Abstract
To investigate long-term outcomes and develop a risk model for pathological multi–station N2 (pN2b) in patients who underwent upfront surgery for clinical single–station N2 (cN2a) non–small cell lung cancer (NSCLC). From 2006 to 2018, 547 patients who had upfront surgery for suspected cN2a NSCLC underwent analysis. A risk model for predicting pN2b metastasis was developed using preoperative clinical variables via multivariable logistic analysis. Among 547 clinical cN2a NSCLC patients, 118 (21.6%), 58 (10.6%), and 371 (67.8%) had pN0, pN1, and pN2. Among 371 pN2 NSCLC patients, 77 (20.8%), 165 (44.5%), and 129 (34.7%) had pN2a1, pN2a2, and pN2b. The 5-year overall survival rates for pN2a1 and pN2a2 were significantly higher than for pN2b (p = 0.041). Histologic type (p < 0.001), age ≤ 50 years (p < 0.001), preoperatively confirmed N2 metastasis (p < 0.001), and clinical stage IIIB (vs. IIIA) (p = 0.003) were independent risk factors for pN2b metastasis. The risk scoring system based on this model demonstrated good discriminant ability for pN2b disease (area under receiver operating characteristic: 0.779). In cN2a NSCLC patients, those with multiple N2 metastases indicate worse prognosis than those with a single N2 metastasis. Our risk scoring system effectively predicts pN2b in these patients.
Similar content being viewed by others
Introduction
Surgical resection is an uncommon treatment option for patients with non-small cell lung cancer (NSCLC) with mediastinal lymph node (LN) metastasis (cN2) because N2 metastasis indicates systemic disease1. When cN2 is confirmed before surgical resection, the treatment approach is definitive concurrent chemoradiotherapy, using platinum-based chemotherapy, plus full-dose radiotherapy (RTx), or induction chemotherapy followed by surgery1,2. Although many researchers have conducted clinical trials of induction chemotherapy or chemoradiotherapy followed by surgery since the 1990s, the role of surgery in the multimodal approach is still controversial3,4,5.
In 2015, the International Association for the Study of Lung Cancer (IASLC) proposed the subdivision of pathological N1 (pN1) and pN2 group patients who have a heterogeneous prognosis, which was made by considering the number of LN metastasis and its location6. Minimal N2 disease, especially skipped single station N2 disease without N1 involvement (N2a1), had a prognosis similar to multi-station N1 disease (N1b), a locally advanced disease. Therefore, it is unclear whether upfront surgery can improve prognosis in a subset of cN2 diseases, including single-station N2 (cN2a) disease. Previous studies exist on upfront surgery for patients with cN2a NSCLC. According to the studies, the rate of skipped N2 metastasis was reported up to 30% in patients with N2 NSCLC, which showed a favorable prognosis7,8,9,10. However, those studies have limitations in that they were simple descriptive reports on surgical outcomes7,11,12. Thus, it is still unclear which patients with cN2a will benefit from upfront surgery.
This study aimed to investigate long-term survival outcomes after upfront surgery and develop a risk model for pathological multiple station N2 (pN2b) metastasis in patients with cN2a NSCLC after complete resection.
Materials and methods
Patients
All clinical records of patients who underwent surgery for NSCLC in the Thoracic Surgery Department at Asan Medical Center in Seoul, South Korea, between 2006 and 2018 were retrospectively collected. The inclusion criteria were as follows: (1) Presence of a single N2 node (regardless of N1 node) on chest computed tomography (CT), with ≥ 10 mm on the largest short axis; (2) Fluorodeoxyglucose (FDG) uptake is higher than that of the mediastinal blood pool on positron emission tomography (PET-CT); and (3) Invasive mediastinal staging was not performed routinely but only targeted for suspected LN (lymph node) involvement. Among the patients (n = 961), the following patients were excluded: (1) Patients with other malignant diseases (n = 80); (2) Patients who received neoadjuvant chemotherapy (n = 203); (3) Patients who underwent open and close procedures (n = 26); (4) Patients who did not undergo lymph node dissection or had incomplete lymph node dissection (number of resected LNs < 6) (n = 98); and (5) Patients who died within 30 days after surgery (n = 7) (Fig. 1). Among them, single station N2 node metastasis was clinically suspected in 547 patients using imaging modalities, such as chest CT or PET-CT included as the final cohort (cN2a) in our study.
The study was approved by the Institutional Review Board of Asan Medical Center, and this center waived the need for informed consent (Study no: 2023–0345, Date of approval: 2023–03-22). All study procedures were performed in accordance with relevant guidelines and regulations.
Preoperative staging and postoperative management
Patient workups for diagnosis, staging, and surgical resection were performed according to well-established, widely accepted protocols13. The following definition of cN2a disease was used: enlarged LN (≥ 10 mm on the largest short axis) on chest CT or PET-positive LNs in single N2 node, according to the Mountain–Dresler modification of the American Thoracic Society14 through 2008 and the IASLC LN map after 200815. LNs were considered positive on PET scans if FDG uptake was higher than the background uptake in the mediastinal blood pool. Mediastinal LN biopsy was not routinely performed in these patients, and when performed, suspicious nodes were selectively confirmed with mediastinoscopy, endobronchial ultrasound, or endoscopic ultrasound. In the case of a borderline size or metabolic uptake of mediastinal LNs on CT or PET scan, mediastinal LN biopsy was conducted to confirm metastasis. Even if the suspected N2 LNs were confirmed to have no malignancy in invasive procedures, these patients were included in this study according to the definition of cN2a disease. The treatment approaches for cN2a disease were determined by a multidisciplinary team, including professional medical oncologists, radiologists, and thoracic surgeons. For cN2a disease, upfront surgery was usually considered if the following criteria were met: (1) the primary tumor could be resected without the need for pneumonectomy, (2) the involved LNs were distinct from the surrounding tissues and < 3.0 cm, and (3) CT or PET scans showed no extra-nodal tumor invasion (full thickness LN capsular invasion or tumor extension beyond the LN capsule).
According to the multidisciplinary team’s assessment, adjuvant chemotherapy (CTx) was recommended for all patients with pN2 disease, except those aged ≥ 75 years or in poor physical condition. Systemic CTx with a platinum-based regimen was recommended with four treatment cycles over 4–6 weeks postoperatively. Since 2008, when targeted treatment became prevalent for patients with active mutations in the epidermal growth factor receptor, tyrosine kinase inhibitors have been mainly used in cases of recurrence after adjuvant CTx. For adjuvant radiotherapy (RTx), 1.8 Gy was administered daily, reaching a total dose of 50.4 Gy for patients with complete resection or 55–60 Gy for patients with positive resection margins.
Follow-up data were collected at regular intervals, including visits every 3 months for the first 2 years after surgery, every 6 months for the next 3 years, and annually thereafter. Patient records were reviewed during these clinic visits. Chest CT was performed as part of routine follow-up visits, and PET-CT was additionally performed when disease recurrence was clinically suspected. In the case of disease recurrence, treatment modalities, and chemotherapy decisions were made based on the judgment of the attending physician.
Statistical analysis
Overall survival (OS) is the interval between the date of operation and the date of death, determined by reviewing the Korean National Security Death Index Database records. Freedom from recurrence was calculated as the time between the date of the operation and the date of recurrence. However, patients without recurrence were censored at the most recent time point known to be recurrence-free. The probability of survival was calculated by using the Kaplan–Meier method and assessed using the log-rank test.
Logistic regression analyses were conducted to assess both univariable and multivariable models, aimed at identifying potential risk factors associated with pN2. The clinical variables included in the analysis comprised age, sex, comorbidity, forced expiratory volume, diffusing capacity of the lungs for carbon monoxide, smoking history, histology, preoperatively confirmed N2 status, subclinical node stage, and clinical staging. The final multivariable model was determined using a systematic backward elimination approach, with variables entering the model at a significance level of p ≤ 0.10 and being retained if their significance level remained at p ≤ 0.05. To quantify the uncertainty surrounding the odds ratios (ORs), bootstrap resampling methods were employed, generating 1,000 sets of bootstrap sampling weights. This facilitated the calculation of 95% confidence intervals (CIs) for the ORs. Calibration of the multivariable logistic regression model was evaluated using the Hosmer–Lemeshow test. Discriminative ability was assessed by presenting the area under the receiver operating characteristic curve (AUROC) as a statistical measure. For risk assessment, a scoring system was established by assigning proportional weights to predictor estimates, with the smallest coefficient receiving a value of 1. The final risk model underwent internal validation to ensure its reliability and generalizability. To facilitate interpretation, optimal cutoff points for continuous variables were determined based on the highest Youden index score, considering both sensitivity and specificity. All the statistical computations were carried out using R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria), with various packages, including Survival, ggplot2, GGally, survminer, pROC, and rms.
Ethical approval
The study was approved by the Institutional Review Board of Asan Medical Center, and this center waived the need for informed consent (Study no: 2023–0345, Date of approval: 2023–03-22).
Results
Baseline patient characteristics
Pathological staging was pN0 and pN1 in 176 (32.2%) patients with cN2a NSCLC (n = 547) after surgery. Among the patients with pN2, there were 77 (14.1%), 165 (30.2%), and 165 (30.2%) patients with pN2a1, pN2a2, and pN2b, respectively (Fig. 1).
Table 1 shows the clinicopathological characteristics of the patients included in this study (n = 547). The median age was 63.1 years, and 434 (79.3%) patients were men. The histologic types included adenocarcinoma (n = 242, 44.2%), squamous cell carcinoma (n = 261, 47.7%), and others (n = 44, 8.0%). Before surgery, 125 (22.9%) patients had N2 LNs using biopsy while 34 patients (6.2%) had have N2 negative LN using biopsy; pathologic N staging details for these patients are presented in Supplementary Fig. 1. Mediastinal LN evaluation was performed in 128 (23.4%) patients using an endobronchial ultrasound scan, two (0.4%) patients using an endoscopic ultrasound scan, and 29 (5.3%) patients using mediastinoscopy. The median size of the cancer was 42.4 mm. Surgical procedures included segmentectomy (n = 4, 0.7%), lobectomy (n = 405, 74%), bilobectomy (n = 65, 11.9%), pneumonectomy (n = 45, 8.2%), and sleeve lobectomy (n = 28, 5.1%) and R0 surgery was achieved in 478 (87.4%) patients. In terms of age, a greater proportion of patients in the N2a group were aged over 50 compared to the N2b group (90.5% vs 6.7%). In the N2a group, there was a higher prevalence of patients with a smoking history (82.2% vs. 67.4%). Additionally, squamous cell carcinoma was less common in the N2b group (46.3% vs. 20.2%), while adenocarcinoma was more prevalent (45.0% vs. 72.9%). Furthermore, a larger proportion of patients in the N2b group had undergone invasive N2 lymph node biopsy (30.2% vs. 41.1%). Consequently, the number of diagnosed patients was also higher in the N2b group (28.1% vs. 41.1%). In terms of clinical T-staging, it was evident that N2b patients were more advanced.
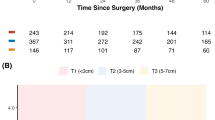
Survival analysis
The 5-year OS rate was 49.2%, and the 5-year recurrence-free survival (RFS) rate was 44.5% (Fig. 2). The 5-year OS rates for cIIIA and cIIIB were 52.5% and 43%, respectively (p = 0.04), and the 5-year RFS rates were 50.5% and 36%, respectively (p = 0.001). In the comparison between clinical sub-N staging and pathologic sub N staging, the 5-year OS rates for cN2a1 and cN2a2 were 50.1% and 48%, respectively (p = 0.5), and the 5-year OS rates for pN2a1, pN2a2, and pN2b were 51.2%, 45.8%, and 29%, respectively (p = 0.03) (Fig. 3A). Figure 3 shows that no difference in survival rate was observed between pN2a1 and pN2a2; however, two groups (pN2a1 and pN2a2) and pN2b had significantly different survival rates (p = 0.041). Similarly, a significant difference was observed between pN2a1, pN2a2, and pN2b in the RFS (p = 0.03) (Fig. 3B).
Risk factors for pN2b metastasis
We performed univariable and multivariable logistic regression analyses to establish a risk model for predicting pN2b disease (Table 2). According to the multivariable analysis, age ≤ 50 years (OR: 2.76, 95% CI: 1.55–4.93, p < 0.0001), adenocarcinoma (OR: 4.74, 95% CI: 2.87–8.03, p < 0.0001), other histology (OR: 1.85, 95% CI: 0.73–4.35, p = 0.17), preoperatively confirmed N2 metastasis (OR: 3.2, 95% CI: 1.98–5.18, p < 0.0001) and clinical stage IIIB (OR: 2.04, 95% CI: 1.29–3.23, p = 0.002) were independent predictors for pN2b disease. The formula for the aggregate score for mortality is (2.5 × adenocarcinoma) + (1 × other histology type) + (1.5 × age ≤ 50 years) + (2 × preoperatively confirmed N2 metastasis) + (1 × clinical stage IIIB). The rate of pathologic N2b metastasis gradually increased as the risk score increased (Fig. 4A). The AUROC for this risk-scoring system was 0.776 (95% CI: 0.729–0.817) (Fig. 4B). According to the risk score, the diagnosis rate from cN2a to pN2b was significantly increased. In groups with high-risk scores (7–8 points), the rate of pN2b disease was diagnosed in approximately 62.5%, compared to 13.4% in those with low-risk scores (0–1 points) (p < 0.001).
Discussion
This study evaluated the long-term prognosis of patients with clinically single N2 NSCLC with 49.2% of 5-year OS and 44.5% of RFS. According to our results, patients with pN2b had a significantly poorer prognosis than those with pN2a1 and pN2a2, even in some patients with cN2a NSCLC. Using preoperative clinical variables, we developed a risk-scoring system for predicting the probability of multiple N2 metastasis in patients with cN2a, which showed excellent discriminant ability (AUROC: 0.773). To the best of our knowledge, this scoring system is the first to present a risk model for postoperative pN2b among cN2a patients, using a sufficient number of patients at a single institution.
The IASLC demonstrated a significant decrease in OS in the order of N2a1, N2a2, and N2b, which was also shown similarly in another cohort6,16. Using our cohort, we also reported that stratification according to the N2 subclassification proposed by the IASLC is prognostically appropriate for patients with pathologically confirmed N2 NSCLC17. However, no significant difference was observed in survival outcomes between cN2a1 and cN2a2 (5-year OS 50.1% vs. 48.2%, p = 0.48), which might be due to the inaccuracy of clinical staging. When survival outcomes were analyzed according to pN2a1, pN2a2, and pN2b, no significant difference was observed between patients with pN2a1 and pN2a2 (5-year OS: 51.1% vs. 45.8%, p = 0.509). This finding is probably a result of the selection bias that occurred by including only patients with clinical single station N2 NSCLC in the study rather than overall N2 NSCLC. Patients with pN2b (5-year OS: 29.0%) had significantly worse OS than those with pN2a1 (51.1%, p = 0.041) and pN2a2 (45.8%, p = 0.041) in patients with cN2a NSCLC. Thus, we developed a risk model for predicting pN2b metastasis in patients with cN2a NSCLC after complete resection. The ninth edition of the staging system for NSCLC also reflects this by distinguishing and consistently discriminating subgroups in patients with N2 disease; specifically between single-station involvement (N2a) and multiple-station involvement (N2b)18.
According to our risk model for pN2b in patients with cN2a NSCLC, age ≤ 50 years, histologic type, preoperatively confirmed N2 metastasis, and clinical stage IIIB were identified as independent risk factors. Hyun Sung Chung et al.19 showed that younger age (< 60 years and 60–70 years) was one of the risk factors for pN2-3 disease diagnosed by Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration (EBUS-TBNA) or surgery. In our study, younger age (≤ 50 years) was also a risk factor for multiple N2 metastases when single N2 metastasis was suspected on imaging modality (OR: 2.76, CI: 1.55–4.92, p = 0.0006). It is well-known that older age is a risk factor for survival in most cancers20,21. Thus, aggressive multimodal treatment, including surgery, seems more available and effective for younger patients. However, Minami et al.22 reported that the positive prognostic impact of younger age was present only in early-stage NSCLC and was absent in advanced-stage NSCLC which is consistent with our findings. In our study, the 5-year postoperative survival rate for cN2 patients was 48.5% in patients over 50 years, compared to 54.1% in patients 50 years old or younger (p = 0.3). This suggests that aggressive surgical treatment for advanced NSCLC, especially for patients with cN2a, should be should be determined cautiously even in young patients.
Several studies have compared long-term outcomes between adenocarcinoma (ADC) and squamous cell carcinoma (SqCC) but failed to obtain consistent results23,24,25. Recently, in a study based on surveillance, epidemiology, and results database, Grosu et al. demonstrated that among patients with surgically resected stage I NSCLC, those with ADC had a lower risk of death than those with SqCC26. However, in patients with stage II and III NSCLC, we reported that ADC had a higher risk of recurrence than SqCC, with no difference in OS27. The distribution of histological types across stages was also different between ADC and SqCC. A large database showed that most patients with ADC were diagnosed at clinical stage IV (46%), whereas only 30% of patients with SqCC were diagnosed at clinical stage IV28. Additionally, patients with ADC tend to have earlier clinical T staging than patients with SqCC, whereas patients with ADC tend to have more metastasis tendencies than those with SqCC24,29. In this study, the histologic type (ADC vs. SqCC) (OR: 4.74, 95% CI: 2.87–8.03, p < 0.001) and clinical stage (IIIB vs. cIIIA) (OR: 2.04, 95% CI: 1.29–3.23, p = 0.002) were risk factors for multiple N2 metastasis in patients with clinical single N2 metastasis. Therefore, if a single N2 LN metastasis is suspected in patients with ADC and ≥ T3, the treatment strategy should be determined considering the possibility of multiple N2 node metastasis.
Enhanced CT and PET-CT are useful diagnostic tools for detecting LN metastasis; however, the sensitivity is unsatisfactory30. A meta-analysis assessed the agreement between clinical N stage and pathologic N stage, and the relationship between cN2 and pN2 was 67% (104/155). In addition, this study showed that clinically over-staged patients (cN2, pN0–1) account for 30% (47/155), which could benefit from the surgery31,32. Herein, 176 (32.2%) patients with clinical single N2a NSCLC were down-staged to pN0 and pN1 after surgery. These results imply that invasive mediastinal staging should be performed before surgery for cN2 NSCLC suspected on imaging modalities such as contrast-enhanced CT and PET-CT. However, the strategy for treating resectable cN2 NSCLC in our hospital was upfront surgery followed by adjuvant therapy13. Based on this strategy, many patients with cN2 NSCLC skipped mediastinal LN biopsy on the premise that the treatment regimen is not changed, and even when surgery is performed, suspicious nodes were confirmed selectively rather than systemically. Recently, as EBUS has become common and poor surgical outcomes have been reported for multiple N2 NSCLC, we routinely perform systemic mediastinal lymph node biopsy for cN2 NSCLC at our hospital.
This study has several limitations. (1) The retrospective nature of the analysis introduces inherent selection bias, given its reliance on observational data from a single institution. (2) Including a relatively small sample size within specific subgroups could mask significant differences, making some findings statistically insignificant. (3) Given that the data exclusively encompass surgery patients, the survival curves may diverge from those with a higher population of patients with NSCLC. Despite conducting internal validation with an independent dataset from our institution, external validation using data from other centers has yet to be performed on our model. A prospective, multicenter, randomized controlled study is imperative to overcome these limitations and substantiate our findings.
Among patients with clinical single-station N2 NSCLC, those with pN2b disease had significantly worse prognoses than those with pN2a1 and pN2a2. Our risk scoring system using a large volume of patient data for predicting pN2b has good discriminant ability in patients with clinical single-station N2 NSCLC. We believe that this scoring system will assist clinicians in selecting the appropriate treatment plan for a diverse group of patients with clinical single N2 NSCLC.
Data availability
The databases used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- LN:
-
Lymph node
- RTx:
-
Radiation therapy
- CTx:
-
Chemotherapy
- OS:
-
Overall survival
- AUROC:
-
Area under the receiver operating characteristic curve
- ADC:
-
Adenocarcinoma
- SqCC:
-
Squamous cell carcinoma
- OR:
-
Odds ratio
- DLCO:
-
Diffusing capacity of the lungs for carbon monoxide
- EBUS:
-
Endobronchial ultrasound scan
- EUS:
-
Endoscopic ultrasound scan
- FEV1:
-
Forced expiratory volume
- VATS:
-
Video-assisted thoracoscopic surgery
References
Ettinger, D. S. et al. Non-small cell lung cancer, Version 3.2022, NCCN Clinical practice guidelines in oncology. J. Natl. Compr. Canc. Netw. 20(5), 497–530 (2022).
in 2019 exceptional surveillance of lung cancer: Diagnosis and management (NICE guideline NG122). 2019.
Watanabe, Y. et al. Aggressive surgical intervention in N2 non-small cell cancer of the lung. Ann. Thorac. Surg. 51(2), 253–261 (1991).
Rosell, R. et al. A randomized trial comparing preoperative chemotherapy plus surgery with surgery alone in patients with non-small-cell lung cancer. N. Engl. J. Med. 330(3), 153–158 (1994).
Choi, N. C. et al. Potential impact on survival of improved tumor downstaging and resection rate by preoperative twice-daily radiation and concurrent chemotherapy in stage IIIA non-small-cell lung cancer. J. Clin. Oncol. 15(2), 712–722 (1997).
Asamura, H. et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the N Descriptors in the Forthcoming 8th edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 10(12), 1675–1684 (2015).
Hishida, T. et al. Surgical outcomes after initial surgery for clinical single-station N2 non-small-cell lung cancer. Jpn. J. Clin. Oncol. 44(1), 85–92 (2014).
Riquet, M. et al. Skip mediastinal lymph node metastasis and lung cancer: A particular N2 subgroup with a better prognosis. Ann. Thorac. Surg. 79(1), 225–233 (2005).
Yoshino, I. et al. Skip metastasis to the mediastinal lymph nodes in non-small cell lung cancer. Ann. Thorac. Surg. 62(4), 1021–1025 (1996).
Misthos, P. et al. Skip metastases: Analysis of their clinical significance and prognosis in the IIIA stage of non-small cell lung cancer. Eur. J. Cardiothorac. Surg. 25(4), 502–508 (2004).
Inoue, M. et al. Results of surgical intervention for p-stage IIIA (N2) non-small cell lung cancer: Acceptable prognosis predicted by complete resection in patients with single N2 disease with primary tumor in the upper lobe. J. Thorac. Cardiovasc. Surg. 127(4), 1100–1106 (2004).
Yoshino, I. et al. Surgical outcome of stage IIIA- cN2/pN2 non-small-cell lung cancer patients in Japanese lung cancer registry study in 2004. J. Thorac. Oncol. 7(5), 850–855 (2012).
Yun, J. K. et al. Long-term outcomes of upfront surgery in patients with resectable pathological N2 non-small-cell lung cancer. Eur. J. Cardiothorac. Surg. 58(1), 59–69 (2020).
Mountain, C. F. & Dresler, C. M. Regional lymph node classification for lung cancer staging. Chest 111(6), 1718–1723 (1997).
Rusch, V. W. et al. The IASLC lung cancer staging project: A proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J. Thorac. Oncol. 4(5), 568–577 (2009).
Park, B. J. et al. Recommended change in the n descriptor proposed by the international association for the study of lung cancer: A validation study. J. Thorac. Oncol. 14(11), 1962–1969 (2019).
Yun, J. K. et al. Comparison between lymph node station- and zone-based classification for the future revision of node descriptors proposed by the International Association for the Study of Lung Cancer in surgically resected patients with non-small-cell lung cancer. Eur. J. Cardiothorac. Surg. 56(5), 849–857 (2019).
Huang, J. et al. The International Association for the Study of Lung Cancer Staging Project for Lung Cancer: Proposals for the Revision of the N Descriptors in the Forthcoming Ninth Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 19(5), 766–785 (2024).
Chung, H. S. et al. Prediction models for mediastinal metastasis and its detection by endobronchial ultrasound-guided transbronchial needle aspiration in potentially operable non-small cell lung cancer: A prospective study. Chest 164(3), 770–784 (2023).
Asmis, T. R. et al. Age and comorbidity as independent prognostic factors in the treatment of non small-cell lung cancer: A review of National Cancer Institute of Canada Clinical Trials Group trials. J. Clin. Oncol. 26(1), 54–59 (2008).
Malhotra, J. et al. Risk factors for lung cancer worldwide. Eur. Respir. J. 48(3), 889–902 (2016).
Minami, H. et al. Lung cancer treated surgically in patients <50 years of age. Chest 120(1), 32–36 (2001).
Kawaguchi, T. et al. Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: A comprehensive analysis of 26,957 patients with NSCLC. J. Thorac. Oncol. 5(5), 620–630 (2010).
Chansky, K. et al. The International Association for the Study of Lung Cancer Staging Project: Prognostic factors and pathologic TNM stage in surgically managed non-small cell lung cancer. J. Thorac. Oncol. 4(7), 792–801 (2009).
Hirsch, F. R. et al. The prognostic and predictive role of histology in advanced non-small cell lung cancer: A literature review. J. Thorac. Oncol. 3(12), 1468–1481 (2008).
Grosu, H. B. et al. Survival disparities following surgery among patients with different histological types of non-small cell lung cancer. Lung Cancer 140, 55–58 (2020).
Yun, J. K. et al. Clinical impact of histologic type on survival and recurrence in patients with surgically resected stage II and III non-small cell lung cancer. Lung Cancer 176, 24–30 (2023).
Meza, R. et al. Lung cancer incidence trends by gender, race and histology in the United States, 1973–2010. PLoS One 10(3), e0121323 (2015).
Wang, B. Y. et al. The comparison between adenocarcinoma and squamous cell carcinoma in lung cancer patients. J. Cancer Res. Clin. Oncol. 146(1), 43–52 (2020).
Toloza, E. M., Harpole, L. & McCrory, D. C. Noninvasive staging of non-small cell lung cancer: A review of the current evidence. Chest 123(1 Suppl), 137S-146S (2003).
Wang, Y. Q. et al. Identification of resectable N2 in NSCLC: A single center experience and review of the SEER database. Front. Oncol. 11, 647546 (2021).
Vansteenkiste, J. et al. Randomized controlled trial of resection versus radiotherapy after induction chemotherapy in stage IIIA-N2 non-small cell lung cancer. J. Thorac. Oncol. 2(8), 684–685 (2007).
Acknowledgements
This study is based on data from Asan Medical Center, and the authors would like to express our gratitude to the patients, physicians, and data managers. We would like to thank Editage (www.editage.co.kr) for English language editing.
Author information
Authors and Affiliations
Contributions
J.Y.K.: Data curation, writing-original draft, review and editing H.P.L.: Data curation, Software, visualization, writing-reviewing and editing. J.K.Y.: Conceptualization, supervision. G.D.L.: Software, validation. S.C.: Methodology. H.R.K.: Software, validation. Y.–H.K.: Validation. D.K.K.: Validation. S.–I.P.: Project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, J.Y., Lee, H.P., Yun, J.K. et al. Risk prediction of multiple-station N2 metastasis in patients with upfront surgery for clinical single-station N2 non-small cell lung cancer. Sci Rep 14, 18800 (2024). https://doi.org/10.1038/s41598-024-69260-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-69260-3