Abstract
It has been reported that a scenario-based cognitive behavioral therapy mobile app including Todac Todac was effective in improving depression in the general public. However, no study has been conducted on whether Todac Todac is effective in dialysis patients. Therefore, this study was intended to determine whether the use of this app was effective in improving depression in dialysis patients. Sixty-five end-stage kidney disease patients receiving dialysis at Soonchunhyang University Cheonan Hospital were randomly assigned to the Todac Todac app program (experimental group) or an E-moods daily mood chart app program (control group) for 3 weeks. The degree of depression was measured before and after using the app.After the end of the 3-week program, a small but significant improvement was observed in the Trait anxiety (p < 0.05) and Beck depression index (p < 0.05) in E-moods group and DAS-K scores (p < 0.05) in Todac Todac group. However, no differences were seen in any parameters between the two groups. In addition, Todac Todac was not statistically more effective than the control intervention in the subgroup analysis. The Todac Todac, a scenario-based cognitive behavioral therapy mobile app, seemed to have a limited effect on improving depression in dialysis patients. Therefore, it is necessary to develop new tools to improve depression in dialysis patients.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is irreversible damage to kidney structure or function that persists for over 3 months, primarily caused by hypertension, diabetes, glomerulonephritis, etc.1,2. Patients with end-stage kidney disease (ESKD), the final stage of CKD, require kidney replacement therapies such as hemodialysis, peritoneal dialysis, or kidney transplantation to survive. Patients with CKD are significantly affected not only in terms of physical health but also mental health, exhibiting a relatively high risk of depression compared to the general population3,4.
During the coronavirus disease-2019 (COVID-19) pandemic recently, psychological distress and symptoms of mental illness were significant issues worldwide, even in the general public without psychiatric problems5,6,7. COVID-19-related psychological distress is caused not only by concerns about infection but also by large-scale isolation and overall socioeconomic problems8. Previous studies revealed the psychological impact of the COVID-19 pandemic on anxiety, depressive symptoms, and sleep quality9.
CKD patients were particularly affected by these mental health issues during the pandemic, highlighting the importance of managing mental health for them. Our previous studies, conducted on CKD patients with non-dialysis kidney diseases and those undergoing dialysis, revealed that they experienced COVID-19-related psychological disorders such as depression, anxiety, stress, and insomnia10,11. The frequency of anxiety and insomnia increased with the progression of CKD stages. Additionally, we observed that the severity of psychological distress varied depending on the dialysis modality among dialysis patients, which may be attributed to cognitive biases and differences in precautionary measures depending on the dialysis modality.
Numerous studies have been conducted to identify factors related to depression in CKD patients, such as urea levels, gut microbiota, and exercise, as well as to evaluate the efficacy and safety of antidepressants12,13,14,15. However, there are still few established treatments and little interest in caring for these patients. Recently, few studies have reported that emerging mobile app-based cognitive-behavioral therapy was effective in improving several depression scale scores and improving insomnia in the general population16,17,18. A recent study reported that a digital therapeutic app called Todac Todac was clinically effective in patients diagnosed with other specified depressive disorders18.
Even though efforts to apply cognitive-behavioral therapy have been made to manage depression in ESKD patients, forms of treatment vary, and currently there are lack of established protocols19,20. Therefore, this study was conducted to confirm whether mobile app-based cognitive-behavioral therapy, which was effective in general populations in recent studies, would be effective in dialysis patients. Our study hypothesized that the application of Todac Todac could reduce depressive symptoms in ESKD patients, particularly during the COVID-19 pandemic.
Results
Baseline characteristics of the participants
The baseline characteristics of the study participants are presented in Table 1. Initially, 80 participants were selected as participants; however, 14 declined during the consent explanation, and 1 withdrew consent during the experiment, leaving a total of 65 participants (Fig. 1). Among them, 40 completed the full 3-week treatment (E-mood: 20, Todac Todac: 20). 11 participants missed 1–3 days (E-mood: 5, Todac Todac: 6), 5 participants missed 4–7 days (E-mood: 4, Todac Todac: 1), and 9 participants completed less than 10 days of the treatment (E-mood: 3, Todac Todac: 6).
Study participant enrollment flow chart : The study population was selected from patients who had been receiving hemodialysis or peritoneal dialysis stably for more than 3 months at Soonchunhyang University Hospital Cheonan and was limited to those aged between 20 years and 65 years. Patients with a history of physical and mental hospitalization within 1 month and diagnosed with major psychological disorders were excluded. Patients expected to have difficulty using mobile apps were also excluded. Finally, a total of 65 dialysis patients who visited Soonchunhyang University Cheonan Hospital from January 14, 2021, to June 1, 2021, were included in the study. aDAS-K : dysfunctional attitude scale.
The mean age of all participants was 48.3 ± 9.91 years, and the male proportion was 61.5%. The number of patients receiving peritoneal dialysis was 40 (61.5%), and others received hemodialysis (38.5%). In addition to the characteristics, including mean age, biochemical parameters were randomly divided, and there was no statistical significance between the 2 groups except for calcium levels.
Psychological measurements
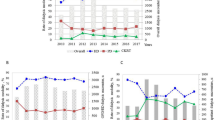
E-moods and Todac Todac therapy were conducted for 3 weeks in 2 randomly divided groups of 65 people. Figure 2 depicts a comparison of the scores of all patients. After implementing 3-week E-mood and Todac Todac programs, significant decreases were observed in the Beck depression index (Fig. 2C, p < 0.05) and Dysfunctional Attitude Scales-Korean version (DAS-K) scores (Fig. 2D, p < 0.01) in the overall patient group, but no significant differences were found in state anxiety (Fig. 2A, p > 0.05) and trait anxiety scores (Fig. 2B, p > 0.05) between the 2 groups. Table 2 shows the baseline psychological scale scores of the patients according to treatment modality. No statistically significant differences were seen between the 2 groups.
Comparison of scores of all patients. (a) State anxiety, (b) trait anxiety, (c) Beck depressive inventory, and (d) DAS-K. : After implementing 3-week E-mood and Todac Todac programs, significant decreases were observed in the Beck depression index (C) and DAS-K scores (D) in the overall patient group, but no significant differences were found in state anxiety (A) and trait anxiety scores (B) between the 2 groups. aDAS-K : dysfunctional attitude scale.
After the experiment, both trait anxiety and Beck depression index scores showed relevant improvements in the E-moods group (Table 3; Fig. 3, p < 0.05), and a relevant improvement was confirmed only in DAS-K scores in Todac Todac group (Table 3; Fig. 3, p < 0.05). However, there was no significant difference in the comparison of P-value (Δ(Pre-Post)) between the two groups in any parameters (State anxiety, Trait anxiety, Beck depressive index, DAS-K) (Table 3, p > 0.05).
Additionally, subgroup analysis was conducted for additional evaluation, and differences (Δ (pre-post)) between E-moods and Todac Todac were compared based on an age of 50, Diabetes Mellitus (DM) or non-DM, and peritoneal dialysis or hemodialysis (Fig. 4). In patients without diabetes, Todac Todac showed a higher average treatment effect than E-moods in 3 out of 4 parameters (State anxiety, Beck depressive index, DAS-K). However, in patients with diabetes, E-moods exhibited a greater average treatment effect across all 4 parameters. Among these, the difference in treatment effects between E-moods and Todac Todac for state anxiety was significant depending on the presence of diabetes (p < 0.05).
Comparison of results between the E-mood and Todac Todac groups : In the E-moods group, both trait anxiety and Beck depression index scores showed relevant improvements, and in Todac Todac group, a relevant improvement was confirmed only in DAS-K scores. However, there was no significant difference in the comparison of P-value (Δ(Pre-Post)) between the two groups in any parameters. aDAS-K : dysfunctional attitude scale.
Discussion
As modern society becomes more complex, the incidence of depression continues to increase worldwide, and digital therapeutics are being designed to improve depression without meeting with a psychiatrist in person21. Todac Todac, a scenario-based cognitive behavioral therapy mobile app developed by the Korean National Mental Health Center in 2017, helps to organize depression and anxiety by having the user read scenarios about day-to-day experiences. It can also be used to advise or share similar experiences with others to improve user compliance with treatment.
In the present study, dialysis patients with depression and anxiety were divided into the E-moods group and the Todac Todac group, and various psychological measurement parameters were compared. Mobile-app-based cognitive-behavioral therapy showed improvement in some indices in the overall group. There were significant decreases in depressive symptoms and dysfunctional beliefs in the entire patient cohort over the study period. It suggests that daily mood evaluation and cognitive interventions might be helpful to patients with CKD, especially during the pandemic periods when this study was performed.
Todac Todac was developed to correct distorted negative cognition in people with depression and was not specifically designed for the psychological stress of CKD patients. Since then, only the decrease in DAS-K scores was statistically significant in the Todac Todac group, even though the average of all 4 parameters decreased. A previous randomized controlled trial with patients with depression reported that Dysfunctional Attitude Scale scores in the Todac Todac group were lower than in the control group after completing a 3-week program18. Although Hur’s study reported that an improvement in anxiety was evident in both groups, a group difference was found in BDI-II scores at the trend level. Only DAS-K scores were statistically significant in a previous study in a purely depressed population. Therefore, it is possible that the intervention was more effective in reducing dysfunctional beliefs by correcting distorted cognition than it was in correcting anxiety.
No significant difference in pre- and post-intervention effects in various psychological variables was seen in the 2 groups. The scenario-based cognitive behavioral therapy mobile app (Todac Todac), which was proven effective in previous studies, was not significantly effective compared to the control group in this study. The reasons can be considered as follows.
First, there is a possibility that the mobile app-based intervention may not have sufficiently motivated patients with chronic diseases. Better results might have been seen if face-to-face cognitive behavioral therapy had been implemented. Second, cognitive behavioral therapy based on cognitive intervention may have been less effective than in the normal group because patients with chronic diseases may have factors such as declines in cognitive function. Third, because this was not a specialized intervention program for CKD patients, it was likely to be less effective in improving distress. Lastly, since the depressive symptom scores of the patients in our study were within the mild range, participants might have recovered over time without any specific intervention, which could explain why there was no significant difference in the Todac Todac group compared to the E-mood group22.
This study may have a limitation due to the small sample size. Also, the degree of depression in the general depression group and the dialysis patients with depression may have been different. Thus, there is a possibility that the effect may be minimal in patients with severe comorbidities, such as ESKD. Additionally, since the app developed in Korea was applied only to Koreans, effectiveness may vary depending on cultural differences.
In conclusion, although the scenario-based cognitive behavioral therapy mobile app did not have a significant effect, the mental health management of dialysis patients can be seen as important in the current medical environment, including non-face-to-face care, which is increasing due to COVID-19. Therefore, it is necessary to develop alternative therapies for better treatment.
Subgroup analysis of various parameters (age > 50 or < 50, DM or non-DM, peritoneal dialysis or hemodialysis): As previously explained, we did not observe any statistically significant differences between the general E-moods and Todac Todac groups. Therefore, we conducted subgroup analysis based on various variables that we initially examined at the start of the trial, such as age, presence of diabetes mellitus, and type of dialysis (peritoneal dialysis or hemodialysis). However, as shown, we also did not find any significant statistical differences in these subgroup analysis. aPD : peritoneal dialysis; bHD : hemodialysis; cDAS-K: dysfunctional attitude scale.
Materials and methods
Study population
Figure 1 depicts the study design and a flowchart of the study participants. The Institutional Review Board and Ethics Committee of Soonchunhyang University Hospital Cheonan approved the study (IRB number: 2022-11-022). All methods were carried out in this study by regulations of the Institutional Review Board and Ethics Committee of Soonchunhyang University Hospital Cheonan. All patients provided written informed consent before enrollment. The study population was selected from patients receiving hemodialysis or peritoneal dialysis stably for more than 3 months at Soonchunhyang University Hospital Cheonan and was limited to those aged between 20 years and 65 years. Patients with a history of physical and mental hospitalization within 1 month and diagnosed with major psychological disorders (major depressive disorder, bipolar disorder, Alzheimer’s disease, etc.) were excluded. Patients expected to have difficulty using mobile apps were also excluded, specifically participants with severe cognitive impairment or unfamiliar with smartphones, who were unable to install and use the mobile app despite receiving 2–3 explanations. Finally, a total of 65 dialysis patients who visited Soonchunhyang University Cheonan Hospital from January 14, 2021, to June 1, 2021, were included in the study.
Clinical data collection
The characteristics of patients such as age, sex, body mass index (BMI), presence of diabetes or hypertension, and dialysis modalities (PD or HD) were collected from medical records. Additionally, hemoglobin, hematocrit, creatinine, phosphorus, calcium, potassium, and intact parathyroid hormone (PTH) levels were measured through blood and endocrine tests. Furthermore, dialysis adequacy, as indicated by kt/V, was assessed. These data were collected during the study period.
Mobile app-based cognitive behavioral therapy
The patients were randomly divided into two groups: patients using E-moods and those using Todac Todac. Todac Todac is a scenario-based cognitive behavioral therapy mobile app designed to reduce dysfunctional beliefs in individuals with depression. The app guides users through identifying cognitive distortions in various scenarios, such as an employee sensitive to evaluations or a young man worried about job failure. It includes steps for de-catastrophizing unrealistic concerns and offering advice to friends or family members in similar situations. Through these exercises, users learn to recognize and challenge their negative thoughts and beliefs. The experimental group performed cognitive-behavioral therapy using the mobile app (Todac Todac, National Mental Health Center) for more than 10 min every day, and the control group recorded their mood every day.
Survey development
Before and after 3 weeks of mobile app-based cognitive behavioral therapy, multiple self-report questionnaires were completed to investigate psychiatric symptoms23. This included the State-Trait Anxiety Inventory (STAI), the DAS-K, and the Beck Depression Inventory-II (BDI-II)24,25.
STAI, a widely used psychological inventory for measuring anxiety in adults, distinguishes between two types of anxiety: state anxiety (a temporary condition experienced in specific situations) and trait anxiety (a general tendency to respond with anxiety in various situations). Respondents rate items such as “I feel calm” or “I feel nervous and restless” on a 4-point scale ranging from “Almost Never” to “Almost Always”, with scores summed to provide an overall measure of anxiety. Regarding the reliability of the STIA, Cronbach’s alpha values are reported to assess the internal consistency of the inventory. In addition, DAS-K assessed the depression, anxiety, and stress levels, and BDI-II evaluated the degree of depression.
Each questionnaire was scored, and the severity was divided into normal, mild, moderate, and severe according to each score. Total scores of measurement tools were interpreted as follows: State-Trait Anxiety, normal (20–37), mild (38–44), moderate (45–52), and severe (53–80); DAS-K, normal (0–9), mild (10–13), moderate (14–20), severe (21–27) and extremely severe (28 − 24) depression; normal (0–7), mild (8–9), moderate (10–14), severe (15–19) and extremely severe (20–42) anxiety; normal (0–14), mild (15–18), moderate (19–25), severe (26–33) and extremely severe (34–42) stress; BDI-II, normal (0–13), mild (14–19), moderate (20–28), and severe (29–63) depression. Participants were asked to fill in the missing items if the completion rate was low upon submission, with additional explanations. Therefore, the questionnaires were nearly all completed.
Statistical analysis
Statistical analyses were performed using R version 4.1.1 (The R Foundation for Statistical Computing, Vienna, Austria). Categorical variables are expressed as counts (percentage), normally distributed continuous variables as means ± standard deviation (SD), and non-normally distributed continuous variables as medians (interquartile ranges). Differences between 2 independent groups (E-moods and Todac Todac) were analyzed by unpaired t-tests for normally distributed continuous variables and by the Mann-Whitney U test for non-normally distributed continuous variables. Paired samples t-tests were used to analyze the score changes between pre-treatment and post-treatment for normally distributed continuous variables. Categorical variables were analyzed using Pearson’s Chi-squared test or Fisher’s exact test, as appropriate. In subgroup analyses, p-values were calculated by linear regression using interaction terms between subgroup variables and test modalities. P-values of < 0.05 were regarded as statistically significant, and two-tailed tests were performed for all hypothesis tests.
Data availability
The datasets used and/or analyzed during the current survey available from the corresponding author on reasonable request.
References
Kim, K. M., Lee, S., Shin, J. H. & Park, M. A comparative study of epidemiological characteristics, treatment outcomes, and mortality among patients undergoing hemodialysis by health insurance types: Data from the korean renal data system. Kidney Res. Clin. Pract. (2023).
Kalantar-Zadeh, K., Jafar, T. H., Nitsch, D., Neuen, B. L. & Perkovic, V. Chronic kidney disease. Lancet 398, 786–802 (2021).
Palmer, S. et al. Prevalence of depression in chronic kidney disease: Systematic review and meta-analysis of observational studies. Kidney Int. 84, 179–191 (2013).
Jeon, Y. H. et al. The impact of severe depression on the survival of older patients with end-stage kidney disease. Kidney Res. Clin. Pract. (2023).
Bao, Y., Sun, Y., Meng, S., Shi, J. & Lu, L. 2019-nCoV Epidemic: Address Mental Health care to Empower Society. Lancet 395, e37–e38 (2020).
Santomauro, D. F. et al. Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 due to the COVID-19 Pandemic. Lancet 398, 1700–1712 (2021).
Hao, F. et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain. Behav. Immun. 87, 100–106 (2020).
Hossain, M. M. et al. Epidemiology of mental health problems in COVID-19: A review. F1000Research 9 (2020).
Huang, Y. & Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 288, 112954 (2020).
Yu, J. Y. et al. Psychological distress of patients with end-stage kidney disease undergoing dialysis during the 2019 coronavirus disease pandemic: A cross-sectional study in a university hospital. PLoS ONE 16, e0260929 (2021).
Lee, K. M. et al. The higher the CKD stage, the higher the psychological stress in patients with CKD during COVID-19 pandemic. J. Clin. Med. 11, 4776 (2022).
Levassort, H. et al. Urea level and depression in patients with chronic kidney disease. Toxins 16, 326 (2024).
Li, Q. et al. Gut microbiota profiling reflects the renal dysfunction and psychological distress in patients with diabetic kidney disease. Front. Endocrinol. 15, 1410295 (2024).
Nagler, E. V., Webster, A. C., Vanholder, R. & Zoccali, C. Antidepressants for depression in stage 3–5 chronic kidney disease: A systematic review of pharmacokinetics, efficacy and safety with recommendations by European renal best practice (ERBP). Nephrol. Dialysis Transpl. 27, 3736–3745 (2012).
Takamatsu, K. et al. Physical and psychological effects of a long-term supervised self-exercise program during hemodialysis in elderly dialysis patients: A single-site pilot study in a Japanese community setting. Medicine 103, e38963 (2024).
Sharma, G. et al. Brief app-based cognitive behavioral therapy for anxiety symptoms in psychiatric inpatients: Feasibility randomized controlled trial. JMIR Form. Res. 6, e38460 (2022).
Horsch, C. H. et al. Mobile phone-delivered cognitive behavioral therapy for insomnia: A randomized waitlist controlled trial. J. Med. Internet. Res. 19, e70 (2017).
Hur, J. W., Kim, B., Park, D. & Choi, S. W. A scenario-based cognitive behavioral therapy mobile app to reduce dysfunctional beliefs in individuals with depression: A randomized controlled trial. Telemed. e-Health 24, 710–716 (2018).
Zegarow, P., Manczak, M., Rysz, J. & Olszewski, R. The influence of cognitive-behavioral therapy on depression in dialysis patients–meta-analysis. Arch. Med. Sci. 15, (2020).
Jhamb, M. et al. Effects of technology assisted stepped collaborative care intervention to improve symptoms in patients undergoing hemodialysis: The TĀCcare randomized clinical trial. JAMA Intern. Med. 183, 795–805 (2023).
Liu, Q. et al. Changes in the global burden of depression from 1990 to 2017: Findings from the global burden of disease study. J. Psychiatr. Res. 126, 134–140 (2020).
Stegenga, B. T., Kamphuis, M. H., King, M., Nazareth, I. & Geerlings, M. I. The natural course and outcome of major depressive disorder in primary care: The PREDICT-NL study. Soc. Psychiatry Psychiatr. Epidemiol. 47, 87–95 (2012).
Wang, C. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17, 1729 (2020).
Fountoulakis, K. N. et al. Reliability and psychometric properties of the greek translation of the state-trait anxiety inventory form Y: Preliminary data. Ann. Gen. Psychiatry 5, 1–10 (2006).
Lovibond, P. F. & Lovibond, S. H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 33, 335–343 (1995).
Funding
This study was supported by Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Contributions
In line with CRediT Author Statement: D.S.K.: Investigation; Writing - Original Draft; Writing - Review & Editing; Visulization; H.S.S.: Investigation; K.M.L.: Investigation; J.G.L.: Writing - Review & Editing; Visulization; S.Y.: Investigation; J.L.: Formal analysis; Data Curation; N.H.H.: Formal analysis; Data Curation; J.S.K.: Supervision; Writing - Review & Editing; N.J.C.: Formal analysis; Investigation; Visualization; Supervision; S.P.: Supervision; H.W.G.: Supervision; E.Y.L.: Conceptualization; Methodology; Writing - Original Draft; Writing - Review & Editing; Supervision; Project administration; Funding Acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, DS., Song, H.S., Lee, KM. et al. The effect of a scenario-based cognitive behavioral therapy mobile app on end-stage kidney disease patients on dialysis. Sci Rep 14, 20339 (2024). https://doi.org/10.1038/s41598-024-70986-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70986-3