Abstract
Hereditary transthyretin (ATTRv) amyloidosis is a rare, adult-onset, progressive, multisystemic condition caused by TTR pathogenic variants. Reliable biomarkers are needed to allow early diagnosis and to monitor disease severity and progression. We measured serum concentrations of growth differentiation factor-15 (GDF-15) and uromodulin (Umod) in ATTRv patients to evaluate correlations with standard markers of disease severity (FAP stage and PND score). Blood samples were collected from 16 patients diagnosed with ATTRv amyloidosis and a verified TTR variant and from 26 healthy controls. ATTRv patients were stratified by clinical phenotype (neurologic vs. mixed), genotype (V30M vs. non-V30M), and disease severity. We found significantly higher levels of serum GDF-15 in ATTRv patients compared with controls. Mean serum Umod levels were significantly lower in patients with ATTRv than controls. A positive correlation was found between serum Umod and estimated glomerular filtration rate (eGFR), while an inverse correlation was found with cystatin C levels. Conversely, GDF-15 showed a negative correlation with eGFR, and a direct correlation with cystatin C levels. No correlation was demonstrated between GDF-15 or Umod levels and traditional cardiac biomarkers. The results identify alteration of serum levels of GDF-15 and Umod in ATTRv amyloidosis.
Similar content being viewed by others
Introduction
Hereditary transthyretin (ATTRv) amyloidosis, a rare, adult-onset, and progressive multisystemic condition caused by pathogenic variants in the TTR gene, is inherited as an autosomal dominant disorder with highly variable penetrance1,2. The disease is caused by the progressive aggregation of transthyretin (TTR)—a liver transport protein of thyroxine and retinol—and the subsequent extracellular deposition of amyloid fibrils in various organs, predominantly affecting the somatic and autonomic peripheral nervous systems and the heart, with frequent ocular, gastroenterological, and renal manifestations3,4,5. Due to its heterogeneous presentation, diagnosing ATTRv can be challenging for clinicians, leading to a delay in initiating therapy. As of today, several disease-modifying drugs have been approved for ATTRv, making it a priority to identify reliable disease biomarkers to support an early diagnosis and increase patients’ survival. In our previous studies on patients with ATTRv, we have already investigated the possible role of both inflammatory and metabolic molecules as biomarkers of the disease. Our population showed elevated IFN-alpha and IFN-gamma levels indicative of immune activation and lower IL-7 levels suggesting disrupted lymphocyte homeostasis6. Additionally, reduced serum levels of palmitic acid suggested a dysregulation in lipid metabolism, potentially linked to mitochondrial dysfunction and neuroinflammation7.
Growth differentiation factor-15 (GDF-15) is a transforming growth factor-β superfamily cytokine with a role in a variety of biological processes and pathological conditions, including inflammation, cellular responses to stress signals, and tissue repair after acute injuries8. This stress-responsive cytokine was reported as a useful marker of disease development, progression, and prognosis in patients with cardiovascular disease9,10. GDF-15 has been documented to be a valid prognostic marker in patients with light-chain amyloidosis11, and to be a diagnostic biomarker in a specific subgroup of neurogenetic disorders defined as primary mitochondrial diseases12.
Uromodulin (Umod) is a kidney-specific protein mainly produced by tubular epithelial cells and involved in electrolyte handling and the regulation of sodium transport processes. Umod has emerged as a novel early biomarker for renal function and the detection of kidney disease due to the correlation of Umod urinary and serum levels with tubular mass and renal function13,14.
In this study, we measured serum concentrations of GDF-15 and Umod in the cohort of ATTRv patients, comparing them with the control group and evaluating the possible correlation between these values and clinical or laboratory markers of disease severity.
Materials and methods
Patient population
Details of the patient population have been published in Luigetti et al. 20227. In brief, blood samples were collected from a case series of individuals with a confirmed pathogenic TTR variant and a diagnosis of ATTRv amyloidosis with a confirmed polyneuropathy, with or without multisystem involvement. Control blood samples were collected from healthy individuals with no evidence of neurologic, cardiac, or renal disease. All serum samples were stored at − 80 °C until analysis7.
The study was conducted in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its amendments and approved by the Ethics Committee of Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy (protocol ID 5470). Informed consent was obtained from all subjects involved in the study.
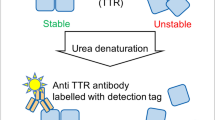
Biomarker profiling
Protein detection was performed with Luminex xMAP technology using the bead-based Human Luminex® Discovery Assay (R&D Systems) according to the manufacturer’s instructions. All samples were analyzed for cystatin C, uromodulin, and GDF-15; serum samples were centrifuged at 16,000 g at 4 °C for 4 min and then diluted two-fold and run in duplicate. Analyte-specific antibodies pre-coated onto magnetic microparticles embedded with fluorophores at set unique ratios were incubated with samples. Biotinylated antibodies specific to the target analytes were added to each reaction well. Following repeated washing, streptavidin–phycoerythrin conjugate was added to measure the amount of analyte bound to the microparticle. The process utilized ≥ 50 beads per analyte, and median fluorescence intensities were measured using Luminex-200 technology (Luminex, Bio-Rad) and analyzed with Bio-Plex Manager software version 6.1 (Bio-Rad). A CCD camera with a set of filters to differentiate excitation levels was used. Standard curves for each cytokine were generated using the premixed lyophilized standards provided in the kits. Serial threefold dilutions of the standards were run. Cytokine concentrations in samples were determined according to the manufacturer’s protocol utilizing 5-point regression to transform mean fluorescence intensities from the standard curve into concentrations. Each sample was run in duplicate and averaged to provide the measured concentration.
Clinical assessment scores and laboratory evaluations
A specialist in ATTRv amyloidosis disease conducted a complete neurological and neurophysiological evaluation of all patients, assessing several outcome measures, including familial amyloid polyneuropathy (FAP) stage, polyneuropathy disability (PND) score, the Neuropathy Impairment Score (NIS), and the Quality of Life-Diabetic Neuropathy (Norfolk QoL-DN) questionnaire7. Electrochemical skin conductance measurements on all enrolled patients using Sudoscan were performed as previously described15. Other laboratory data and outcome measures, including high-sensitivity troponin (hs-TnT), N-terminal pro-B-type natriuretic peptide (NT-proBNP), and creatinine were collected. Interventricular septum (IVS) thickness and estimated glomerular filtration rate (eGFR) were also measured. eGFR was obtained with the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, based on serum creatinine alone (2021 CKD-EPI Creatinine equation) and serum creatinine and cystatin C combined (2021 CKD-EPI Creatinine-Cystatin C equation).
ATTRv patients were stratified according to genotype (V30M vs. non-V30M), clinical phenotype (neurologic vs. mixed), and disease severity according to FAP stage and PND score.
Statistical analysis
Data were summarized as frequencies (number/percentage) or mean ± standard deviation (SD), and as median and IQR, as appropriate. The Kolmogorov–Smirnov and Shapiro–Wilk tests were used to assess variable distributions. Levene’s test was performed to assess homogeneity of variance. Comparisons between two independent groups were performed with independent samples t-test or Mann–Whitney U test as appropriate.
A Spearman’s rank-order correlation test was used to identify any potential linear relationship between explored biomarkers and demographic, clinical and laboratory data in the ATTRv group (age at evaluation, disease duration, NIS, Norfolk QoL-DN questionnaire, Sudoscan of lower and upper limbs, IVS thickness, standard cardiac and renal biomarkers). A two-tailed p-value < 0.05 was considered statistically significant. Statistical analysis was performed using the IBM SPSS Statistics software (version 25.0).
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Fondazione Policlinico Universitario A. Gemelli IRCCS, Roma, Italia (protocol ID 5470).
Results
A total of 42 subjects were included in the study. As reported in Luigetti et al. 2022, there were 16 ATTRv patients and 26 healthy controls (HCs). Median age of patients in the control group was 50.0 years (interquartile range [IQR] 45.25–59.25), of whom 50% were male. In the ATTRv patients, median age was 69.5 years (IQR 65.75–75.00), of whom 81.3% were male. The main demographic and clinical data of the cohort of the ATTRv patients have been reported earlier6 and are summarized in Table 1. Laboratory results are summarized in Table 2. At the time of the study, most patients (14 out of 16) were on disease-modifying therapies: specifically, 5 patients were taking a TTR-stabilizer (Tafamidis) and 9 patients were on gene silencers (8 patients with Patisiran and 1 patient with Inotersen).
Umod levels were significantly lower in the ATTRv group (median 48.70 ng/mL, IQR 33.36–109.12; p = 0.004) compared with HCs (median 105.39 ng/mL, IQR 85.97–132.22). Conversely, GDF-15 levels were significantly higher in ATTRv patients (median 897.60 pg/mL, IQR 585.71–1209.81) than in HCs (median 445.59 pg/mL, IQR 330.78–638.02; p = 0.002), as were cystatin C levels (median 1.18 mg/L, IQR 0.92–1.31 in the patient group vs. median 0.33 mg/L, IQR 0.24–0.48 in HCs; p < 0.001).
Considering the laboratory and instrumental biomarkers, we found a statistically significant direct correlation between serum Umod levels and the eGFR calculated through the 2021 CKD-EPI creatinine-cystatin C equation (rS = 0.648, p = 0.007), and a strong, inverse relationship between serum Umod levels and cystatin C levels (rS = − 0.772, p < 0.001). Conversely, GDF-15 levels showed a negative correlation with the eGFR (2021 CKD-EPI creatinine-cystatin C equation; rS = − 0.587, p = 0.017), and a positive correlation with cystatin C levels (rS = 0.563, p = 0.023). No correlation was found between either Umod or GDF-15 levels and the eGFR calculated through the equation based on creatinine alone. Analogously, neither Umod nor GDF-15 levels showed any correlation with cardiac biomarkers (NT-proBNP, hs-TnT, and IVS thickness).
As regards clinical data, the only statistically significant relationship was an inverse correlation between GDF-15 values and Sudoscan values from upper limbs (rS = − 0.513, p = 0.042). No statistically significant difference in terms of Umod or GDF-15 levels was found stratifying ATTRv patients based on genotype (V30M vs. non-V30M), clinical phenotype (mixed vs neuropathic) or disease severity (PND score of FAP stage).
Discussion
ATTRv is a severe multiorgan disease caused by the extracellular accumulation of amyloid fibrils, and it can manifest with different clinical phenotypes: an axonal sensory, autonomic, and motor neuropathy (FAP), an infiltrative hypertrophic cardiomyopathy (familial amyloid cardiomyopathy), or a mixed phenotype that includes both1. The clinical course is progressive and disabling and leads to death within 4–15 years from onset if left untreated. However, the development of disease-modifying therapies over the past years has changed the natural history of the disease, especially when treatment is started early. For this reason, there is an urgent need for reliable biomarkers to reach an early diagnosis and to monitor disease severity and progression.
In patients with FAP, as well as in patients with a mixed phenotype, the use of serum biomarkers such as NT-proBNP and eGFR has now been validated and incorporated into clinical practice to determine disease staging, prognosis, and to stratify patient enrollment in clinical trials investigating novel therapies16. Our study aimed to investigate whether non-traditional biomarkers, such as GDF-15 and Umod, can identify patients with ATTRv and determine disease severity when correlated with clinical scales or instrumental evaluation.
As noted, GDF-15 is a stress-responsive cytokine prominently expressed in several tissues, including the heart, gastrointestinal tract, liver, kidney, brain, and skeletal muscle8,17. Cardiac myocytes produce and release GDF-15 in response to various triggers such as oxidative stress, stimulation with proinflammatory cytokines, ischemia, and mechanical stretch18,19,20,21. As a result, plasma GDF-15 concentrations increase in hypertrophic cardiomyopathy, ischemia, and at various stages of heart failure, reflecting the increased left ventricular mass index, even in the preclinical stage10,22. For this reason, GDF-15 has been evaluated as a prognostic biomarker in cardiovascular disease, in addition to conventional cardiac markers, such as NT-proBNP and hs-TnT23,24,25,26.
In patients with light chain amyloidosis, higher levels of serum GDF-15 are associated with an increased risk of early mortality, poor overall survival, and progression to dialysis, independently of other conventional biomarkers. Considering the widespread distribution of this cytokine, these findings may reflect both the degree of cardiac stress and the systemic proinflammatory condition caused by direct toxic effects related to amyloidogenic light chains11,27. Regarding ATTRv, a retrospective study by Okada et al.28 revealed increased levels of plasma GDF-15 even in asymptomatic subjects with TTR variants, and a significant correlation between these values and cardiac biomarkers, including serum BNP and hs-TnT values, IVS thickness, and cardiac magnetic resonance imaging results. Another interesting finding that emerged from the study was the detection of varying levels of GDF-15 in patients with different TTR genotypes, suggesting that different types of TTR fibrils may affect cardiac involvement and, consequently, the production of GDF-15.
A key role in the expression of GDF-15 is played by the integrated stress response, an elaborate signaling pathway activated in mammalian cells in response to several known cellular stress factors, including amino acid deprivation, hypoxia, and endoplasmic reticulum stress29,30. More specifically, numerous recent published papers have documented both in mouse models and human mitochondrial myopathy that the mitochondrial integrated stress response is associated with profound metabolic rewiring occurring in muscle and systemically via secretion of myokines such as fibroblast growth factor-21 and GDF-1531,32,33.
Considering what has been documented so far, it is unsurprising that GDF-15 is considered a valid biomarker in primary mitochondrial diseases12. Furthermore, increased serum levels of GDF-15 have been detected in several muscle-related conditions such as sarcopenia, autoimmune and viral myositis, as a part of tissue stress response34. Whether the induction of GDF-15 primarily benefits or detrimentally affects muscle recovery remains unclear, as this stress-responsive cytokine can activate very different pathogenetic pathways, resulting in fibrotic changes and myoblast proliferation34. Analogous to mitochondrial disease, in ATTRv, a redox imbalance effect underlying tissue damage caused by the deposition of misfolded and aggregated proteins can be hypothesized. Notably, results of in vitro studies with Schwannoma cell lines suggest that aggregated TTR stimulates the production of reactive oxygen species, leads to lower levels of endogenous antioxidants, and decreases overall cellular antioxidant capacity35,36. The relationship of mitochondrial DNA and TTR mutations is intriguing, as reported in a patient with mitochondrial myopathy and pathogenic TTR variant in which multiple mitochondrial DNA deletions have been detected in muscle biopsy37.
Our data documented higher levels of GDF-15 in ATTRv subjects compared to healthy controls, supporting a potential role of GDF-15 in the diagnostic work-up. However, no differences were observed in terms of GDF-15 levels stratifying ATTRv patients based on genotype, clinical phenotype, and clinical scales used to assess disease severity and progression. This underscores the necessity of integrating serologic testing with comprehensive clinical evaluation, neurophysiological assessments, and imaging studies to achieve precise patient stratification. In contrast to the finding of Okada and colleagues, our study found no correlation between GDF-15 levels and other traditional cardiac biomarkers. This discrepancy may be attributed to the composition of our cohort, where no patient presented with a pure cardiological phenotype but rather with an exclusively neuropathic or mixed phenotype, in which cardiac involvement is less pronounced.
Umod, also known as Tamm-Horsfall protein, is the most abundant urinary protein, primarily produced by tubular cells in the thick ascending limb of the loop of Henle and to a lesser extent in the distal kidney tubule. Present in the urine in large aggregates, Umod serves several important physiological functions and is known for its immunoregulatory properties, involvement in protecting against urinary tract infections and kidney stone formation, and regulation of ion transportation38. While tubular cells express Umod primarily at the apical membrane, it is also found to a lesser extent at the basal membrane, contributing to its presence at very low concentrations in the blood39. Umod has been evaluated as a biomarker of tubular function in healthy individuals and dysfunction of tubular cells in patients with kidney disease40. The relationship between the urinary Umod excretion and glomerular filtration remains controversial, with some studies showing positive correlations while others do not41. In multivariate analyses, spot Umod concentration and 24-h Umod excretion have shown linear and positive associations with eGFR42. Even in healthy subjects, serum Umod concentrations correlate with urinary Umod excretion, although Umod concentrations in urine are approximately 1000-fold higher than those in serum43. Previous studies have demonstrated that serum Umod decreases with declining kidney function, with positive correlations between serum Umod levels and eGFR observed in patients across chronic kidney disease stages 1–5, those with chronic obstructive nephropathy, and healthy people aged ≥ 60 years44,45,46.
In our cohort, mean serum Umod values were lower in patients with ATTRv compared with healthy controls. These data support the use of serum Umod measurements in addition to eGFR, which is already a validated marker for cardiac amyloidosis according to the Gillmore staging system16. A positive correlation was found between serum Umod levels and eGFR based on the 2021 CKD-EPI creatinine-cystatin C equation, while an inverse correlation was found with cystatin C levels, in line with the results of other studies14,44,45,,46. The relationship of GDF-15 and Umod with the cystatin C-related equation appears to be determined by cystatin C itself, given its inverse relationship with eGFR. The lack of relationship between GDF-15 and Umod with eGFR based on creatinine alone suggests differential glomerular filtration results using the two different equations in this cohort. Cystatin C-based eGFR equations may provide more accurate estimations of glomerular filtration in patients with body weight loss and muscle wasting, such as those with ATTRv. This discrepancy highlights the potential for creatinine alone to overestimate glomerular filtration in these patients, impacting drug indications related to eGFR47.
No correlation was demonstrated between Umod levels and traditional cardiac biomarkers, and no difference was observed stratifying ATTRv patients based on genotype, clinical phenotype, or disease severity. As for GDF-15, this result may be explained by our cohort not including patients with pure cardiomyopathy or, alternatively, by the mild or sub-clinical renal involvement in late-onset ATTRv3,48.
Furthermore, our study is limited due to the small number of patients recruited and because the patient and control groups are not balanced with respect to age and sex. Patients with ATTRv were older than healthy controls, and the male-to-female ratio was different between the two groups.
Conclusions
The data reported here result from preliminary investigations of a large study aimed at characterizing and validating disease biomarkers in ATTRv (ClinicalTrials.gov ID: NCT05929209). Specifically, the results suggest that modifications in serum levels of GDF-15 and Umod are characteristic of ATTRv amyloidosis. Larger and longitudinal studies, including patients with more pronounced, if not exclusive, cardiac involvement, are needed to determine whether these markers can be used in clinical settings in addition to those already validated to assess disease severity and treatment response.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Adams, D., Koike, H., Slama, M. & Coelho, T. Hereditary transthyretin amyloidosis: A model of medical progress for a fatal disease. Nat. Rev. Neurol. 15, 387–404. https://doi.org/10.1038/s41582-019-0210-4 (2019).
Manganelli, F. et al. Hereditary transthyretin amyloidosis overview. Neurol. Sci. 43, 595–604. https://doi.org/10.1007/s10072-020-04889-2 (2022).
Ferraro, P. M. et al. Renal involvement in hereditary transthyretin amyloidosis: An Italian single-centre experience. Brain Sci. 11, 980. https://doi.org/10.3390/brainsci11080980 (2021).
Minnella, A. M. et al. Ocular involvement in hereditary transthyretin amyloidosis: A case series describing novel potential biomarkers. Genes (Basel) 12, 927. https://doi.org/10.3390/genes12060927 (2021).
Luigetti, M. et al. Gastrointestinal manifestations in hereditary transthyretin amyloidosis: A single-centre experience. J. Gastrointestin. Liver Dis. 29, 339–343. https://doi.org/10.15403/jgld-2474 (2020).
Luigetti, M. et al. Serum inflammatory profile in hereditary transthyretin amyloidosis: Mechanisms and possible therapeutic implications. Brain Sci. 12, 1708. https://doi.org/10.3390/brainsci12121708 (2022).
Luigetti, M. et al. A metabolic signature of hereditary transthyretin amyloidosis: A pilot study. Int. J. Mol. Sci. 23, 16133. https://doi.org/10.3390/ijms232416133 (2022).
Wang, D. et al. GDF15: Emerging biology and therapeutic applications for obesity and cardiometabolic disease. Nat. Rev. Endocrinol. 17, 592–607. https://doi.org/10.1038/s41574-021-00529-7 (2021).
George, M., Jena, A., Srivatsan, V., Muthukumar, R. & Dhandapani, V. E. GDF 15–a novel biomarker in the offing for heart failure. Curr. Cardiol. Rev. 12, 37–46. https://doi.org/10.2174/1573403x12666160111125304 (2016).
Wollert, K. C., Kempf, T. & Wallentin, L. Growth differentiation factor 15 as a biomarker in cardiovascular disease. Clin. Chem. 63, 140–151. https://doi.org/10.1373/clinchem.2016.255174 (2017).
Kim, D. et al. Prognostic values of novel biomarkers in patients with AL amyloidosis. Sci. Rep. 9, 12200. https://doi.org/10.1038/s41598-019-48513-6 (2019).
Lin, Y. et al. Accuracy of FGF-21 and GDF-15 for the diagnosis of mitochondrial disorders: A meta-analysis. Ann. Clin. Transl. Neurol. 7, 1204–1213. https://doi.org/10.1002/acn3.51104 (2020).
Mizdrak, M., Kumrić, M., Kurir, T. T. & Božić, J. Emerging biomarkers for early detection of chronic kidney disease. J. Pers. Med. 12, 548. https://doi.org/10.3390/jpm12040548 (2022).
Leiherer, A. et al. The value of uromodulin as a new serum marker to predict decline in renal function. J. Hypertens. 36, 110–118. https://doi.org/10.1097/HJH.0000000000001527 (2018).
Luigetti, M. et al. Sudoscan in the evaluation and follow-up of patients and carriers with TTR mutations: Experience from an Italian Centre. Amyloid 25, 242–246. https://doi.org/10.1080/13506129.2018.1545640 (2018).
Gillmore, J. D. et al. A new staging system for cardiac transthyretin amyloidosis. Eur. Heart J. 39, 2799–2806. https://doi.org/10.1093/eurheartj/ehx589 (2018).
Desmedt, S. et al. Growth differentiation factor 15: A novel biomarker with high clinical potential. Crit. Rev. Clin. Lab. Sci. 56, 333–350. https://doi.org/10.1080/10408363.2019.1615034 (2019).
Kempf, T. et al. The transforming growth factor-beta superfamily member growth-differentiation factor-15 protects the heart from ischemia/reperfusion injury. Circ. Res. 98, 351–360. https://doi.org/10.1161/01.RES.0000202805.73038.48 (2006).
Clerk, A., Kemp, T. J., Zoumpoulidou, G. & Sugden, P. H. Cardiac myocyte gene expression profiling during H2O2-induced apoptosis. Physiol. Genomics 29, 118–127. https://doi.org/10.1152/physiolgenomics.00168.2006 (2007).
Frank, D. et al. Gene expression pattern in biomechanically stretched cardiomyocytes: Evidence for a stretch-specific gene program. Hypertension 51, 309–318. https://doi.org/10.1161/HYPERTENSIONAHA.107.098046 (2008).
Widera, C. et al. Identification of follistatin-like 1 by expression cloning as an activator of the growth differentiation factor 15 gene and a prognostic biomarker in acute coronary syndrome. Clin. Chem. 58, 1233–1241. https://doi.org/10.1373/clinchem.2012.182816 (2012).
Wang, F. et al. Growth differentiation factor 15 in different stages of heart failure: potential screening implications. Biomarkers 15, 671–676. https://doi.org/10.3109/1354750X.2010.510580 (2010).
Kempf, T. et al. Prognostic utility of growth differentiation factor-15 in patients with chronic heart failure. J. Am. Coll. Cardiol. 50, 1054–1060. https://doi.org/10.1016/j.jacc.2007.04.091 (2007).
Kempf, T. et al. Growth-differentiation factor-15 for risk stratification in patients with stable and unstable coronary heart disease: Results from the AtheroGene study. Circ. Cardiovasc. Genet. 2, 286–292. https://doi.org/10.1161/CIRCGENETICS.108.824870 (2009).
Eggers, K. M. et al. Relations of growth-differentiation factor-15 to biomarkers reflecting vascular pathologies in a population-based sample of elderly subjects. Scand. J. Clin. Lab. Investig. 72, 45–51. https://doi.org/10.3109/00365513.2011.626072 (2012).
Lok, D. J. et al. Incremental prognostic power of novel biomarkers (growth-differentiation factor-15, high-sensitivity C-reactive protein, galectin-3, and high-sensitivity troponin-T) in patients with advanced chronic heart failure. Am. J. Cardiol. 112, 831–837. https://doi.org/10.1016/j.amjcard.2013.05.013 (2013).
Kastritis, E. et al. Growth differentiation factor-15 is a new biomarker for survival and renal outcomes in light chain amyloidosis. Blood 131, 1568–1575. https://doi.org/10.1182/blood-2017-12-819904 (2018).
Okada, M. et al. Plasma growth differentiation factor 15: A novel tool to detect early changes of hereditary transthyretin amyloidosis. ESC Heart Fail. 8, 1178–1185. https://doi.org/10.1002/ehf2.13176 (2021).
Tsai, V. W. W., Husaini, Y., Sainsbury, A., Brown, D. A. & Breit, S. N. The MIC-1/GDF15-GFRAL pathway in energy homeostasis: Implications for obesity, cachexia, and other associated diseases. Cell Metab. 28, 353–368. https://doi.org/10.1016/j.cmet.2018.07.018 (2018).
Patel, S. et al. GDF15 provides an endocrine signal of nutritional stress in mice and humans. Cell Metab. 29, 707-718 e708. https://doi.org/10.1016/j.cmet.2018.12.016 (2019).
Nikkanen, J. et al. Mitochondrial DNA replication defects disturb cellular dNTP pools and remodel one-carbon metabolism. Cell Metab. 23, 635–648. https://doi.org/10.1016/j.cmet.2016.01.019 (2016).
Suomalainen, A. & Battersby, B. J. Mitochondrial diseases: The contribution of organelle stress responses to pathology. Nat. Rev. Mol. Cell Biol. 19, 77–92. https://doi.org/10.1038/nrm.2017.66 (2018).
Southwell, N. et al. A coordinated multiorgan metabolic response contributes to human mitochondrial myopathy. EMBO Mol. Med. 15, e16951. https://doi.org/10.15252/emmm.202216951 (2023).
De Paepe, B. The cytokine growth differentiation factor-15 and skeletal muscle health: Portrait of an emerging widely applicable disease biomarker. Int. J. Mol. Sci. 23, 13180. https://doi.org/10.3390/ijms232113180 (2022).
Sousa, M. M. et al. Familial amyloid polyneuropathy: Receptor for advanced glycation end products-dependent triggering of neuronal inflammatory and apoptotic pathways. J. Neurosci. 21, 7576–7586. https://doi.org/10.1523/JNEUROSCI.21-19-07576.2001 (2001).
Fong, V. H. & Vieira, A. Pro-oxidative effects of aggregated transthyretin in human Schwannoma cells. Neurotoxicology 39, 109–113. https://doi.org/10.1016/j.neuro.2013.08.013 (2013).
Luigetti, M. et al. Progressive axonal polyneuropathy in a mitochondrial disorder: An uncommon association with familial amyloid neuropathy. Amyloid 25, 261–262. https://doi.org/10.1080/13506129.2018.1506919 (2018).
Devuyst, O., Olinger, E. & Rampoldi, L. Uromodulin: From physiology to rare and complex kidney disorders. Nat. Rev. Nephrol. 13, 525–544. https://doi.org/10.1038/nrneph.2017.101 (2017).
Sikri, K. L., Foster, C. L., MacHugh, N. & Marshall, R. D. Localization of Tamm-Horsfall glycoprotein in the human kidney using immuno-fluorescence and immuno-electron microscopical techniques. J. Anat. 132, 597–605 (1981).
Ix, J. H. & Shlipak, M. G. The promise of tubule biomarkers in kidney disease: a review. Am. J. Kidney Dis. 78, 719–727. https://doi.org/10.1053/j.ajkd.2021.03.026 (2021).
O’Seaghdha, C. M. et al. Analysis of a urinary biomarker panel for incident kidney disease and clinical outcomes. J. Am. Soc. Nephrol. 24, 1880–1888. https://doi.org/10.1681/ASN.2013010019 (2013).
Pruijm, M. et al. Associations of urinary uromodulin with clinical characteristics and markers of tubular function in the general population. Clin. J. Am. Soc. Nephrol. 11, 70–80. https://doi.org/10.2215/CJN.04230415 (2016).
Dawnay, A. B. & Cattell, W. R. Serum Tamm-Horsfall glycoprotein levels in health and in renal disease. Clin. Nephrol. 15, 5–8 (1981).
Fedak, D. et al. Serum uromodulin concentrations correlate with glomerular filtration rate in patients with chronic kidney disease. Pol. Arch. Med. Wewn. 126, 995–1004. https://doi.org/10.20452/pamw.3712 (2016).
Risch, L. et al. The serum uromodulin level is associated with kidney function. Clin. Chem. Lab. Med. 52, 1755–1761. https://doi.org/10.1515/cclm-2014-0505 (2014).
Vukmirović Papuga, M. et al. Serum uromodulin, a potential biomarker of tubulointerstitial damage, correlates well with measured GFR and ERPF in patients with obstructive nephropathy. Medicina (Kaunas) 58, 1729. https://doi.org/10.3390/medicina58121729 (2022).
D’Ambrosio, V., Ferraro, P. M., Guglielmino, V. & Luigetti, M. Kidney involvement in hereditary transthyretin amyloidosis: Is there a role for cystatin C?. Clin. Kidney J. 16, 397–398. https://doi.org/10.1093/ckj/sfac156 (2023).
Luigetti, M. et al. Trajectories of kidney function in patients with ATTRv treated with gene silencers. Genes (Basel) 13, 2236. https://doi.org/10.3390/genes13122236 (2022).
Acknowledgements
Marco Luigetti, Angela Romano, Serenella Servidei, and Guido Primiano are members of the European Reference Network for Neuromuscular Diseases—Project ID No 870177. An Italian Ministry of Health Young Researcher Project Grant (GR-2021-12372306 to A.R. and G.P.) contributed towards the preparation of this research. The authors thank Ray Hill, an independent medical writer, and Carmen Innes of Springer Healthcare Communications who provided native-English editing and styling assistance on this manuscript prior to submission. This work was unconditionally funded by Sobi Srl, Milan, Italy.
Author information
Authors and Affiliations
Contributions
ML, FV, AR, GP conceived and designed the study. All Authors contributed to the acquisition and analysis of the data. ML, FV, AR, GP drafted a substantial portion of the original manuscript. All authors participated in the editing and critical review of the manuscript and read and approved the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
M. Luigetti received financial grants (honoraria and speaking) from Ackea, Alnylam, Sobi, and Pfizer and travel grants from Ackea, Alnylam, Sobi, Pfizer, Kedrion, and Grifols. A. Romano received financial grants (honoraria and speaking) from Akcea and travel grants from Akcea, Alnylam, Pfizer, and Csl Behring. P. M. Ferraro received grants/consultant fees from Allena Pharmaceuticals, Alnylam, Amgen, AstraZeneca, BioHealth Italia, Gilead, Otsuka Pharmaceuticals, and Vifor Fresenius. Guido Primiano received financial grants (honoraria and speaking) from Sanofi. The other authors have no conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Luigetti, M., Vitali, F., Romano, A. et al. Emerging multisystem biomarkers in hereditary transthyretin amyloidosis: a pilot study. Sci Rep 14, 18281 (2024). https://doi.org/10.1038/s41598-024-69123-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-69123-x