Abstract
Radiation-free one-stage bedside endoscopic stone removal and biliary drainage for severe acute cholangitis (SAC) caused by choledocholithiasis in intensive care unit (ICU) has not been reported. Herein, we introduce our preliminary experience of such intervention. Radiation-free bedside digital cholangioscope-assisted one-stage endoscopic stone removal and biliary drainage was performed in an urgent manner. Data on clinical outcomes and follow-up from thirty patients were retrospectively analyzed. Time interval was 7.6 ± 4.7 (2–18) h between ICU admission and endoscopic intervention, and was 35.5 ± 14.5 (5–48) h between the seizure and endoscopic intervention. A 100% technical success was achieved. Except for one mild pancreatitis, no other complication occurred. Patients showed good responses to endoscopic interventions, which were reflected by ameliorated disease severities and laboratory findings. Time lengths of ICU stay and total in-hospital stay were 8.7 ± 4.9 (2–23) days and 14.5 ± 7.4 (5–39) days, respectively. In-hospital mortality occurred in three patients. According to a 6-month follow-up, two patients died of pneumonia and acute myocardial infarction. No SAC and/or biliary stone residual occurred. The current intervention demonstrated favorable results compared to traditional endoscopic retrograde cholangiopancreatography. Our study provides a novel bedside endoscopic intervention method for SAC caused by choledocholithiasis.
Similar content being viewed by others
Introduction
Severe acute cholangitis (SAC) is a life-threatening infection, with choledocholithiasis as the leading cause. Bedside endoscopic nasobiliary drainage or stenting in intensive care unit (ICU) are most commonly performed for SAC in an urgent (≤ 24 h after admission) manner. Such endoscopic drainage always induces insufficient biliary drainage, which leads to no improvement in organ functions1. Subsequently, in-hospital mortality of SAC remains high1. It is important to provide a more effective bedside biliary drainage method.
According to the guideline from the American Society for Gastrointestinal Endoscopy (ASGE), one-session endoscopic stone removal is recommended for acute cholangitis caused by choledocholithiasis2. However, it is not practical in ICU due to lack of fluoroscopic platforms and radioprotective shelters. Also, transportation from ICU to fluoroscopy equipped gastrointestinal endoscopy unit or operation room poses great risks of mortality to patients with SAC3. These contribute to lack of proper bedside one-stage endoscopic lithotomy in ICU. Recently, non-radiation endoscopic removal for choledocholithiasis is technically feasible by enrolling a novel digital cholangioscope (DCS) into the intervention system4,5. Current literatures4,5 and our previous publications6,7 have shown technical feasibilities of DCS-assisted non-radiation endoscopic lithotomy. Hence, DCS-assisted bedside non-radiation endoscopic intervention for SAC has been proposed4. Since no study is available, this study aimed to report DCS-assisted radiation-free bedside one-session endoscopic lithotomy and biliary drainage for patients suffering from SAC caused by choledocholithiasis.
Methods
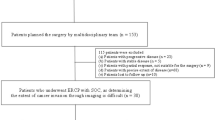
Our interventions were consent to the Helsinki Declaration of 1975. The principle was to achieve stone removal and biliary drainage in one endoscopic procedure. Patients suffering from SAC caused by choledocholithiasis were initially recruited. Diagnosis of choledocholithiasis was confirmed by abdominal computed tomography (CT) scan prior to ICU admission, which was performed upon the emergency visit. The exclusion criteria included: (1) SAC caused by other causes; (2) with Billroth II, Roux-en-Y or Whipple anatomy; (3) coagulopathy (platelet count < 50,000/µL or prothrombin time international normalized ratio > 2.0); (4) receiving anticoagulation therapy; (5) chaperon’s preference to conservative medications; (6) choledocholithiasis ≥ 30 mm in size.
Clinical medications in ICU
Medications, including aggressive hydration, organ support and antibiotic therapy, were initially executed upon ICU admission. Bedside endoscopic intervention was performed in an urgent manner. Early correction of coagulation dysfunction was timely executed in patients with coagulopathy and/or ongoing anticoagulant therapy. All patients underwent furthermore medications in ICU, such as organ support, antibiotic therapy and close monitoring, after endoscopic intervention.
Endoscopic intervention techniques
Written informed consent was obtained from legal guardian of each patient before endoscopic intervention. Prophylactic rectal indomethacin (100 mg) was administered prior to endoscopic intervention. Endoscopic intervention was performed with patients underwent intravenous anesthesia with propofol and endotracheal intubation, and monitored by a competent ICU physician. Additionally, all patients were placed in a supine position. For the aim of avoiding and decreasing potential adverse events, endoscopic interventions were performed by Dr. Yadong Feng, who is our chief expert endoscopist in endoscopic retrograde cholangiopancreatography (ERCP). Due to the very low incidence of disease, this did not pose great burden to us, and our staff was available during the research period.
Endoscopic platform consisted of a 4.2-mm therapeutic duodenoscope (TJF-260, Olympus, Tokyo, Japan) and either of two commercially available DCSs, including Spyglass DS™ (Boston Scientific, Marlborough, MA, USA) and eye Max™ (Microtech Co., Nanjing, China). A holmium laser system (Potent Co., Guangzhou, China) was used as the energy platform for laser lithotripsy.
Key steps are listed as follows. Firstly, biliary access was attempted by using a sphincterotome (Microtech Co., Nanjing, China) and a 0.035-inch guidewire (Microtech Co., Nanjing, China). Double-guidewire technique and/or transpancreatic precut were applied for difficult biliary access as necessary. A 5-Fr*5 cm pancreatic stent (COOK Medical, Bloomington, IN, USA) was placed for inadvertently repeated (≥ three times) pancreatic duct access, which was judged by clear aspiration in the catheter. Successful biliary access was confirmed by visible purulent bile aspiration. Then, about 20–30 ml bile were aspirated. Shallow cannulation was adopted in cannulation attempts for biliary access. A shallow (≤ 5 cm) guidewire insertion into the duct was initially attempted, and a deeper (5–10 cm) guidewire insertion was executed when biliary access was confirmed. Secondly, biliary orifice was established by endoscopic sphincterotomy (EST) followed by endoscopic papillary balloon dilation (EPBD). A 2–3 mm EST was performed with a high-frequency electric generator (EVIO 300D, ERBE, Tübingen, German) with the settings of ENQOCUT, effect 2 and 50 w. EPBD was performed by using a 6–10 mm balloon (Microtech Co., Nanjing, China), which size was determined to prior imaging features relevant to the width of the distal common bile duct, the size of stones and presence of a large peri-ampullary diverticulum. Thirdly, DCS was introduced into the biliary duct for visualization of choledocholithiasis. DCS-guided laser lithotripsy (1.2–1.4 J, 20 Hz), and/or basket stone removal were performed. Repeated endoscopic lithotomy was performed for stone residual. Sterilized saline water was irrigated as necessary, and suction by the duodenoscope was constantly performed. Finally, a plastic stent (Microtech Co., Nanjing, China) was deployed. Endoscopic clipping was performed by using one-to-three rotatable titanium clips (Microtech Co., Nanjing, China).
Outcome measures
The primary aim was to assess the efficacy of this bedside endoscopic intervention. Outcomes, including responses to endoscopic intervention, disease severities, in-hospital mortality and follow-up data were analyzed. The second aim was to evaluate the safety of this technique by reviewing adverse events.
Follow-up
A 6-month outpatient follow-up was arranged in those survivors, which was performed at 1, 3 and 6 months after discharge. Outcomes, including laboratory examinations, imaging (abdominal B-ultrasonography or CT), re-admission due to SAC recurrence and death and cause, were collated.
Definitions
Diagnoses were determined to the Tokyo Guideline 20188, the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)9, the Acute Physiology and Chronic Health Evaluation (APACHE-II) score10 and Sequential Organ Failure Assessment (SOFA) score10, respectively. Complications were defined by the criteria by the ASGE workgroup11.
Statistical analysis
Continuous variables are presented as mean ± standard deviation (SD) or median and inter-quartile range (IQR), and categorical variables are expressed as frequency and percentage. The Student’s t tests, one-way analysis of variance (ANOVA), Bonferroni’s test and binary univariate logistic regression were performed in SPSS statistical software, version 20.0 (SPSS Inc, Chicago, IL, USA). A P < 0.05 was considered to be statistically significant.
Ethics approval and consent to participate
Our performances were approved by the review broad of Zhongda Hospital, Southeast University (approval number 2019ZDSYLL093-P01 and 2019ZDSYLL094-P01). All patients and/or their chaperons were informed that the anonymous data would be used for research and publication. In addition, they all consented to participate this research.
Consent for publication
All patients and/or their chaperons consented that results of this research would be anonymously disseminated to the scientific community through peer reviewed journal articles and/or international conference presentation.
Results
General characteristics
Between June 2020 and January 2023, 42 patients suffering from SAC caused by choledocholithiasis were initially enrolled. Twelve patients’ guardians refused invasive biliary drainage, and 30 patients were included. Detailed patient characteristics and initial medications are listed in Table 1. Right upper quadrant or epigastric pain, fever, jaundice and disturbance of consciousness, respectively were manifested in 26, 18, 18 and 15 patients, respectively. Five and 25 patients developed sepsis and septic shock, respectively. Biliary stones, with the mean size of 7 mm, were found in all patients. APACHE II and SOFA scores were 24.6 ± 6.4 (13–38) and 11.9 ± 3.3 (3–18), respectively. Twenty-four, 24, 8 and 7 patients needed vasopressor support, mechanical ventilation, high-flow oxygen therapy and continuous renal replacement therapy, respectively.
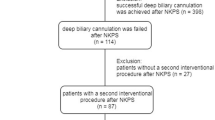
Endoscopic interventions
Time interval was 7.6 ± 4.7 (2–18) h between ICU admission and endoscopic intervention, and was 35.5 ± 14.5 (5–48) h between symptoms presentation and endoscopic intervention. A 100% technical success rate was achieved in biliary access, stone clearance and biliary drainage. DCS-guided laser lithotripsy was used in two patients. Mean time lengths of biliary access, biliary visualization and endoscopic intervention were 3.8 ± 4.5 (1.5–14) min, 10.2 ± 3.8 (6–38) min and 31.6 ± 12.7 (14–70) min, respectively. Expect for one mild pancreatitis, there was no other complication. Detailed information of endoscopic interventions is listed in Table 2.
Responses to medications post endoscopic intervention
As shown in Table 3 and Fig. 1, ameliorated disease severities and key laboratory findings were present. APACHE (F = 164.300, P < 0.001) and SOFA (F = 135.900, P < 0.001) scores were significantly reduced after endoscopic intervention. Decreased levels of leucocyte count (F = 10.220, P < 0.001), serum lactate (F = 32.200, P < 0.001), C-reactive protein (F = 24.740, P < 0.001), procalcitonin (F = 22.380, P < 0.001), serum total bilirubin (F = 23.640, P < 0.001), alanine trans aminase (F = 20.410, P < 0.001), aspartate aminase (F = 16.360, P < 0.001) and creatinine (F = 8.611, P = 0.002) were present.
Comparison of disease severities and laboratory findings prior and post endoscopic intervention. Results of disease severities and laboratory findings at Day 0, 1, 3 and 7 were collated and compared. (A) APACHE II and SOFA scores; (B) leucocyte counts; (C) serum arterial lactate; (D) serum total bilirubin; (E) serum ALT and AST; (F–H) serum procalcitonin, C-reactive protein and creatinine. *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001; ns non-sense, APACHE-II acute physiology and chronic health evaluation, SOFA sepsis-related organ failure, ALT alanine transaminase, AST aspartate transaminase.
Outcomes
Time lengths of ICU stay and total hospitalization were 8.7 ± 4.9 (2–23) days and 14.5 ± 7.4 (5–39) days, respectively. In-hospital mortality occurred in three patients, with causes of multiple organs failure and ventilator-associated pneumonia in two and one patient(s), respectively. According to a binary univariate logistic regression analysis (Table 4), clinical characteristics and organ support measures were not predictive for in-hospital mortality.
Follow-up
One patient died due to pneumonia at 2 months after discharge, and another died due to acute myocardial infarction at 4 months after discharge. No attack of SAC, stone residual and stone recurrence occurred in the remaining 25 survivors who completed the 6-month follow-up. Normal laboratory findings, including complete blood count, liver function and serum creatinine, were found in those survivors.
Comparison of outcomes to those of traditional ERCP
Between January 2017 and December 2019, forty-five patients were admitted to the ICU at Zhongda Hospital and underwent urgent traditional ERCP for biliary drainage due to severe acute cholangitis resulting from choledocholithiasis. All ERCP procedures were executed in operation units equipped with fluoroscopy. The patients received intravenous anesthesia with propofol and underwent endotracheal intubation, all under the vigilant monitoring of a proficient ICU physician. These patients served as the control group for comparative analyses. The baseline characteristics, cannulation techniques, successful biliary access rates, biliary access, and successful biliary drainage exhibited no significant differences, as delineated in Table 5. Notably, DCS-assisted endoscopic intervention demonstrated a higher one-session stone clearance (P = 0.015). Furthermore, DCS-assisted endoscopic intervention proved superior to traditional ERCP, manifesting significantly reduced ICU stay duration (P = 0.043), total hospitalization (P < 0.001), in-hospital mortality (P = 0.021), re-endoscopic intervention post-discharge (P < 0.001), and 6-month mortality after discharge (P = 0.032).
Discussion
An additional ERCP is always needed for stone removal when SAC was alleviated. Such intervention also poses high risks of adverse events to patients12,13. Therefore, to achieve one-stage biliary stone removal and biliary drainage is desirable12. In this study, we demonstrate one-stage bedside non-radiation “mother-and-baby” endoscopic intervention, which is based on our experience of one-stage ERCP for ascending acute cholangitis caused by choledocholithiasis14 and DCS-assisted radiation-free lithotomy6,7.
Although bedside endoscopic biliary drainage for SAC is promising, it is important to assess benefits and risks. In this study, coagulation disorder, very large (≥ 30 mm) stone size and post-surgical anatomy were set as main contraindications. This setting is due to some considerations. Firstly, intra-procedure massive hemorrhage is difficult to be negotiated15. Therefore, early correction of coagulation dysfunction should be performed timely for patients with coagulopathy and/or ongoing anticoagulant therapy. Secondary, a very large stone is difficult to be removed in single session16. Also, a significantly prolonged time length is needed, and there are some worries of aggravation of SAC. Thirdly, post-surgical anatomy always leads to a low technical success, which may aggravate the disease severity17.
In this study, patients showed good responses to medications after endoscopic intervention. Compared with previous reports1,18,19, enrolled patients were with more serious disease severities, as reflected by higher APACHE II and SOFA scores. By contrast, in-hospital mortality was 10%, and was much lower than data from France (about 29%)1 and Morocco (28%)19. This may be due to more sufficient biliary drainage was achieved, which ameliorated disease severities and improved organ functions. Consequently, clinical characteristics and medication measures were not predictive to in-hospital mortality due to the low incidence of mortality in this patient cohort. Our method yielded less endoscopic intervention sessions than previous data, which demonstrate that about 2.8–3.3 ERCP sessions are often needed per patient2. Also, due to one-session stone clearance, risks of SAC recurrence and other adverse events were reduced. This may contribute to a better prognosis. Relevantly, our follow-up data showed the 6-month mortality rate (2/27, 7.41% vs. 48%18) was significantly reduced. To better comprehend the novelty of DCS-assisted bedside intervention, we conducted comparative analyses using a retrospective patient cohort as the control group. Both groups achieved a high technical success rate of biliary access, indicating the feasibility of endoscopic drainage for critically ill patients. Despite similar patient characteristics, the outcomes of DCS-assisted bedside intervention were superior. These findings highlight the advantages of DCS-assisted bedside intervention over traditional ERCP.
Due to intraluminal high pressure of the bile duct, non-radiation biliary access is not difficult to be fulfilled4,5,6,7. Also, followed steps are easily realized by expert endoscopists. Therefore, it is not technically challenging to execute this endoscopic biliary intervention, as reflected by a 100% technical success rate was achieved. In our practice, while performing shallow cannulation for biliary access, initially shallow guidewire insertion was also attempted. This is meaningful for inadvertently pancreatic access, and the tip of guidewire could be kept in the main pancreatic duct or its main branch. And, this is sufficient for necessary pancreatic stenting. Outcomes from this study and previous reports4,5,6,7,20,21 have shown the safety and feasibility of non-radiation biliary access.
It is important to consider possible complications relevant to endoscopic intervention. Lenze et al.22 reported the incidence of adverse events from DCS-assisted ERCP was about 25%. Recent literatures6,21 showed the adverse events rate was about 10%, and was not statistically differed to that from conventional ERCP. Our data showed the complication rate was 3.33%, and was significantly lower than that (14%, 40/285) from the study by Lavillegrand et al.1.
Our measures for minimizing complications included small incision and EPBD, balancing water irrigation and outflow and endoscopic clipping. Our performance of EST combined with 6–10 mm EPBD was to decrease potential risks of delayed bleeding or micro-perforation, which may be higher in standard and large EST. Our intervention was sufficient in providing the biliary outlet for DCS advancement into the bile duct and followed removal of stones or stone fragments. Additionally, this was partly due to initially planned DCS-guided laser lithotripsy for large or unexpectedly large stones4,5,6. The second one is positive biliary depression. Beyond 20–30 ml bile aspiration, intra-procedure water flow balancing4,5,6,7,23 by avoiding excessive water irrigation and performing regular suction was mandatorily required. This was clinically significant in avoiding iatrogenic deterioration of disease severities. Also, prophylactic biliary stenting after stone clearance was performed to provide a continuous biliary drainage. The third one is endoscopic clipping, which was performed for reducing risks of delayed papillary hemorrhage and/or type-II micro-perforation.
The roles of endoscopic ultrasound (EUS) diagnosis and EUS assisted interventions for such patients are worth of considering. Although EUS is promising in detecting choledocholithiasis, such diagnosis is invasive than CT scan. In addition, linear EUS based anterograde lithotomy is not suitable for such patients. This is not only due to ERCP is suggested as the first-line endoscopic approach2, but also due to the fact of EUS-guided anterograde lithotomy should be performed under guidance of fluoroscopy. Park et al. reported technical feasibility of intraductal ultrasound (IDUS) guided non-radiation endoscopic management of bile duct stones21. However, IDUS guided approach may be limited by the indirect imaging and possibly excessive intraductal gas. By contrast, direct visualization from DCS provides a convincing determination of stone clearance.
The most interest is the significantly reduced in-hospital mortality and deaths after discharge. Due to the high cost of DCS, the cost of such endoscopic intervention is higher than single ERCP. However, since repeated endoscopic sessions are remitted, total cost of in-hospital medication could be reduced2. Since July 2021, with the introduction of eye Max™, the cost of DCS has greatly decreased in China. According to our manipulation feelings, the eye Max™ system can provide a wider visualization filed than Spyglass DS™. However, there is no difference relevant to ease of usage, visualization of the bile duct and choledocholithiasis between two platforms. The reduced cost of DCS apparatus makes such approach acceptable in ICU medications.
There are several limitations. Firstly, the conclusion may be biased due to the limited sample size, given the very low incidence of the disease. Secondly, this was not a randomized prospective study, as decisions were influenced not only by patient guardians, but also by the severity of the disease. The limited sample size resulting from the low disease incidence is also a contributing factor. Thirdly, all endoscopic interventions were carried out by a single expert endoscopist, in consideration of minimizing potential adverse events. Additionally, we cited our previous publications, establishing ourselves as pioneering experts in DCS-assisted radiation-free retrograde intervention for biliary diseases. Furthermore, we have been committed to performing urgent one-session ERCP for critically ill patients for over a decade.
In conclusion, DCS-assisted bedside one-stage endoscopic lithotomy and biliary drainage yields an improved quality in endoscopic intervention for SAC caused by choledocholithiasis. We suggest that this intervention to be executed for strictly assessed patients.
Data availability
All data analyzed during the current study are included in this published article.
Abbreviations
- APACHE-II:
-
Acute Physiology and Chronic Health Evaluation
- ASGE:
-
American Society for Gastrointestinal Endoscopy
- DCS:
-
Digital cholangioscope
- EUS:
-
Endoscopic ultrasound
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- EPBD:
-
Endoscopic papillary balloon dilation
- EST:
-
Endoscopic sphincterotomy
- IDUS:
-
Intraductal ultrasound
- IQR:
-
Inter-quartile range
- ICU:
-
Intensive care unit
- SAC:
-
Severe acute cholangitis
- SD:
-
Standard deviation
- SOFA:
-
Sequential Organ Failure Assessment
References
Lavillegrand, J. R. et al. Acute cholangitis in intensive care units: Clinical, biological, microbiological spectrum and risk factors for mortality: A multicenter study. Crit. Care 25, 49 (2021).
Buxbaum, J. L. et al. ASGE guideline on the management of cholangitis. Gastrointest. Endosc. 94, 207-221.e14 (2021).
Brunsveld-Reinders, A. H. et al. A comprehensive method to develop a checklist to increase safety of intra-hospital transport of critically ill patients. Crit. Care 19, 214 (2015).
Barakat, M. T. et al. A prospective evaluation of radiation-free direct solitary cholangioscopy for the management of choledocholithiasis. Gastrointest. Endosc. 87, 584-589.e1 (2018).
Ridtitid, W. et al. Endoscopic clearance of non-complex biliary stones using fluoroscopy-free direct solitary cholangioscopy: Initial multicenter experience. DEN Open 4, e241 (2023).
Feng, Y. et al. Digital cholangioscopy-assisted nonradiation endoscopic retrograde cholangiopancreatography for retrieval of common bile duct stone. Surg. Laparosc. Endosc. Percutan. Tech. 32, 203–208 (2021).
Feng, Y. et al. Digital cholangioscopy-assisted, direct visualization-guided, radiation-free, endoscopic retrograde intervention for cholelithiasis: Technical feasibility, efficacy, and safety. Surg. Endosc. 38, 1637–1646 (2024).
Yokoe, M. et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholecystitis (with videos). J. Hepatobiliary Pancreat. Sci. 25, 41–54 (2018).
Singer, M. et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315, 801–810 (2016).
Quintairos, A., Pilcher, D. & Salluh, J. I. F. ICU scoring systems. Intensive Care Med. 49, 223–225 (2023).
ASGE Standards of Practice Committee et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest. Endosc. 89, 1075-1105.e15 (2019).
Eto, K. et al. Single-stage endoscopic treatment for mild to moderate acute cholangitis associated with choledocholithiasis: A multicenter, non-randomized, open-label and exploratory clinical trial. J. Hepatobiliary Pancreat. Sci. 22, 825–830 (2015).
Galeazzi, M. et al. Endoscopic retrograde cholangiopancreatography in the elderly: Results of a retrospective study and a geriatricians’ point of view. BMC Gastroenterol. 18, 38 (2018).
Zhang, X. et al. The efficacy and safety of one-stage endoscopic treatment for ascending acute cholangitis caused by choledocholithiasis with severe comorbidities. Surg. Endosc. 34, 3963–3970 (2020).
Orlandini, B. et al. Fibrin glue injection: Rescue treatment for refractory post-sphincterotomy and post-papillectomy bleedings. Dig. Endosc. 33, 815–821 (2021).
Doshi, B. et al. Current endoscopic strategies for managing large bile duct stones. Dig. Endosc. 30(Suppl 1), 59–66 (2018).
Khashab, M. A. et al. Delayed and unsuccessful endoscopic retrograde cholangiopancreatography are associated with worse outcomes in patients with acute cholangitis. Clin. Gastroenterol. Hepatol. 10, 1157–1161 (2012).
Novy, E. et al. Prognostic factors associated with six month mortality of critically ill elderly patients admitted to the intensive care unit with severe acute cholangitis. HPB (Oxford) 23, 459–467 (2021).
Touzani, S. et al. Factors associated with mortality in severe acute cholangitis in a moroccan intensive care unit: A retrospective analysis of 140 cases. Gastroenterol. Res. Pract. 2021, 4583493 (2021).
Park, S. Y. et al. Intraductal US-directed management of bile duct stones without radiocontrast cholangiography. Gastrointest. Endosc. 82, 939–943 (2015).
Ridtitid, W. et al. Uncomplicated common bile duct stone removal guided by cholangioscopy versus conventional endoscopic retrograde cholangiopancreatography. Surg. Endosc. 32, 2704–2712 (2018).
Lenze, F. et al. Safety, diagnostic accuracy and therapeutic efficacy of digital single-operator cholangioscopy. United Eur. Gastroenterol. J. 6, 902–909 (2018).
Maydeo, A. P. et al. Cholangioscopy-guided lithotripsy for difficult bile duct stone clearance in a single session of ERCP: Results from a large multinational registry demonstrate high success rates. Endoscopy 51, 922–929 (2019).
Acknowledgements
We thanked Mrs. Qingmei Ji, Yuanyuan Han and Danhui Zhu from Digestive Endoscopy Center, Zhongda Hospital, and Dr. Lanqi Guo from ICU, Zhongda Hospital for their help in all medications.
Funding
This research was supported by Technological Development Program of Nanjing Healthy Commission (YKK22276).
Author information
Authors and Affiliations
Contributions
Yadong Feng and Liang Pan conceptualized and designed this study. Yadong Feng, Yan Liang and Yuanyuan Li performed endoscopic interventions. Shuaijing Huang and Yan Liang were in charge of prior endoscopic intervention assessment and further medications. Shuaijing Huang, Bin Wang and Yang Liu performed follow-up. Ruihua Shi supervised this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, S., Liang, Y., Li, Y. et al. Digital cholangioscope assisted radiation-free bedside one-stage endoscopic lithotomy and biliary drainage for severe acute cholangitis caused by choledocholithiasis. Sci Rep 14, 18830 (2024). https://doi.org/10.1038/s41598-024-69943-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-69943-x
This article is cited by
-
Safety and efficacy of single-stage endoscopic stone removal and the timing of ERCP for acute cholangitis: a multicenter study
BMC Gastroenterology (2026)
-
Beyond the Shadows: Redefining ERCP Without Radiation
Digestive Diseases and Sciences (2025)