Abstract
The purpose of this study was to evaluate the efficacy of different techniques in removing calcium silicate intracanal medicament (Bio-C Temp). Forty human single-canaled premolars were randomly distributed into five groups (n = 8). All root canals were instrumented, then filled with Bio-C Temp. Following 1-week incubation, the intra-canal medicament was removed using one of five techniques according to tooth group: conventional syringe irrigation, Endo Activator, passive ultrasonic irrigation (PUI), ProTaper Universal F3 and XP-endo Finisher (XPF). Micro-CT scanning was performed before and after removal of Bio-C Temp. All techniques significantly reduced the volume of Bio-C Temp (p < 0.001) without reaching complete elimination. The percentage of Bio-C Temp removed was significantly higher in the XPF group (98.2%) compared to conventional syringe irrigation (70.6%), the Endo Activator (75.7%), and the ProTaper Universal (76.6%). There was no significant difference between the XPF and PUI (95.1%) groups. None of the removal techniques were able to completely remove Bio-C Temp from the root canal. However, XPF was the most effective method, but was not statistically significant when compared to PUI. Clinical Relevance: This study demonstrated that both XPF and PUI outperform conventional irrigation in removing Bio-C Temp intracanal medicament.
Similar content being viewed by others
Introduction
The main objective of endodontic therapy is to eradicate microbial infection from root canal systems1. These systems are complex, harboring intricate isthmuses, auxiliary canals, and dentinal tubules, which offer refuge for bacterial biofilms2 and render mechanical preparation alone insufficient to disinfect canals3. Therefore, it is advised to apply intracanal medication following root canal instrumentation4 to enhance the elimination of residual bacteria, reduce periapical inflammation, discouraging bacterial proliferation and further infection5.
Several intracanal medicaments have been advocated: calcium hydroxide Ca(OH)2, aldehydes, halides, steroids, chlorhexidine, phenolic compounds, and antibiotics6. To date, Ca(OH)2 is recognized as the "gold standard" intracanal medicament for endodontic treatment7. It offers effective antibacterial action due to its high pH, low solubility, and appropriate flow, in addition to its ability to dissolve tissue and suppress tooth resorption8. According to a systematic review, Ca(OH)2 lowers endotoxin levels9. and can inactivate pro-inflammatory mediators such as the tumor necrosis factor-alpha (TNF-α), thereby promoting tissue healing10,11.
Bio-ceramic material are widely used in endodontic non-surgical and surgical root canal treatment, in addition to vital pulp therapy and regenerative endodontic therapy12. Not only do they exhibit exceptional physical and chemical properties, but they also possess biocompatibility and bioactivity, which allows them to influence cellular reactions, promoting healing and tissue repair13.
With the advancement of bio-ceramic materials, a novel calcium silicate-based bioactive material (Bio-C Temp/Angelus Indústria de Produtos Odontológicos S/A, Londrina, PR, Brazil) has been recently introduced as an intracanal medicament. According to the manufacturer, Bio-C Temp® is indicated as an intracanal dressing when treating necrotic teeth, teeth with external and internal resorptions, incomplete root development, teeth requiring endodontic retreatment, and treatment of perforation14.
Bio-C Temp's contains polyethylene glycol, titanium oxide, a resin base, calcium tungsten as a radiopacifier, and an active component composed of tricalcium aluminate, calcium oxide, and calcium silicate. It boasts high biocompatibility, ease of manipulation, and ease of removal, in addition to high alkalinity (pH = 12) and radiopacity (9). It was reported that Bio-C Temp has a bioactive ability that favors osteoblasts’ survival and differentiation, thereby promoting periapical repair15.
Intracanal medicaments must be completely removed from the root canal before obturation to ensure an adequate seal of the final root filling16,17. Several methods have been proposed for the effective removal of intracanal medicaments17,18. The most commonly described method involves the use of instrumentation along with sodium hypochlorite (NaOCl) and ethylenediaminetetraacetic acid (EDTA) irrigant solutions17. Recently, other methods have been suggested, such as passive ultrasonic irrigation (PUI), sonic activation using the Endo Activator system, and the use of nickel-titanium (NiTi) rotary instruments17,18,19,20. The XP-endo Finisher (FKG Dentaire, La Chaux de Fonds, Switzerland) is a NiTi rotary non-tapered file with an ISO 25-diameter tip advocated for the removal of intracanal medicaments21. Due to its unique shape-memory properties, it expands within the canal, allowing it to access canal surfaces reaching the regions inaccessible with conventional instruments.
To date, the effectiveness of various methods for removing Bio-C Temp from the root canal system has not yet been evaluated. Thus, the purpose of this study was to evaluate the effectiveness of different techniques in removing Bio-C Temp from relatively straight canals. Micro-computed tomography scanning was used to determine the volume and percentage of Bio-C Temp removed.
The null hypothesis was that there is no difference in the ability of sonic activation, PUI, NiTi rotary instrumentation and XP-endo Finisher (XPF) to remove Bio-C Temp intracanal medicament.
Materials and methods
This ex vivo study received ethical approval by the Princess Nourah Bint Abdulrahman University (PNU) Institutional Review Board in Riyadh, Saudi Arabia (IRB Number: 22-0234). All research procedures were conducted in strict accordance with relevant guidelines and regulations set forth by PNU Institutional Review Board.
Specimen preparation
Sample size calculation was conducted using G*Power 3.1 software (Heinrich-Heine-Universität, Düsseldorf, Germany). At a level of significance of α = 5%, an estimated standard deviation of 0.05, and a power of 90%, the total sample size was determined to be 40 teeth. Sample size per group required to conduct the experiment was found to be 8. The study utilized single-rooted human teeth with fully formed apices, extracted for reasons unrelated to this research, with informed consent obtained from all patients and/or their legal guardian(s). Inclusion criteria included teeth with single root canals with minor apical curvature (< 20°), free from any signs of calcification, internal or external resorption, previous endodontic treatment, caries, or cracks. Mesio-distal and bucco-lingual radiographs were taken for each tooth to measure the canals’ width at the middle third and exclude excessively oval canals. Canals where the bucco-lingual to mesio-distal ratio exceeded 2 were excluded. Teeth with excessively long (> 25 mm), or short (< 20 mm) roots were also excluded. The external root surfaces were scaled with ultrasonic instruments and washed with distilled water for the removal of any calculus or soft tissue. The teeth were de-coronated at 16 mm from the apex to standardize the length of the roots, then placed in phosphate-buffer saline until preparation. The patency of the canals was verified by passing a file size #K-15 (Dentsply Maillefer) through the apical foramina. The working length (WL) was determined to be 1 mm short of the length where the file extruded the apical foramen. Specimens were mounted into resin molds after the tip of the root was closed with a small piece of molding wax to mimic the clinical situation and prevent the resin material from blocking the root canal. The root canals were instrumented by a single operator with ProTaper rotary files (Dentsply International, Tulsa, OK, USA) up to #F3, according to the manufacturer’s instructions. All the canals were irrigated with 5 mL of 2.5% NaOCl followed by a final rinse of 5 mL of saline during and after using each rotary file.
Bio-C temp placement
After drying all canals with absorbent paper points, another single operator introduced Bio-C Temp (Angelus Indústriade Produtos Odontológicos S/A, Londrina, PR, Brazil) inside the root canal. A syringe with an applicator tip was inserted 3 mm from the WL, and retracted progressively until the entire canal was filled. Access to the root canal was temporarily sealed with cotton pellets and temporary filling material (Orafil-G, Prevest DenPro, Jammu, India), and the teeth were incubated at 37 °C and 100% humidity for 1 week. Micro-Computed Tomography (Micro-CT) imaging was acquired (Pre-scan) to ensure complete filling of the canals.
Removal of the Bio-C temp
After the initial scan was completed, all specimens were accessed and randomly allocated to five groups (n = 8/group) according to the removal techniques. Conventional Syringe Group: A 27-G side-vented needle (Endo Eze Irrigator; Ultradent Products Inc., South Jordan, USA) was inserted in the canals up to 2 mm short of the WL, moved in an up-and-down motion, and irrigated for 2 min with 5 mL 2.5% NaOCl. Endo Activator Group: 5 mL 2.5% NaOCl were used with one minute activation using the EndoActivator (Maillefer Instruments Holding, Ballaigues; Switzerland) set at 10,000 cycles per minute and 25/0.02 tip. Passive ultrasonic irrigation (PUI) Group: 5 mL 2.5% NaOCl was used with ultrasonic file 15/0.02 mounted on a piezoelectric ultrasonic unit (NEWTRON XS P5 B.LED Acteon, Mount Laurel, NJ, USA) at an energy power setting of 8. The ultrasonic file was inserted 1 mm short of the WL and activated for three 20 s cycles amounting to a total of 1 min22. Pro-Taper Universal F3 Group: conventional syringe irrigation (a 27-G needle) with 5 mL 2.5% NaOCl in conjunction with rotary instrumentation to the WL using the Pro-Taper Universal # F3 for 1 min. The rotation speed was 300 rpm at a torque of 2 N cm; XPF Group: The XPF instrument (FKG Dentaire, La Chaux-de-Fonds, Switzerland) was used for one minute to the WL at a speed of 800 rpm and torque of 1 N cm in gentle longitudinal movements with a small amplitude, followed by irrigation with 5 mL of 2.5% NaOCl using a disposable syringe with a 27-G side-vented needle.
Micro-CT scanning
Micro-CT scanning was performed twice for each tooth, after placement of Bio-C Temp in the canals (Pre-Scan) and after its removal (Post Scan), using the Bruker SkyScan 1172 high-resolution micro-CT scanner (Bruker SkyScan, Kontich, Belgium). Standardized scanner configurations used were: 99 kV voltage, 100 μA anode current, 316 ms exposure time, 20.73 μm image pixel size, a 0.6 rotation step for 360° angle, frame averaging of 4 for an improved signal-to-noise ratio, random movement of 8 to minimize ring artifacts, and a Cu + Al filter to minimize beam hardening.
After scanning, an image reconstruction was performed using ©N-Recon, version 1.6.9.4 (Bruker Skyscan, Kontich, Belgium), to produce reconstructed cross-section images. The numerical parameters needed to establish the best image results were checked and adjusted. A ring artifact reduction of 5 for the non-uniformity of the background image; 25% beam hardening compensation; and a smoothing of 2 using a Gaussian kernel were applied. Reconstructed images were loaded into the DataViewer program version 1.5.6.2 (Bruker Skyscan, Kontich, Belgium) software to co-register pre- and post-scan data sets, as well as determine image quality, reorient, resize, and visually inspect the 3D image data set. ©CTAn version of the 1.20.8.0 software was used to binarize the images and quantify the volume of intracanal medicament within the entire root canals and for every canal third, pre- and post-removal. Accordingly, the percentage of removed material was calculated. To quantify the volume of each third, the apical 4mm of the canal was considered to be the apical third. The remaining canal length was measured and divided into two equal regions of interest: middle and coronal thirds. Finally, CTVol 2.3.2.0 (Bruker Skyscan, Kontich, Belgium) was used for the 3D production of color-coded images.
Statistical analysis
The data were analyzed using SPSS software (version 25; SPSS Inc., Chicago, IL, USA). The Shapiro–Wilk test was used to check data normality. Friedman’s two-way analysis of variance by ranks and Kruskal–Wallis followed by pair comparison tests were used. Statistical significance was set at p ≤ 0.05.
Results
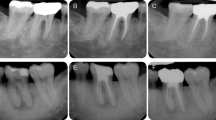
All removal techniques were able to significantly reduce the quantity of Bio-C Temp in the root canals. No method, however, managed to completely eradicate it (Fig. 1). There was a significant difference in the mean volume of Bio-C Temp before and after removal among the different removal techniques (p ≤ 0.001) (Table 1). XPF was associated with the highest percentage of removed material (98.2%), which was statistically significant from conventional syringe irrigation (70.6%); (p = 0.003), the Endo Activator (75.7%); (p = 0.034), and Pro-Taper Universal (76.6%); (p = 0.017). However, it was not statistically significant from PUI (95.1%); (p > 0.999) (Table 1). PUI, on the other hand, removed significantly more Bio-C Temp compared to conventional syringe irrigation (p = 0.009) and Pro-Taper Universal (p = 0.042).
Taking each third individually, XPF was significantly better in removing Bio-C Temp than conventional syringe irrigation and the Endo Activator (p = 0.002) at the apical third. In the middle third, both PUI and XPF removed more Bio-C Temp compared to the Endo Activator (p = 0.001). As for the coronal third, XPF and PUI were significantly better in removing Bio-C Temp than conventional syringe irrigation (p < 0.001). There was no significant difference between the other removal techniques (Table 2).
Discussion
Effective removal of intracanal medicaments before root canal obturation is crucial for a proper seal. Any remaining material can block sealer penetration into dentinal tubules16,17, may interfere with the setting reaction of sealing materials23, and thus ease the coronal/apical leakage24. Recently, a new calcium silicate-based medicament, Bio-C Temp, has been introduced with manufacturer claims of high and rapid Ca + 2 ion release and easy removal25.
This study compared various techniques described in the literature for the removal of Bio-C Temp. According to the results, Bio-C Temp could not be entirely removed from the root canal, which is consistent with other studies. A meta-analysis and systematic review found that while neither XPF nor PUI could completely remove Ca(OH)2 from root canals, both techniques performed better compared to conventional syringe irrigation16,26. Likewise, in this study, the use of XPF significantly outperformed conventional syringe irrigation, the Endo Activator, and the Pro-Taper Universal F3 in terms of the amount of Bio-C Temp removed from the root canals, regardless of the canal thirds. This is in agreement with other studies that showed XPF to be the most effective in removal of triple antibiotic paste27 and Ca(OH)228.
According to Gokturk et al., PUI and XPF showed no significant difference in intracanal medicament removal, both outperforming conventional irrigation29. On the other hand, other studies showed that PUI was more effective than XPF in the removal of Ca(OH)216,26. This was attributed to XPF's small size and non-taper, which is less suited for larger apical canal preparations (size 40/0.04). In the present study, apical preparation was limited to F3, which is equivalent to a size 30 file.
The findings of this study showed that PUI removed significantly more Bio-C Temp compared to conventional syringe irrigation and Pro-Taper Universal, which contradict with Aksel et al.’s (2017) study, which reported no significant difference between PUI and conventional syringe irrigation in the removal of TAP from the canal's three-thirds30. This was attributed to the irrigation protocol, which employed side-vented needles with an up-and-down motion. Although the same technique was applied in the present study, PUI was associated with significantly more material removal in the coronal third compared to conventional syringe irrigation. The consistency of the intracanal medicament could also account for such a difference. Another study comparing PUI and Profile NiTi rotary files in the removal of Ca(OH)2 also found no significant difference between both methods20. One explanation for these dissimilar results is the different cross-sections and tapers of the NiTi files used.
The current findings showed no significant difference between conventional syringe irrigation and the Endo Activator. Similar findings have been reported by Al-Shahrani et al., in which the Endo Activator system did not improve Ca(OH)2 removal31.
In the canal’s apical third, PUI and XPF proved more effective than conventional irrigation in removing intracanal medicament, consistent with previous studies, including those on curved canals32,33. However, there was no significant difference between the effectiveness of PUI and the EndoActivator, which mirrors previous findings32.
There was also no difference between PUI and XPF in the material removal from the last apical third. While this is in accordance with many studies29,30,31,34, a previous study measuring the amount of Ca(OH)2 remaining in artificial apical grooves reported that PUI is superior to XPF in removing the medicament35. Another study that did not employ the grooves methodology showed that XPF was superior to PUI in the apical third36. Different methodologies and quantitative techniques may have led to these contradictory results.
The micro-CT technology used in the present study is a non-invasive, non-destructive, high-resolution analytical method that allows the three-dimensional rendering of the root canal morphology and its filling material, as well as the identical reconstruction of this morphology before and after applying the studied technique37.
The present study was limited to relatively straight canals, excluding excessively oval canals and roots with multiple-canal systems. Therefore, current findings may not apply to those anatomies, and further studies are required to verify this. Although the study protocols mimicked the clinical situation, there was a certain variation in root canal volume between the specimens that should be considered a limitation to standardization.
A meta-analysis26 that looked at how well PUI and XPF removed intracanal medication found that the final flush irrigation solution could affect how well XPF worked. It was suggested that EDTA be used as a final irrigant to enhance removal. In the present study, although EDTA was not used, there was no significant difference between the two techniques. This seems to be in accordance with a previous study38 that found that the final irrigation solution had little effect on the removal of Ca(OH)2. A recent study using confocal laser scanning microscopy found that using 70% ethanol irrigation enhanced the removal of Ca(OH)2. Typically, chelating agents such as EDTA are employed to remove inorganic substances, like calcium silicates, by binding to its metal ions. It is recommended that future research use EDTA in their protocol and further investigate the influence of the final irrigant solution on Bio-C Temp removal.
Conclusion
Within the limitations of this study, none of the removal techniques were able to completely remove Bio-C Temp from the root canal. However, XPF was the most effective method, resulting in the highest percentage of material removal and was not statistically significant from PUI.
Data availability
The datasets generated and analyzed in this study are available as a supplementary file.
References
Haapasalo, M., Endal, U., Zandi, H. & Coil, J. M. Eradication of endodontic infection by instrumentation and irrigation solutions. Endod. Top. 10(1), 77–102 (2005).
Trope, M. & Bergenholtz, G. Microbiological basis for endodontic treatment: Can a maximal outcome be achieved in one visit?. Endod. Top. 1(1), 40–53 (2002).
Young, G., Parashos, P. & Messer, H. The principles of techniques for cleaning root canals. Aust. Dent. J. 52(1 SUPPL), S52-63. https://doi.org/10.1111/j.1834-7819.2007.tb00526.x (2007).
Torabinejad, M., Handysides, R., Khademi, A. A. & Bakland, L. K. Clinical implications of the smear layer in endodontics: A review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 94(6), 658–666. https://doi.org/10.1067/moe.2002.128962 (2002).
Chong, B. S. & Ford, T. R. P. The role of intracanal medication in root canal treatment. Int. Endod. J. 25(2), 97–106. https://doi.org/10.1111/j.1365-2591.1992.tb00743.x (1992).
Gomes, B. P. F. A. et al. Effectiveness of 2% chlorhexidine gel and calcium hydroxide against Enterococcus faecalis in bovine root dentine in vitro. Int. Endod. J. 36(4), 267–275. https://doi.org/10.1046/j.1365-2591.2003.00634.x (2003).
Zehnder, M., Söderling, E., Salonen, J. & Waltimo, T. Preliminary evaluation of bioactive glass S53P4 as an endodontic medication in vitro. J. Endod. 30(4), 220–224. https://doi.org/10.1097/00004770-200404000-00009 (2004).
Kuga, M. C., de Campos, E. A., de Faria-Junior, N. B., Só, M. V. R. & Shinohara, A. L. Efficacy of NiTi rotary instruments in removing calcium hydroxide dressing residues from root canal walls. Braz. Oral. Res. 26(1), 19–23 (2012).
Bedran, N. R. et al. Does calcium hydroxide reduce endotoxins in infected root canals? Systematic review and meta-analysis. J. Endod. 46(11), 1545–1558. https://doi.org/10.1016/j.joen.2020.08.002 (2020).
Khan, A. A., Sun, X. & Hargreaves, K. M. Effect of calcium hydroxide on proinflammatory cytokines and neuropeptides. J. Endod. 34(11), 1360–1363. https://doi.org/10.1016/j.joen.2008.08.020 (2008).
Meng, L. J. et al. The effect of calcium hydroxide on IL-6 and TNF-α expression of osteoblast in periapical tissues. Shanghai Kou Qiang Yi Xue. 25(1), 32–37 (2016).
Wan, Q. Q. et al. Immunomodulatory effects of tricalcium silicate-based cements on osteogenesis. Appl. Mater. Today. 1(24), 101145 (2021).
Song, W., Li, S., Tang, Q., Chen, L. & Yuan, Z. In vitro biocompatibility and bioactivity of calcium silicate-based bioceramics in endodontics (review). Int. J. Mol. Med. 48(1), 128. https://doi.org/10.3892/ijmm.2021.4961 (2021).
Bio-C Temp® [Internet]. Angelus. 2022. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.ultimatedental.com/uploads/Angelus_BIO-C-Temp_Brochure.pdf.
Lopes, C. S. et al. Hepatic enzymes and immunoinflammatory response to Bio-C Temp bioceramic intracanal medication implanted into the subcutaneous tissue of rats. Sci. Rep. 12(1), 1–14. https://doi.org/10.1038/s41598-022-06545-5 (2022).
Denna, J., Shafie, L. A., Alsofi, L., Al-Habib, M. & AlShwaimi, E. Efficacy of the rotary instrument xp-endo finisher in the removal of calcium hydroxide intracanal medicament in combination with different irrigation techniques: A microtomographic study. Materials (Basel). 13(10), 2222 (2020).
Üstün, Y., Aslan, T., Sagsen, B. & DInçer AN.,. The effects of different irrigation protocols on removing calcium hydroxide from the root canals. Niger. J. Clin. Pract. 19(4), 465–470 (2016).
Bhuyan, A., Seal, M. & Pendharkar, K. Effectiveness of four different techniques in removing intracanal medicament from the root canals: An in vitrostudy. Contemp. Clin. Dent. 6(3), 309–312 (2015).
Van Der Sluis, L. W. M., Wu, M. K. & Wesselink, P. R. The evaluation of removal of calcium hydroxide paste from an artificial standardized groove in the apical root canal using different irrigation methodologies. Int. Endod. J. 40(1), 52–57. https://doi.org/10.1111/j.1365-2591.2006.01182.x (2007).
Kenee, D. M., Allemang, J. D., Johnson, J. D., Hellstein, J. & Nichol, B. K. A quantitative assessment of efficacy of various calcium hydroxide removal techniques. J. Endod. 32(6), 563–565 (2006).
Santos, A. S. dos, de Sá, M. A. B., Duarte, M. A. H., Horta, M. C. R., Silveira, F. F., Nunes, E. Endodontic Cement Penetration After Removal of Calcium Hydroxide Dressing Using XP-Endo Finisher, vol. 36 (Brazilian Oral Research. Scielo, 2022).
Căpută, P. E., Retsas, A., Kuijk, L., Chávez de Paz, L. E. & Boutsioukis, C. Ultrasonic irrigant activation during root canal treatment: A systematic review. J. Endod. 45(1), 31-44.e13 (2019).
Margelos, J., Eliades, G., Verdelis, C. & Palaghias, G. Interaction of calcium hydroxide with zinc oxide-eugenol type sealers: A potential clinical problem. J. Endod. 23(1), 43–48 (1997).
Kim, S. K. & Kim, Y. O. Influence of calcium hydroxide intracanal medication on apical seal. Int. Endod. J. 35(7), 623–628 (2002).
Bio-C Temp High performance in fewer sessions !. (2021) https://chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Fwww.angelusdental.com%2Fimg%2Farquivos%2Ffolder_bio_c__temp_angelus_en.pdf&clen=1706767&chunk=true.
Zhou, J., Liu, T. & Guo, L. Effectiveness of XP-Endo Finisher and passive ultrasonic irrigation on intracanal medicament removal from root canals: A systematic review and meta-analysis. BMC Oral Health. 21(1), 1–15. https://doi.org/10.1186/s12903-021-01644-7 (2021).
Turkaydin, D. et al. Efficacy of Endoactivator, CanalBrush, and passive ultrasonic irrigation in the removal of calcium hydroxide paste with iodoform and p-chlorophenol from root canals. Niger. J. Clin. Pract. 23(9), 1237 (2020).
Taneja, S., Kumar, P., Dheer, A. Comparative evaluation of efficacy of XP Endo Finisher, sonic, and ultrasonic irrigation in removal of calcium hydroxide and subsequent adaptation of gutta percha in simulated internal resorption cavity—An in vitro study. Endodontology. 34(4) (2022). https://journals.lww.com/eddt/Fulltext/2022/34040/Comparative_evaluation_of_efficacy_of_XP_Endo.4.aspx.
Gokturk, H., Ozkocak, I., Buyukgebiz, F. & Demir, O. An in vitro evaluation of various irrigation techniques for the removal of double antibiotic paste from root canal surfaces. J. Appl. Oral Sci. 24(6), 568–574 (2016).
Aksel, H., Küçükkaya Eren, S. & Serper, A. Comparison of triple antibiotic paste removal by different irrigation techniques. Dent. Mater. J. 36(3), 303–308 (2017).
Al-Shahrani, S., Al-Garni, S., Al-Maflehi, N. & Al-Nazhan, S. Evaluation of calcium hydroxide removal using EndoActivator system: An in vitro study. Saudi Endod. J. 4(1), 13 (2014).
Wang, Y. et al. An in vitro study on the efficacy of removing calcium hydroxide from curved root canal systems in root canal therapy. Int. J. Oral Sci. 9(2), 110–116. https://doi.org/10.1038/ijos.2017.14 (2017).
Shi, L., Wu, S., Yang, Y. & Wan, J. Efficacy of five irrigation techniques in removing calcium hydroxide from simulated S-shaped root canals. J. Dent. Sci. 17(1), 128–134. https://doi.org/10.1016/j.jds (2022).
Wigler, R., Dvir, R., Weisman, A., Matalon, S. & Kfir, A. Efficacy of XP-endo finisher files in the removal of calcium hydroxide paste from artificial standardized grooves in the apical third of oval root canals. Int. Endod. J. 50(7), 700–705. https://doi.org/10.1111/iej.12668 (2017).
Donnermeyer, D., Wyrsch, H., Bürklein, S. & Schäfer, E. Removal of calcium hydroxide from artificial grooves in straight root canals: Sonic activation using EDDY versus passive ultrasonic irrigation and XPendo finisher. J. Endod. 45(3), 322–326 (2019).
Hamdan, R., Michetti, J., Pinchon, D., Diemer, F., Georgelin-Gurgel, M. The XP-Endo Finisher for the removal of calcium hydroxide paste from root canals and from the apical third. J. Clin. Exp. Dent. 9(7) (2017).
Versiani, M. A., Keleș, A. Applications of micro-CT technology in endodontics. In Micro-computed Tomography (micro-CT) in Medicine and Engineering 183–211 (Springer International Publishing, 2020). https://doi.org/10.1007/978-3-030-16641-0_12.
Lambrianidis, T., Margelos, J. & Beltes, P. Removal efficiency of calcium hydroxide dressing from the root canal. J. Endod. 25(2), 85–88 (1999).
Funding
This research was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R162), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly to this manuscript: Conceptualization, R.B., R.A. and H.B.; methodology, R.B. and R.A. and H.B.; software, R.B. and L.B.; validation, R.B., R.A., and H.B. formal analysis, R.B. and L.B.; investigation, A.L., Sh.Alresh and Sh.Allu.; resources, A.L., Sh.Alresh and Sh.Allu.; data curation, R.B. and R.A. and L.B.; writing—original draft preparation, A.L., Sh. Alresh and Sh. Allu.; review and editing, R.B. and R.A. and H.B.; visualization, R.B. and R.A. and H.B.; supervision, R.B. and R.A.; project administration, R.B.; funding acquisition, R.A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Almohareb, R.A., Barakat, R.M., Alreshaidan, S. et al. Efficacy of various techniques in calcium silicate-based intracanal medicament removal: a micro-CT analysis. Sci Rep 14, 19705 (2024). https://doi.org/10.1038/s41598-024-69849-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-69849-8