Abstract
Bariatric surgery is an approved treatment for obesity that consistently improves metabolic syndrome, with well-documented beneficial effects on dyslipidemia, cardiovascular risk, nonalcoholic fatty liver disease and glucose homeostasis. In this study, we determined the differential expression genes in three periods after bariatric surgery: short-term (4-months), medium-term (1- and 2-years), and long-term (5-years) periods. Two microarray profiles were downloaded from the Gene Expression Omnibus (GEO) database. Differentially expressed genes (DEGs) were identified by comparing the expression of adipose tissue genes before surgery compared to short, medium and long-term periods following surgery. Shared DEGs for the medium-term were evaluated by comparing the DEGs for both 1 and 2 years. 165, 65, and 59 DEGs were identified in short–medium–long periods. The protein–protein interactions were analyzed by STRING. A co-expression network was constructed by mapping the DEGs onto the GeneMANIA plugin of Cytoscape. Gene Ontology (GO) enrichment, Kyoto Encyclopedia of Genes and Genomes (KEGG) and wikipathway analysis were done for each group of DEGs. Interleukin-8 receptor activity, complement receptor activity and opsonin receptor activity/N-formyl peptide receptor activity in GO Function enrichment and cellular response to interleukin-8, positive regulation of hippocampal neuron apoptotic process, and positive regulation of hippocampal neuron apoptotic process in GO Process showed the best scores in short-, medium-, and long-term periods, respectively. Eight genes, including CCL2 (Chemokine ligand 2), CXCR4 (CXC motif chemokine receptor 4), EGR2 (Early Growth Response 2), FPR1 (Formyl Peptide Receptor 1), IL6 (interleukin-6), RGS2 (regulator of gene protein signaling2), SELPLG (Selectin P Ligand), and THBS1 (Thrombospondin 1) were identified as shared DEGs in the three periods after surgery. Importantly, results of DAVID database analysis showed 7, 6, 4, and 4 of these genes have roles in immune/ cancer/cardiovascular diseases, type 2 diabetes, myocardial infarct, and atherosclerosis, respectively.
Similar content being viewed by others
Introduction
Obesity is increasing in prevalence resulting in a global epidemic. In patients with severe obesity, bariatric surgery can be an effective intervention resulting in significant and sustained weight loss with documented effects on improving health-related quality of life, longevity and remission of type 2 diabetes (T2D)1,2,3,4,5,6,7,8,9,10,11,12. Bariatric surgery may be performed using several different procedures that include Roux-en-Y gastric bypass, sleeve gastrectomy, adjustable gastric band, biliopancreatic diversion with duodenal switch, and single anastomosis duodeno-ileal bypass with sleeve gastrectomy13. Various bariatric surgery proceedures are associated with substantial and durable weight loss14. Many benefits of bariatric surgery appear to occur rapidly after surgery with a marked reduction in cardiovascular risk factors15 and with rapid improvement in glycemic control in those with diabetes16, effects that may last at least 12 years10. It is therefore evident that the clinical and biochemical parameters improve following bariatric surgery10, but it is unclear if the metabolic processes normalize even if body mass index (BMI) remains elevated above the accepted upper limit of normal (BMI above 25kg/m2).
Microarray is a technology to show gene expression patterns in various tissues, which can help us understand the biology and molecular mechanisms. This tool can be used to find differentially expressed genes (DEGs), biomarkers, and therapeutic targets17. Increasing global obesity and its associated public health burden underscores a pressing need for early biomarker predictors of weight-loss success. There is differential gene expression after bariatric surgery, as shown in the bioinformatic study on subcutaneous adipose tissue, which demonstrated differential gene expression for immunoregulation after bariatric surgery. Identification differential gene expression after bariatric surgery could help scientists to elucidate the mechanistic beneficial effects of bariatric surgery. The gene MXRA5 was suggested to be involved in the regulation of lipid metabolism18. This is indicative of the metabolic processes and improved function19 that are reported following surgery. The differential gene expression at differing time points following surgery is less clear; however, their analysis would give an indication of the overarching dynamic processes occurring because of surgery, whether these are maintained after surgery or if they return to pre-surgery expression levels, hence the rationale for this study.
Methods
Data collection and preprocessing
We used two gene expression profiles including GSE29411 and GSE199063 to explore the gene expression differences caused by bariatric surgery (Table 1). These data were downloaded from the Gene Expression Omnibus (GEO, https://www.ncbi.nlm.nih.gov/geo) and preprocessed with GEO2R (Version information of R script: R 3.2.3, Biobase 2.30.0, GEOquery 2.40.0, limma 3.26.8).
Identification of DEGs
Differentially expressed genes (DEGs) before and after surgery were constructed, short-, medium- and long-term periods were investigated as shown in Table 2. For the medium-term period, shared DEGs between the two time points, one and 2 years, were assessed. Genes with a Log fold change (LFC) > 1 and p-value < 0.05 were considered to be DEGs. A positive fold change value indicates an increase in gene expression, while a negative fold change indicates a decrease in gene expression. A p-value of < 0.05 was accepted as showing significant gene expression changes. The series matrix files were annotated with official gene symbols using the platform files and annotation packages in the R software. For GSE199063, only NCBI accession numbers were given, which were converted to the gene symbols using the NCBI database (https://www.ncbi.nlm.nih.gov/). Venn plot, volcano plot, and gene fold change bar plot created by SRPLOT tools (https://www.bioinformatics.com.cn/en). Other related plots were created using GEO2R analysis.
Interaction networks
The STRING online tool (https://string-db.org/) was used for the identification of protein–protein interactions (PPI) of identified DEGs. The STRING database covers the number of 67.6 million proteins from 14,094 organisms. It provides direct (physical) interactions and indirect (functional) associations; they stem from computational prediction, knowledge transfer between organisms, and from interactions aggregated from other (primary) databases.
The interaction networks at the gene level were built by the GeneMANIA Cytoscape plugin. Gene co-expression network of DEGs contain physical, co-expression, and pathway gene–gene interactions were constructed. Moreover, Transcription Factor Enrichment Analysis (TFEA), Kinase Enrichment Analysis (KEA), and eXpression2Kinases Network were retrieved from X2Kweb (https://maayanlab.cloud/X2K/).
Gene ontology and pathway enrichment analysis.
Gene ontology, KEGG and WIKIpathway analysis were retrieved from string results. Pathway analysis bar graph of DEGs after weight loss was retrieved from EnrichR (https://maayanlab.cloud/Enrichr/).
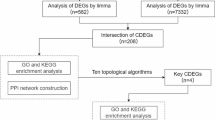
Evaluation of shared key genes in short-, medium- and long-term periods after metabolic surgery
DEGs identified in short-, medium- and long-term periods were compared and shared DEGs in these three periods were discovered. The effect of these genes in metabolic-related disease was evaluated using DAVID bioinformatics resources (https://david.ncifcrf.gov) and were converted to GO chord format using metascape to GO chord format conversion tool (https://www.bioinformatics.com.cn/GO_chord_data_format_convert_t002_en). Then chord plots were designed using GO chord tool (https://www.bioinformatics.com.cn/plot_basic_GOplot_chord_plot_085_en).
Results
Identification of the DEGs
Bariatric surgery was considered as the target treatment; therefore, gene expression of patients before and after treatment was compared. Plots including volcano plot, gene expression value distribution for dataset, Q-Q plot, mean variance trend and expression density curve were applied for each comparison of the datasets (Fig. 1).
Identification of DEGs. Rows: 1: after 4 months, 2: after 1 year, 3: after 2 years, 4: after 5 years. Columns: A. volcano plot, B. Gene expression value distribution for dataset (Each box plot represents gene expression value of one patient sample), C: Q-Q plot, D: mean variance trend, E: expression density curve.
The genes with p-value < 0.05 and │LFC│ > 1 were considered DEGs. DEGs of GSE29411 and GSE199063 in each group were identified (Table 2).
Identification of DEGs in short-term following bariatric surgery
In GSE29411, we compare gene expression before and 4 months (short-term) after bariatric surgery. In total, 92 up- and 73 down-regulated DEGs were found for short-term and Supplementary Table 1 shows the list of identified DEGs in short-term after bariatric surgery. The top 20 DEGs for short-term, based on the magnitude of │LFC│, was given in the gene fold change bar plot (Fig. 2A). FOSB, NR4A2, and FOS were the most up-regulated and CSN1S1 and EGFL6 were the most down-regulated for short-term DEGs. Further X2K analysis were done to identify up-stream regulation of the top short-term DEGs. Results demonstrated STAT3, SRF, and RUNX1 and MAPK1, CDK1, and ERK1 as up-stream transcription factors and kinases (Fig. 2B–D).
Identification of DEGs in medium-term following bariatric surgery
DEGs in each data sets of GSE199063 and GSE29411 were identified compared to baseline prior to surgery (Supplementary Tables 2 and 3). Subsequently, the 515 DEG genes in GSE199063 were compared with the 300 DEGs in GSE29411. Finally, 65 shared DEGs in the medium-term were identified (Fig. 3 and Table 3). IL6, RGS1, CCL2, and EGR2 were the most up-regulated and TF, SLC7A10, and FGFBP2 were the most down-regulated DEGs in the medium-term. Up and down regulated genes were shown in gene fold change bar plot (Fig. 4A and B). Further X2K analysis were done to identify up-stream regulation of top medium-term DEGs. Results demonstrated SPI1, RUNX1, POU5F1 and CSNK2A1, MAPK1, and MAPK3 as up-stream transcription factors and kinases (Fig. 4C–E).
Gene fold change bar plot of shared DEGs in the medium-term following bariatric surgery. (A) Fold change of genes after 2 years in GSE199063. (B) Fold change of genes after 1 year in GSE29411. Red bars represent up-regulated genes and green bars represent down-regulated genes. (C) Transcription Factor Enrichment Analysis (TFEA). (D) Kinase Enrichment Analysis (KEA). (E) eXpression2Kinases Network. CCL2, and EGR2 TF, SLC7A10, and FGFBP2.
Identification of DEGs in long-term following bariatric surgery
In GSE199063, gene expression was compared before and 5 years after bariatric surgery. In total, 59 up- and 43 down-regulated DEGs were found in long-term following bariatric surgery as shown in Supplementary Table 4. Top 20 DEGs in long-term based on the magnitude of │LFC│ was given in the gene fold change bar plot (Fig. 5A). TYROBP, FCER1G, and VSIG4 and ELOVL6 were the most up-regulated and SLC27A2 and PKP2 were the most down-regulated long-term DEGs. Further X2K analysis were done to identify up-stream regulation of top long-term DEGs. Results demonstrated SPI1, RUNX1, and IRF8 and MAPK3, ABL1, and MAPK1 as up-stream transcription factors and kinases (Fig. 5B–D).
Interaction networks of the DEGs
The PPI was analyzed by the STRING online tool. In total, 401 DEGs in short-term, 65 DEGs in medium-term, and 855 DEGs in long-term were separately analyzed (Fig. 6). Properties of the networks are shown in Table 4. P-values of all these networks are very significant, indicating that the proteins have more interactions among themselves than what would be expected for a random set of proteins of the same size and degree distribution drawn from the genome. Such an enrichment indicates that the proteins are at least partially biologically connected as a group.
Co-expression network for DEGs were constructed by mapping genes onto a database of functional-interaction datasets in the GeneMANIA plugin of Cytoscape (Fig. 7). Gene-correlation interactions consisting of 182 nodes and 5040 edges in short-term, 85 nodes and 2589 edges in medium-term, and 79 nodes and 2574 edges in long-term.
GO enrichment and, pathway analysis
GO enrichments including component, function, and process were done for each group of DEGs. Five top results of GO enriched terms in each time period based on the false discovery rate and strength are shown in Table 5. Moreover, Pathway analysis using KEGG and WikiPathways studies were done for each group of DEGs. Five top pathway results in each time period based on the false discovery rate and strength are shown in Table 6.
Key DEGs in short-, medium- and long-term periods after bariatric surgery
Shared DEGs in short-, medium- and long-term periods were evaluated and named as key genes. 8 key genes including CCL2, CXCR4, EGR2, FPR1, IL6, RGS2, SELPLG, and THBS1 were identified as shared genes in the three periods (Table 7). The effect of these genes on metabolic-related diseases was investigated. As shown in Fig. 8, results of DAVID database showed that 7 genes have roles in immune, cancer, and cardiovascular diseases. Moreover, 6, 4, and 4 genes play roles in Type 2 Diabetes, myocardial infarct and atherosclerosis, respectively.
Comparing DEGs after bariatric surgery with DEGs after diet-induced weight loss
To explain whether the gene expression change that occurred was due to weight loss or due to the impact of surgery, we used microarray data set from subcutaneous adipose tissue obtained in 27 moderate obese women who underwent diet induced weight loss (GSE112307). Gene expression before and after diet induced weight loss was analyzed and DEGs were identified. Diet-DEGs were compared with three sets of DEGs (short, medium, and long-term following bariatric surgery) separately; however, no similar DEGs were found. Further functional analysis showed that diet-DEGs impacted on pathways of the Sterol Regulatory Element Binding Proteins (SREBP) signaling, biosynthesis of unsaturated fatty acids, and regulation of cholesterol biosynthesis by SREBP (Fig. 9).
Evaluation of key DEGs
To evaluate the identified key DEGs, we evaluated identified key DEGs in another microarray dataset (GSE83223) that contain transcriptional profiling of women following Roux-en-Y Gastric Bypass in peripheral blood samples. LFC of key DEGs in this dataset after 6 months is shown in Fig. 10. Expression of IL6 and CCL2 were not found in this dataset. RGS2, EGR2, CXCR4, SELPLG, THBS1, FPR1 were found to be up-regulated in adipose samples after bariatric surgery in three time point. Similarly, in blood samples of GSE83223 profile, CXCR4, SELPLG, THBS1, FPR1 were upregulated; although, RGS2 and EGR2 were down-regulated.
Discussion
This study has shown that there was a marked increase in the number of DEGs following bariatric surgery. The best scores in the short, medium, and long-term period following bariatric surgery were for interleukin-8 receptor activity, complement receptor activity and opsonin receptor activity/N-formyl peptide receptor activity in GO Function enrichment and cellular response to interleukin-8, positive regulation of hippocampal neuron apoptotic process and positive regulation of hippocampal neuron apoptotic processes. Eight genes including CCL2, CXCR4, EGR2, FPR1, IL6, RGS2, SELPLG, and THBS1 were identified as sharing DEGs in the three periods after surgery. These genes have roles in immunity, cancer and cardiovascular diseases and have been related to disease processes, including type 2 diabetes, myocardial infarction, and atherosclerosis. This is seen from a clinical perspective with an improvement in diabetes10,23 a reduction in cardiovascular events24 and the long-term reduction in cancer incidence25.
Rapid weight loss following surgery is anticipated, with a sustained and progressive loss over the first year that tends to plateau after that26. Marked improvement in the metabolic features is seen in the short term (4 months), and therefore it was expected that the DEGs would be increased compared to baseline following surgery; however, the number of DEGs increased further at 1 year and then overall fell subsequently, though still greater than baseline. The chemokine CCL2, which has an important role in the infiltration of monocytes/macrophages in inflammation27, increased within 4 months and increased further at 1 year before decreasing thereafter, but not to presurgical levels. CXCR4, which improves T cell homing and function28, increased within 4 months and increased further at 1 year before decreasing to presurgical levels at 2 years, but it is unclear why it increased again at 5 years. EGR2, which is important in macrophage function29, increased within 4 months and increased further at 1 year before decreasing to presurgical levels at 2 years. FPR1, which is important in chemoattraction of macrophages, phagocytosis, and the inflammatory profile of macrophages30, increased within 4 months before decreasing to presurgical levels at 1 year, but it is unclear why there was an increase again at 5 years. IL6, which has pleiotropic functions in both immune and nonimmune cells31, increased within 4 months and was still elevated at 1 year before decreasing to presurgical levels at year two. RGS2, which has a role in vascular contractility32, increased at 4 months and at 1 year before decreasing, but not to presurgical levels, but again it is unclear why there was an increase again at 5 years. SPLG, which is involved in the recruitment of activated lymphocytes33, increased at 1 year and continued to be expressed at 2 and 5 years.
THBS1, which is involved in the inflammatory response with TGF-beta134, increased within 4 months and maintained at that level of expression for up to 5 years. It can be seen that all of these genes are involved in the immune response and/or the inflammatory response, and the results are in accord with other bioinformatic studies on subcutaneous adipose tissue where there is evidence of differential gene expression for immunoregulation and inflammation after bariatric surgery18,19. Speculatively, this suggests that DEGs expression occurs immediately after surgery, but that there is likely an evolution of further DEGs over the first year when weight loss is expected to continue, which may reflect the progressive, beneficial effect of weight loss. Unfortunately, in this data set, the BMIs were not available to answer the questions that arose from this study. For example, are the DEGs reflecting absolute or relative weight loss, the rate of weight loss or the type of bariatric procedure employed. It appeared that the number of DEGs fall after the first year that may be explained by the potential scenario of weight loss of the first year that then plateaus. However, many of the DEGs remain above baseline in the medium and long term and that may suggest this is the new "normal" following surgery. It would be particularly interesting to compare these DEGs prospectively in a cohort following surgery or compared to an overweight and a non-obese weight population to determine if this is gene expression, which was affected by weight gain, has been reversed, or whether the DEGs are still being activated as a response to weight loss surgery. In a systematic review of differentially expressed genes in subcutaneous adipose tissue of lean, obese and post-Roux-en-Y bariatric surgery at distinct time points, the lean state as well as the post- Roux-en-Y were similar in terms of increased gene expression for insulin-sensitization, lipogenesis induction and downregulating inflammation cytokines and markers35, however, it was not clear at what BMI that gene expression normalized.
Investigation of gene ontology process of identified DEGs demonstrated that these genes mostly affect immune function. DEGs in the short-term were mostly involved in interleukin 8-receptor activity and interleukin 8 binding, whilst the DEGs in the medium- and long-term were mostly involved in complement receptor activity and complement binding. Kerr et al. showed the involvement of down-regulated genes after bariatric surgery in immune response processes36. Liu et al. evaluate DEGs after bariatric surgery and found that DEGs play roles in the immune response and neutrophil-mediated immunity19.
Ortega et al. using bioinformatics analysis of microarray datasets found that bariatric surgery led to increased expression of interleukin 6, interleukin 8, tumor necrosis factor α and lipopolysaccharide-binding protein and decreased expression of GLUT4, IRS1, and adiponectin37. Berisha et al. reported DEGs after bariatric surgery in whole blood from eleven obese subjects with type 2 diabetes. Their results showed that 200 DEGs were altered; among them GGT1, CAMP, DEFA1, LCN2, TP53, PDSS1, OLR1, CNTNAP5, DHCR24, HHAT and SARDH that have been implicated in lipid metabolism, obesity and/or type 2 diabetes38. Van der Kolk et al. investigated differential mitochondrial gene expression in adipose tissue after weight loss through bariatric surgery or diet. Their results showed upregulation of the OXPHOS pathway after bariatric surgery39. Nicoletti et al. identified differentially methylated and expressed genes in leukocytes after bariatric surgery. Their results demonstrated differentially methylation in the promoter region and gene body of ZFP36L1 and USP32 after bariatric surgery that affects NIK/NF-kappaB signaling, MAPK cascade, and cellular responses to an insulin stimulus. These genes were enriched in functions of orexigenic, adipogenesis, insulin metabolism pathways and oxidative stress40.
To explain that the gene expression change that occurred was due to weight loss or due to the impact of surgery, DEGs after diet induced weight loss were compared to DEGs after bariatric surgery; however, no similar DEGs were found. Moreover, pathways analysis showed different effect caused by bariatric surgery.
The strength of this study was the identification of the DEGs over the short medium and long term that reflects the clinical information that is well recognized following bariatric surgery. This study is limited by the number of databases that we had access to and the demographic data available. The study does not answer the questions arising on the effect on DEG depending on the type of surgery, or expression of DEG to absolute versus relative weight loss and if the rapidity of weight loss is also important; however, the fold increase in DEG for some of the genes increasing to 1 year would suggest that progressive weight loss over this period may be an important parameter.
In conclusion, this analysis has shown that DEG expression for CCL2, CXCR4, EGR2, FPR1, IL6, RGS2, SELPLG and THBS1 occurs in the short-, medium-, and long-term period following bariatric surgery, which have important functions related to immunity, cancer, cardiovascular diseases and type 2 diabetes, reflecting the clinical improvement seen in patients undergoing successful bariatric surgery.
Data availability
This study used four datasets including GSE199063 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE199063), GSE29411 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE29411), GSE83223 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE83223), and GSE112307(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE112307), with all RNA sequencing data from the Gene Expression Omnibus database (GEO, https://www.ncbi.nlm.nih.gov/geo). All datasets are publicly available datasets. Datasets were preprocessed as indicated and those versions that were used in this study and any additional information and data can be available upon request to Maryam Mahjoubin-Tehran (mmahjoubin@gmail.com). Results are also provided in Supplementary Information.
References
Hong, Y. R., Kelly, A. S., Johnson-Mann, C., Lemas, D. J. & Cardel, M. I. Degree of cardiometabolic risk factor normalization in individuals receiving bariatric surgery: Evidence from NHANES 2015–2018. Diabetes Care 44(3), e57–e58 (2021).
Mentias, A. et al. Long-term cardiovascular outcomes after bariatric surgery in the medicare population. J. Am. Coll. Cardiol. 79(15), 1429–1437 (2022).
Wang, L. et al. Cardiometabolic improvements after metabolic surgery and related presurgery factors. J. Endocr. Soc. 8(5), bvae027 (2024).
Jamialahmadi, T. et al. Effect of bariatric surgery on flow-mediated vasodilation as a measure of endothelial function: A systematic review and meta-analysis. J. Clin. Med. 11(14), 4054 (2022).
Jamialahmadi, T., Banach, M., Almahmeed, W., Kesharwani, P. & Sahebkar, A. Impact of bariatric surgery on circulating PCSK9 levels as a marker of cardiovascular disease risk: A meta-analysis. Arch. Med. Sci. 18(5), 1372–1377 (2022).
Jamialahmadi, T. et al. The effect of bariatric surgery on circulating levels of lipoprotein (a): A meta-analysis. BioMed Res. Int. https://doi.org/10.1155/2022/8435133 (2022).
Jamialahmadi, T. et al. The effect of bariatric surgery on circulating levels of oxidized low-density lipoproteins is apparently independent of changes in body mass index: A systematic review and meta-analysis. Oxid. Med. Cell. Longev. https://doi.org/10.1155/2021/4136071 (2021).
Jamialahmadi, T. et al. Impact of bariatric surgery on pulse wave velocity as a measure of arterial stiffness: A systematic review and meta-analysis. Obes. Surg. 31(10), 4461–4469 (2021).
Nabavi, N. et al. Impact of bariatric surgery on carotid intima-media thickness in patients with morbid obesity: A prospective study and review of the literature. Obes. Surg. 32(5), 1563–1569 (2022).
Adams, T. D. et al. Weight and metabolic outcomes 12 years after gastric bypass. N. Engl. J. Med. 377(12), 1143–1155 (2017).
Sjostrom, L. et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 357(8), 741–752 (2007).
Adams, T. D. et al. Long-term mortality after gastric bypass surgery. N. Engl. J. Med. 357(8), 753–761 (2007).
Ji, Y. et al. Effect of bariatric surgery on metabolic diseases and underlying mechanisms. Biomolecules. 11(11), 1582 (2021).
O’Brien, P. E. et al. Long-term outcomes after bariatric surgery: A systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes. Surg. 29(1), 3–14 (2019).
English, W. J., Spann, M. D., Aher, C. V. & Williams, D. B. Cardiovascular risk reduction following metabolic and bariatric surgery. Ann. Transl. Med. 8(Suppl 1), S12 (2020).
Grenier-Larouche, T., Carreau, A. M. & Carpentier, A. C. Early metabolic improvement after bariatric surgery: The first steps toward remission of type 2 diabetes. Can. J. Diabetes. 41(4), 418–425 (2017).
Tang, W. et al. Microarray analysis identifies lncFirre as a potential regulator of obesity-related acute lung injury. Life Sci. 340, 122459 (2024).
Chen, S. et al. Bioinformatics analysis to obtain critical genes regulated in subcutaneous adipose tissue after bariatric surgery. Adipocyte. 11(1), 550–561 (2022).
Liu, Y. et al. Integrative analyses of biomarkers and pathways for adipose tissue after bariatric surgery. Adipocyte. 9(1), 384–400 (2020).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51(D1), D587–D592 (2023).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 28(11), 1947–1951 (2019).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28(1), 27–30 (2000).
Affinati, A. H., Esfandiari, N. H., Oral, E. A. & Kraftson, A. T. Bariatric surgery in the treatment of type 2 diabetes. Curr. Diab. Rep. 19(12), 156 (2019).
Aminian, A. et al. Association of bariatric surgery with major adverse liver and cardiovascular outcomes in patients with biopsy-proven nonalcoholic steatohepatitis. JAMA. 326(20), 2031–2042 (2021).
Aminian, A. et al. Association of bariatric surgery with cancer risk and mortality in adults with obesity. JAMA. 327(24), 2423–2433 (2022).
Haghighat, N. et al. How does fat mass change in the first year after bariatric surgery? A systemic review and meta-analysis. Obes. Surg. 31(8), 3799–3821 (2021).
Singh, S., Anshita, D. & Ravichandiran, V. MCP-1: Function, regulation, and involvement in disease. Int. Immunopharmacol. 101(Pt B), 107598 (2021).
Kim, M. Y. CXCR4 to improve both T cell homing and function. Blood. 141(21), 2546–2547 (2023).
McCowan, J. et al. The transcription factor EGR2 is indispensable for tissue-specific imprinting of alveolar macrophages in health and tissue repair. Sci. Immunol. 6(65), eabj2132 (2021).
Zhu, S., Hu, X., Bennett, S., Mai, Y. & Xu, J. Molecular Structure, expression and role of TAFA4 and its receptor FPR1 in the spinal cord. Front. Cell Dev. Biol. 10, 911414 (2022).
Murakami, M., Kamimura, D. & Hirano, T. Pleiotropy and specificity: Insights from the interleukin 6 family of cytokines. Immunity. 50(4), 812–831 (2019).
Phan, H. T. N., Jackson, W. F., Shaw, V. S., Watts, S. W. & Neubig, R. R. Loss-of-function mutations in human regulator of G protein signaling RGS2 differentially regulate pharmacological reactivity of resistance vasculature. Mol. Pharmacol. 96(6), 826–834 (2019).
Fenoglio, C. et al. SELPLG and SELP single-nucleotide polymorphisms in multiple sclerosis. Neurosci. Lett. 394(2), 92–96 (2006).
Mo, L. et al. Integrated bioinformatic analysis of the shared molecular mechanisms between osteoporosis and atherosclerosis. Front. Endocrinol. 13, 950030 (2022).
Cruz-García, E. M., Frigolet, M. E., Canizales-Quinteros, S. & Gutiérrez-Aguilar, R. Differential gene expression of subcutaneous adipose tissue among lean, obese, and after RYGB (different timepoints): Systematic review and analysis. Nutrients. 14(22), 4925 (2022).
Kerr, A. G., Andersson, D. P., Rydén, M., Arner, P. & Dahlman, I. Long-term changes in adipose tissue gene expression following bariatric surgery. J. Intern. Med. 288(2), 219–233 (2020).
Ortega, F. J. et al. Bariatric surgery acutely changes the expression of inflammatory and lipogenic genes in obese adipose tissue. Surg. Obes. Relat. Dis. 12(2), 357–362 (2016).
Berisha, S. Z., Serre, D., Schauer, P., Kashyap, S. R. & Smith, J. D. Changes in whole blood gene expression in obese subjects with type 2 diabetes following bariatric surgery: A pilot study. PLoS ONE. 6(3), e16729 (2011).
van der Kolk, B. W. et al. Differential mitochondrial gene expression in adipose tissue following weight loss induced by diet or bariatric surgery. J. Clin. Endocrinol. Metab. 106(5), 1312–1324 (2021).
Nicoletti, C. F. et al. Altered pathways in methylome and transcriptome longitudinal analysis of normal weight and bariatric surgery women. Sci. Rep. 10(1), 6515 (2020).
Author information
Authors and Affiliations
Contributions
Conceptualization: AS writing-original draft: MMT Investigation: MMT, SLA, TJ, MK, AHE, WA, AS writing—review and editing: SLA, TJ, MK, AHE, WA, AS approval of the final version: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mahjoubin-Tehran, M., Atkin, S.L., Jamialahmadi, T. et al. The differential expression of adipose tissue genes in short, medium and long-term periods after bariatric surgery. Sci Rep 14, 19991 (2024). https://doi.org/10.1038/s41598-024-70629-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70629-7