Abstract
Acute kidney injury (AKI) is related to adverse clinical outcomes. Therefore, identifying patients at increased risk of postoperative AKI and proactively providing appropriate care is crucial. However, only a limited number of modifiable risk factors have been recognized to mitigate AKI risk. We retrospectively analyzed adult patients who underwent endotracheal intubation and mechanical ventilation of more than 2 h during non-cardiac surgery at Seoul National University Hospital from January 2011 to November 2022. Patients were grouped into low- or high-tidal volume groups based on their intraoperative tidal volume relative to their predicted body weight (PBW) of 8 ml/kg. The association between intraoperative tidal volume and postoperative AKI was evaluated using inverse probability of treatment weighting (IPTW), adjusting for various preoperative confounders. Among the 37,726 patients included, the incidence of postoperative AKI was 4.1%. The odds of postoperative AKI risk were significantly higher in the high-tidal volume group than in the low-tidal volume group before and after IPTW (odds ratio [OR] 1.20, 95% confidence interval [CI] 1.08–1.32, P = 0.001 and OR: 1.10, 95% CI 1.02–1.19, P = 0.010, respectively). In the multivariable logistic regression analysis after IPTW, a high tidal volume was independently associated with an increased risk of postoperative AKI (OR: 1.21, 95% CI 1.12–1.30, P < 0.001). In this propensity score-weighted analysis, an intraoperative high tidal volume of more than 8 ml/kg PBW was significantly associated with an increased risk of postoperative AKI after IPTW in non-cardiac surgical patients. Intraoperative tidal volume showed potential as a modifiable risk factor for preventing postoperative AKI.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a frequently encountered complication after surgery, occurring in up to 40% of high-risk patients1,2. Postoperative AKI is associated with poor clinical outcomes and higher hospital costs3,4,5, and even any stage of postoperative AKI is associated with a longer length of hospital stay and higher in-hospital and 1-year mortalities6. Therefore, identifying patients at increased risk of postoperative AKI and proactively providing appropriate care is crucial. However, despite extensive research on various risk factors, few modifiable risk factors for postoperative AKI have been identified7.
In surgical patients, the lung-protective ventilation strategy is essential for intraoperative ventilation8, and the tidal volume delivered to the patients is a critical element of this strategy9. A tidal volume of 6–8 ml/kg predicted body weight (PBW) is recommended at the initial setting of mechanical ventilation for surgical patients10. However, positive pressure ventilation can cause systemic inflammation and reduction in renal blood flow due to various mechanisms, such as the neurohormonal or hemodynamic response and pulmonary inflammatory reactions11,12,13,14. Mechanical ventilation was found to be an independent risk factor for AKI in critically ill patients15,16. However, prior investigations regarding the association between intraoperative tidal volume and postoperative AKI showed conflicting results17,18,19,20,21. Therefore, this association remains inconclusive.
The present study investigated the relationship between intraoperative tidal volume and postoperative AKI in patients undergoing non-cardiac surgery under general anesthesia. We hypothesized that a higher intraoperative tidal volume would be associated with an increased risk of postoperative AKI.
Results
Of the 60,326 initially eligible patients, 22,600 patients were excluded; thus, 37,726 patients were included in the final analysis (Fig. 1). Among them, 19,001 patients received low-tidal volume ventilation based on the optimal threshold of 8 ml/kg PBW, whereas 18,725 received high-tidal volume ventilation. Table 1 compares demographic and preoperative perioperative variables between the low- and high-tidal volume groups. All variables in Table 1 were balanced, with an SMD less than 0.1 (Supplementary Figure S1).
The total cohort's median deviation tidal volume was 8.0 (7.3–8.8) ml/kg PBW. The low-tidal volume group had a mean tidal volume of 7.3 (6.8–7.7) ml/kg PBW, whereas the high-tidal volume group had a mean tidal volume of 8.8 (8.4–9.5) ml/kg PBW. There were significant differences in mean tidal volume between patients with postoperative AKI and those without (452.4 [IQR 401.6–506.5] vs. 472.6 [416.2–523.7] ml, median difference 20.22 [95% CI 13.95 to 26.11], P < 0.001). The distribution of the average tidal volume and the incidence of postoperative AKI are depicted in Fig. 2. Tidal volume showed a decreasing trend over the years, with a more pronounced decline observed after 2014 (Supplementary Figure S2).
Postoperative AKI occurred in 1534 patients (4.1%), with 1230 (3.3%) cases of mild AKI and 304 (0.8%) cases of moderate-to-severe AKI. Significant differences were observed in the length of postoperative hospital stays between patients with postoperative AKI and those without (10.0 [7.0–18.0] days vs. 7.0 [5.0–10.0] days, P < 0.001). Postoperative AKI occurred in 707 patients (3.7%) and 827 patients (4.4%) in the low- and high-tidal volume groups, respectively. The risk of postoperative AKI was significantly higher in the high-tidal volume group before and after IPTW (OR, 1.20 95% CI 1.08–1.32, P = 0.001 and OR: 1.10, 95% CI 1.02–1.19, P = 0.010, respectively, Table 2).
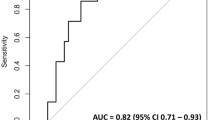
In the multivariable binary logistic regression analysis, high-tidal volume was an independent risk factor for postoperative AKI (OR: 1.21, 95% CI 1.12–1.30, P < 0.001, Table 3). Other significant risk factors included male sex, higher body mass index, comorbidities of hypertension and diabetes mellitus, history of chronic kidney disease, emergency surgery, earlier year of surgery, department of surgery, use of preoperative nephrotoxic agents, lower preoperative hemoglobin and albumin level, higher preoperative white blood cell count and serum creatinine. Intraoperative factors such as transfusion, longer duration of surgery, balanced anesthesia (as opposed to total intravenous anesthesia), and higher time-weighted averages of mean blood pressure below 65 mmHg. In the restrictive cubic spline regression model, the risk of postoperative AKI linearly increased with the increase in tidal volume (Fig. 3).
We conducted propensity score matching as an additional analysis, and the results regarding differences in variables between patients receiving low- and high-tidal volumes before and after 1:1 propensity score matching are presented in Supplementary Table S1. High tidal volume remained significantly associated with an increased risk of postoperative AKI after propensity score matching (OR: 1.17, 95% CI 1.03–1.33, P = 0.017; Supplementary Table S2). Multivariable regression and restricted cubic spline analyses after propensity score matching yielded similar results to those obtained after IPTW (Supplementary Table S3 and Supplementary Figure S3). Across all three statistical methods, high tidal volume consistently showed a significant association with increased AKI risk (Supplementary Figure S4).
In the subgroup analysis based on the type of surgery, the association between high tidal volume and postoperative AKI remained significant in both subgroups (gynecological/urologic surgery: OR 1.56, 95% CI 1.30–1.87, P < 0.001; non-gynecological/urologic surgery: OR 1.19, 95% CI 1.09–1.30, P < 0.001). In the subgroup analysis by sex, the results revealed that high tidal volume was associated with a significantly increased risk of postoperative AKI in male patients (OR 1.24, 95% CI 1.13–1.36, P < 0.001). However, this association was not statistically significant in female patients (OR 1.11, 95% CI 0.96–1.28, P = 0.166). Although the effects of acid–base status variables, minute ventilation, and positive end-expiratory pressure on the relationship between intraoperative tidal volume and postoperative AKI was significant, the difference was not clinically meaningful (Supplementary Table S4).
Discussion
Although AKI is associated with a longer hospital stay and higher mortality, few modifiable risk factors for AKI have been identified. Our study found a significant association between a higher intraoperative tidal volume and postoperative AKI, even after adjusting for various preoperative confounders using IPTW, in patients undergoing non-cardiac surgery. This association remained consistent in the propensity score matching analysis.
Prior research on intraoperative tidal volume and postoperative AKI has yielded conflicting results18,19,20,21,22. Some studies have only included patients who underwent cardiovascular or cardiac surgery, thus limiting the finding’s generalizability to other populations19,21. In a randomized controlled trial comparing tidal volumes among patients who underwent major surgery, those with a higher tidal volume showed a higher incidence of postoperative AKI, although statistical significance was not reached18. Another retrospective study on non-cardiac surgical patients reported a positive association between high tidal volume and postoperative AKI using multivariable logistic regression analysis20. However, our study varies in methodology, as IPTW was used to adjust for various preoperative clinical and laboratory data. A recent randomized controlled study reported no difference in the incidence of postoperative AKI between low- and high-tidal volume ventilation22. However, in this study, the duration of mechanical ventilation was shorter, averaging approximately a median of 150 min in each group, than those in our study (median, 250 min) and other studies (> 200 min) that reported a positive relationship between tidal volume and postoperative AKI19,20. Additionally, most surgeries were low-risk ones.
Postoperative AKI is a well-known complication that can negatively affect postoperative morbidity and mortality3,5. Various risk factors have been reported7,23,24,25,26,27. The identified risk factors for postoperative AKI in our study aligned with previous findings3,7,19,20,24. Unfortunately, most of them are unmodifiable. Although some risk factors, such as preoperative laboratory test results of albumin, hemoglobin, and glucose, may be somewhat modifiable28, it is important to recognize that they may not be readily modifiable. In contrast, intraoperative tidal volume is a risk factor that can be modified during surgery and presents an opportunity for further investigation in future clinical trials to evaluate its effects on postoperative AKI.
Several explanations regarding the relationship between intraoperative tidal volume and postoperative AKI have been suggested. Positive pressure ventilation can decrease cardiac output, alter neurohormonal systems, cause hemodynamic impairment, and lead to the redistribution of intrarenal blood flow, resulting in reduced renal perfusion and blood flow11,12,13. Additionally, mechanical ventilation can induce an inflammatory response14. Mechanical ventilation-induced lung inflammation can lead to systemic inflammation, which may affect the development of AKI29, as evidenced in previous animal studies30,31. However, the exact mechanisms underlying the complex interplay between the lung and kidney remain elusive32. Thus, future research is necessary to elucidate these mechanisms.
Propensity score analysis offers an advantage over conventional regression analysis by integrating many variables to achieve similar distributions of measured covariates between exposed and unexposed patients33. However, it is crucial to acknowledge that residual confounding factors may still exist, as only measured variables can be accounted for. Moreover, in cases where the sample size is large, there can be a limited overlap in the distribution of propensity scores, potentially resulting in poor performance in propensity score matching34. Therefore, the application of propensity score analysis should be approached with caution, depending on the dataset’s characteristics35.
The strength of the present study lies in its inclusion of a wide range of non-cardiac surgeries, avoiding the limitation of confining the analysis to specific types of surgeries (e.g., cardiovascular or cardiac surgery). This approach significantly enhances the generalizability of our findings to the broader population. Additionally, our study had a large sample size, and we included only patients with complete data, contributing to the improved statistical power and robustness of the findings. We intentionally excluded intraoperative variables because covariates that were determined post-anesthesia at the point of group assignment may be inappropriate for the propensity score calculation36. This may have been helpful in reducing selection bias.
However, this study has some limitations. First, the causal relationship between intraoperative tidal volume and AKI incidence cannot be confirmed due to the study’s retrospective nature. While we adjusted for various potential preoperative confounders using IPTW, unmeasured or unknown confounding factors may have affected our analysis. To assess this impact, we calculated the E-value. The E-value for the observed OR was 1.43 and 1.31 for the lower bound, suggesting that unmeasured confounders are unlikely to fully explain the link between high tidal volume and postoperative AKI. Second, we could not fully account for the potential impact of individual anesthesiologist practices on tidal volume selection and AKI risk. Although our additional multilevel analysis using the operating room section as a proxy showed that high tidal volume remained significantly associated with increased AKI risk, residual confounding from anesthetic practices may still exist. Third, while we found significant differences in intraoperative acid–base parameters between low- and high-tidal volume groups, these differences were not clinically significant, and their impact on AKI risk could not be fully elucidated. Lastly, since the study included patients over approximately ten years of surgery, changes in perioperative management surgical techniques over time may have introduced potential confounders, even though the surgery year was considered in the propensity score calculation.
In summary, this propensity score-weighted analysis found that higher intraoperative tidal volume is significantly associated with an increased risk of postoperative AKI after IPTW and PSM in patients undergoing non-cardiac surgery. Although the differences observed between the low- and high-tidal volume groups were small, intraoperative tidal volume showed potential as a modifiable risk factor for preventing postoperative AKI.
Methods
Ethics
Ethical approval was provided by the Institutional Review Board of Seoul National University Hospital (Seoul, Korea; approval number: 2301-047-1393; Chairperson Prof. Young Tae Kim) on 6 February 2023. This study was conducted according to the tenets of the Declaration of Helsinki. Because of the retrospective aspect of our study, the Institutional Review Board of Seoul National University Hospital waived the need for informed consent.
Study design and patient population
This retrospective observational study evaluated adult patients aged 20–90 years who received endotracheal intubation and mechanical ventilation of ≥ 2 h during non-cardiac surgery at Seoul National University Hospital between January 2011 and November 2020. The exclusion criteria were as follows: (1) preoperative kidney dysfunction, defined as preoperative serum creatinine ≥ 4 mg/dL or a history of renal replacement therapy within three months before surgery; (2) one lung ventilation; (3) organ transplantation or donor surgery; (4) kidney or bladder resection surgery; (5) recorded counts of intraoperative tidal volumes < 24; (6) PBW ≤ 30 kg; (7) reoperation within seven days after surgery, (8) tracheostomy or presence of tracheostoma, and (9) missing data on confounding variables, including height, weight, and intraoperative tidal volume. We aimed to include only complete cases in the final analysis to reduce biases.
Primary exposure
The primary exposure of interest was the mean tidal volume applied during intraoperative mechanical ventilation divided by the PBW. This mean tidal volume was determined based on the actual values delivered to the patients rather than the pre-set values. Patient monitors SolarTM 8000 M (GE Healthcare, Wauwatosa, WI, USA) and Intellivue MX800 (Philips Healthcare Canada, Saint-Laurent, QC, Canada) were used. The ventilators used were Primus (Drager, Lubeck, Germany) and Datex-Ohmeda (GE Healthcare). Due to technical limitations at our institution, data on tidal volume were collected from anesthesia records at 5-min intervals between January 2011 and August 2013 and at 1-min intervals after August 2013. For intraoperative tidal volume, we excluded outliers (tidal volume < 200 ml or > 1200 ml) and cases with recorded counts of intraoperative tidal volume less than 24 before calculating the mean value. The PBW was calculated as follows: for male patients, 50 + 0.91 (centimeters of height—152.4); for female patients, 45.5 + 0.91(centimeters of height—152.4)37. Patients were categorized into the high- or low-tidal volume group based on whether their tidal volume was > 8 ml/kg PBW or ≤ 8 ml/kg PBW.
All data were extracted from our hospital's clinical data warehouse (SUPREME version 1.0 and 2.0). Demographic and clinical data, such as age, sex, height, weight, American Society of Anesthesiologists (ASA) physical status classification, and comorbidities, such as hypertension, diabetes mellitus, and a history of chronic kidney disease, were collected. Additionally, preoperative nephrotoxic agent and preoperative laboratory test results were collected, including hemoglobin, white blood cell count, serum creatinine, albumin, and surgery-related variables, such as the type of surgery and whether it was emergency surgery. Intraoperative data included tidal volume, duration of anesthesia, type of anesthesia (inhalational versus total intravenous anesthesia), transfusion, and mean values of mean blood pressure, calculated from invasive or non-invasive measurements at 1–5-min intervals from anesthesia records. To quantify hypotension exposure, we calculated a time-weighted average (TWA) of mean blood pressure (MBP) < 65 mmHg. We collected MBP values at 1- to 5-min intervals throughout the surgery. Using the trapezoidal rule for numerical integration, we calculated the area between the 65 mmHg threshold and the MBP curve when MBP was below 65 mmHg. This area was then divided by the total area under the MBP curve for the entire surgery duration38.
Primary outcome
The primary outcome was the development of AKI within seven days postoperatively. AKI was diagnosed according to the Kidney Disease Improving Global Outcomes (KDIGO) criteria on the basis of changes in the serum creatinine level7,39. The baseline serum creatinine value was defined as the most recent one measured within three months before surgery. The secondary outcomes included the incidence of AKI based on severity (mild: stage 1 AKI; moderate-to-severe: stage 2 or 3 AKI) and the length of hospital stay.
Statistical analysis
Continuous data are described as the median (interquartile range) or the mean (standard deviation) and were compared using the Mann–Whitney U test or independent t-test, respectively, according to the normality of their distribution on the Shapiro–Wilk test. Categorical data are described as numbers (percentages) and were analyzed using the chi-square or Fisher exact test according to their expected counts.
Our statistical analysis consisted of several steps. First, we calculated propensity scores using a logistic regression model. We then used these scores to perform inverse probability of treatment weighting (IPTW). Following this, we conducted our primary analysis comparing outcomes between the two groups using weighted logistic regression models. We also performed multivariable logistic regression and restricted cubic spline regression analyses to further examine the relationship between tidal volume and postoperative AKI. Finally, we conducted an additional analysis using propensity score matching to confirm the robustness of our study.
For the propensity score calculation, we initially considered 13 variables in the multivariable logistic regression model which were identified using a directed acyclic graph (Supplementary Figure S5). To assess multicollinearity, we calculated variance inflation factors for all variables in the model. Due to multicollinearity concerns, we removed the orthopedic surgery variable. The final model for the propensity score calculation included 12 variables: age, sex, body mass index, ASA physical status (ASA I–II vs III–IV), the presence of diabetes mellitus, hypertension, history of chronic kidney disease, year of surgery, type of surgery (general surgery, neurosurgery, and gynecologic/urologic surgery), and emergency surgery. Subsequently, we conducted stabilized IPTW to adjust for confounding variables and enhance the validation of our results40. For the IPTW calculation, we used a logistic regression model with the tidal volume group as the dependent variable and all 12 covariates from the propensity score model as independent variables. For treated patients, the stabilized weight was the marginal probability of treatment divided by the patient’s propensity score. For untreated patients, it was one minus the marginal probability of treatment, divided by one minus the patient’s propensity score. To mitigate the influence of extreme weights, we applied a truncation level of 0.01, replacing weights below the 1st percentile or above 99th percentile with the corresponding percentile values41. The balance between variables in the two groups was assessed using the standardized mean difference (SMD). Variables with an SMD < 0.1 were deemed balanced.
The primary and secondary outcomes were compared between the two groups in both the unweighted and weighted cohorts after IPTW. For each outcome, we fitted a separate logistic regression model with the tidal volume group as the independent variable and specific outcome as the dependent variable. These models were weighted using the calculated IPTW values. From each model, the odds ratio, 95% CI, and P-value for the effect of high tidal volume on the outcome were extracted. This process was repeated for all primary and secondary outcomes between the two groups. Additionally, we conducted a multivariable logistic regression analysis, incorporating intraoperative variables into the covariates used in the IPTW analysis to evaluate their impact on postoperative AKI. We used a generalized linear model with a binomial family and logit link function, weighted by the IPTW values. Before inclusion in the model, all continuous variables were standardized using the scale function. The model incorporated the covariates used in the IPTW analysis along with additional intraoperative variables included high intraoperative tidal volume (> 8 ml/kg PBW), anesthesia duration, total intravenous anesthesia use, intraoperative transfusion, and time-weighted mean blood pressure. A restricted cubic spline regression analysis was conducted to examine the relationship between the intraoperative tidal volume and log odds of postoperative AKI. We fitted a logistic regression model with restricted cubic splines, using three knots for intraoperative tidal volume. The model was adjusted for the same variables used in the IPTW calculation and was weighted using the IPTW values. The results were visualized using a plot showing the estimated odds of postoperative AKI across the range of intraoperative tidal volumes, with 95% confidence intervals.
As an additional analysis to assess the robustness of the main results, propensity score matching was also performed with a 1:1 optimal nearest neighbor matching and a caliper of 0.1 using propensity scores with covariates the same as those in IPTW analysis. After propensity score matching, multivariable logistic regression and restricted cubic spline regression analyses were also performed. The multivariable logistic regression model included the same covariates as in the main analysis. For the restricted cubic spline regression, three knots were used for the tidal volume variable. During the revision process, we were requested to evaluate the effects of acid–base status, minute ventilation and positive end-expiratory pressure on the relationships between tidal volume and postoperative AKI. We performed the multivariable logistic regression analysis incorporating the abovementioned variables. Subgroup analyses based on sex and type of surgery were also additionally performed. All statistical analyses were conducted using R, version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria). A two-sided P-value of < 0.05 was considered statistically significant.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Boyer, N., Eldridge, J., Prowle, J. R. & Forni, L. G. Postoperative acute kidney injury. Clin. J. Am. Soc. Nephrol. 17, 1535–1545 (2022).
Gumbert, S. D. et al. Perioperative acute kidney injury. Anesthesiology 132, 180–204 (2020).
Gameiro, J., Fonseca, J. A., Neves, M., Jorge, S. & Lopes, J. A. Acute kidney injury in major abdominal surgery: Incidence, risk factors, pathogenesis and outcomes. Ann. Intensive Care 8, 1–10 (2018).
Hobson, C. et al. Cost and mortality associated with postoperative acute kidney injury. Ann. Surg. 261, 1207 (2015).
O’connor, M., Kirwan, C., Pearse, R. & Prowle, J. Incidence and associations of acute kidney injury after major abdominal surgery. Intensive Care Med. 42, 521–530 (2016).
French, W. B. et al. Mortality and costs associated with acute kidney injury following major elective, non-cardiac surgery. J. Clin. Anesth. 82, 110933 (2022).
Prowle, J. R. et al. Postoperative acute kidney injury in adult non-cardiac surgery: Joint consensus report of the Acute Disease Quality Initiative and PeriOperative Quality Initiative. Nat. Rev. Nephrol. 17, 605–618 (2021).
Deng, Q.-W. et al. Intraoperative ventilation strategies to prevent postoperative pulmonary complications: A network meta-analysis of randomised controlled trials. Br. J. Anaesth. 124, 324–335 (2020).
Guay, J., Ochroch, E. A. & Kopp, S. Intraoperative use of low volume ventilation to decrease postoperative mortality, mechanical ventilation, lengths of stay and lung injury in adults without acute lung injury. Cochrane Database Syst. Rev. CD011151 (2018).
Young, C. C. et al. Lung-protective ventilation for the surgical patient: International expert panel-based consensus recommendations. Br. J. Anaesth. 123, 898–913. https://doi.org/10.1016/j.bja.2019.08.017 (2019).
Koyner, J. L. & Murray, P. T. Mechanical ventilation and lung–kidney interactions. Clin. J. Am. Soc. Nephrol. 3, 562–570 (2008).
Annat, G. et al. Effect of PEEP ventilation on renal function, plasma renin, aldosterone, neurophysins and urinary ADH, and prostaglandins. Anesthesiology 58, 136–141 (1983).
Pannu, N. & Mehta, R. L. Effect of mechanical ventilation on the kidney. Best Pract. Res. Clin. Anaesthesiol. 18, 189–203 (2004).
Dreyfuss, D. & Saumon, G. Ventilator-induced lung injury: Lessons from experimental studies. Am. J. Respir. Crit. Care Med. 157, 294–323 (1998).
Chertow, G. M. et al. Predictors of mortality and the provision of dialysis in patients with acute tubular necrosis. The Auriculin Anaritide Acute Renal Failure Study Group. J. Am. Soc. Nephrol. 9, 692–698 (1998).
van den Akker, J. P., Egal, M. & Groeneveld, A. Invasive mechanical ventilation as a risk factor for acute kidney injury in the critically ill: A systematic review and meta-analysis. Crit. Care (London, England) 17, 1–9 (2013).
Cortjens, B. et al. Lung-protective mechanical ventilation does not protect against acute kidney injury in patients without lung injury at onset of mechanical ventilation. J. Crit. Care 27, 261–267 (2012).
Karalapillai, D. et al. Effect of intraoperative low tidal volume vs conventional tidal volume on postoperative pulmonary complications in patients undergoing major surgery: A randomized clinical trial. Jama 324, 848–858 (2020).
Tojo, K., Mihara, T. & Goto, T. Effects of intraoperative tidal volume on incidence of acute kidney injury after cardiovascular surgery: A retrospective cohort study. J. Crit. Care 56, 152–156 (2020).
Argalious, M. Y., Mao, G., Davison, R. K., Chow, C. & Bhavani, S. Association of intraoperative tidal volumes and acute kidney injury after noncardiac surgery. Anesth. Analg. 130, 925–932 (2020).
Bae, J. et al. Relationship between intraoperative tidal volume and acute kidney injury following off-pump coronary artery bypass grafting: A retrospective observational study. Medicine 101, e31563 (2022).
Jia, X.-Y. et al. Effect of intraoperative low vs. conventional tidal volume on the incidence of postoperative acute kidney injury after noncardiac surgery: A two-center randomized clinical trial. Minerva Anestesiol. (2023).
Kheterpal, S. et al. Predictors of postoperative acute renal failure after noncardiac surgery in patients with previously normal renal function. Anesthesiology 107, 892–902 (2007).
Kheterpal, S. et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: Results from a national data set. Anesthesiology 110, 505–515 (2009).
Bell, S. et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery—development and validation of a risk score and effect of acute kidney injury on survival: Observational cohort study. Bmj 351, h5639 (2015).
Li, S., Wang, S., Priyanka, P. & Kellum, J. A. Acute kidney injury in critically ill patients after non-cardiac major surgery: Early versus late onset. Crit. Care Med. 47, e437 (2019).
Sun, L. Y., Wijeysundera, D. N., Tait, G. A. & Beattie, W. S. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 123, 515–523 (2015).
Nie, S., Tang, L., Zhang, W., Feng, Z. & Chen, X. Are there modifiable risk factors to improve AKI?. BioMed Res. Int. 2017, 5605634 (2017).
Kuiper, J. W., Groeneveld, A. B. J., Slutsky, A. S. & Plötz, F. B. Mechanical ventilation and acute renal failure. Crit. Care Med. 33, 1408–1415 (2005).
Imai, Y. et al. Injurious mechanical ventilation and end-organ epithelial cell apoptosis and organ dysfunction in an experimental model of acute respiratory distress syndrome. Jama 289, 2104–2112 (2003).
Gurkan, O. U., O’Donnell, C., Brower, R., Ruckdeschel, E. & Becker, P. M. Differential effects of mechanical ventilatory strategy on lung injury and systemic organ inflammation in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 285, L710–L718 (2003).
Alge, J. et al. Two to tango: Kidney-lung interaction in acute kidney injury and acute respiratory distress syndrome. Front. Pediatr. 744110 (2021).
Amoah, J. et al. Comparing propensity score methods versus traditional regression analysis for the evaluation of observational data: A case study evaluating the treatment of gram-negative bloodstream infections. Clin. Infect. Dis. 71, e497–e505 (2020).
Wilkinson, J. D., Mamas, M. A. & Kontopantelis, E. Logistic regression frequently outperformed propensity score methods, especially for large datasets: A simulation study. J. Clin. Epidemiol. 152, 176–184 (2022).
Kurth, T. et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am. J. Epidemiol. 163, 262–270 (2006).
Chesnaye, N. C. et al. An introduction to inverse probability of treatment weighting in observational research. Clin. Kidney J. 15, 14–20 (2022).
Network, A. R. D. S. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. New Engl. J. Med. 342, 1301–1308 (2000).
Maheshwari, K. et al. A randomized trial of continuous noninvasive blood pressure monitoring during noncardiac surgery. Anesth. Analg. 127, 424 (2018).
Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 120, c179–c184 (2012).
Brookhart, M. A., Wyss, R., Layton, J. B. & Stürmer, T. Propensity score methods for confounding control in nonexperimental research. Circ. Cardiovasc. Qual. Outcomes 6, 604–611 (2013).
Schulte, P. J. & Mascha, E. J. Propensity score methods: Theory and practice for anesthesia research. Anesth. Analg. 127, 1074–1084 (2018).
Author information
Authors and Affiliations
Contributions
Ji-Yoon Jung: conceptualization, methodology, software, validation, formal analysis, investigation, data curation, writing of the original draft and visualization; Seung Eun Song, So Yeong Hwang, Won Ho Kim: methodology, validation and investigation; Suhyun Hwangbo: methodology, formal analysis, validation, investigation and visualization; Hyun-Kyu Yoon: conceptualization, methodology, project administration, supervision, and review and editing of the original draft. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jung, JY., Song, S.E., Hwangbo, S. et al. Association between intraoperative tidal volume and postoperative acute kidney injury in non-cardiac surgical patients using a propensity score-weighted analysis. Sci Rep 14, 20079 (2024). https://doi.org/10.1038/s41598-024-71134-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71134-7