying face. This scale is often used for self-assessment and communication of severity of pain7. In this study it was utilized to compare satisfaction with aesthetics of the corresponding area before treatment and the temporary crown in the recall session. OHRQoL was determined via the shortened version of the Oral Health Impact Profile (OHIP 14) in its German version (OHIP-G 14), providing a Lickert scale with numerical values where higher sum values represent a compromised OHRQoL and vice versa.
3D printed temporary crowns
Fabrication (see Fig. 1 for an exemplary production process) of all restorations followed a standardized protocol: After the preparation of the teeth, followed by conventional impression taking, plaster models were cast and digitalized with the laboratory scanner inEos X5 (Dentsply Sirona, Bensheim, Germany). Restorations were designed in accordance with Formlabs’ guidelines utilizing inLab 20 (Dentsply Sirona, Bensheim, Germany). The general construction requirements resulted in a minimum thickness of the restorations of 1mm, the cement gap was set at 0.04 mm and the drill compensation was disabled. The restorations were imported into the printing software Preform (Formlabs GmbH, Berlin, Germany) for upload to a Form3B (Formlabs GmbH, Berlin, Germany). Temporary crowns were 3D printed with Permanent Crown Resin. Postprocessing was conducted in accordance with the manufacturer’s guidelines by washing, drying, removing supports, post-curing, blasting, finishing, and polishing the temporary crowns. All restorations were cemented with RelyX Unicem (3M ESPE AG, Seefeld, Germany).

(Source: own figure) (a). Conventional impression (b). Plaster model (c). Digitalization with a laboratory scanner (d). Designed restoration in a virtual model (e). 3D printed restoration with resin residues and support structures (f). Test fitting of non-finished restoration on the plaster model (g). Finished 3D printed temporary crown.
Exemplary production process of a 3D printed temporary crown.
Statistics
A minimal sample size of n = 66 restorations was calculated for a relevant statement upon the survival rate, assisted by the Department of Clinical Epidemiology and Biostatistics of the University of Würzburg, under the assumptions that a good survival rate is represented by a failure rate per year of equal or less than 2% and a bad survival rate is represented by 15% or above. As 98 restorations were fabricated between 01 December 2021 and 30 June 2023, all were included in this retrospective cohort study.
Anonymized data was evaluated and analyzed, utilizing Excel (Microsoft Cooperation, Redmond, USA) and IBM SPSS Statistics (Version 29; IBM, Armonk, USA). Descriptive analysis was conducted, and the significance level was set at α = 0.05. For survival analysis, a Kaplan–Meier curve was generated. Kolmogorov–Smirnov was utilized for testing the normality of the distribution of USPHS, aesthetics and OHIP data, followed by the Wilcoxon test for OHIP data and the Chi-squared test for aesthetics data. Cronbach’s alpha was calculated for OHIP data to determine the reliability.
Results
Survival
98 temporary crowns of 63 patients were included with a mean observation time (standard deviation) of 266 (± 130) days, reaching from 18 to 557 days (Table 2). Patients were 63 years old on average and included 27 men and 36 women.
Within the observation period two catastrophic failures occurred due to chipping and fracture resulting in 96 censored restorations. Other non-catastrophic complications included decementation (n = 2), loss of teeth due to trauma and endodontic complication (n = 2), and removals for replacement with a permanent crown (n = 7) – see Table 3. Data was visualized with a Kaplan–Meier curve (Fig. 2).
Overall, the survival rate of the 3D printed temporary crowns was 98% at the end of the observation period, thus the null hypothesis had to be rejected.
Clinical parameters
As further analysis was conducted for 42 temporary crowns of 24 patients, their mean observation time (standard deviation) was 210 (± 120) days, reaching from 29 to 535 days (Table 2). Upon analysis with the Kolmogorov Smirnov test, no normality of the distribution of USPHS data was observed (p < 0.001). Data was visualized with a bar chart (Fig. 3).
The following three aspects were evaluated ≥ 98% with “alpha”: anatomical form, secondary caries and postoperative sensitivity to air. “Alpha” was scored at 81% for color match, 79% for surface texture, 74% for both marginal integrity and marginal discoloration and 69% for restoration color stability. Marginal inflammation was evaluated at 79% with “bravo”.
Patient satisfaction with aesthetics
For the cohort including 42 temporary crowns of 24 patients, data was analyzed for the baseline session (T0) regarding satisfaction with aesthetics in the corresponding area, and for the recall sessions (T1) regarding satisfaction with aesthetics of the temporary crown. A Kolmogorov Smirnov test revealed no normality of the distribution of data (T0 p = 0.016, T1 p < 0.001).
83% of patients rated their satisfaction with aesthetics with the happiest face at T1, compared to 25% at T0. Overall, patient satisfaction with aesthetics improved from T0 to T1 significantly (p < 0.001). Data is visualized in a bar chart (Fig. 4).
Impact on OHRQoL
For 42 restorations of 24 patients, OHIP 14 data was analyzed for the baseline (T0) and at recall (T1) for evaluation of an impact on OHRQoL. OHIP mean sum values (standard deviation) were 6.63 (± 6.80) for T0 and 2.21 (± 4.53) for T1. Upon a Kolmogorov Smirnov test, the data was seen to not be normally distributed (T0 and T1 p < 0.001). Cronbach’s alpha was α = 0.788 for T0 and α = 0.803 for T1, yielding good reliability (Table 4). The Wilcoxon test revealed a significant (p = 0.005) improvement in OHIP sum values from T0 to T1, implying a significantly positive impact on OHRQoL.
Discussion
The study included 98 temporary crowns of 63 patients for survival analysis, with a mean observation time of 266 days, and further analysis for 42 restorations of 24 patients, with a mean observation time of 210 days. Observation time and restorations were limited, however, Permanent Crown Resin was released in 2020 as a limiting factor overall. Studies with s-CAM resin based restorations had observation periods of several years, e.g., 5 years4, and data on conventionally fabricated crowns exists for longer observation periods, e.g., 15 years8. As this study dealt with temporary crowns, although cemented permanently with Rely X Unicem, the observation period seems to be appropriate.
As there is an increasing trend in the accessibility and growth of the 3D printing industry9, several materials for the fabrication of permanent fixed dental prothesis have been introduced10. The Form3B 3D printer is equipped with a 250mW laser and features an XY resolution of 25µm and a layer thickness of 25µm, varying by material. CAD/CAM allows fast and reproducible production processes11, enabling an easy reproduction in case of a failure. A single crown requires approximately 0.3ml of resin, resulting in approximately 0.40€ costs—thus representing a feasible production.
The findings of this study revealed a survival rate of 98% with two catastrophic failures such that at the end of the observation rate 96 restorations remained in-situ. Thus, it could be stated that the 3D printed temporary crowns performed equally to s-CAD resin based restorations, based upon data from other studies with a survival of 100% after 6 months5, and the null-hypothesis was rejected.
3D printed crowns can be utilized as temporary crowns in pre-prosthetics, as in this study, or for testing new vertical dimensions in complex cases12. The findings do not underline the necessity of a temporization and there was no resulting interference with the restorations’ success, prognosis or demise. USPHS criteria are often used for evaluation of dental restorations, they have been criticized and FDI criteria were recommended13,14. The evaluation of the restorations’ clinical parameters was conducted in preclinical education, supervised by experienced dentists. Although calibration of examiners is recommended15, this could not be taken into account within this study’s design.
Permanent Crown Resin is a ceramic infiltrated resin, however, surface texture was evaluated as “bravo” for 21%. Several studies showed, that aging processes have an influence on the surface structure of composite resins16,17 and Papathanasiou et al. additionally found visible but acceptable color changes for milled composite resins. Thus, the results of the present study are in line with these findings. Marginal inflammation was evaluated at 79% with “bravo”, however, teeth were partially in compromitted state, yielding the indication of a temporary crown. This might explain the relatively high rate of inflammation in these compromised teeth. Although no other in vivo or in vitro studies exist with Permanent Crown Resin to the authors’ knowledge, composites are compatible with subgingival health18. Wuersching et al. concluded that monomer composition, presence and type of photo initiator and mode of polymerization affected the biocompatibility of dental resins and suggested further post-processing, i.e. additional light curing and washing, to improve the biocompatibility10. OHIP 14 sum values revealed a significant improvement (p = 0.005) from T0 to T1, implying a significant positive impact on OHRQoL. OHIP 5, the shortened form with 5 items, can already provide an insight into patients’ perception19. Overall, the cohort was very inhomogeneous and could not be stratified in discrete subgroups due to the limited number of patients. However, factors such as position of the restoration, age and gender of the patients affect the OHRQoL20,21.
A significant improvement was found regarding patient satisfaction with aesthetics. However, the cohort was very inhomogeneous, and restorations were located at various regions. Thus, generalization of the findings is limited. The Wong-Baker FACES scale is an established instrument22, whereas visual analog scales provide an objective and reliable instrument with high validity23.
The 3D printed temporary crowns were monolithic with a homogenous color. Advanced aesthetics could be achieved by utilizing light-cured glaze and characterization, such as GC OPTIGLAZE™ (GC Cooperation, Hongo, Bunkyo-ku, Tokyo).
Patient related variables such as parafunctional habits, caries activity, general and periodontal health, as well as operator related variables influence can influence dental restorations’ survival24. The absence of exclusion criteria, resulting in inclusion of teeth with diverse conditions before treatment and inclusion of patients with diverse risk factors, and diverse operators represent limitations of the study’s findings. Future studies should contain further stratification to analyze different risk factors individually upon the restorations’ survival and clinical parameters.
Conclusions
The 3D printed temporary crowns fabricated out of Permanent Crown Resin achieved a survival rate of 98% within this retrospective cohort study. Patients benefitted from significant improvements in oral health-related quality of life and satisfaction with aesthetics. The analysis of clinical parameters demonstrated encouraging results of the 3D printed temporary crowns.
Data availability
All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials.
References
Miyazaki, T. & Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 56, 97–106. https://doi.org/10.1111/j.1834-7819.2010.01300.x (2011).
Mühlemann, S., Hjerppe, J., Hämmerle, C. H. F. & Thoma, D. S. Production time, effectiveness and costs of additive and subtractive computer-aided manufacturing (CAM) of implant prostheses: A systematic review. Clin. Oral Implants Res. 32, 289–302. https://doi.org/10.1111/clr.13801 (2021).
Balhaddad, A. A. et al. Three-dimensional (3D) printing in dental practice: Applications, areas of interest, and level of evidence. Clin. Oral Investig. 27, 2465–2481. https://doi.org/10.1007/s00784-023-04983-7 (2023).
Komine, F. et al. Clinical outcomes of single crown restorations fabricated with resin-based CAD/CAM materials. J. Oral Sci. 62, 353–355. https://doi.org/10.2334/josnusd.20-0195 (2020).
Dirxen, C., Blunck, U. & Preissner, S. Clinical performance of a new biomimetic double network material. Open Dent. J. 7, 118–122. https://doi.org/10.2174/1874210620130904003 (2013).
Vanoorbeek, S., Vandamme, K., Lijnen, I. & Naert, I. Computer-aided designed/computer-assisted manufactured composite resin versus ceramic single-tooth restorations: a 3-year clinical study. Int J Prosthodont 23, 223–230 (2010).
Mendonça, F. L. et al. Sensitivity treatments for teeth with molar incisor hypomineralization: Protocol for a randomized controlled trial. JMIR Res. Protoc. 11, e27843. https://doi.org/10.2196/27843 (2022).
Erpenstein, H., Kerschbaum, T. & Fischbach, H. Verweildauer und klinische Befunde bei Kronen und Brücken Eine Langzeitstudie. Dtsch Zahnärztl Z 47, 315–319 (1992).
Tahayeri, A. et al. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 34, 192–200. https://doi.org/10.1016/j.dental.2017.10.003 (2018).
Wuersching, S. N., Hickel, R., Edelhoff, D. & Kollmuss, M. Initial biocompatibility of novel resins for 3D printed fixed dental prostheses. Dent. Mater. 38, 1587–1597. https://doi.org/10.1016/j.dental.2022.08.001 (2022).
Fasbinder, D. J. Digital dentistry: innovation for restorative treatment. Compend. Contin. Educ. Dent. 31(4), 2–11 (2010).
Höhne, C. & Schmitter, M. Control of occlusal rehabilitation with 3D-printed crowns. Int. J. Comput. Dent. 25, 325–332. https://doi.org/10.3290/j.ijcd.b3380909 (2022).
Hickel, R. et al. Revised FDI criteria for evaluating direct and indirect dental restorations-recommendations for its clinical use, interpretation, and reporting. Clin. Oral Investig. 27, 2573–2592. https://doi.org/10.1007/s00784-022-04814-1 (2023).
Marquillier, T. et al. The use of FDI criteria in clinical trials on direct dental restorations: A scoping review. J. Dent. 68, 1–9. https://doi.org/10.1016/j.jdent.2017.10.007 (2018).
Hickel, R. et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Int. Dent. J. 57, 300–302. https://doi.org/10.1111/j.1875-595x.2007.tb00136.x (2007).
Imtiaz, T., Ganesh, S. B. & Jayalakshmi, S. Surface roughness changes of two composite resin restorative materials after thermocycling. J. Adv. Pharm. Technol. Res. 13, S466-s469. https://doi.org/10.4103/japtr.japtr_255_22 (2022).
Papathanasiou, I., Zinelis, S., Papavasiliou, G. & Kamposiora, P. Effect of aging on color, gloss and surface roughness of CAD/CAM composite materials. J. Dent. 130, 104423. https://doi.org/10.1016/j.jdent.2023.104423 (2023).
Bertoldi, C. et al. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin. Oral Investig. 24, 1001–1011. https://doi.org/10.1007/s00784-019-02998-7 (2020).
Schierz, O. & Reissmann, D. R. Dental patient-reported outcomes – the promise of dental implants. J. Evid. Based Dent. Pract. 21, 101541. https://doi.org/10.1016/j.jebdp.2021.101541 (2021).
Özhayat, E. B. & Gotfredsen, K. Effect of treatment with fixed and removable dental prostheses. An oral health-related quality of life study. J. Oral Rehabil. 39, 28–36. https://doi.org/10.1111/j.1365-2842.2011.02245.x (2012).
Sukumar, S., John, M. T., Schierz, O., Aarabi, G. & Reissmann, D. R. Location of prosthodontic treatment and oral health-related quality of life–an exploratory study. J. Prosthodont. Res. 59, 34–41. https://doi.org/10.1016/j.jpor.2014.11.003 (2015).
Garra, G. et al. Validation of the wong-baker FACES pain rating scale in pediatric emergency department patients. Acad. Emerg. Med. 17, 50–54. https://doi.org/10.1111/j.1553-2712.2009.00620.x (2010).
Schmitter, M., List, T. & Wirz, S. The assessment of pain intensity using one-dimensional scales. Z Evid Fortbild Qual Gesundhwes 107, 279–284. https://doi.org/10.1016/j.zefq.2013.05.008 (2013).
Laske, M., Opdam, N. J. M., Bronkhorst, E. M., Braspenning, J. C. C. & Huysmans, M. Risk factors for dental restoration survival: A practice-based study. J. Dent. Res. 98, 414–422. https://doi.org/10.1177/0022034519827566 (2019).
Acknowledgements
The authors gratefully acknowledge all colleagues and students involved in this study.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
M.H. Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing—Original Draft Preparation I.L. Data Curation, Investigation, Writing—Review & Editing C.H. Conceptualization, Methodology, Writing—Review & Editing M.S. Conceptualization, Project Administration, Resources, Supervision, Writing—Review & Editing
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
del Hougne, M., Di Lorenzo, I., Höhne, C. et al. A retrospective cohort study on 3D printed temporary crowns. Sci Rep 14, 17295 (2024). https://doi.org/10.1038/s41598-024-68354-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68354-2
Keywords
This article is cited by
-
3D printed teeth for bridge preparation training: development and assessment in dental education
BMC Medical Education (2025)
-
3D printed tooth for endodontic training in dental education
Scientific Reports (2025)