Abstract
Prolonged disorder of consciousness (DoC) is a rising challenge. Pediatric data on diagnosis and prognosis of prolonged DoC were too limited and heterogeneous, making it difficult to define the natural course and evaluate the prognosis. The present study explored the emergence from the Minimally Conscious State (eMCS) incidence at different months postinjury drawing the natural course, and detected the predictors of the incidence in children with prolonged DoC. A hospital-based prospective cohort study was conducted. Kaplan–Meier curves, as well as univariate and multivariate COX regression analysis, were performed. The study enrolled 383 pediatric DoC individuals, including 220 males (57.4%), with an average age of 3.9 (1.9–7.3) years. The median duration between onset and rehabilitation is 30.0 (21.0–46.0) days. At enrollment, the ratio of vegetative state/unresponsive wakefulness syndrome (VS/WUS) to MCS is 78.9%–21.1%. Traumatic brain injury and infection are the major etiologies (36.8% and 37.1%, respectively), followed by hypoxia cerebral injury (12.3%). For children with prolonged DoC, the cumulative incidence of eMCS at months 3, 6, 12, and 24 was 0.510, 0.652, 0.731, 0.784 VS 0.290, 0.418, 0.539, 0.603 in the traumatic VS non-traumatic subgroup, respectively. For children in a persistent vegetative state (PVS), the cumulative incidence of emergence at months in 3, 6, 12, 24, 36 and 48 was testified as 0.439, 0.591, 0.683, 0.724, 0.743 and 0.743 in the traumatic subgroup, and 0.204, 0.349, 0.469, 0.534, 0.589 and 0.620 in the non-traumatic subgroup. Participants who exhibit any of the following four demographical and/or clinical characteristics—namely, older than 4 years at onset, accepted rehabilitation within 28 days of onset, remained MCS at enrollment, or with etiology of traumatic brain injuries—had a significantly positive outcome of consciousness recovery (eMCS). Moreover, both prolongation of the central somatosensory conductive time (CCT) (level 2) and absence of N20 (level 3) independently predict a negative outcome. In children with prolonged DoC, we found that 12 months postinjury was critical to eMCS, and a preferred timepoint to define chronic vegetative state (VS). The characteristics including age, etiology, time before rehabilitation, consciousness state, and SEP results were useful predictors of conscious recovery.
Trial registration Registered 06/11/2018, the registration number is chiCTR1800019330 (chictr.org.cn). Registered prospectively.
Similar content being viewed by others
Background
Prolonged (i.e., lasting at least 28 days) disorder of consciousness (DoC) in children is a rising challenge not only in the medical field, but also for society and the involved family1. Prolonged DoC includes the vegetative state/unresponsive wakefulness syndrome (VS/UWS)2,3 and the minimally conscious state (MCS)4, resulting from severe acquired brain injury (ABI) that disrupts the brain’s arousal and awareness systems. Benefiting from the rapid development of pediatric intensive care medicine, an increasing number of individuals with prolonged DoC survive are admitted to rehabilitative therapy. The prognosis is a complex process that involves prognostic counseling, treatment strategy, and the following plan of the involved family1,5. This process may incur heavy medical expenses6 and is the greatest concern for both the physician and the family.
Despite the enormity of the challenge in pediatric prolonged DoC, related clinical studies on prognosis are scarce and no practice guidelines are available7. According to the 2018 American Academy of Neurology (AAN) practice guideline on DoC, tests including structural MRI, the coma recovery scale-revised (CRS-R), and Single-Photon Emission Computed Tomography (SPECT) can assist prognostication in adults. However, no tests are shown to improve prognostic accuracy in children. The guideline also recommends that the term permanent VS should be replaced by chronic VS/UWS (i.e., 3 months after non-traumatic brain injury (TBI) and 12 months after TBI). However, for children with prolonged DoC, the natural course of disease and prognosis are unclear5, whether the cut-off point of the chronic VS/UWS of adults is appropriate for pediatric individuals remained a puzzle.
At present, most available studies focus on adult individuals with prolonged DoC. From the studies, the characteristics and clinical data including age, gender, level of consciousness, time before rehabilitation, etiology, and so on are significant prognostic factors. Younger onset, shorter length of stay in the intensive care unit, and traumatic etiology were the independent prognostic predictors of better outcomes10,11. The absence of N20 for somatosensory evoked potential (SEP) and of wave V for brainstem auditory evoked potential (BAEP) were correlated with worse outcomes5,11,12,13. In general, MCS at the admission of rehabilitation from the intensive care unit had higher survival rates and facilitation of consciousness recovery14. However, it is challenging to obtain consistent results from children due to their development character and the great plasticity potential after injury. On the other hand, the results from limited DoC studies in children were mainly on single etiology (traumatic or hypoxia), with the conclusion remaining controversial8,9,15,16,17,18. Pediatric data on prognosis reported were too limited and heterogeneous to arrive at viable conclusions. The natural course of pediatric DOC had not been defined clearly, notably, there was no outstanding proposal for accurate prognostication.
Given the lack of reliable knowledge worldwide, especially the absence of reports focusing on the prognosis of pediatric inpatients with prolonged DOC in China, we implemented a prospective cohort study at the Children’s Hospital of Chongqing Medical University. Because the prognosis model with multi-technique integration would facilitate the accuracy of prediction19, we analyzed both the demographical and clinical characteristics, especially the evoked potentials. This real-world cohort study aimed to find out the accumulative recovery rate of pediatric inpatients with prolonged DoC, and further reveal the prognosis predictors, which can be easily obtained in clinical practice.
Material and methods
Study design
The present study was an ambispective observational cohort study. Individuals admitted from January 2014 to December 2018 were enrolled through a retrospective chart study. Individuals admitted to rehabilitation from January 2019 to December 2021 were prospectively recruited and followed up. The study was approved by the ethics committee of the Children’s Hospital of Chongqing Medical University. Written informed consent was obtained from parents or legal caregivers before the beginning of the study.
Participants
The study was performed at the Children’s Hospital of Chongqing Medical University, and all participants with prolonged DoC were admitted consecutively to the rehabilitation department for the first time between January 2014 and December 2021. The inclusion criteria were listed as follows: (1) diagnosed as VS/UWS, or MCS according to the standard diagnosis criteria2,20; (2) aged younger than 17 years; (3) the vital signs were stable, and there was no life-threatening comorbidity. Exclusion criteria were as follows: (1) there was a definite past history of heredity diseases, congenital metabolic diseases, tumor, or cerebral injuries; (2) the subjects showed developmental disorders like intelligence disorder or impaired daily function prior to the injuries; (3) clinical behavioral tests had not been performed promptly at hospitalization.
During the hospital stay, all subjects accepted a multi-disciplinary rehabilitative program. The standard daily treatments rehabilitation therapy, as determined by their injuries and dysfunctions comprised the followings: (1) passive mobilization and movement stimulation (e.g., normal limb position, sitting and upright position training); (2) prevention and treatment of medical comorbidities (joint contracture, infection, malnutrition, epilepsy, etc.); (3) perception stimulation to facilitate consciousness; (4) speech therapy and cognitive supervision. Rehabilitation goals varied depending on individual severity. After the final discharge, most individuals received rehabilitative treatment in out-patient, while the rest returned to home-based local rehabilitation facilities per family decision.
Procedure and variates extraction
We collected the following demographic and clinical data from medical charts: (1) age of onset; (2) gender; (3) etiology (trauma, infection, hypoxia, others); (4) consciousness state at the rehabilitative admission; (5) the interval between onset and rehabilitative admission; (6) score of Coma Recovery Scale-Revised (CRS-R), (7) somatosensory evoked potential (SEP) results, and 8) brainstem auditory evoked potential (BAEP) results. Subjects with incomplete aforementioned data were excluded. Furthermore, past history of intelligence, behavioral testing for conscious evaluation, and the time of follow-up endpoint were obtained. Finally, we coded the eight factors to analyze as covariates.
In retrospective chart collection, data were obtained and evaluated by two experienced rehabilitation specialists. The diagnosis of consciousness state was confirmed by the previous criteria according to the clinical records4,21, and the Alvarez criteria22 was applied to evaluate the consciousness of toddler subjects younger than 4. For subjects admitted from January 2019, the two rehabilitation specialists each performed two clinical behavioral evaluations within 3 days of admission independently. Considering the fluctuation of consciousness during hospitalization, any change in communicating, staring, pain locating, etc., observed by caregivers or medical staff would be evaluated by an additional behavioral test.
Evaluation and therapy
Somatosensory evoked potential (SEP) and brainstem auditory evoked potential (BAEP) were recorded within one week after the first admission of rehabilitation in most subjects. The Dantec Keypoint Focus EMG/NCS/EP system was utilized and technical standards were set according to the guidelines of the American clinical neurophysiology society for evoked potentials. According to the Judson criteria23, SEP was graded into 3 levels, grade I referred to normal bilateral central somatosensory conductive time (CCT), and grades II and III referred to unilateral or bilateral prolonged CCT and absent cortical potential, respectively. CANT criteria classified BAEPs according to the increase in wave I-V interval or the loss of Wave V24. Grade I means normal BAEPs, grade II means abnormal BAEPs without the absence of wave V of either ear, and grade III means the unilateral or bilateral absence of wave V.
Outcome ascertainment
The end of follow-up included emergence from MCS (eMCS) or death. Death was recorded in detail by the date, consciousness state prior to the death, and the cause. The interest event was defined as an eMCS; survival time was defined as the duration between onset and the emergence. The latest end time for follow-up was March 1st, 2022.
Follow-up
The consciousness state (CRS-R) and functions of daily living (the Glasgow Outcome Scale Extended, GOSE), playing, and learning were mainly evaluated during the follow-up. The majority of participants continued rehabilitative treatments by repeat admission or received outpatient rehabilitation in our hospital. Their follow-up evaluations were obtained through face-to-face interviews regularly. Additional interviews and evaluations were organized promptly in the case of conscious alteration, including functional communication (eye contact, body language, or even verbal communication), functional object use, or playing toys. Telephone interviews were made for the participated family who cannot get back to the hospital, and evaluations were finished by video recordings with the guidance of rehabilitative specialists.
Statistical analysis
Data processing and analysis were performed using R version 4.2.0 (The R Foundation for Statistical Computing, Vienna, Austria). The continuous variables were shown by means with standard deviation (normally distributed), or medians with the first and the third quartile (non-normally distributed). Numbers and percentages were utilized to describe categorical variables. The baseline examination including the chi-square test and Kruskal–Wallis were performed as appropriate, to compare the differences among etiological subgroups (trauma, infection, hypoxia, and others).
The survival time was calculated as the duration between the ABI onset and the eMCS, which was recorded during the follow-up or by the clinical chart. To reveal the survivor pattern of every individual variable, we tested survivor distribution and the cumulative emergence rates using the Kaplan–Meier method. The statistical significance of differences in the survival curves between subgroups was determined by the Log-Rank test.
Finally, unadjusted and adjusted Cox proportional hazards regression analysis was conducted to describe the predictive efficiency of every individual variable over the incidence of eMCS. Basing on the minimum relevant effect size, the sample size for the Cox regression analysis should be 15–20 times of independent variables or more. We extracted 7 independent variables (age of onset, gender, etiology, consciousness state at the rehabilitative admission, the interval between onset and rehabilitative admission, SEP results, and BAEP results), and the minimum sample size of outcome event is 105 to 140. Adjustments were made for gender, age of onset, the interval between onset and rehabilitative admission, etiology, and consciousness state at admission, as appropriate. Differences with a p-value of < 0.05 were considered statistically significant.
Ethics approval and informed consent
This study and all protocols were approved by the Ethics Committee of CHCMU and adhered to all principles of the Declaration of Helsinki. Legal caregivers of participants were given informed consent before their eligibility assessment.
Results
Four hundred and seventeen individuals admitted between 2019 and 2021 were included in the study initially. Thirty-four subjects were excluded according to the criteria. Finally, 383 pediatric individuals with DoC were included (Fig. 1).
Baseline characteristics
The demographic and clinical characteristics of the enrolled participants are shown in Table 1. The data are presented as n (%), median (interquartile range (IQR)). 57.4% of participants were males (n = 220). The median age of injury onset was 3.9 years (IQR: 1.9–7.3 years). The median interval between onset and rehabilitative admission was 30 days (IQR: 21–46 days). During the follow-up period, 240 participants (62.7%) emerged from MCS.
As shown in Table 1, all participants were divided into four etiological subgroups, which were trauma (n = 141 (36.8%)), infection (n = 142 (37.1%)), hypoxia (n = 47 (12.3%)), and the others (n = 53 (13.8%)). Specifically, the other causes consisted of 15 NMDAR-antibody encephalitides, 1 acute disseminated encephalomyelitis (ADEM), 1 stroke from vascular malformation, 4 convulsion-induced brain injury, 2 acute necrotizing encephalopathies (ANE), 9 congenital metabolic disorders, and 21 suspicious infections with pathogen unrevealed. The age distribution of ABI onset showed significant statistical differences across etiological subgroups (P < 0.05), and the hypoxic subgroup showed the youngest onset age (median: 1.9, IQR: 1.3–4.7; P < 0.01) (shown in Table 1). The distribution of gender, the interval between ABI onset and rehabilitative admission, or the consciousness state at admittance showed no significant difference between these four etiological subgroups (P > 0.05).
Of the total 383 participants, 286 (74.67%) underwent SEP tests, and 228 (59.53%) finished BAEP tests within one week of the rehabilitative admission. For both SEP and BAEP, the distribution of gradings showed significant differences among etiological subgroups (P < 0.05); the traumatic subgroup showed a worse BAEP outcome than the hypoxic group (P < 0.01) (Table 1).
Cumulative incidence of emergence from MCS
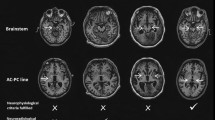
As shown in Fig. 2, the overall consciousness recovery is analyzed by evaluating the cumulative incidence of emergence changes with time. For children with prolonged DoC, the cumulative emerging analyzed in traumatic and non-traumatic subgroups at different months post-onset. KM analysis showed that the cumulative incidence of emergence at months 3, 6, 12, 24, 36 and 48 was 0.510, 0.652, 0.731, 0.784, 0.800 and 0.800 in the traumatic subgroup, and 0.290, 0.418, 0.539, 0.603, 0.644 and 0.692 in the non-traumatic subgroup, respectively. The time of 50% incidence of the emergence was 2.8 months (95% confidence interval (CI) 2.2–4.9) in the TBI subgroup versus 9.2 months (95%CI 6.9–19.1) in the non-TBI subgroup (Fig. 2A,B, n = 383).
Cumulative incidence of emergence from MCS (hereinafter referred as cumulative incidence of eMCS) in the TBI and non-TBI groups. (A & B) show a higher incidence of eMCS in the TBI group in prolonged DoC. (C & D) show a higher incidence of eMCS in the TBI group in PVS. TBI = traumatic brain injury; PVS = persistent vegetative state.
Furthermore, to reveal the natural course of persistent VS (PVS) in children, we repeated the same analysis in 302 PVS participants specifically. For children in a persistent vegetative state (PVS), the cumulative incidence at months in 3, 6, 12, 24, 36 and 48 was testified as 0.439, 0.591, 0.683 and 0.724, 0.743 and 0.743 in the traumatic subgroup, and 0.204, 0.349, 0.469, 0.534, 0.589 and 0.620 in the non-traumatic subgroup. As shown in Fig. 2C,D (n = 302), the time of 50% incidence of emergence occurred in the traumatic and non-traumatic subgroup was 4.5 months (95%CI 2.6–6.1) versus 16.5 months (95%CI 9.1–38.4). The consciousness emergence incidence kept significantly dramatic increasing within 12 months postinjury, regardless of etiological causes. After one year, the cumulative incidence of emerging event showed entering a relative stable phase with slowly increasing, although several subjects had occasionally consciousness recovery.
Affecting factors of consciousness rehabilitation
Kaplan–Meier survival analysis
Age of onset Because the median age of injury onset was 3.9 years (Table 1), we adopted 4 years old as the cutoff point to divide the participants into two subgroups (4 years and older subgroup (≥ 4y), younger than 4 years subgroup (< 4y)). From the Kaplan–Meier analysis, older subgroup showed a significant higher cumulative incidence and speed of consciousness recovery, compared to the < 4 years subgroup (Log-Rank p < 0.001). The time of the 50% cumulative emergence (95%CI) of < 4 years subgroup was 19.9 months (95%CI 7.7–40.3), much longer than 4.4 months (95%CI 3.0–5.6) between 4 years and older subgroup (Fig. 3A).
Kaplan–Meier plot of Cumulative incidence of eMCS in subgroups of different characteristics including age of onset (A), gender (B), etiology (C), time before rehabilitation (D), consciousness state at admission (E) (n = 383). Time to the 50% cumulative incidence of eMCS hereinafter referred as M. CI = confidence interval; NE = Non Existent.
Gender As shown in Fig. 3B, there is no significant difference between genders in cumulative eMCS (LogRank p = 0.68). The time of 50% cumulative emergence incidence (95% CI) for male and female subgroups was 6 months (95%CI 4.9–9.0) versus 5.6 months (95%CI 3.8–9.4).
Etiology Kaplan–Meier analysis showed that statistically significant differences exist in cumulative incidence of emergence among four etiological subgroups listed as traumatic, infection, hypoxia, and the others. The time of 50% emergence between these four subgroups was 2.8 months (95%CI 2.2–4.9), 7.1 months (95%CI 4.6–13.9), 53.6 months (95%CI 19.1-not existence [NE]), and 9.1 months (95%CI 5.2–19.9), respectively, with the global Log-Rank p-value being less than 0.001 (Fig. 3C).
The interval from onset to rehabilitative admission The median interval between ABI onset and rehabilitative admission was 30 days (IQR: 21–46 days). To reveal the association of interval and consciousness recovery, we analyzed the cumulative incidence of eMCS in three subgroups with different interval, which was < 4 weeks, ≥ 4 weeks ~ < 8 weeks and ≥ 8 weeks, respectively. The interval made a significant difference on consciousness recovery, the longer interval connected with poorer consciousness recovery (longer rehabilitation time and lower cumulative incidence of emergence), with the global p-value of Log-Rank test being less than 0.001. The time of 50% emergence (95%CI) was as follows: 2.6 months (95%CI 2.1–4.1) (interval < 4 weeks) versus 7.7 months (95%CI 5.1–9.5) (interval ≥ 4 weeks ~ < 8 weeks), and the 50% survival time for the subgroup of interval ≥ 8 weeks was not existence (NE). (Fig. 3D).
Consciousness state at admission At admission of rehabilitation department, 302 individuals (78.9%) displayed VS/UWS, and the other 81 (21.1%) displayed MCS (Table 1). The time of 50% emergence event (95%CI) for each subgroup was 2.2 months (95%CI 1.9–2.6) (MCS subgroup) versus 9 months (95%CI 6.1–16.6) (VS/UWS subgroup). Besides the much shorter time to 50% emergence event, the cumulative incidence of emerging in MCS subgroup was statistically significant higher in every default time point, comparing with the VS/UWS subgroup; global Log-Rank p < 0.001 (Fig. 3E).
Evoked potentials Of 286 participants took SEP tests, according to the Judson criteria, 104 (36.6%), 29 (10.2%) and 151 (53.2%) individuals were classified as Grade I, II and III, respectively. Of each SEP subgroup, the time to the 50% emergence event was 3.7 months (95%CI 2.6–7.7) for grade I, 5.1 months (95%CI 2.7-NE) for grade II, and 46.4 months (95%CI 24.2-NE) for grade III, respectively. There were significant differences between SEP grading subgroups; the global Log-Rank p < 0.001 (Fig. 4A).
Kaplan–Meier plot of Cumulative incidence of eMCS in subgroups of evoked potentials including somatosensory evoked potential (SEP) grading (A) and brainstem auditory evoked potentials (BAEP) grading (B). Number of cases for SEP and BAEP was 286 and 228 respectively. Abbreviations as in Fig. 3.
Regarding 228 participants who finished BAEP tests, the precent of grade I, II and III according to CANT criteria accounted for 79.4% (n = 181), 13.2% (n = 30) and 7.4% (n = 17), respectively. No significant difference was found across the BAEP grading subgroups in cumulative incidence of emergence; the global Log-Rank p = 0.98. The time to the 50% eMCS was 9.2 months (95%CI 6.4–16.9) for grade I, 6.0 months (95%CI 3.1-NE) for grade II and 5.2 months (95%CI 2.3-NE) for grade III, respectively (Fig. 4B).
Multivariable Cox regression model analysis
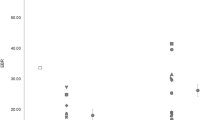
Independent predictors with reduced hazard ratio for consciousness recovery To reveal the effects of all covariates on the event of eMCS, we afterwards processed Cox proportional hazards regression analysis. With the adjusted of the other covariates, five characteristics—namely age of onset, etiology, time before rehabilitative admission, consciousness states at admission (Fig. 5), as well as SEP (Fig. 6)—remained independently responsible for consciousness recovery (p < 0.05).
Multivariate Cox regression analysis for prolonged DoC in children (n = 383). Hazard ratios (HRs) of incident emergence were estimated by Cox proportional hazards regression models adjusted for age of onset, gender, time before rehabilitative admission, consciousness at admission, and etiology. Significant levels: P < 0.05. TBR = time before rehabilitation; CAA = consciousness at admission; HR = hazards ratio. Other abbreviations as in Fig. 3.
Univariate and Multivariate Cox regression analysis of pediatric individuals with prolonged DoC on somatosensory evoked potentials (SEP). *Adjusted for age, time before rehabilitative admission, consciousness at admission, and etiology. Abbreviations as in Fig. 3.
For etiology, hypoxia identified subjects at a lowest incidence of eMCS (HR: 0.366; 95%CI 0.227–0.592; p < 0.001), and infection of central nervous system (CNS) matched a significant lower incidence of emergence (HR: 0.646; 95%CI 0.484–0.834; p = 0.003) comparing with TBI. For the interval between onset and rehabilitative admission, longer time before rehabilitative admission including ≥ 4 ~ < 8 weeks (HR: 0.590; 95%CI 0.453–0.769; p < 0.003), ≥ 8 weeks (HR: 0.179; 95%CI 0.106–0.301; p < 0.001) was associated with significant lower incidence of eMCS. Notably, incidence of emergence in older age subgroup (onset ≥ 4 years; HR: 1.911; 95%CI 1.473–2.478; p < 0.001) was significant higher than that in the younger age subgroup (onset < 4 years). Besides, VS/UWS at admission (HR: 0.395; 95%CI 0.299–0.523; p < 0.001) was associated with lower incidence of emergence (Fig. 5).
To assess the predictive effect of SEP and BAEP results to conscious recovery, we calculated Hazard Ratios (HRs) for the emergence incidence of every evoked potential grading subgroup individually. According to univariate analysis, the SEP grade III which referred as the absence of N20 recognized individuals at lower possibility of eMCS (HR: 0.36; 95%CI 0.261–0.507; p < 0.001), while the SEP grade II referred as CCT delay made no significant difference on the emergence incidence of prolong DoC (HR: 0.911; 95%CI 0.562–1.474; p = 0.703). However, in the adjusted multivariate analysis, conduction delay of SEP was testified an independent negative predictor of emergence (HR: 0.534; 95%CI 0.320–0.891, p = 0.016), as well as the absence of N20 with the even lower hazards ratio (HR: 0.370; 95%CI 0.254–0.539, p < 0.001) (Fig. 6). Simultaneously, the BAEP grading including Grade II (HR: 0.852; 95%CI 0.486–1.492; p = 0.575) and Grade III (HR: 0.870; 95%CI 0.437–1.729; p = 0.69), likely made no significant difference in terms of incidence of eMCS by adjusted multivariate regression analysis (Fig. 7).
Univariate and Multivariate Cox regression analysis of pediatric individuals with prolonged Doc on brainstem evoked potentials (BAEP). *Adjusted for age, time before rehabilitative admission, consciousness at admission, and etiology. Abbreviations as in Fig. 3.
Discussion
This study focused on the investigation of the natural course of prolonged DoC in children, and the potential predictors of conscious recovery after severe acquired brain injury. To our best knowledge, this is the first real-world cohort study to determine the prognosis and the relevant predictive factors of pediatric prolonged DoC with a large study population (n = 383).
Previous studies have reported that TBI is one of the most common etiologies of pediatric DoC25, and infection of the central neurological system is another main cause for individuals younger than 5 years26,27, especially in developing countries and areas28. Similar etiology distributions are observed in our cohort, where TBI and infection of CNS accounted for 36.8% and 37.1%, respectively. Hypoxia brain injury contributes 12.3% as a prominent etiology, especially in younger (median age: 1.9 years; IQR: 1.3–4.7) prolonged DoC. Cerebral vascular injury, which is the most common etiology of prolonged DoC in adults remains little proportion (one stroke in 383) in our cohort.
The natural course of prolonged DoC encompassing the time of emergence and diagnosis of chronic VS/UWS are of particular importance to deliver treatments, which are meaningful for medical strategy and family plan. Because a substantial minority of participants recovered consciousness beyond the preceding time frame (12 months post TBI, 3 months post non-TBI), the 2018 American Academy of Neurology (AAN) practice guideline on DoC replaced permanent VS with the term chronic VS/UWS, which indicates the stability of the condition and a dramatically decreasing likelihood of recovery5. The guidance from the Royal College of Physicians, however, considered that six months post injury was the cut-off point for non-traumatic brain injury to define permanent VS29. However, for children with prolonged DoC, the natural course and prognosis are not well-defined and there is no available evaluation to predict the prognosis accurately to date5. In our cohort, all participants with prolonged DoC experienced remarkable recovery in the first 12 months postinjury, and ongoing recovery after 12 months although at a much lower incidence across etiological groups. Specifically, for the children in persistent VS, the cumulative incidence of eMCS showed the same processing mode, although TBI subgroup showed much faster velocity of emergence incidence than non-TBI subgroup, the both groups have the majority of emerging event incidence within 12 months postinjury. Speculatively, we infer that 12 months is a proper time point to define chronic VS/UWS for pediatric individuals with traumatic and nontraumatic DOC. Additionally, given the substantial frequency of recovery of consciousness beyond 12 months compared to adult individuals, accurate prognostic counseling on pediatric individuals with chronic VS should be provided to educate families and guide treatment decisions, in particular withdrawal of rehabilitative therapy.
Over the follow-up period of as long as nearly 8 years, the traumatic subgroup showed the shortest time of the 50% eMCS at 2.8 months, which is significantly shorter than that of the other three subgroups. Multivariant Cox regression model analysis confirmed that etiology was an independent risk factor to the consciousness recovery of pediatric prolonged DoC. By contrast, nontraumatic etiologies, for whether internal causes including infection of CNS, hypoxia or other undefined etiologies, are proved to be negative factors to consciousness recovery. Out of all etiologies, anoxic brain injury is associated with the worst prognosis in consciousness recovery. Therefore, etiology is a key prognosis indicator of consciousness recovery, which is consistently reported in previous studies1,30,31,32.
Age of onset is reported as an independent factor that affects the prognosis of severe ABI, teenagers and young adults showed better outcomes than the elderly12,32,33,34,35. The common notion was that individuals of young adulthood or childhood gained better recovery due to the assumption of increased neurological plasticity at an early age36. However, several studies showed that the younger age group was associated with a worse prognosis of pediatric DoC37,38,39,40,41. Consistent with previous studies, the present study showed that age younger than 4 years was a negative factor for consciousness recovery, of which the time of the 50% eMCS was 19.9 months, far longer than that of age ≥ 4 years (4.4 months). Moreover, multivariable Cox regression model analysis confirmed that age younger than 4 years was a negative factor for consciousness recovery with significant reduced Hazards Ratio (p < 0.001). Notably, differing from the studies mentioned above based on a single etiology of TBI, we investigated multicausal pediatric DoC and concluded a similarity in the age-dependent outcome. Therefore, early age (< 4 years) at injury is a vulnerability factor for all prolonged DoC rather than TBI only. Age-matched rehabilitation is essential to promote the prognosis and outcome of pediatric prolonged DoC.
Human studies have yielded controversial results on sex effects on the recovery of pediatric DOC. Several preclinical and real-world studies represented significant sex differences in both the response to therapy and the recovery from TBI at all pediatric ages. A cohort study with 16,586 participants with nonpenetrating TBI suggested that, gender made no significant difference on in-hospital mortality rate, total hospital length of stay, and functional outcome15. Similarly, there were no overall difference in mortality rates after TBI between genders in prepubertal and peripubertal age groups. In the post-pubertal group, however, girls showed a reduced mortality rate42,43. The potential mechanism of gender differences may refer to sex hormones. In our study, 220 out of 383 (57.3%) participants are male, there is no significant difference in gender structure across all etiological groups. Moreover, multivariable Cox hazards proportional regression analysis showed that gender is not independently associated with consciousness recovery with HR at 0.99 (p = 0.913), consistent with the study of Pozzi et al. in pediatric ABI40.
Of 383 participants, VS/UWS subgroup identified participants with longer duration of 50% emerging to CS (9 months, n = 302) and a lower cumulative incidence of emergence event. Further, VS/UWS at rehabilitative admission is an independent negative factor for the emergence event compared to MCS (HR = 0.45, P < 0.001). Our finding is consistent with previous clinical prospective studies on DOC10,44,45, indicating that consciousness state at rehabilitative admittance is a clinical prognosis marker. Thus, rigorous assessments of consciousness states at rehabilitative admittance are essential for future prognosis evaluation more than for the following therapy.
Interval between ABI onset and rehabilitation was closely associated with mechanical ventilation, feeding devices, venous access, and other supports which are proceeded in the intensive care unit. In other words, the time before rehabilitation may indicate injury severity. In our study, a shorter time before rehabilitation, in particular, < 4 weeks showed a faster velocity and higher cumulative incidence of consciousness recovery, which is consistent with the previous studies both in childhood and adulthood40. Ultimately, this analysis indicated time before rehabilitation was a strong predictor for the prognosis of prolonged DoC beyond the other variables. Since early rehabilitation improve the prognosis and outcomes of pediatric prolonged DoC, we highly recommend early rehabilitative intervention during the stay of ICU, to promote the rehabilitation of children with DoC as soon as possible46.
Neurophysiological assessments (i.e. electroencephalogram, evoked potentials, event-related potential) have been widely utilized in the clinic. However, the scarcity of available data is focus on the diagnostic and prognostic approaches of prolonged DoC47. In present study, multiple variates COX regression analysis revealed that SEP grading is an independent predictor for consciousness recovery. The higher SEP grading indicated the worse prognosis in children with prolonged DoC (SEP grade 2 HR = 0.522, P = 0.013; SEP grade 3 HR = 0.382, P < 0.001). Furthermore, the absence of cortical potential unilaterally or bilaterally was a strong negative indicator of weak prognosis, which was consistent with the previous study1. BEAP was considered as an ideal clinical indicator to predict the prognosis of adult individuals with prolonged DoC in numerous studies, and the absence of V waves bilaterally was a strong predictor for severe prognosis11,48. From our data, however, the participants with BAEP abnormalities (grade II and III) showed no significant differences compared to the ones with BAEP grade I neither in K-M survival curves (P > 0.05), or in COX hazards proportional regression analysis (grade II HR = 0.80, P = 0.442; grade III HR = 0.77, P = 0.466). The underlying reasons could be as follows: firstly, BAEP reflects the auditory pathway integrity which mainly exists in the brainstem. If the lesion did not involve the brainstem, BAEP would be normal. In our study, the abnormal rate of BAEP was highest in traumatic subgroup, by contrast, none of which existed in the hypoxic subgroup (P < 0.01). Therefore, BAEP is not an accurate indicator of the severity of cerebral injury in pediatric DoC individuals. Secondly, all participants in our study were recruited in the rehabilitation department, the conscious states at admission were VS/UWS or MCS, that meant the function of the brainstem and hypothalamus were relatively preserved. As a result, BAEP results were testified to be normal in most subjects. The individuals with brainstem severe involved may have died as early as in the acute phase. In consequence, we conclude that BAEP abnormalities are not always accompanied by cerebral injuries, either are not recommended to be the prognostic predictor for pediatric in our study with prolonged DoC.
Limitations
The prominent limitation of the study is the assessment of pediatric DoC. For pediatric individuals with prolonged DoC, especially for younger children, skill acquisition is age-related and respectively different, and accurate assessment for young children is extremely difficult. We assigned the assessment task to the experienced doctor, furthermore, reassessments are performed regularly. Thirdly, our study is a single-center study. Song et al. declared in the meta-analysis on the prognosis models of DoC that any single method was at a high risk of misprediction, the integration of multiple technologies in a prediction model may improve the accuracy of the prediction for individuals with DoC19. Next, we are building the prognostic prediction model for pediatric DoC integrating the demographic variables, SEP results, electroencephalogram (EEG), and image results, and conducting external validation in multi-center mode.
Implications
Our finding that more than 50% pediatric individuals with prolonged DoC would emerge from severe disorder of consciousness within 12 months postinjury has important implications for the treatment strategy of prolonged DoC. From our study, the cumulative emerging incidence of prolonged DoC get a continuous progress at 0.510, 0.652, 0.731, 0.784 in the traumatic subgroup, and 0.290, 0.418, 0.539, 0.603 in the non-traumatic subgroup at months 3, 6, 12, 24, respectively. Our study provide a real world reference on the natural course of prolonged DoC. Furthermore, the cumulative emerging incidence of PVS at months 3, 6, 12 and 24 was testified as 0.439, 0.591, 0.683 and 0.724 in the traumatic subgroup, and 0.204, 0.349, 0.469 and 0.534 in the non-traumatic subgroup. That referred pediatric PVS owns a much more promising outcome than that of adults. And in the other word, either 3 months (AAN) or 6 months (European) postinjury to define the chronic VS is not suitable for the children with PVS. According to survive curve, after 1 year postinjury, the cumulative emerging incidence entered a relative stable phase with slowly increasing. We implicated that 1 year, or 2 years post injury is a prefer time to define or diagnosis chronic VS, which is of great value for treatment strategy and help the involved family to make a plan.
Conclusions
In summary, our study revealed for children with prolonged DoC or in persistent VS, the first 12 months postinjury (traumatic or nontraumatic) was a critical time to eMCS. The cumulative emerging incidence is keeping increasing significantly within 12 months of ABI onset. 12 months post injury is a preferred time point to define chronic VS/UWS, and indicates individuals entering stable consciousness condition. The age of onset, etiologies, the consciousness state at the admission of rehabilitation, the interval between onset and rehabilitation, and SEP grade are the independent factors for consciousness recovery. 4 years and older, traumatic etiology, MCS at admission, earlier rehabilitative intervention (< 4 weeks) and normal SEP results are the positive factors for the prognosis. There were no significant differences between genders or BAEP grading subgroups in conscious recovery.
Data availability
Anonymized data are available upon reasonable request by contacting FY.
Abbreviations
- DoC:
-
Disorder of consciousness
- MCS:
-
Minimally conscious state
- CCT:
-
Central somatosensory conductive time
- VS:
-
Vegetative state
- ABI:
-
Acquired brain injury
- AAN:
-
American Academy of Neurology
- CRS-R:
-
The coma recovery scale-revised
- SPECT:
-
Single-Photon Emission Computed Tomography
- TBI:
-
Traumatic brain injury
- SEP:
-
Somatosensory evoked potential
- BAEP:
-
Brainstem auditory evoked potential
- IQR:
-
Interquartile range
- ADEM:
-
Acute disseminated encephalomyelitis
- ANE:
-
Acute necrotizing encephalopathies
- PVS:
-
Persistent vegetative state
- CNS:
-
Central nervous system
- HRs:
-
Hazard ratios
References
Giacino, J. T. et al. Comprehensive systematic review update summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 91(10), 461–470 (2018).
Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state (1). N. Engl. J. Med. 330(21), 1499–1508 (1994).
Laureys, S. et al. Unresponsive wakefulness syndrome: A new name for the vegetative state or apallic syndrome. BMC Med. 8, 68 (2010).
Giacino, J. T. et al. The minimally conscious state: Definition and diagnostic criteria. Neurology 58(3), 349–353 (2002).
Giacino, J. T. et al. Practice guideline update recommendations summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 91(10), 450–460 (2018).
Goss, A. L. & Creutzfeldt, C. J. Prognostication, ethical issues, and palliative care in disorders of consciousness. Neurol. Clin. 40(1), 59–75 (2022).
Molteni, E. et al. Scoping review on the diagnosis, prognosis, and treatment of pediatric disorders of consciousness. Neurology 101(6), e581–e593 (2023).
Liesiene, R., Kevalas, R., Uloziene, I. & Gradauskiene, E. Search for clinical and neurophysiological prognostic patterns of brain coma outcomes in children. Medicina (Kaunas). 44(4), 273–279 (2008).
Abend, N. S. & Licht, D. J. Predicting outcome in children with hypoxic ischemic encephalopathy. Pediatr. Crit. Care Med. 9(1), 32–39 (2008).
Eilander, H. J., Wijnen, V. J., Scheirs, J. G., de Kort, P. L. & Prevo, A. J. Children and young adults in a prolonged unconscious state due to severe brain injury: Outcome after an early intensive neurorehabilitation programme. Brain Inj. 19(6), 425–436 (2005).
Kang, J. et al. A dynamic model to predict long-term outcomes in patients with prolonged disorders of consciousness. Aging (Albany NY). 14(2), 789–799 (2022).
Estraneo, A. et al. Predictors of recovery of responsiveness in prolonged anoxic vegetative state. Neurology 80(5), 464–470 (2013).
Carrai, R., Grippo, A., Lori, S., Pinto, F. & Amantini, A. Prognostic value of somatosensory evoked potentials in comatose children: A systematic literature review. Intensive Care Med. 36(7), 1112–1126 (2010).
Faugeras, F. et al. Survival and consciousness recovery are better in the minimally conscious state than in the vegetative state. Brain Inj. 32(1), 72–77 (2018).
Morrison, W. E., Arbelaez, J. J., Fackler, J. C., De Maio, A. & Paidas, C. N. Gender and age effects on outcome after pediatric traumatic brain injury. Pediatr. Crit. Care Med. 5(2), 145–151 (2004).
Keenan, H. T., Clark, A. E., Holubkov, R., Cox, C. S. Jr. & Ewing-Cobbs, L. Trajectories of children’s executive function after traumatic brain injury. JAMA Netw. Open 4(3), e212624 (2021).
Valera, E. M. et al. Understanding traumatic brain injury in females: a state-of-the-art summary and future directions. J. Head Trauma Rehabil. 36(1), E1–E17 (2021).
Gupte, R., Brooks, W., Vukas, R., Pierce, J. & Harris, J. Sex differences in traumatic brain injury: What we know and what we should know. J. Neurotrauma. 36(22), 3063–3091 (2019).
Song, M. et al. Prognostic models for prolonged disorders of consciousness: An integrative review. Cell Mol. Life Sci. 77(20), 3945–3961 (2020).
Bernat, J. L. Chronic disorders of consciousness. Lancet 367(9517), 1181–1192 (2006).
Bruno, M. A., Vanhaudenhuyse, A., Thibaut, A., Moonen, G. & Laureys, S. From unresponsive wakefulness to minimally conscious PLUS and functional locked-in syndromes: Recent advances in our understanding of disorders of consciousness. J. Neurol. 258(7), 1373–1384 (2011).
Alvarez, G., Suskauer, S. J. & Slomine, B. Clinical features of disorders of consciousness in young children. Arch. Phys. Med. Rehabil. 100(4), 687–694 (2019).
Judson, J. A., Cant, B. R. & Shaw, N. A. Early prediction of outcome from cerebral trauma by somatosensory evoked potentials. Crit. Care Med. 18(4), 363–368 (1990).
Cant, B. R., Hume, A. L., Judson, J. A. & Shaw, N. A. The assessment of severe head injury by short-latency somatosensory and brain-stem auditory evoked potentials. Electroencephalogr. Clin. Neurophysiol. 65(3), 188–195 (1986).
Molteni, E. et al. Joint neuropsychological assessment through coma/near coma and level of cognitive functioning assessment scales reduces negative findings in pediatric disorders of consciousness. Brain Sci. 10(3), 162 (2020).
Bale, J. F. Jr. Virus and immune-mediated encephalitides: Epidemiology, diagnosis, treatment, and prevention. Pediatr. Neurol. 53(1), 3–12 (2015).
Wong, C. P., Forsyth, R. J., Kelly, T. P. & Eyre, J. A. Incidence, aetiology, and outcome of non-traumatic coma: A population based study. Arch. Dis. Child 84(3), 193–199 (2001).
Collaborators, G. B. D. N. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18(5), 459–480 (2019).
Working Party of the Royal College of P. The vegetative state: guidance on diagnosis and management. Clin. Med. (Lond) 3(3), 249–254 (2003).
Shaklai, S., Peretz, R., Spasser, R., Simantov, M. & Groswasser, Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain Inj. 28(7), 915–921 (2014).
Estraneo, A. et al. Multi-center study on overall clinical complexity of patients with prolonged disorders of consciousness of different etiologies. Brain Inj. 35(1), 1–7 (2021).
Nekrasova, J. et al. One-Year demographical and clinical indices of patients with chronic disorders of consciousness. Brain Sci. 11(5), 651 (2021).
Kowalski, R. G. et al. Recovery of consciousness and functional outcome in moderate and severe traumatic brain injury. JAMA Neurol. 78(5), 548–557 (2021).
Groswasser, Z., Cohen, M. & Costeff, H. Rehabilitation outcome after anoxic brain damage. Arch. Phys. Med. Rehabil. 70(3), 186–188 (1989).
Andruszkow, H. et al. Physical and psychological long-term outcome after traumatic brain injury in children and adult patients. Health Qual. Life Outcomes 12, 26 (2014).
Gutchess, A. Plasticity of the aging brain: New directions in cognitive neuroscience. Science 346(6209), 579–582 (2014).
Levin, H. S. et al. Severe head injury in children: Experience of the traumatic coma data bank. Neurosurgery 31(3), 435–443 (1992).
Freeman, S. S., Udomphorn, Y., Armstead, W. M., Fisk, D. M. & Vavilala, M. S. Young age as a risk factor for impaired cerebral autoregulation after moderate to severe pediatric traumatic brain injury. Anesthesiology 108(4), 588–595 (2008).
Chapman, S. B., Max, J. E., Gamino, J. F., McGlothlin, J. H. & Cliff, S. N. Discourse plasticity in children after stroke: Age at injury and lesion effects. Pediatr. Neurol. 29(1), 34–41 (2003).
Pozzi, M. et al. Severe acquired brain injury aetiologies, early clinical factors, and rehabilitation outcomes: A retrospective study on pediatric patients in rehabilitation. Brain Inj. 33(12), 1522–1528 (2019).
Lang, S. S. et al. Trajectory of long-term outcome in severe pediatric diffuse axonal injury: An exploratory study. Front. Neurol. 12, 704576 (2021).
Ley, E. J. et al. Gender impacts mortality after traumatic brain injury in teenagers. J. Trauma Acute Care Surg. 75(4), 682–686 (2013).
Phelan, H. A. et al. Use of a pediatric cohort to examine gender and sex hormone influences on outcome after trauma. J. Trauma. 63(5), 1127–1131 (2007).
Rodgin, S. et al. Very long-term outcomes in children admitted in a disorder of consciousness after severe traumatic brain injury. Arch. Phys. Med. Rehabil. 102(8), 1507–1513 (2021).
Chen, W. G. et al. Recovery from prolonged disorders of consciousness: A dual-center prospective cohort study in China. World J. Clin. Cases. 8(12), 2520–2529 (2020).
Zhang, T. et al. Implementation of early rehabilitation for critically ill children in China: A survey and narrative review of the literature. Front. Pediatr. 10, 941669 (2022).
Vitello, M. M. et al. Neuroimaging and neurophysiological diagnosis and prognosis in paediatric disorders of consciousness. Dev. Med. Child Neurol. 64(6), 681–690 (2022).
Hall, J. W. 3rd., Huang-fu, M. & Gennarelli, T. A. Auditory function in acute severe head injury. Laryngoscope 92(8 Pt 1), 883–890 (1982).
Acknowledgements
We thank Mengjia Gong for assisting and coordinating the project.
Funding
This study was supported by the Science-Health Joint Medical Scientific Research Project of Chongqing (No. 2023MSXM144) and the Youth Basic Research Project from the Ministry of Education Key Laboratory of Child Development and Disorders (No. YBRP-202106).
Author information
Authors and Affiliations
Contributions
D.X.L.: Conceptualization, Methodology, Investigation, Analysis, Interpretation, Writing, Funding Acquisition. F.Y.: Methodology, investigation, analysis, supervision. X.N.: Conceptualization, Methodology, Supervision, Writing. Z.T.: Investigation, Writing. C.Y.X.: Investigation, Interpretation. H.X.Q.: Investigation, Interpretation. H.Q.Y.: Neurological electrophysiology performing. L.T.S.: Investigation, Interpretation. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Legal caregivers of Participants were given informed consent for publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Duan, X., Zhang, T., Chen, Y. et al. Natural course and predictors of consciousness recovery in children with prolonged disorder of consciousness. Sci Rep 14, 17417 (2024). https://doi.org/10.1038/s41598-024-68370-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68370-2