Abstract
Stroke is a severe cerebrovascular disease. This study aimed to determine the association between triglyceride‑glucose (TyG) index and stroke among middle-aged and elderly Chinese. Data was extracted from China Health and Retirement Longitudinal Study survey 2015 and survey 2018. Logistic regression, trend test and subgroup analysis were conducted to assess the association. Possible nonlinear relationships were explored with restricted cubic spline (RCS). Propensity score matching (PSM) was conducted to attenuate the effect of confounding factors. ORs of stroke was positively associated with TyG index. The ORs in RCS analysis also increased with the rising TyG, though p for non-linearity was bigger than 0.05. After PSM, the ORs in the full adjusted models were 1.28 (1.01, 1.62). TyG was suggested as an independent risk factor for stroke in the middle aged and elderly Chinese.
Similar content being viewed by others
Introduction
Stroke remains a global risk to public health, which is a pernicious source of mortality and loss of independence in those afflicted1. Therefore, it is essential to focus on the prevention of stroke attack. Till now, numbers of elements have been identified as stimulators to stroke. For example, the ageing problem was obviously related with the prevalence of stroke2,3,4; Some chronic diseases such as hypertension and atrial fibrillation were also proved as critical risk factors to stroke5,6. Except those, lipid and glucose metabolic alterations have been demonstrated to involves in the pathogenesis of stroke7,8,9,10,11. However, an interesting phenomenon is that patients with severe stroke tend to have lower serum triglyceride levels12, which seems conflict with its stimulating effect to stroke. Besides, the fluctuation of serum glucose level varies among stroke patients13, and it has been reported that greater glucose variability could impair the neurological improvement14. Nonetheless, researchers found serum glucose is positively correlated with functional outcome in acute stroke patients15. Therefore, the glucolipid metabolism among stroke patients differs from the normal persons, both glucose and triglyceride appear contrary effect on stroke pathological process. Given that, it is necessary to further explore the affection of glucolipid-related factors to stroke.
TyG index, which is calculated as the formular Ln (fasting triglycerides [TG, mg/dl] × fasting blood glucose [mg/dl]/2), recently gained popularity in clinical practice. It was initially used to estimate insulin resistance (IR)16,17,18. Recent studies also revealed that TyG correlated with the stimulative factors for atherogenesis, such as endothelial dysfunction, thrombosis, glucolipid metabolism disorders and inflammation19,20. In addition, TyG is closely related to the prevalence of cardiovascular system diseases such as arterial stiffness, coronary artery disease, etc.21,22. However, the effect of TyG index has not been well explored in stroke, and its possibility to predict stroke remains insufficiently evaluated. In view of this, CHARLS was utilized to determine the association between TyG index and the prevalence of stroke in the middle and elderly Chines population.
Methods
Data source and sample
Information was retrieved from the CHARLS (survey 2015 and survey 2018). CHARLS is a nationwide survey conducted by the Chinese Center for Disease Control and Prevention. The participants were from 28 provinces and 150 counties in China. The surveys mainly contain two parts: home interview and a medical examination; and it offered health information, demographics, socioeconomic status as well as physical and physiological measurements of Chinese middle and aged population. Specific descriptions regarding the CHARLS could be accessed via the official study website (http://charls.pku.edu.cn/) or publications23.
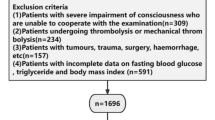
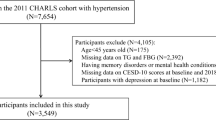
In the present study, there are a total of 21,095 participants were involved in survey 2015. The excluding criteria were displayed as follows: (1) participants aged less than 45; (2) lack of fasting blood glucose or triglyceride to calculate TyG; (3) participants with stroke in the CHARLS 2015 survey. There were 1965 participants lost and 889 ones died during the follow-up. After data cleaning, there are a total of 11,196 individuals adopted to analysis. The detail was shown in Fig. 1.
All procedures performed in this study were in accordance with the Declaration of Helsinki (revised in 2013) and were approved by the Ethics Committee of Peking University (IRB 00001052-11014).
Data collection and covariates
In CHARLS survey, basic information was obtained through questionnaires and physical examination by experienced interviewers23. Fasting venous blood of participants was collected and centrifuged to acquire plasma, then they were immediately stored under appropriate frozen condition (-20℃) until transporting to the Chinese Center for Disease Control and Prevention in Beijing for testing within 2 weeks. Laboratory results were obtained from serum specimens. Blood biomarkers including triglyceride, blood glucose, low-density lipoprotein (LDL), etc., were determined using enzymatic colorimetric tests23,24.
TyG index was calculated as Ln (fasting triglycerides [mg/dl] × fasting blood glucose [mg/dl]/2)25. Then, the study population was divided into 4 groups according to the quartiles (Qs) of TyG. The evaluation of stroke was mainly based on self-reported physician diagnosis. The participants were asked, “Have you been diagnosed with stroke by a doctor?” Answers from respondents were recorded by the researchers26,27.
The covariates involved in this study were list as follows. Demography characteristics mainly contains age, gender, marital status, settlements, cigarette consumption, body mass index; daily living behaviors includes alcohol consumption, sleep duration, afternoon napping, depression reflected by the Center for Epidemiologic Studies Depression scale (CESD)-10 questionnaire; basic health condition involves hepatic disease, renal disease, digestive disease, renal disease, heart disease, diabetes mellitus (DM), hypertension (HP), arthritis, hyperuricemia and laboratory examinations such as blood urea nitrogen (BUN), LDL, total cholesterol. Marital status was categorized into two groups: with spouse present and others (containing single, divorced or widowed status). Cigarette consumption was categorized into 2 groups: current smoker (current smoking) and non-smoker (including participants quite smoking). Depression was assessed by CESD-10, and participants got score > 10 were identified as depressive state28. Hyperuricemia was defined as uric acid ≥ 420 μmol/L for the male population and ≥ 357 μmol/L for the female population29. Hepatic diseases included hepatitis, liver cyst, hepatic aneurysm, etc. except for fatty liver, tumors, and cancer. Renal diseases (excluding tumor or cancer) included kidney calculi, chronic kidney diseases, etc. Digestive diseases (excluding tumor or cancer) covered digestive ulcer, gastritis, etc. Basic characteristics were converted into categorical variables and digitally coded before logistical regression. The coding was displayer as follows: age grade (45 to 60 years = 1, ≥ 60 years = 2), stroke (no = 0,yes = 1), gender (male = 1, female = 2), marital status (with spouse present = 1, others = 0), settlements (suburb area = 1, rural area = 0), cigarette consumption (current-smoker = 1, non-smoker = 2), alcohol consumption (drink more than once a month = 1, drink less than once a month = 2), nap (no = 0,yes = 1), sleep duration (< 6 h less than 6 h = 1, 6–8 h = 2, ≥ 8 h hours = 3), blood urea nitrogen (< 20 mg/dL = 0, ≥ 20 mg/dL = 1), low density lipoprotein (< 120 mg/dL = 0, ≥ 120 mg/dL = 1), total cholesterol (< 200 mg/dL = 0, ≥ 200 mg/dL = 1), hyperuricemia (bigger than 420 μmol/L in male = 1 or bigger than 357 μmol/L in female = 1, or else = 0), depression (no = 0, yes = 1), arthritis (no = 0, yes = 1), heart disease (no = 0, yes = 1), digestive disease (no = 0, yes = 1), renal disease (no = 0, yes = 1), hepatic disease (no = 0, yes = 1), HP. (no = 0, yes = 1), DM(no = 0, yes = 1).
Statistical analyses
All analyses were performed using Stata 16.1 (Stata Corporation, College Station, TX, United States) and R software 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria). Data with normal distribution were presented as mean ± standard deviation, and those with non-normal distribution were displayed as median (25–75% quantiles) in continuous variables. Categorical data are shown as proportions (%). One-way analysis of variance, Kruskal–Wallis, or chi-square test were used to test differences among the groups depending on the data type and distribution. Four logistic regression models were established to assess the association between TyG and stroke Model 1: univariable logistic regression; Model 2: adjusted by age grade, gender, marital and region; Model 3: further adjusted by sleep, nap, smoke, drink and depression based on model 2; Model 4: further adjusted by hyperuricemia, BUN, LDL, total cholesterol, heart disease, hepatic disease, renal disease, digestive disease, arthritis, DM, HP, and BMI based on model 3. Then tendency analysis was performed. Glucolipid metabolism can be influenced by factors such as gender30, alcohol consumption31, cigarette consumption32 and sleep duration33, etc., meanwhile, HP and DM were considered as the traditional risk factors. Therefore, subgroup analysis was conducted in these covariates to further explore the association. Restricted cubic spline was adopted to model and visualize the relationship between stroke and TyG with 3 knots34. To attenuate the affection of confounding factors, PSM was employed to balance the covariates between the two groups which were bound by the median of TyG. The caliper of nearest neighbor matching was set at 0.03, and 1:1 no-replacement matching was adopted. After PSM, univariable and multivariable logistic regression were conducted again to assess the association between TyG and stroke. P < 0.05 (two-sided) was considered statistically significant.
Ethical approval and consent to participate
All procedures performed in this study were in accordance with the Declaration of Helsinki (revised in 2013) and were approved by the Ethics Committee of Peking University (IRB 00001052-11014). All participants provided written informed consent. No experimental interventions were performed.
Results
Demographic characteristics of the study population
A total of 11,196 participants attending the CHARLS 2015 were enrolled. Among them, 5135 were male, and 6059 were female. The median age of the enrolled participants was 60.00 [52.00, 67.00]. The participants were divided into four groups according to the quartiles of TyG: Q1 (TyG < 8.25), Q2(8.25 ≤ TyG < 8.62), Q3(8.62 ≤ TyG < 9.07), Q4(TyG ≥ 9.07). It showed that in Q4 group, participants were more likely to be female, living in suburb area and complicated with the chronic diseases such as hyperuricemia, HP and DM. There was no significant difference among the groups in marital status, depression, arthritis and digestive disease. The details of the baseline profiles are shown in Table 1.
The association between TyG and stroke among participants
The prevalence of stroke exhibited a gradually rising trend across the quartiles of TyG index, they were 4.14%, 4.78%, 6.33% and 6.86%, respectively. In all models, the ORs of stroke increased with the climbing of TyG levels. Besides, all p values for trend analysis showed statistical significance, though the p value were all bigger than 0.05. Especially, in the full adjusted model (Model 4), the ORs were 1.17(0.88, 1.56), 1.36(1.03, 1.80) and 1.38(1.03, 1.86) across Q2 to Q4 compared with the reference group. These results indicated that increase of TyG index was positively associated with the stroke risk among Chinese middle aged and elderly population. The details were shown in Table 2.
The subgroup analysis and interaction effect
Factors such as HP, DM, etc. were traditional risk factors to stroke. To further examine whether the positive association still exist in specific subgroups of these factors, the full adjusted multivariate logistic regression was employed for subgroup analyses. Results showed that all p values for interaction showed no statistically significant. This suggested that the in these subgroups, the levels of TyG still positively associated with the prevalence of stroke, and the model was comparatively robust. Details were displayed in Table 3.
Restricted cubic spline regression
Restricted cubic splines analysis was employed to flexibly model and visualize the association between TyG and stroke. In Fig. 2A, the curves generally presented a positive correlation between TyG and stroke; though the p for overall was 0.047, the p for non-linearity exhibited no statistical significance. This indicated the stroke risk was linearly correlated with TyG index. The same were found in the gender, HP and DM subgroups (Fig. 2B–D). Overall, apparent non-linear relationship was not found between the TyG and stroke in RCS analysis.
Propensity score matching analysis
In this part, participants were grouped by the median of TyG (8.62). Followed, PSM was conducted to attenuate the interference of confounding factors. The distribution of the propensity scores in the two groups were shown in Fig. 3A. Figure 3B–E exhibited the proportion of propensity scores in the raw groups (TyG < 8.62) and matched groups (TyG ≥ 8.62) before and after PSM; the histogram displayed a well-matched condition. After PSM, 3088 pairs of participants were reserved for further logistic regression. The baseline profiles after PSM were shown in Table 4, and the differences among the groups were apparently minimized. ORs of univariate and full adjusted logistic regression after were 1.36(1.08, 1.71) and 1.28(1.01, 1.62) (Fig. 4), suggesting the positive association between the TyG and risk of stroke existed.
Discussion
With the ageing problem rising, stroke attacks more frequently in the elder population, and becomes the third major cause of morbidity and mortality in many developed countries35; accordingly, exploration to supervise and alarm the attack of stroke is merited. CHARLS, a nationwide investigation targeting the aging problems in China, provided us the opportunity to explore the association between TyG index and stroke. To the best of our knowledge, this is the first study to examine the association between the stroke and TyG index among the population aged over 45 years in China using the nationally representative data. In this longitudinal analysis involving 11,196 participants, a positive association between stroke and TyG index was found, and the capabilities of TyG index to predict the risk of stroke were preliminarily verified.
As we know, stroke is the manifestation for cerebrovascular accident caused by the rupture or blockage of blood vessels. Besides HP and atrial fibrillation, atherosclerosis is one of the most important factors predisposing to stroke 36. Previous study has proved the risk of stroke in participants with the carotid atherosclerosis elevated to 2.55 times bigger than normal participants37. Moreover, the pathogenesis of atherosclerosis is mainly relevant to serum lipid such as cholesterol, triglycerides, high-density lipoprotein (HDL) and low-density lipoprotein. Among these markers, triglyceride has been verified to result in a higher risk of atherosclerosis with its increasing level in serum37. In addition, Jennifer S Lee, etc. discovered that high triglyceride plus low HDL levels were associated with a 2.13-fold greater risk for stroke. Given that, TyG as an indicator reflecting glucolipid metabolism may has the ability to predict the risk of stroke. In addition to impaired lipids metabolism described above, abnormal glycol-metabolism was also found to evoke stroke, for instance, it has been demonstrated that the morbidity of stroke increased to 132% when glucose variability exists38. In view of this, TyG integrating glucose metabolism and lipid metabolism, should have the capability to predict stroke.
In this paper, results from longitudinal logistic regression confirmed that the risk of stroke rose correspondingly with the increase of TyG; even after adjusted by the traditional risk factors such HP, DM, total cholesterol, etc., the positive association still hold. In the full adjusted model after PSM, the incidence rate of stroke raised by 28% in the fourth quartile compared with the first quartile. This indicates that TyG plays an essential, detrimental role in stroke patients, which could be another explanation for the residual risks of stroke. Trend analysis further strengthened and verified the tendency of stroke incidence increased with the range of TyG quartiles. Furthermore, nonlinear relationship between stroke and TyG index was explored by using RCS analysis. Though no exact U- or J- shaped line was discovered, the outcomes still indicated ORs of stroke linearly increased with the elevated TyG index. Moreover, PSM was conducted. And the positive association between stroke and TyG keep existing reflected by logistic regression and RCS after PSM, which enhanced the robustness of the model.
In essence, stroke is a critical cerebral-vascular accident. Therefore, the pathological effect of TyG and its components (triglyceride and glucose) to blood vascular matters. Researchers have certified TyG can induce the vascular related diseases. For example, higher TyG level and variability were independently associated with higher incidence of cardiovascular disease39. Besides, a cohort study with follow-up of 8.78 years demonstrated TyG index was positively associated with the risk of heart failure40. One of the underlying mechanisms may be related to the effect of TyG on the vascular system and results in cardiovascular and cerebrovascular diseases. This is also partially proven by some previous researches. Omar Sajdeya, etc. showed higher TyG index led to higher odds of subclinical atherosclerosis and arterial stiffness17. Another paper confirmed the significant association of the higher TyG index with brachial-ankle pulse wave velocity, which represent the arterial stiffness extent41. Moreover, Wenzhen Li directly demonstrated the participants with elevated TyG have higher prevalence of carotid intima-media thickness, plaques and stenosis severity by using ultrasonography 12. Taken together, TyG can influence the structure and reconstruction of vascular wall by the abnormal glucolipid metabolism, which further led to the vascular fragility and impair the inner and middle layer arterial wall, and finally the vascular accident emerged. Glucose and lipid metabolism could be influenced by specific factors such as gender30, alcohol consumption31, cigarette consumption32 and sleep duration33, etc. .Meanwhile, former studies documented that cigarette smoke can induce iron mediated mobilization from ferritin and other specific prooxidant mechanisms in vivo42. Besides, sleep disorder has been proved to affect the blood lipid composition and glucose level43. This indicates that the effect of TyG on stroke may be different in these subgroups. Therefore, subgroup group analysis was adopted. While all p for interaction showed no significance, suggesting the association do not differ in these subgroups. In conclusion, the positive association between TyG and the prevalence of stroke was discovered in this paper. TyG is a convenient and economical promising index to predict stroke in clinical practice.
In this study, although a national longitudinal survey was used to investigate the association between TyG and stroke, some limitations still should be noted. Part of the basic information collected from the respondents based on self-reports. Though this method has been reported practicably44, the disadvantages still existed. First, the information may be not that precise due to the participants lack of professional medical knowledge, and this could cause missing values and interfere the statistical analysis. Second, the diagnose of stroke based on questionnaire; This method might missed the participants who died of fatal stroke in the follow-up, which could cause bias in the longitudinal analysis. Third, the specific subtypes of stroke were not documented. According to the medical theory and previous articles, TyG are more likely to positively associated with the stroke caused by atherosclerotic pathological process. But because of absence of stroke subtypes, it is hardly to deduce which kind of subtypes are more relevant to high level of TyG. Prospective clinical study should be designed to cover the deficiency. Despites of these shortages, the longitudinal results still support TyG effect on predicting stroke to a certain extent, and may guide people adjusting the blood glucose and lipid levels.
Data availability
The datasets generated and/or analyzed during the current study are available in the CHARLS repository, http://charls.pku.edu.cn/.
Abbreviations
- BUN:
-
Blood urea nitrogen
- CESD:
-
Center for epidemiologic studies depression
- CHARLS:
-
China Health and Retirement Longitudinal Study
- CI:
-
Confidence interval
- DM:
-
Diabetes mellitus
- HP:
-
Hypertension
- IR:
-
Insulin resistance
- LDL:
-
Low-density lipoprotein
- PSM:
-
Propensity score matching
- Qs:
-
Quartiles
- RCS:
-
Restricted cubic spline
- TyG:
-
Triglyceride-glucose index
References
In Stroke (ed S. Dehkharghani) (Exon Publications Copyright© 2021 Exon Publications, 2021).
Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England) 388, 1603–1658. https://doi.org/10.1016/s0140-6736(16)31460-x (2016).
Johnston, S. C., Mendis, S. & Mathers, C. D. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet. Neurol. 8, 345–354. https://doi.org/10.1016/s1474-4422(09)70023-7 (2009).
Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England) 388, 1459–1544. https://doi.org/10.1016/s0140-6736(16)31012-1 (2016).
Buonacera, A., Stancanelli, B. & Malatino, L. Stroke and hypertension: An appraisal from pathophysiology to clinical practice. Curr. Vasc. Pharmacol. 17, 72–84. https://doi.org/10.2174/1570161115666171116151051 (2019).
Choi, S. E., Sagris, D., Hill, A., Lip, G. Y. H. & Abdul-Rahim, A. H. Atrial fibrillation and stroke. Expert Rev. Cardiovasc. Ther. 21, 35–56. https://doi.org/10.1080/14779072.2023.2160319 (2023).
Hackam, D. G. & Hegele, R. A. Lipid-modifying therapies and stroke prevention. Curr. Neurol. Neurosci. Rep. 22, 375–382. https://doi.org/10.1007/s11910-022-01197-4 (2022).
Dopler, B. Stroke prevention. Delaware J. Public Health 9, 6–10. https://doi.org/10.32481/djph.2023.08.003 (2023).
Herrington, W., Lacey, B., Sherliker, P., Armitage, J. & Lewington, S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ. Res. 118, 535–546. https://doi.org/10.1161/circresaha.115.307611 (2016).
Shi, Y. et al. Risk factors for ischemic stroke: differences between cerebral small vessel and large artery atherosclerosis aetiologies. Folia Neuropathol. 59, 378–385. https://doi.org/10.5114/fn.2021.112007 (2021).
Gujjar, A. R. Diabetes and stroke: More than just accelerated atherosclerosis?. Sultan Qaboos Univ. Med. J. 18, e261–e263. https://doi.org/10.18295/squmj.2018.18.03.001 (2018).
Devulapalli, R. Correlation between serum triglyceride levels and severity of stroke. J. Assoc. Physicians India 70, 11–12 (2022).
Peng, X. et al. Longitudinal average glucose levels and variance and risk of stroke: A Chinese cohort study. Int. J. Hypertens. 2020, 8953058. https://doi.org/10.1155/2020/8953058 (2020).
Palaiodimou, L. et al. Glycemic variability of acute stroke patients and clinical outcomes: A continuous glucose monitoring study. Ther. Adv. Neurol. Disord. 14, 17562864211045876. https://doi.org/10.1177/17562864211045876 (2021).
Ntaios, G., Egli, M., Faouzi, M. & Michel, P. J-shaped association between serum glucose and functional outcome in acute ischemic stroke. Stroke 41, 2366–2370. https://doi.org/10.1161/strokeaha.110.592170 (2010).
Son, D. H., Lee, H. S., Lee, Y. J., Lee, J. H. & Han, J. H. Comparison of triglyceride-glucose index and HOMA-IR for predicting prevalence and incidence of metabolic syndrome. Nutr. Metab. Cardiovasc. Dis. 32, 596–604. https://doi.org/10.1016/j.numecd.2021.11.017 (2022).
Sajdeya, O. et al. Triglyceride glucose index for the prediction of subclinical atherosclerosis and arterial stiffness: A meta-analysis of 37,780 individuals. Curr. Probl. Cardiol. 47, 101390. https://doi.org/10.1016/j.cpcardiol.2022.101390 (2022).
Vasques, A. C. et al. TyG index performs better than HOMA in a Brazilian population: A hyperglycemic clamp validated study. Diabetes Res. Clin. Pract. 93, e98–e100. https://doi.org/10.1016/j.diabres.2011.05.030 (2011).
Demirci, I. et al. Triglyceride-glucose index levels in patients with congenital hypogonadotropic hypogonadism and the relationship with endothelial dysfunction and insulin resistance. Endokrynol. Pol. 72, 232–237. https://doi.org/10.5603/EP.a2021.0019 (2021).
Jiang, Z. Z. et al. A high triglyceride-glucose index value is associated with an increased risk of carotid plaque burden in subjects with prediabetes and new-onset type 2 diabetes: A real-world study. Front. Cardiovasc. Med. 9, 832491. https://doi.org/10.3389/fcvm.2022.832491 (2022).
Wang, X. et al. Association between the triglyceride-glucose index and severity of coronary artery disease. Cardiovasc. Diabetol. 21, 168. https://doi.org/10.1186/s12933-022-01606-5 (2022).
Wu, S. et al. Association between triglyceride-glucose index and risk of arterial stiffness: A cohort study. Cardiovasc. Diabetol. 20, 146. https://doi.org/10.1186/s12933-021-01342-2 (2021).
Zhao, Y., Hu, Y., Smith, J. P., Strauss, J. & Yang, G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 43, 61–68. https://doi.org/10.1093/ije/dys203 (2014).
Xiong, Y., Zhang, Y., Tan, J., Qin, F. & Yuan, J. The association between metabolic syndrome and lower urinary tract symptoms suggestive of benign prostatic hyperplasia in aging males: Evidence based on propensity score matching. Transl. Androl. Urol. 10, 384–396. https://doi.org/10.21037/tau-20-1127 (2021).
da Silva, A. et al. Triglyceride-glucose index is associated with symptomatic coronary artery disease in patients in secondary care. Cardiovasc. Diabetol. 18, 89. https://doi.org/10.1186/s12933-019-0893-2 (2019).
Li, W., Taskin, T., Gautam, P., Gamber, M. & Sun, W. Is there an association among sleep duration, nap, and stroke? Findings from the China Health and Retirement Longitudinal Study. Sleep Breathing = Schlaf & Atmung 25, 315–323. https://doi.org/10.1007/s11325-020-02118-w (2021).
Yang, D. et al. Associations between intensity, frequency, duration, and volume of physical activity and the risk of stroke in middle- and older-aged Chinese People: A cross-sectional study. Int. J. Environ. Res. Public Health 17, e13568. https://doi.org/10.3390/ijerph17228628 (2020).
Andresen, E. M., Byers, K., Friary, J., Kosloski, K. & Montgomery, R. Performance of the 10-item Center for Epidemiologic Studies Depression scale for caregiving research. SAGE open medicine 1, 2050312113514576. https://doi.org/10.1177/2050312113514576 (2013).
Jayachandran, M. & Qu, S. Harnessing hyperuricemia to atherosclerosis and understanding its mechanistic dependence. Med. Res. Rev. 41, 616–629. https://doi.org/10.1002/med.21742 (2021).
Link, J. C. & Reue, K. Genetic basis for sex differences in obesity and lipid metabolism. Annu. Rev. Nutr. 37, 225–245. https://doi.org/10.1146/annurev-nutr-071816-064827 (2017).
Jeon, S. & Carr, R. Alcohol effects on hepatic lipid metabolism. J. Lipid Res. 61, 470–479. https://doi.org/10.1194/jlr.R119000547 (2020).
Zhang, Y. et al. SIRT1 prevents cigarette smoking-induced lung fibroblasts activation by regulating mitochondrial oxidative stress and lipid metabolism. J. Transl. Med. 20, 222. https://doi.org/10.1186/s12967-022-03408-5 (2022).
Broussard, J. & Brady, M. J. The impact of sleep disturbances on adipocyte function and lipid metabolism. Best Pract. Res. Clin. Endocrinol. Metab. 24, 763–773. https://doi.org/10.1016/j.beem.2010.08.007 (2010).
Xiong, Y., Zhang, Y. C., Jin, T., Qin, F. & Yuan, J. H. Depressive males have higher odds of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A retrospective cohort study based on propensity score matching. Asian J. Androl. 23, 633–639. https://doi.org/10.4103/aja.aja_12_21 (2021).
Unnithan, A. K. A., J, M. D. & Mehta, P. in StatPearls (StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC., 2023).
Majerczyk, M., Wajda, J., Holecki, M. & Chudek, J. Osteoprotegerin as a marker of atherosclerosis and a prognostic factor in stroke. Postepy Hig. Med. Dosw.(Online) 69, 1505–1511 (2015).
Ohira, T. et al. Carotid artery wall thickness and risk of stroke subtypes: the atherosclerosis risk in communities study. Stroke 42, 397–403. https://doi.org/10.1161/strokeaha.110.592261 (2011).
Lee, D. Y. et al. Glucose variability and the risks of stroke, myocardial infarction, and all-cause mortality in individuals with diabetes: retrospective cohort study. Cardiovasc. Diabetol. 19, 144. https://doi.org/10.1186/s12933-020-01134-0 (2020).
Li, H. et al. Triglyceride-glucose index variability and incident cardiovascular disease: a prospective cohort study. Cardiovasc. Diabetol. 21, 105. https://doi.org/10.1186/s12933-022-01541-5 (2022).
Xu, L. et al. Triglyceride-glucose index associates with incident heart failure: A cohort study. Diabetes Metab. 48, 101365. https://doi.org/10.1016/j.diabet.2022.101365 (2022).
Su, Y. et al. Triglyceride glucose index associated with arterial stiffness in Chinese community-dwelling elderly. Front. Cardiovasc. Med. 8, 737899. https://doi.org/10.3389/fcvm.2021.737899 (2021).
Lapenna, D. et al. Cigarette smoke, ferritin, and lipid peroxidation. Am. J. Respir. Crit. Care Med. 151, 431–435. https://doi.org/10.1164/ajrccm.151.2.7842202 (1995).
Barikani, A., Javadi, M. & Rafiei, S. Sleep quality and blood lipid composition among patients with diabetes. Int. J. Endocrinol. Metab. 17, e81062. https://doi.org/10.5812/ijem.81062 (2019).
Hare, D. L., Toukhsati, S. R., Johansson, P. & Jaarsma, T. Depression and cardiovascular disease: A clinical review. Eur. Heart J. 35, 1365–1372. https://doi.org/10.1093/eurheartj/eht462 (2014).
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, F., Feng, Y. & Zhong, X. Higher triglyceride‑glucose index is associated with increased risk of stroke among middle-aged and elderly Chinese: a national longitudinal study. Sci Rep 14, 19054 (2024). https://doi.org/10.1038/s41598-024-70008-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70008-2
Keywords
This article is cited by
-
Association between dynamic changes in the triglyceride-glucose index and prognosis in patients with acute ST-segment elevation myocardial infarction
Cardiovascular Diabetology (2025)
-
Does diabetes modify the triglyceride–glucose index associated with cardiovascular events and mortality? A meta-analysis of 50 cohorts involving 7,239,790 participants
Cardiovascular Diabetology (2025)
-
Joint effects of triglyceride glucose index and its obesity-related derivatives with estimated glucose disposal rate on cardiometabolic multimorbidity in middle-aged and older Chinese adults: a nationwide cohort study
Cardiovascular Diabetology (2025)
-
Assessment of six insulin resistance surrogate indexes for predicting stroke incidence in Chinese middle-aged and elderly populations with abnormal glucose metabolism: a nationwide prospective cohort study
Cardiovascular Diabetology (2025)
-
Association between the triglyceride glucose-Chinese visceral adiposity index and new-onset stroke risk: a national cohort study
Cardiovascular Diabetology (2025)