Abstract
Diabetic peripheral neuropathy is a common complication of diabetes mellitus that has dire outcomes, affecting the economic profile of a country. Despite the multifactorial background of the pathogenesis of this disease, the mechanism underlying peripheral neuropathy is still unclear. Endothelial damage is a new determinant of pathogenesis, with endocan as a potential biomarker for endothelial dysfunction in diabetic peripheral neuropathy patients. In this cross-sectional study, with 49 patients with diabetes with peripheral neuropathy and 48 patients with diabetes without neuropathy, endothelial biomarkers such as endocan, hs-CRP, vitamin D, and lipid profiles were measured and analyzed in both groups. The standardized scores for dyslipidemia, inflammation, vitamin D and endocan were calculated. All of these biomarkers were significantly altered in peripheral neuropathy patients. A strong correlation between endocan levels and lipid profiles and between hs-CRP and vitamin D levels was detected. The inflammatory score and a combined score including all the above biomarkers might help in the early stratification of diabetic patients who are at greater risk of developing peripheral neuropathy.
Similar content being viewed by others
The worldwide prevalence of diabetes mellitus has risen dramatically, with a diabetes incidence estimate in India of 125 million in 20451,2. The most common complication is diabetic peripheral neuropathy(DPN), with a prevalence ranging from 18.84 to 45.6%3,4,5,6,7,8. DPN mainly involves small nerve fibers and is diagnosed after excluding peripheral neuropathies due to other causes9. With an insidious onset, symptoms in the early stages are rare, so symptoms eventually progress to the late stage, causing serious complications such as diabetic foot ulcers resulting in amputations affecting the quality of life10.
DPN with a multifactorial pathophysiology has interactions between hyperglycemic vascular factors and metabolic cascade pathophysiological factors11,12. The vascular influence of altered function of the blood-nerve-barrier(BNB) with endoneurial microangiopathy seems to be the first marker for the development of DPN13. Histopathologically the endoneurial microvessels show as thickening of capillary basement membrane, loss of capillary pericyte coverage along with hyperplasia of endothelial cells and increased vascular permeability11. Furthermore, there is a continued electrolyte imbalance and thickening of the basal laminae, leading to progressive edema and ischemia of the neurons13,14. The above changes result in microcirculatory disturbances leading to tissue hypoxia and the promoting activity of vascular endothelial growth factor(VEGF) pathway to increase BNB permeability and thus BNB breakdown15.
Endocan, secreted by endothelial cells and is expressed by tissues, including capillary endothelial cells and neurons16. Proinflammatory cytokines and VEGF, upregulate the expression of endocan releasing molecules that increase the adhesion of leukocytes to endothelial cells, promoting the migration of inflammatory cells and damage16. Thus, an increase in endocan may be a potential immune-inflammatory marker. A positive association between endocan and diabetes and microvascular complications such as diabetic retinopathy and diabetic neuropathy has been observed, indicating that endocan is a new biomarker of angiogenesis in patients with complications of diabetes17,18.
The diagnosis of DPN is based on nerve conduction studies, wherein a positive finding is associated with late manifestation of DPN10. The screening methods proposed for the early detection of DPN are still not widely used due to their disadvantages. Therefore, it is necessary to develop a grading or scoring system to assess the severity of DPN, perform early intervention and improve the quality of life. Endocan is involved in endothelial dysfunction and a similar status has been suggested for the pathogenesis of DPN. However, studies conducted in this area are grossly inadequate, and therefore, this study could be of diagnostic and therapeutic importance for characterizing alterations in endocan in patients with diabetes and DPN.
Therefore, the aim of this study was to measure and analyze the angiogenic biomarker endocan between individuals with diabetes with and without neuropathy and to compare the inflammatory state among the groups.
Materials and methods
Study design
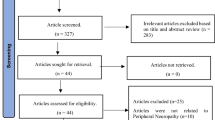
This was a hospital-based cross-sectional study conducted in the Department of Biochemistry and Endocrinology of our institute. The study was granted ethical approval by the Institute Ethics Committee vide Proposal No. AIIMSRPR/IEC/2022/1227 and Approval Ref No 2492/IEC-AIIMSRPR/2022, dated 26th September 2022. All procedures of the study followed the guidelines of the Declaration of Helsinki and Tokyo. The recruitment of subjects and analysis of the samples were performed between April 2023 and December 2023. The study population comprised 97 adult patients with diabetes who visited the OPD of the Department of Endocrinology for more than five years. The patients were categorized into two groups: those with diabetes with peripheral neuropathy (DPN, n = 49) and those with diabetes without peripheral neuropathy (No DPN, n = 48).
DPN was defined as impairment in one or more of the following criteria: a vibration perception threshold ≥ 25 V, heat pain threshold > 48 °C, or cold pain threshold < 10 °C. Conversely, the absence of peripheral neuropathy was determined by the presence of all specified conditions: a vibration perception threshold ≤ 15 V, heat pain threshold < 42 °C, and cold pain threshold > 20°C19,20,21.
The exclusion criteria included diabetes with clinical evidence of cardiovascular disease like coronary, peripheral or carotid artery disease, major disease(hepatic or renal failure, malignancy, autoimmune disease and any acute or chronic infections), recent trauma or surgery within one month, thyroid disease, megaloblastic anemia, chronic alcoholism, and pregnancy.
Study procedure
Patients who satisfied the inclusion criteria were enrolled after providing informed written consent. The detailed clinical history of the patient and any recent biochemical data (within three months) were obtained from patient records. The demographic profiles of age and sex were recorded, and biophysical parameters such as height, weight, and systolic and diastolic blood pressure were measured. The ankle brachial pressure index (ABPI) was assessed to rule out peripheral arterial disease (PAD). Diabetic peripheral neuropathy assessment was performed on areas of both feet(great toe, first meta-tarsal, fifth metatarsal, medial arch, lateral arch and heel) of an individual by quantitative sensory testing (QST) using a Vibrotherm-Dx neuropathy analyzer.
Blood sampling
Blood samples for investigations, such as glucose (fasting and postprandial), urea, creatinine, lipid profile, hs-CRP, and vitamin D, were collected and processed the same day in an AU5800 autoanalyzer (Beckman Coulter, Inc.). HbA1c was measured by ion exchange high-performance liquid chromatography (HPLC) using D-10 equipment from Bio-Rad Laboratories, Inc. Serum vitamin D was estimated by chemiluminescence immunoassay (CLIA) in a Siemens Advia Centaur XP autoanalyzer. The plasma was collected in EDTA vials, centrifuged at − 4 °C and stored at − 80 °C for Endocan analysis.
Endocan assay
The quantitative determination of human endothelial cell-specific molecule-1/Endocan (ESM-1/Endocan) activity was performed based on the principle of a double-antibody sandwich enzyme immunoassay (ELISA) kit. (Coon Koon Biotech China, Cat No. CK-Bio11325, LOT No. 202304). The samples were processed within 2 months of collection and stored at − 80 °C to avoid loss of bioactivity. The intra-assay CV% was < 7%, with a sensitivity of 1 pg/mL.
Statistical analysis
All the statistical analyses were performed using Jamovi software version 2.3.26 (Sydney, Australia). The Shapiro–Wilk test was used to assess normality. Normally and nonnormally distributed data are represented as the mean and standard deviation (SD) and as the median and interquartile range (IQR), respectively. Comparisons were performed using Student’s t test and the Mann‒Whitney U test. Spearman’s rho was used to determine the correlation of endocan with various biochemical parameters. Binomial logistic regression analysis was performed to identify the best predictive model, and based on this, the sensitivity, specificity, positive predictive value (PPV) and negative predictive value of the ROC curve were measured. A p value < 0.05 was considered to indicate statistical significance.
Results
This study was performed to assess the difference in endocan levels between two groups of diabetic patients without peripheral neuropathy and those with peripheral neuropathy. According to the operational definitions, 49 diabetic patients suffered from peripheral neuropathy, whereas 48 diabetic patients did not have neuropathy.
The clinico-anthropometric measurements of the study population are summarized in Table 1. The two groups were similar in age and sex distribution. A comparable height, weight, BMI, and systolic and diastolic blood pressure were observed in both groups.
Table 2 compares the biochemical variables between the study groups. Fasting plasma glucose (FPG) did not significantly differ between the groups (p = 0.198), while postprandial plasma glucose (PPPG) was significantly greater in the DPN group (p = 0.015). Notably, the DPN group exhibited elevated HbA1c levels compared to those in the non-DPN group (p = 0.006). Additionally, significant differences were observed in total cholesterol (p = 0.005), TG (p = 0.003), HDL cholesterol (p < 0.001), urea (p < 0.001), creatinine (p = 0.004), eGFR (p = 0.004), hs-CRP (p = 0.002), vitamin D (p < 0.001), and Endocan (p < 0.001).
To calculate the dyslipidemia score, we standardized all the variables by calculating Z scores for LDL-C, TG and HDL-C using the mean and standard deviation. Thereafter, the dyslipidemia score was calculated according to the following equation: average of the standardized variables (LDL-C + TG)/2 minus standardized HDL-C22. The inflammation score was also determined in both groups after standardization of hs-CRP; similarly, the standardized vitamin D and standardized endocan levels were determined. Figure 1 shows high standardized dyslipidemia (p = 0.007*), high standardized inflammation markers such as hs-CRP (p < 0.001*), high standardized endocan (p = 0.004*) and low standardized vitamin D (p < 0.001*) scores between diabetic patients with and without neuropathy. These results highlight significant differences in these parameters between the two groups, providing insights into potential associations with diabetic neuropathy.
The results from Spearman’s correlation analysis of the interrelationship of endocan with various biochemical parameters and standardized scores are presented in Table 3. Notably, endocan was significantly positively correlated with T-CSF, TG, LDL, urea, creatinine, standardized hs-CRP, and the standardized Dys score. Conversely, it exhibits a significant negative correlation with HDL, eGFR and standardized vitamin D. These findings suggest potential associations between endocan levels and the abovementioned variables, shedding light on its potential implications in various physiological processes.
With the above findings, the authors assessed the influence and extent of dyslipidemia, inflammation and endothelial factors as comprehensive DIVE scores in both groups. The DIVE score, as shown in Fig. 2, was significantly greater (p < 0.021) in patients with DPN than in those without DPN. This finding implies that the DIVE score could serve as a useful metric for distinguishing between these two groups in the context of diabetic peripheral neuropathy.
In-depth independent associations of clinical data were tested with binomial logistic regression analysis to determine the influence of endocan, Std hs-CRP, the Std Dys score, Std Vit D and the DIVE score on DPN. The best models that determined the variability in the distinct scores are shown in Table 4. Predictive models using multivariate logistic regression identified endocan and the other standardized scores as independent predictors for DPN (odds ratio of endocan: 1.002, p = 0.002; odds ratio of Std hsCRP: 2.672, p = 0.017; odds ratio of Std Dys score: 1.118, p = 0.05; odds ratio of Std Vit D: 0.480, p = 0.019; odds ratio of DIVE score: 1.28, p = 0.022). The adjusted R2 indicated that approximately 28% of the variability in Std Dys score values, 45.3% of the variability in hsCRP, 34.8% of the variability in vitamin D, and 27.2% of the variability in endocan were related to DPN. The adjusted R2 indicated that approximately 7.8% of the DIVE score was responsible for DPN.
The ROC curve (Fig. 3) and analysis in Table 5 reveal the diagnostic efficacy of various biomarkers in distinguishing diabetic peripheral neuropathy (DPN) patients from diabetic patients without DPN. Notably, hs-CRP had a robust AUC of 0.781, indicating high discriminative power. The standardized Dys score, with a cutoff of 0.07, exhibited moderate sensitivity (63.27%) and specificity (72.92%). Despite its high sensitivity (89.8%), vitamin D has a low specificity (6.25%) at a cutoff of 9.73. Endocan achieved a balanced performance with sensitivity (81.63%) and specificity (56.25%), resulting in an AUC of 0.739. At a cutoff of -0.58, the DIVE score had a moderate AUC of 0.636, reflecting satisfactory sensitivity (77.55%) and specificity (54.17%). These findings provide valuable insights into the ability of biomarkers to accurately identify individuals with DPN.
Discussion
To the best of our knowledge, this is the first study to explore the complex interplay between immune-inflammatory markers, dyslipidemia, vitamin D levels, and endocan in patients with diabetes and peripheral neuropathy. The increasing global prevalence of diabetes mellitus and its associated complications, including DPN, emphasizes the urgency for in-depth investigations to unveil potential biomarkers and pathways for early diagnosis that can aid early intervention.
First, the study revealed a significant association between dyslipidemia and DPN. The dyslipidemia score, which incorporates the standardized variables LDL-C, TG, and HDL-C, revealed distinct differences between diabetic patients with and without neuropathy. Dyslipidemia has long been a modifiable risk factor for the incidence and progression of DPN23.The interaction of dyslipidemia with the entry of long-chain fatty acids through the blood–neutrophil barrier triggers neurogenic inflammation and the release of a cascade of cytokines and chemokines, promoting tissue injury. The role of a high-fat diet in inducing DPN and subsequent dietary reversal, demonstrating the normalization of neuropathy, adds importance to the role of dyslipidemia in the pathogenesis of DPN24. Recent lipidomic studies revealed alterations in lipid classes related to mitochondrial dysfunction in patients who developed peripheral neuropathy25.
Second, the study explored the status of inflammation in the two groups of patients with diabetes with and without peripheral neuropathy. The inflammation score, determined by standardized hs-CRP levels, demonstrated a pronounced difference between the two groups. In this study, both groups exhibited a cluster of metabolic factors characterized by mild chronic inflammation that shifted the immune microenvironment to a proinflammatory state. In one follow-up study, hs-CRP above 2.5 mg/L was shown to predict the development of diabetic neuropathy26. Inflammatory cells in diabetic nerves release excessive TNF-α or interleukins and activate the mitogen activated protein (MAP)-kinase pathway and NF‐κB pathway, causing microangiopathy in diabetic neuropathy27.
Moreover, this study examined the potential impact of vitamin D deficiency on DPN. Evidence from studies has shown that vitamin D deficiency might affect the development of DPN28,29,30. These studies suggest early monitoring and evaluation of vitamin D in the early stages of disease. Moreover, vitamin D increases the level of nerve growth factor, preventing neurotrophic deficits. The vitamin D receptor is highly expressed in the dorsal ganglion of small fibers that respond to pain, an explanation for painful neuropathy in diabetes patients31 In this study, standardized vitamin D levels were significantly different between individuals with and without DPN, supporting the hypothesis that vitamin D status may play a role in the pathogenesis of painful DPN through elevated inflammation.
Although there are diverse underlying factors in the pathogenesis of DPN, endothelial dysfunction is a mainstay and crucial aspect. This leads to altered blood–nerve–barrier permeability, impacting nutrition and oxygen supply and subsequent demyelination of nerves in DPN patients12. A novel aspect of the study involves the investigation of endocan as a potential biomarker for DPN. Endocan levels were greater in patients with DPN than in those without DPN. Endocan, a secreted and expressed vascular endothelial cell, regulates endothelium activation, permeability, and proliferation. It is controlled by proinflammatory cytokines and is increased in inflammation and disorders such as atherosclerosis and hypertension32. Since it affects inflammatory and vasculo-protective signals, it may be a marker of endothelial dysfunction. A meta-analysis by Khalaji A et al. revealed that endocan levels are increased in diabetic patients and are greater in diabetic patients with complications; therefore, endocan may play a functional role in endothelium-dependent pathological disorders such as DPN33. In this study, correlation analysis revealed associations between endocan and various biochemical parameters, emphasizing the potential relevance of these parameters for endothelial dysfunction in DPN pathophysiology. Considering these findings, endocan and a combination of these biomarkers might be suitable candidates for early identification of the risk of developing complications such as peripheral neuropathy in diabetes patients.
The study's integrative approach culminated in the development of a comprehensive DIVE score, incorporating dyslipidemia, inflammation, vitamin D, and endocan scores. The DIVE score demonstrated a statistically significant difference between individuals with and without DPN, suggesting its potential utility as a metric for distinguishing between these two groups. The predictive models, derived from multivariate logistic regression analysis, highlighted the independent predictive value of endocan, standardized hs-CRP, standardized dyslipidemia score, standardized vitamin D, and the DIVE score for DPN. These findings underscore the multifactorial nature of DPN, involving dyslipidemia, inflammation, and vitamin D status, with endocan emerging as a potential key player. The ROC analysis evaluated the cutoff value with the highest Youden’s index of various biomarkers. Individually, hs-CRP exhibited high discriminative power, and the DIVE score demonstrated moderate sensitivity and specificity, reinforcing the potential utility of this integrated approach in clinical settings. Future studies are needed to assess the predictive ability of the DIVE score for DPN onset. Some individuals in the cohort without DPN might be at risk, which could explain the poorer AUC for the DIVE score.
Strengths and limitations
To the best of our knowledge, this is the first study in the Indian subcontinent to comprehensively characterize direct and surrogate endothelial biomarkers that are related to diabetic neuropathy. Using these biomarkers, the authors have derived a novel summary score (DIVE score) for the first time that contributes to the potential development of risk prediction tools, aiding clinicians in identifying individuals at greater risk for DPN. Although QST for DPN, involves subjective assessments, since outcomes depend on patient responses, we have used clear cut-off points for severely impaired sensory thresholds.
However, to reach well-reasoned conclusions about our new findings, prospective studies are needed to measure the ability of these combined biomarkers and scores to mitigate the risk of DPN. Future studies should be done to assess the association of the DIVE score and endocan with objective assessments for early neurodegeneration, including corneal confocal microscopy, skin biopsies, and nerve conduction studies.
Conclusion
In conclusion, this study revealed the overexpression of endocan in patients with DPN. This research contributes valuable insights into the intricate web of factors influencing DPN in individuals with diabetes mellitus. This comprehensive approach, encompassing dyslipidemia, inflammation, vitamin D, and endocan, provides a holistic perspective on the pathogenesis of DPN. The findings pave the way for further research and potential clinical applications aiming to improve early diagnosis and intervention for DPN, ultimately enhancing the quality of life for individuals with diabetes.
Data availability
Data and materials supporting the results of this article are included within the article.
Abbreviations
- IDF:
-
International Diabetes Federation
- DPN:
-
Diabetic peripheral neuropathy
- BNB:
-
Blood-nerve-barrier
- VEGF:
-
Vascular endothelial growth factor
- ABPI:
-
Ankle Brachial Pressure Index
- PAD:
-
Peripheral artery disease
- OPD:
-
Out patient department
- CLIA:
-
Chemiluminescence immunoassay
- BMI:
-
Body mass index
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglycerides
- eGFR:
-
Estimated glomerular filtration rate
- ELISA:
-
Enzyme-linked immunosorbent assay
- IQR:
-
Interquartile range
- ROC:
-
Receiver operating characteristics curve
References
Kumar, A., Gangwar, R., Ahmad Zargar, A., Kumar, R. & Sharma, A. Prevalence of diabetes in India: A review of IDF diabetes atlas 10th edition. Curr. Diabetes Rev. 20(1), 6130423215752. https://doi.org/10.2174/1573399819666230413094200 (2024).
Diabetes - India [Internet]. [cited 2024 Feb 17]. Available from: https://www.who.int/india/health-topics/mobile-technology-for-preventing-ncds
Ashok, S., Ramu, M., Deepa, R. & Mohan, V. Prevalence of Neuropathy in type 2 diabetic patients attending a diabetes centre in South India. J Assoc. Physicians India 50, 546–550 (2002).
Rani, P., Raman, R., Rachapalli, S. R., Pal, S. S. & Kulothungan, V. Prevalence and risk factors for severity of diabetic neuropathy in type 2 diabetes mellitus. Indian J. Med. Sci. 64, 51–57. https://doi.org/10.4103/0019-5359.94400 (2010).
Agrawal, R. P. et al. Prevalence of micro and macrovascular complications and their risk factors in type-2 diabetes mellitus. J. Assoc. Physicians India 62(6), 504–508 (2014).
Baxi, H. et al. Prevalence of peripheral neuropathy and associated pain in patients with diabetes mellitus: Evidence from a cross-sectional study. J. Diabetes Metab. Disord. 19(2), 1011–1017. https://doi.org/10.1007/s40200-020-00597-y (2020).
Jasmine, A. et al. Prevalence of peripheral neuropathy among type 2 diabetes mellitus patients in a rural health centre in South India. Int. J. Diabetes Dev. Ctries 41, 293–300. https://doi.org/10.1007/s13410-020-00885-6 (2021).
Kamalarathnam, S. & Varadarajan, S. Diabetic peripheral neuropathy in diabetic patients attending an urban health and training centre. J. Family Med. Prim. Care 11, 113. https://doi.org/10.4103/jfmpc.jfmpc_470_21 (2022).
Tesfaye, S. et al. Diabetic neuropathies: Update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 33, 2285. https://doi.org/10.2337/dc10-1303 (2010).
Yu, Y. Gold standard for diagnosis of DPN. Front. Endocrinol. 12, 719356. https://doi.org/10.3389/fendo.2021.719356 (2021).
Østergaard, L. et al. The effects of capillary dysfunction on oxygen and glucose extraction in diabetic neuropathy. Diabetologia 58(4), 666–677. https://doi.org/10.1007/s00125-014-3461-z (2015).
Kobayashi, M. & Zochodne, D. W. Diabetic neuropathy and the sensory neuron: New aspects of pathogenesis and their treatment implications. J. Diabetes Investig. 9(6), 1239–1254. https://doi.org/10.1111/jdi.12833 (2018).
Galiero, R. et al. Peripheral neuropathy in diabetes mellitus: Pathogenetic mechanisms and diagnostic options. Int. J. Mol. Sci. 24(4), 3554. https://doi.org/10.3390/ijms24043554 (2023).
Takeshita, Y., Sato, R. & Kanda, T. Blood–nerve barrier (BNB) pathology in diabetic peripheral neuropathy and in vitro human BNB model. Int. J. Mol. Sci. 22(1), 62. https://doi.org/10.3390/ijms22010062 (2021).
Richner, M. et al. Functional and structural changes of the blood-nerve-barrier in diabetic neuropathy. Front. Neurosci. 12, 01038. https://doi.org/10.3389/fnins.2018.01038 (2019).
Chen, J. et al. Endocan: A key player of cardiovascular disease. Front. Cardiovasc. Med. 8, 798699. https://doi.org/10.3389/fcvm.2021.798699 (2022).
Abu El-Asrar, A. M. et al. The angiogenic biomarker endocan is upregulated in proliferative diabetic retinopathy and correlates with vascular endothelial growth factor. Curr. Eye Res. 40, 321–331. https://doi.org/10.3109/02713683.2014.921312 (2015).
Bilir, B. et al. Association of Apelin, Endoglin and Endocan with diabetic peripheral neuropathy in type 2 diabetic patients. Eur. Rev. Med. Pharmacol. Sci. 20(5), 892–898 (2016).
Ziegler, D., Mayer, P. & Gries, A. Evaluation of thermal, pain, and vibration sensation thresholds in newly diagnosed type 1 diabetic patients. J. Neurol. Neurosurg. Psychiatry 51(11), 1420–1424. https://doi.org/10.1136/jnnp.51.11.1420 (1988).
Young, M. J., Breddy, J. L., Veves, A. & Boulton, A. J. M. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds a prospective study. Diabetes Care 17(6), 557–560. https://doi.org/10.2337/diacare.17.6.557 (1994).
Rashad, N. M., Amer, M. M., Al-Sayed, R. M., Abd El-Fatah, A. H. & Fathy, H. A. Endothelial-specific molecule 1 (Endocan) as a marker of vascular endothelial regulation of obesity-associated peripheral polyneuropathy in the non-diabetic obese patients. Med. J. Cairo Univ. 88, 345–354. https://doi.org/10.21608/MJCU.2020.93996 (2020).
Blagojević, I. P. et al. Evaluation of a Summary Score for Dyslipidemia, Oxidative Stress and Inflammation (The DOI Score) in women with polycystic ovary syndrome and its relationship with obesity. J Med. Biochem. 37, 476–485. https://doi.org/10.2478/jomb-2018-0008 (2018).
Selvarajah, D. et al. Diabetic peripheral neuropathy: Advances in diagnosis and strategies for screening and early intervention. Lancet Diabetes Endocrinol. 7(12), 938–948. https://doi.org/10.1016/S2213-8587(19)30081-6 (2019).
Stino, A. M., Rumora, A. E., Kim, B. & Feldman, E. L. Evolving concepts on the role of dyslipidemia, bioenergetics, and inflammation in the pathogenesis and treatment of diabetic peripheral neuropathy. J. Peripher. Nerv. Syst. 25(2), 76–84. https://doi.org/10.1111/jns.12387 (2020).
Afshinnia, F. et al. Serum lipidomic determinants of human diabetic neuropathy in type 2 diabetes. Ann. Clin. Transl. Neurol. 9(9), 1392–1404. https://doi.org/10.1002/acn3.51639 (2022).
Aryan, Z. et al. Baseline high-sensitivity c-reactive protein predicts macrovascular and microvascular complications of type 2 diabetes: A population-based study. Ann. Nutr. Metab. 72(4), 287–295. https://doi.org/10.1159/000488537 (2018).
Yagihashi, S., Mizukami, H. & Sugimoto, K. Mechanism of diabetic neuropathy: Where are we now and where to go?. J. Diabetes Investig. 2(1), 18–32. https://doi.org/10.1111/j.2040 (2011).
Alireza, E. et al. Non-linear contribution of serum vitamin D to symptomatic diabetic neuropathy: A case-control study. Diabetes Res. Clin. Pract. 111, 44–50. https://doi.org/10.1016/j.diabres.2015.10.018 (2016).
Abdelsadek, S. E., El Saghier, E. O. & Abdel Raheem, S. I. Serum 25(OH) vitamin D level and its relation to diabetic peripheral neuropathy in Egyptian patients with type 2 diabetes mellitus. Egypt. J. Neurol. Psychiatr. Neurosurg. 54(1), 36. https://doi.org/10.1186/s41983-018-0036-9 (2018).
Assy, M. H., Draz, N. A., Fathy, S. E. & Hamed, M. G. Impact of vitamin D level in diabetic people with peripheral neuropathy. Egypt. J. Neurol. Psychiatry Neurosurg. 57, 117. https://doi.org/10.1186/s41983-021-00370-9 (2021).
Putz, Z. et al. Vitamin D in the prevention and treatment of diabetic neuropathy. Clin. Ther. 44(5), 813–823. https://doi.org/10.1016/j.clinthera.2022.03.012 (2022).
Hirooka, Y. How can endocan be used as a specific biomarker of endothelial dysfunction in hypertension?. Hypertens. Res. 47, 794–795. https://doi.org/10.1038/s41440-023-01542-1 (2024).
Khalaji, A. et al. Endocan in prediabetes, diabetes, and diabetes-related complications: A systematic review and meta-analysis. Diabetol. Metab. Syndr. 15(1), 102. https://doi.org/10.1186/s13098-023-01076-z (2023).
Author information
Authors and Affiliations
Contributions
P.P.J.: Sample collection, gathering clinical data, and initial draft of the paper. R.N.: Conception, design, and conduct of the study and edited and approved the final version of the manuscript. A.G.: Design of study, resources, investigation, edited the manuscript. S.P.: Conceptualization, analysis, writing—review and editing of manuscript S.S.: Supervision, investigation, data curation, manuscript editing. E.M.: Design of study, investigation, supervision, editing the final draft. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jena, P.P., Nanda, R., Ghosh, A. et al. Endocan expression and correlation with other endothelial determinants in developing a score for early identification of diabetic peripheral neuropathy. Sci Rep 15, 850 (2025). https://doi.org/10.1038/s41598-024-68790-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68790-0