Abstract
Systemic inflammation generally coexists with functional limitations that seriously affect quality of life. This study aimed to investigate the association between systemic inflammation in midlife and the risk of functional limitations in late-life. A total of 10,044 participants with an average age of 53.9 ± 5.7 years at baseline were included in a cohort study. At the last follow-up, the prevalence of impaired activities of daily living (ADLs), instrumental activities of daily living (IADLs), and lower extremity function (LEF) was 14.7%, 21.6%, and 50.3%, respectively. The values of four inflammatory biomarkers were used to calculate the inflammation composite score. Compared with the participants in the lowest quartile of the inflammation composite score (Q1), those in the highest quartile (Q4) exhibited an odds ratio (OR) of 1.589 and a 95% confidence interval (CI) of 1.335–1.892 for impaired ADLs, an OR of 1.426 and a 95% CI of 1.228–1.657 for impaired IADLs, and an OR of 1.728 and a 95% CI of 1.526–1.957 for impaired LEF. The association between systemic inflammation and functional limitations was partly mediated by cardiac and brain function. The present study provides evidence that systemic inflammation in midlife is associated with a higher risk of late-life functional limitations. Protecting vital organ functions in midlife may have a positive impact on reducing the risk of future functional limitations.
Trial registration: www.clinicaltrials.gov; Unique identifier: NCT00005131.
Similar content being viewed by others
Introduction
Functional limitations are defined as basic age-related physical dysfunction. Functional limitations include the ability to carry out self-care and domestic life activities, athletic ability and the ability to participate in social labor1. In United States, approximately 20–30% of adults aged 60–69 have one or more functional limitations, while the proportion of adults aged 80 and above increases 2-fold2,3. The number of the elderly with functional limitations will continue to increase with aging. Functional limitations are considered as a major precursor of disability4,5, imposing a heavy burden on late-life quality of individuals and public healthcare services6. Functional limitations have been widely shown to be a key prognostic determinant of adverse outcomes7,8,9. Therefore, we have an urgent front-burner to predict and prevent functional limitations, and find modifiable risk factors for targeted intervention.
Systemic inflammation refers to inflammation caused by infectious or non-infectious injury that can not be locally restricted by organisms10. Systemic inflammation and functional limitations share the common risk factors and pathophysiological pathways. It is widely accepted to use biomarkers of peripheral blood to describe the state of systemic inflammation. Several cross-sectional studies reported that high-level peripheral inflammatory biomarkers commonly coexists with functional limitations11,12. Moreover, prospective studies have found that high-level peripheral inflammatory biomarkers were associated with functional limitations in the elderly13,14. However, these studies were designed as cross-sectional studies or exhibited a short follow-up time. And advanced age interacts with high-level inflammatory biomarkers and a high incidence of functional limitations, which make these association can not well established. Moreover, previous studies only evaluate inflammation by single biomarkers, which could not accurately reflect the systemic inflammation status. Therefore, this study used composite biomarkers from the middle-aged populations to elucidate the causal relationship between inflammation.
A slew of studies have shown that several important inflammatory pathways are involved in the aging and injury of various organs15,16, suggesting that inflammation may lead to impairment of physical functions by damaging organ function. Systemic inflammation may lead to diseases of important organs, such as the heart, brain, lungs, liver, and kidneys17,18. Previous studies have demonstrated that cardiac function has been independently associated with functional limitations and disability and that brain function may be a stronger predictor19,20,21,22. The relationship between other systemic diseases and functional limitations has not been proven to be independent. However, several studies have shown that respiratory insufficiency is associated with limited activity and limited walking capacity23,24. Other studies have reported that patients with liver disease may experience motor incoordination and impaired cognitive function through the neuroinflammatory pathway25,26. Additional studies have reported that kidney function is associated with worse daily activity function and cognitive performance27,28. However, few studies have comprehensively explored the impact of organ function impairment on the pathways in which inflammation leads to physical functional limitations. To fill this research gap, we aimed to explore the association between mid-life systemic inflammation and late-life functional limitations and whether this association is mediated by organ function impairment.
Methods
Study design and population
This was a secondary analysis of data from the Atherosclerosis Risk in Communities (ARIC) study29. Data were obtained from the public database of the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository Information Coordinating Center(https://biolincc.nhlbi.nih.gov/home/).
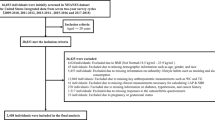
A total of 15,792 participants aged 45–64 years were recruited from 1987 to 1989 (Visit 1) and followed up every three years. Visit 2 was conducted in 1990–1992, Visit 3 in 1993–1995 and Visit 4 in 1996–1998. The ARIC study was approved by the institutional review committee of all participating institutions with the informed consent from all participants. Visit 1 was regarded as the baseline and Visit 4 as the research outcome. Some of the data were collected during Visit 2, and functional limitations were assessed for the first time in Visit 4. Among the potential participants presenting at Visit 4 (n = 15,028), the exclusion criteria were as follows: absence of an inflammatory biomarker assessment (n = 336), absence of one or more covariates (n = 1111), and absence of an assessment of functional limitations (n = 3537). After the exclusion of participants who met one of the exclusion criteria, a total of 10,044 participants remained for enrollment in the study.
Inflammatory biomarkers
The physiological response of biomarkers to stress varies across individuals. One biomarker may be compensated by the effective function of other regions and may not accurately describe the overall physiological function and the body’s response to stress30. As a single measurement may not adequately capture inflammation chronicity, inflammation composite scores are used to avoid this risk. In this study, four biomarkers in plasma collected from Visit 1 were used to describe the state of systemic inflammation, including white blood cell count (log-transformed to correct skewness), von Willebrand factor, fibrinogen and factor VIII. The inflammation composite score refers to the average value of four biomarkers after standardization to a Z-score. These markers were proinflammatory cytokines whose selection was largely dependent on their availability in the ARIC study. These markers had often been used in the inflammation composite score in other studies31.
In this study, hypersensitive-C-reactive protein (hs-CRP), an acute phase protein whose synthesis is regulated by proinflammatory cytokines32, was measured in blood samples taken during Visits 1 and 2. There was no difference between the relevant conditions of the two measurements. Adding it to the inflammation composite score have led to an overlap of the effects, and therefore it was analyzed as a sub-indicator of systemic inflammation. The hs-CRP level was classified as “low” or “elevated” using a cutoff value of 3.0 mg/L33. According to the hs-CRP values measured from Visit 1 to Visit 2, the following four longitudinal patterns of change were established: (1) Consistent low hs-CRP: initial and final levels were at low levels; (2) Ascending hs-CRP: levels were initially at low levels and then at elevated levels; (3) Descending hs-CRP: levels were initially at elevated levels and then at low levels; (4) Consistent elevated hs-CRP: initial and final levels were at elevated levels.
Functional limitations
At Visit 4, the functional status assessment was completed in the form of a self-reported questionnaire containing designated activities, as was performed in the third National Health and Nutrition Examination Survey4. These activities included activities of daily living (ADLs), which included eating, dressing, arising in the morning, and walking34; instrumental activities of daily living (IADLs), which included cooking, housework, and financial management35; and lower-extremity function (LEF), which included standing up from a chair without arm support, bending, kneeling, walking one-quarter mile, walking upstairs, and carrying 10 pounds36. Participants were required to indicate the level of difficulty in conducting these activities. When participants could not answer for themselves, participant proxies could answer for them with a high degree of reliability. The final result was reported as "no limits" (i.e., no difficulty with any activity) or "function impaired" (i.e., any difficulty with any activity) for each of the three categories. Any difficulty in any of the three categories of functional limitations was defined as impaired ADLs, IADLs, or LEF.
Assessment of multiple organ functions
Organ function was assessed at Visit 4, including cardiac function, brain function, lung function, liver function, and kidney function. Cardiac function was assessed by measuring the level of N-Terminal Pro-Brain Natriuretic Peptide (NT-proBNP) in plasma using electrochemiluminescence immunoassay on an automatic Cobase 411 Analyzer (Roche Diagnosis, Florham Park, NJ, USA). Brain function was assessed using the global composite cognitive score, including the delayed word recall test (DWRT), digit symbol substitution test (DSST), and word fluency test (WFT). The composite cognitive score was the average value of the three tests after standardization to a Z-score37,38,39,40. Lung function was assessed using the ratio of forced expiratory volume in one second/forced vital capacity (FEV1/FVC). The values were measured by the standardized Collins Survey II spirometer41. Liver function was assessed by measuring the plasma alaninetransaminase (ALT) level. Kidney function was assessed by calculating the estimated glomerular filtration rate (eGFR) using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) Eqs. 42.
Baseline covariates
At baseline, the following covariates were assessed based on self-report or medical record evidence: age, gender, race, income, education, hours of the metabolic equivalent of task (MET-hour) per week, the prevalence of medical comorbidities (hypertension, diabetes, coronary heart disease, heart failure, cancer, and chronic obstructive pulmonary disease), and medication use. Total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG) were measured by enzymatic analysis.
Hypertension was defined as blood pressure ≥ 140/90 mmHg or a history of medication use. Diabetes was defined as fasting glucose ≥ 126.0 mg/dl, non-fasting glucose ≥ 200.0 mg/dl, or a history of medication use or insulin therapy. Coronary heart disease was defined as acute coronary syndrome, chronic coronary artery disease, or a history of medication use or coronary revascularization. Chronic obstructive pulmonary disease was identified as FEV1/FVC < 70% after bronchodilator use or a history of medication use. Heart failure and cancer were diagnosed based on evidence from medical records.
Statistical analysis
In this study, continuous variables were represented as medians (25–75th) or means ± standard deviations, and categorical variables were represented with frequency counts (percentages). Continuous variables were compared using the Mann–Whitney U test or ANOVA, and categorical variables were compared using Chi-square test.
Logistic regression models were developed to assess the association between the inflammation composite score at Visit 1, hs-CRP level at Visit 1, and the longitudinal pattern of hs-CRP level from Visit 1 to Visit 2 with functional limitations (impaired ADLs, IADLs, and LEF). Two regression models were established to examine the independent role of these relationships. Model 1 was adjusted according to age, gender, race, education, income, and MET-hour/week. Model 2 was additionally adjusted according to the prevalence of hypertension, diabetes, coronary heart disease, heart failure, cancer, and chronic obstructive pulmonary disease; TC, HDL-C, LDL-C, and TG levels; and cholesterol-lowering and anti-inflammatory medication use. A logistic regression analysis was also developed in Model 2 to assess the effect modification between the inflammation composite score and the functional limitations of age, gender, and race subgroups. The multiplicative interaction term < 0.05 was considered statistically significant.
According to the procedure recommended by Hayes43, pathway analysis was conducted using the structural equation Model 4 to calculate the indirect effects of the inflammation composite score on functional limitations, including cardiac function (NT-proBNP level log-transformed to correct for skewness), brain function (composite cognitive score), lung function (FEV1/FVC), liver function (ALT level), and kidney function (eGFR). In structural equation Model 4, cross-products from estimated mediation effects were considered statistically significant when confidence intervals (CIs) did not include zero. Standardized regression coefficients (β) were used to report point estimates of direct and indirect effects. The mediation percentage was obtained by calculating the ratio of the indirect effect to the total effect, thereby quantifying the size of the mediation effect. The significance of the mediation effect was tested using Bootstrap sampling (times = 1000).
A two-tailed P value of < 0.05 was considered statistically significant. SPSS Statistics (version 36.0, IBM Corp, Armonk, USA), PROCESS (version 3.5 for SPSS) and R software (version 3.5.0, Vienna, Austria) were used for data analysis.
Ethical statement
This study was conducted in conformity to the Declaration of Helsinki and was approved by the Human Ethical Committee of West China Hospital of Sichuan University. The ARIC study was approved by the institutional review committee of all participating institutions with the informed consent from all participants.
Results
Baseline characteristics
The 10,044 participants with an average age of 53.9 ± 5.7 years were categorized into quartiles (Q1, Q2, Q3, and Q4) based on their inflammation composite score. Table 1 shows the baseline participant characteristics. Increased inflammation composite score was associated with older age; female; African American (still lower than Caucasians); lower income and education levels; unhealthy behaviors; higher TC, LDL-C, TG, creatinine, and blood glucose levels; and higher odds of medical comorbidities (p < 0.001 for all).
Inflammation and functional limitations
At Visit 4, the prevalence of impaired ADLs, IADLs, and LEF was 14.7%, 21.6%, and 50.3%, respectively. The higher the inflammation composite score at Visit 1, the higher the risk of having functional limitations at Visit 4 (p < 0.001; Fig. 1).
As shown in Table 2, in the unadjusted logistic regression model, Q2, Q3, and Q4 all showed higher odds of impaired ADLs, IADLs, and LEF compared with Q1. The strength of the correlation was reduced in the adjusted logistic regression model but remained significant. In the adjusted logistic regression Model 2, compared with Q1, which had the lowest inflammation composite score, Q2 exhibited higher odds of impaired ADLs (odds ratio [OR] = 1.212, 95% CI: 1.013–1.450, p = 0.036), impaired IADLs (OR = 1.238, 95% CI 1.065–1.439, p = 0.005), and impaired LEF (OR = 1.271, 95% CI 1.129–1.431, p < 0.001). Q3 also exhibited higher odds of impaired ADLs (OR = 1.319, 95% CI 1.105–1.574, p = 0.002), impaired IADLs (OR = 1.135, 95% CI 0.975–1.321, p = 0.104), and impaired LEF (OR = 1.489, 95% CI: 1.321– 1.679, p < 0.001) compared with Q1, as did Q4 (impaired ADLs: OR = 1.589, 95% CI 1.335–1.892, p < 0.001; impaired IADLs: OR = 1.426, 95% CI 1.228–1.657, p < 0.001; impaired LEF: OR = 1.728, 95% CI 1.526–1.957, p < 0.001). Notably, the OR of impaired ADLs and impaired LEF showed a gradual upward trend with an increase in inflammation composite score.
As shown in Fig. 2, in the unadjusted logistic regression model, participants with elevated hs-CRP levels at Visit 1 showed higher odds of impaired ADLs, impaired IADLs, and impaired LEF compared with those with low hs-CRP levels at Visit 1. The strength of the correlation was reduced in the adjusted logistic regression model but remained significant. In the adjusted logistic regression Model 2, compared with having low hs-CRP levels at Visit 1, having elevated hs-CRP levels at Visit 1 was associated with higher odds of impaired ADLs (OR = 2.076, 95% CI 1.829–2.357, p < 0.001), impaired IADLs (OR = 1.741, 95% CI 1.561–1.941, p < 0.001), and impaired LEF (OR = 1.884, 95% CI 1.719–2.066, p < 0.001).
Unadjusted and adjusted odds ratios (OR) for the association between elevated hs-CRP levels and impaired activities of daily living (ADLs), instrumental ADLs (IADLs), and lower-extremity function (LEF) compared with low hs-CRP levels. Model 1: adjusted by age, sex, race, education (< high school, high school, or > high school), annual household income (< 16 000, 16 000 to 35 000, > 35 000), and physical activity defined by MET-hour/week. Model 2: adjusted by model 1 plus, prevalent of hypertension, diabetes, coronary heart disease, heart failure, cancer, chronic obstructive pulmonary disease, total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides, cholesterol-lowering and anti-inflammatory medication use.
Furthermore, longitudinal pattern of changes in hs-CRP affected late-life functional limitations. In the adjusted logistic regression model, compared with participants with consistent low hs-CRP levels, participants with ascending hs-CRP levels, descending hs-CRP levels, and consistent elevated hs-CRP levels had a higher risk of having functional limitations (Fig. 3).
Adjusted probability of impaired (A) activities of daily living (ADLs), (B) instrumental ADLs (IADLs), and (C) lower-extremity function (LEF) based on longitudinal pattern of changes in hs-CRP levels. Model was adjusted by age, sex, race, education (< high school, high school, or > high school), annual household income (< 16, 000, 16, 000 to 35, 000, > 35, 000), physical activity defined by MET-hour/week, prevalent of hypertension, diabetes, coronary heart disease, heart failure, cancer, chronic obstructive pulmonary disease, total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides, cholesterol-lowering and anti-inflammatory medication use. *p < 0.05, **p < 0.001 compared to the consistent low hs-CRP group.
Subgroup analysis
Figure 4 shows the significant interaction between races (p for interaction: 0.016, 0.004 and 0.037, respectively). Compared with African Americans, Caucasians had a higher risk of mid-life inflammation composite score associated with late-life functional limitations. For participants aged < 54 years, the inflammation composite score revealed a significantly higher risk associated with impaired LEF (p for interaction = 0.002) and a higher but not significant risk associated with impaired ADLs (p for interaction = 0.059). The association between inflammation composite score and functional limitations was consistent among the gender subgroups (p for interaction > 0.05).
Adjusted odds ratios (OR) for the association of inflammation composite score with impaired activities of daily living (ADLs), instrumental ADLs (IADLs), and lower-extremity function (LEF) in different subgroups. Model was adjusted by age, sex, race, education (< high school, high school, or > high school), annual household income (< 16, 000, 16, 000 to 35 000, > 35, 000), physical activity defined by MET-hour/week, prevalent of hypertension, diabetes, coronary heart disease, heart failure, cancer, chronic obstructive pulmonary disease, total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides, cholesterol-lowering and anti-inflammatory medication use.
Path analysis
The mean NT-proBNP level was 216.5 ± 424.3 pg/ml, the mean composite cognitive score was − 0.3 ± 0.8, the mean FEV1/FVC was 74.6 ± 7.6%, the mean ALT level was 16.7 ± 10.8 U/L, and the mean eGFR was 85.4 ± 17.5 ml/min/1.73 m2. Path analysis showed that the inflammation composite score and functional limitations were significantly associated with NT-proBNP level and composite cognitive score (p < 0.01). FEV1/FVC, ALT and eGFR were not found to be mediators. Table 3 shows the pathway estimates and 95% CIs of the mediation model. Figure 5 shows that the effects of the inflammation composite score on the impairment of ADLs, IADLs, and LEF were partly mediated by the NT-proBNP level (5.8%, 9.3%, and 7.2%, respectively) and composite cognitive score (19.5%, 28.2%, and 14.3%, respectively).
Discussion
In this study, participants with a higher level of mid-life systemic inflammation exhibited a gradually increasing risk of late-life functional limitations. Specifically, having a higher inflammation composite score was associated with a 40–70% increased risk of adverse outcomes, and having a higher hs-CRP level was associated with a nearly two-fold increased risk of late-life functional limitations. These findings provide support for the role of systemic inflammation in late-life functional limitations.
The biomarkers measured in the current study are considered reactants involved in peripheral inflammatory signaling. However, von Willebrand factor, fibrinogen, and factor VIII are also involved in other overlapping biological pathways, including hemostasis and clotting, which may also affect physical function44,45, possibly leading to an overestimation of their contribution to systemic inflammation. However, this possibility was mitigated using the hs-CRP level as a sub-indicator, which is a more specific acute-phase reactant for peripheral inflammatory signaling46.
The pattern of consistently elevated or increasing or descending hs-CRP levels was associated with an increased probability of functional limitations compared with consistently low levels. Participants who had elevated hs-CRP levels for 3 years were at the greatest risk, followed by individuals with initially low hs-CRP levels that subsequently became and remained elevated as shown when measured at 3 years. These findings support the hypothesis that long-term inflammation is associated with functional limitations47,48. Furthermore, in addition to existing systemic inflammation, underlying long-term inflammation may play a role in the development of physiological functional limitations49.
Subgroup analysis demonstrated that the association between inflammation composite score and functional limitations was consistent irrespective of gender. However, this association was stronger among Caucasians than African Americans. There has been little research into the underlying factors that contribute to functional limitations caused by inflammation in African Americans. Racial differences in the regulation of inflammatory signaling pathways50; chronic disease burden; and non-physiological factors, such as socioeconomic status, healthcare access, and healthcare affordability51, may explain the race-based differences observed in this study. More importantly, systemic inflammation at a relatively young age was associated with a higher risk of functional limitations, suggesting that early exposure to systemic inflammation may be associated with a higher risk of functional limitations. Furthermore, the morbidity of multiple chronic diseases showed an accelerated trend in midlife. Adjusting for medical comorbidities had a strongly weakening effect on the association between systemic inflammation and functional limitations. These findings indicate that mid-life inflammation may be an important common biological mechanism of late-life multimorbidity and functional limitations52.
According to our findings, the increased risk of functional limitations associated with systemic inflammation is mediated by cardiac and brain function. The lungs, liver, and kidneys were not observed to be involved in this pathway. Indirect effects mediated by cardiac function and brain function accounted for 5–10% and 14–28%, respectively, of this pathway. In general, systemic inflammation may partially cause functional limitations through the heart and brain. There is currently no specific prevention and treatment strategy for functional limitations, but the findings of our study may provide some options. Treatments with specific strategies to improve cardiac and brain function may be associated with a 5.8% and 19.5% improvement in ADLs, a 9.3% and 28.2% improvement in IADLs, and a 7.2% and 14.3% improvement in LEF, respectively. This suggested that researchers can consider formulating prevention programs to protect the important organ functions of middle-aged patients with systemic inflammation, which may have a positive impact on reducing the risk of functional limitations in late-life.
Limitations
There are several limitations in this study. First, functional impaired status in the study was measured only at Visit 4 and not at baseline, and thus cannot demonstrate causality. Second, the midlife hs-CRP pattern from Visit 1 to visit 2 was not fully representative of the overall follow-up trend. Third, the assessment of each organ (NT-proBNP, the global composite cognitive score, FEV1/FVC, ALT and eGFR) cannot fully reflect the contribution of their respective organ function. Fourth, in pathway analysis, only the effects of vital organ function have been studied without assessing the motor system, which may account for a certain proportion of the pathway.
Conclusions
The findings of this study provide evidence that individuals with mid-life systemic inflammation are at increased risk of late-life functional limitations. The association was partly mediated by cardiac and brain function and was stronger among Caucasians and those of relatively younger ages. Protecting vital organ functions in midlife may have a positive impact on reducing the risk of future functional limitations.
Data availability
Data of this study was obtained from the public database of National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository Information Coordinating Center (https://biolincc.nhlbi.nih.gov/home/).
References
Freedman, V. A. Adopting the ICF language for studying late-life disability: A field of dreams?. J. Gerontol. A Biol. Sci. Med. Sci. 64, 1172–1174 (2009).
Holmes, J., Powell-Griner, E., Lethbridge-Cejku, M. & Heyman, K. Aging differently: Physical limitations among adults aged 50 years and over: United States, 2001–2007. NCHS Data Brief, 1–8 (2009).
Ervin, R. B. Prevalence of functional limitations among adults 60 years of age and over: United States, 1999–2002. Adv. Data (375), 1–7 (2006). https://stacks.cdc.gov/view/cdc/84014/cdc_84014_DS1.pdf
Ostchega, Y., Harris, T. B., Hirsch, R., Parsons, V. L. & Kington, R. The prevalence of functional limitations and disability in older persons in the US: Data from the national health and nutrition examination survey III. J. Am. Geriatr. Soc. 48, 1132–1135 (2000).
Jette, A. M. Toward a common language of disablement. J. Gerontol. A Biol. Sci. Med. Sci. 64, 1165–1168 (2009).
Bentley, J. P. et al. Functional status, life-space mobility, and quality of life: A longitudinal mediation analysis. Qual. Life Res. 22, 1621–1632 (2013).
McCusker, J., Kakuma, R. & Abrahamowicz, M. Predictors of functional decline in hospitalized elderly patients: A systematic review. J. Gerontol. A Biol. Sci. Med. Sci. 57, M569-577 (2002).
Rozzini, R. et al. Relationship between functional loss before hospital admission and mortality in elderly persons with medical illness. J. Gerontol. A Biol. Sci. Med. Sci. 60, 1180–1183 (2005).
Koroukian, S. M. et al. Combinations of chronic conditions, functional limitations, and geriatric syndromes that predict health outcomes. J. Gen. Intern. Med. 31, 630–637 (2016).
Marker-Hermann, E. Systemic inflammation. Internist 54, 397–398 (2013).
Cohen, H. J., Pieper, C. F., Harris, T., Rao, K. M. & Currie, M. S. The association of plasma IL-6 levels with functional disability in community-dwelling elderly. J. Gerontol. A Biol. Sci. Med. Sci. 52, M201-208 (1997).
Ferrucci, L. et al. Serum IL-6 level and the development of disability in older persons. J. Am. Geriatr. Soc. 47, 639–646 (1999).
Penninx, B. W. et al. Inflammatory markers and incident mobility limitation in the elderly. J. Am. Geriatr. Soc. 52, 1105–1113 (2004).
Pieper, C. F., Rao, K. M., Currie, M. S., Harris, T. B. & Cohen, H. J. Age, functional status, and racial differences in plasma D-dimer levels in community-dwelling elderly persons. J. Gerontol. A Biol. Sci. Med. Sci. 55, M649-657 (2000).
McGeer, P. L. & McGeer, E. G. Inflammation and the degenerative diseases of aging. Ann. N. Y. Acad. Sci. 1035, 104–116 (2004).
Prasad, S., Sung, B. & Aggarwal, B. B. Age-associated chronic diseases require age-old medicine: Role of chronic inflammation. Prev. Med. 54(Suppl), S29-37 (2012).
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832 (2019).
Liberale, L. et al. Inflammation, aging, and cardiovascular disease: JACC review topic of the week. J. Am. Coll. Cardiol. 79, 837–847 (2022).
Dodge, H. H. et al. Cognitive impairment as a strong predictor of incident disability in specific ADL-IADL tasks among community-dwelling elders: The Azuchi study. Gerontologist 45, 222–230 (2005).
Stuck, A. E. et al. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc. Sci. Med. 48, 445–469 (1999).
Kelly-Hayes, M., Jette, A. M., Wolf, P. A., D’Agostino, R. B. & Odell, P. M. Functional limitations and disability among elders in the Framingham study. Am. J. Publ. Health 82, 841–845 (1992).
Tas, U. et al. Incidence and risk factors of disability in the elderly: The Rotterdam study. Prev. Med. 44, 272–278 (2007).
Berkman, L. F. et al. High, usual and impaired functioning in community-dwelling older men and women: Findings from the MacArthur foundation research network on successful aging. J. Clin. Epidemiol. 46(10), 1129–1140 (1993).
Vermeulen, F., Garcia, G., Ninane, V. & Laveneziana, P. Activity limitation and exertional dyspnea in adult asthmatic patients: What do we know?. Respir. Med. 117, 122–130 (2016).
Llansola, M. et al. Neuroinflammation alters GABAergic neurotransmission in hyperammonemia and hepatic encephalopathy, leading to motor incoordination. Mech. Ther. Implications. Front. Pharmacol. 15, 1358323 (2024).
Cabrera-Pastor, A. et al. Peripheral inflammation induces neuroinflammation that alters neurotransmission and cognitive and motor function in hepatic encephalopathy: Underlying mechanisms and therapeutic implications. Acta Physiol. 226(2), e13270 (2019).
Wang, M. et al. Kidney function and dementia risk in community-dwelling older adults: The Shanghai aging study. Alzheimers. Res. Ther. 13(1), 21 (2021).
Clarkson, M. J., Bennett, P. N., Fraser, S. F. & Warmington, S. A. Exercise interventions for improving objective physical function in patients with end-stage kidney disease on dialysis: A systematic review and meta-analysis. Am. J. Physiol. Renal. Physiol. 316(5), F856–F872 (2019).
design and objectives. The Atherosclerosis risk in communities (ARIC) study The ARIC investigators. Am. J. Epidemiol. 129, 687–702 (1989).
Juster, R. P., McEwen, B. S. & Lupien, S. J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 35, 2–16 (2010).
Walker, K. A. et al. Midlife systemic inflammatory markers are associated with late-life brain volume: The ARIC study. Neurology 89, 2262–2270 (2017).
Gabay, C. & Kushner, I. Acute-phase proteins and other systemic responses to inflammation. N. Engl. J. Med. 340(6), 448–454 (1999).
Biasucci, L. M. CDC/AHA workshop on markers of inflammation and cardiovascular disease: Application to clinical and public health practice: Clinical use of inflammatory markers in patients with cardiovascular diseases: A background paper. Circulation. 110(25), e560–e567 (2004).
Nagi, S. Z. An epidemiology of disability among adults in the United States. Milbank Mem. Fund. Q Health Soc. 54, 439–467 (1976).
Rosow, I. & Breslau, N. A Guttman health scale for the aged. J. Gerontol. 21, 556–559 (1966).
Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A. & Jaffe, M. W. Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. Jama. 185(12), 914–919 (1963).
Li, D. et al. Plasma phospholipid very-long-chain SFAs in midlife and 20-year cognitive change in the atherosclerosis risk in communities (ARIC): A cohort study. Am. J. Clin. Nutr. 111, 1252–1258 (2020).
Knopman, D. S. & Ryberg, S. A verbal memory test with high predictive accuracy for dementia of the Alzheimer type. Arch. Neurol. 46, 141–145 (1989).
Jaeger, J. Digit symbol substitution test: The case for sensitivity over specificity in neuropsychological testing. J. Clin. Psychopharmacol. 38, 513–519 (2018).
Pendleton, M. G., Heaton, R. K., Lehman, R. A. & Hulihan, D. Diagnostic utility of the thurstone word fluency test in neuropsychological evaluations. J. Clin. Neuropsychol. 4, 307–317 (1982).
Rabe, K. F. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care. Med. 176, 532–555 (2007).
Levey, A. S., Inker, L. A. & Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. 63(5), 820–834 (2014).
Igartua, J. J. & Hayes, A. F. Mediation, moderation, and conditional process analysis: Concepts, computations, and some common confusions. Span J. Psychol. 24, e49 (2021).
Tanaka, K. A., Terada, R., Butt, A. L., Mazzeffi, M. A. & McNeil, J. S. Factor VIII: A dynamic modulator of hemostasis and thrombosis in trauma. Anesth. Analg. 136(5), 894–904 (2023).
Baruch, D., Bahnak, B., Girma, J. P. & Meyer, D. von Willebrand factor and platelet function. Baillieres Clin. Haematol. 2(3), 627–672 (1989).
Bach, J., Haubelt, H. & Hellstern, P. Sources of variation in factor VIII, von Willebrand factor and fibrinogen measurements: Implications for detecting deficiencies and increased plasma levels. Thromb. Res. 126(3), e188–e195 (2010).
Singh, T. & Newman, A. B. Inflammatory markers in population studies of aging. Ageing Res. Rev. 10, 319–329 (2011).
Mekli, K., Nazroo, J. Y., Marshall, A. D., Kumari, M. & Pendleton, N. Proinflammatory genotype is associated with the frailty phenotype in the English longitudinal study of ageing. Aging Clin. Exp. Res. 28, 413–421 (2016).
Candore, G., Caruso, C. & Colonna-Romano, G. Inflammation, genetic background and longevity. Biogerontology 11, 565–573 (2010).
Quinones, A. R. et al. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS One 14, e0218462 (2019).
Mahajan, S. et al. Trends in differences in health status and health care access and affordability by race and ethnicity in the United States, 1999–2018. JAMA 326, 637–648 (2021).
Friedman, E. M., Christ, S. L. & Mroczek, D. K. Inflammation partially mediates the association of multimorbidity and functional limitations in a national sample of middle-aged and older adults: The MIDUS study. J. Aging Health 27, 843–863 (2015).
Acknowledgements
The authors thank the staff and participants of the ARIC study and BioLINCC for their important contributions.
Funding
This work was supported financially by grants from Sichuan Science and Technology Program (No. 2023YFS0027, 2023YFS0240, 2023YFS0074, 2023NSFSC1652, 2022YFS0279, 2021YFQ0062, 2022JDRC0148), Sichuan Provincial Health Commission (No. ZH2022-101), Sichuan University West China Nursing Discipline Development Special Fund Project (No. HXHL21016).
Author information
Authors and Affiliations
Contributions
YT and YJ conceived the study design. YT, YJ and AG collected the epidemiological and clinical data. YT, YJ, FL, and AG summarized data and performed the statistical analysis. YT and YJ interpreted the data and drafted the manuscript. RZ participated in the design of the study, acquired the data, and helped to revise the manuscript. All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tong, Y., Jia, Y., Gong, A. et al. Systemic inflammation in midlife is associated with late-life functional limitations. Sci Rep 14, 17434 (2024). https://doi.org/10.1038/s41598-024-68724-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68724-w
Keywords
This article is cited by
-
Exploring the nexus between inflammation and mobility through the lens of healthy aging: current scenario and future perspectives
Aging Clinical and Experimental Research (2026)