Abstract
Systemic lupus erythematosus (SLE) commonly damages the blood system and often manifests as blood cell abnormalities. The performance of biomarkers for predicting SLE activity still requires further improvement. This study aimed to analyze blood cell parameters to identify key indicators for a SLE activity prediction model. Clinical data of 138 patients with SLE (high activity, n = 40; moderate activity, n = 44; mild activity, n = 37; low activity, n = 17) and 100 healthy controls (HCs) were retrospectively analyzed. Data from 89 paired admission–discharge patients with SLE were collected. Differences and associations between blood cell parameters and disease indicators, as well as the relationship between the these parameters and organ damage, were examined. Machine-learning methods were employed to develop a prediction model for disease activity evaluation. Most blood cell parameters (22/26, 84.62%) differed significantly between patients with SLE and HCs. Analysis of 89 paired patients with SLE revealed significant changes in most blood cell parameters at discharge. The standard deviation of lymphocyte volume (SD-V-LY), red blood cell (RBC) count, lymphocyte percentage (LY%), hemoglobin(HGB), hematocrit(HCT), and neutrophil percentage(NE%) correlated with disease activity. By employing machine learning, an optimal model was established to predict active SLE using SD-V-LY, RBC count, and LY% (area under the curve [AUC] = 0.908, sensitivity = 0.811). External validation indicated impressive performance (AUC = 0.940, sensitivity = 0.833). Correlation analysis revealed that SD-V-LY was positively correlated with ESR, IgG, IgA, and IgM but was negatively correlated with C3 and C4. The RBC count was linked to renal and hematopoietic system impairments, whereas LY% was associated with joint/muscle involvement. In conclusion, SD-V-LY is associated with SLE disease activity. SD-V-LY combined with RBC count and LY% contributes to a prediction model, which can be utilized as an effective tool for assessing SLE activity.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disease characterized by immune dysregulation arising from the interaction of various genetic, environmental, and endocrine factors, resulting in the continuous production and deposition of autoimmune complexes throughout the body. Consequently, this triggers systemic inflammation and multiple organ dysfunction1. SLE presents with various clinical symptoms, typically alternating between periods of remission and activity2. Given that the disease activity and manifestations of SLE change over time3, it is important to modify treatment according to the current disease status and to monitor the treatment response in order to minimize organ damage or permanent sequelae in SLE. Thus, developing a precise tool for SLE disease activity assessment is valuable. The Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) is considered the most common tool used for evaluating SLE disease activity, with SLEDAI 2000 (SLEDAI-2 K) being frequently used4. Nonetheless, SLEDAI-2 K is complex, subjective, and limited owing to its reliance on numerous time-consuming tests5.
Hematological diseases such as leukopenia and anemia often accompany SLE development. In cases of autoimmune hemolytic anemia, the red blood cell (RBC) count significantly decreases6,7. Abnormalities in lymphocyte-mediated cellular immune function and apoptosis significantly contribute to the pathogenesis of SLE. Excessive stimulation of antigen-presenting cells results in increased T-lymphocyte apoptosis, wherein DNA and nucleosomes released in substantial quantity during apoptosis may act as self-antigens, thereby eliciting B-lymphocyte activation and subsequent autoantibody production8,9. This cascade of events is frequently accompanied by alterations in lymphocyte quantity, morphology, and internal structure, which may be closely correlated with SLE disease activity.
Aberrant activation of the immune system results in morphological and functional changes in blood cells. This study aimed to analyze the association between blood cell parameters (routine blood parameters and cell population data) and disease activity in hospitalized patients with SLE. We first developed a prediction model to provide a cost-effective and user-friendly tool for assessing disease activity in hospitalized patients with SLE, particularly focusing on clinical utilization and inpatients at grassroots medical institutions.
Methods
Human participants
For this study, data were retrospectively collected from a cohort of 138 hospitalized patients with SLE at a single center. Patients were consecutively enrolled and diagnosed based on the 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for SLE10. The reasons for hospitalization among 138 patients with SLE were as follows: increased disease activity (n = 53), new organ damage as a complication (n = 51), first-time patients seeking systemic treatment (n = 28), and emergence of SLE-related symptoms for a definitive diagnosis (n = 6). Disease activity was evaluated using the SLEDAI-2 K4. Patients were divided into four subgroups according to their SLEDAI-2 K scores at admission: low activity (SLEDAI-2 K ≤ 4, n = 17), mild activity (5 ≤ SLEDAI-2 K ≤ 9, n = 37), moderate activity (10 ≤ SLEDAI-2 K ≤ 14, n = 44), and high activity (SLEDAI-2 K ≥ 15, n = 40). Out of 138 participants, 89 had matched admission–discharge data. Patients with other autoimmune diseases, pregnancy, infections caused by various factors such as bacteria and viruses, or major illnesses were excluded from the SLE cohort. Age- and sex-matched individuals without chronic medical conditions or medication use were recruited as healthy controls (HCs, n = 100) for routine physical examination. Furthermore, 60 patients with SLE and varying disease activity at different time points were included for external validation.
This study employed a retrospective analysis method. All methods were conducted in accordance with relevant guidelines and regulations or with the Declaration of Helsinki. The study protocol was reviewed and approved by the Ethics Committee of Xiangya Hospital, Central South University, where the study was conducted (approval no. 20240235). The need for the acquisition of informed consent was waived by the Ethics Committee of Xiangya Hospital, Central South University owing to retrospective nature of this study.
Laboratory analysis
Demographic data such as sex, age, disease duration, and SLEDAI-2 K score were obtained. Additionally, various laboratory parameters were evaluated in patients with SLE. An indirect immunofluorescence assay (EUROIMMUN Medical Diagnostics, Germany) was used to detect the antinuclear antibody (ANA) spectrum [reference range: negative], anti-double-stranded DNA (dsDNA) antibody [negative], anti-Smith antibody [negative], anti-ribosome P antibody [negative], and anti-nucleosome antibody [negative]. Immunoturbidimetry with an IMMAGE 800 analyzer (Beckman Coulter Inc., Brea, CA, USA) was employed to measure the levels of complement protein 4 (C4) [100.0–400.0 mg/L], complement protein 3 (C3) [790.0–1520.0 mg/L], immunoglobulin G (IgG) [7.0–16.0 g/L], immunoglobulin A (IgA) [700.0–5000.0 mg/L], immunoglobulin M (IgM) [400.0–2800.0 mg/L], and C-reactive protein (CRP) [≤ 8.0 mg/L]. The Westergren method was utilized for detecting terythrocyte sedimentation rate (ESR) [≤ 15 mm/h in males or ≤ 20 mm/h in females]. The UniCel DxH 800 hematology analyzer (Beckman Coulter Inc., Brea, CA, USA)was applied to assess routine blood parameters, which included white blood cell (WBC) count [3.5–9.5 × 109/L], RBC count [4.3–5.8 × 1012/L in males or 3.8–5.1 × 1012/L in females], hemoglobin (HGB) [130.0–175.0 g/L in males or 115.0–150.0 g/L in females], hematocrit (HCT) [40.0–50.0% in males or 35.0–45.0% in females], mean corpuscular volume (MCV) [82.0–100.0 fL], mean corpuscular hemoglobin (MCH) [27.0–34.0 pg], red blood cell distribution width (RDW)[11.0–15.0%], platelet (PLT) count[125.0–350.0 × 109/L], neutrophil count and percentage (NE# and NE%) [1.8–6.3 × 109/L and 40.0–75.0%], lymphocyte count and percentage (LY# and LY%) ([1.1–3.2 × 109/L and 20.0–50.0%], and monocyte count and percentage (MO# and MO%) [0.1–0.6 × 109/L and 3.0–10.0%].The reference ranges for the aforementioned serological and hematological parameters are presented in Supplementary Table 1. Additionally, it provided the following cell population data: mean volume of neutrophils, lymphocytes, and monocytes (MN-V-NE, MN-V-LY, and MN-V-MO, respectively); standard deviation (SD) of neutrophil, lymphocyte, and monocyte volume (SD-V-NE, SD-V-LY, and SD-V-MO, respectively); mean conductivity of neutrophils, lymphocytes, and monocytes (MN-C-NE, MN-C-LY, and MN-C-MO, respectively); and SD of neutrophil, lymphocyte, and monocyte conductivity (SD-C-NE, SD-C-LY, and SD-C-MO, respectively). The demographic data and clinical characteristics of the SLE cohort and 89 paired patients are presented in Tables 1 and 2, respectively.
Statistical analysis
Statistical analyses were performed using SPSS software version 25.0 (IBM SPSS Statistics, IBM Corp., Armonk, NY, USA) and Prism software version 10.1.0 (GraphPad Software Inc., San Diego, CA, USA). Normality of data was assessed using the Kolmogorov–Smirnov test. Significance of standard deviation (SD) comparisons was assessed by the F-test. Normally distributed data with homogeneous variances were presented as mean ± SD, and differences between these groups were compared using the t-test or one-way ANOVA. For non-normally distributed data or variables with heterogeneous variances, data were presented as the median (interquartile range), and group differences were evaluated using the Kruskal–Wallis or Mann–Whitney U test. For categorical data, the Chi-square or Fisher’s exact test was used for component comparison. Bonferroni correction was applied to adjust for multiple comparisons. Paired data were analyzed using the paired-sample t-test or Wilcoxon signed-rank test. Correlations between variables were assessed using Spearman’s rank correlation. Univariate logistic regression (LG) was employed to analyze the associations of SD-V-LY, RBC count, and LY% with a specific binary outcome variable. A p-value < 0.05 was considered statistically significant in all comparisons and correlations.
Prediction model development based on machine learning
The prediction model was developed using the Deepwise and Beckman Coulter DxAI platforms (https://dxonline.deepwise.com/). All 26 clinical features of the blood cell parameters were used as independent variables. Feature selection was performed in three steps. First, a differential analysis and univariate regression analysis were conducted for the 26 variables, identifying seven variables significantly associated with disease activity. A p-value < 0.05 was considered statistically significant. Second, Spearman’s correlation coefficient (SCC) was calculated for variables showing differences. If the SCC value was > 0.7, then one variable was randomly eliminated11. Finally, the variables optimized based on their feature weights were selected for model building. The modeling dataset was randomly split into two subsets: 70% for the training cohort and 30% for the internal validation cohort. The outcome of the dependent variable was classified into two groups: the low activity group with SLEDAI-2 K ≤ 4 and the higher activity group with SLEDAI-2 K ≥ 5. After feature selection, LG was selected as the final model based on its optimal performance. The performance of the LG model was assessed using metrics such as the area under the curve (AUC), accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and F1-score. Additionally, an external validation cohort was collected from various periods to evaluate the generalization capability of the LG model.
Results
Distribution of SD-V-LY, RBC count, and LY% in SLE patients and HCs
The values of SD-V-LY, RBC count, and LY% in patients with SLE and HCs are shown in Supplementary Fig. 1. Notably, patients with SLE exhibited significantly elevated SD-V-LY compared with HCs (median [IQR]: 15.8 [14.2–18.4] vs. 13.1 [12.5–13.9], p < 0.001) (Supplementary Fig. 1a) and showed markedly lower RBC count and LY% than HCs (3.5 [2.9–3.9] × 1012/L vs. 4.4 [4.2–4.6] × 1012/L, p < 0.001 and 20.2% [12.7–27.5] vs. 32.4% [27.7–38.2], p < 0.001) (Supplementary Fig. 1b and c). Apart from WBC count, PLT count, NE#, MO#, and MN-V-NE, all other blood cell parameters demonstrated significant differences between patients with SLE and HCs (Supplementary Table 3).
Discharged patients with SLE had decreased SD-V-LY values compared to those admitted
Discharged patients with SLE demonstrated a significant decrease in SD-V-LY values compared to those in admitted patients (median [IQR]: 15.7 [14.1–17.5] vs. 16.2 [14.5–19.2], p = 0.002) (Supplementary Fig. 2). Higher RBC count and LY% were observed in discharged patients with SLE (mean ± SD: 3.31 ± 0.68 × 1012/L and median [IQR]: 20.0 [12.6–25.5]%) compared with those in admitted patients (3.28 ± 0.82 × 1012/L and 18.9 [11.7–26.1]%). However, no significant differences were observed between the two groups.Additionally, the levels of MCV, MCH, PLT, NE#, LY#, MO#, SD-V-NE, MN-V-LY, SD-C-LY, MN-V-MO, SD-V-MO, MN-C-MO, and SD-C-MO were significantly different between inpatients and discharged patients with SLE (Table 2).
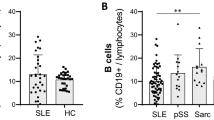
Distribution of SD-V-LY, RBC count, and LY% in patients with SLE based on different disease activities
The distribution of SD-V-LY, RBC count, and LY% in patients with SLE showing different disease activities is depicted in Fig. 1. The 138 patients with SLE were classified into four subgroups according to the SLEDAI-2 K: low activity, mild activity, moderate activity, and high activity. These subgroups differed in terms of the distribution of LY%, RBC count, and SD-V-LY. Patients with mild (median [IQR]: 16.39 [14.4–18.4]) and high (16.6 [15.2–19.8]) activities had substantially elevated SD-V-LY values compared with patients with low activity (14.2 [3.0–15.3]) (Fig. 1a). The RBC count was considerably lower in patients with moderate (mean ± SD: [3.3 ± 0.8] × 1012/L) and high ([3.2 ± 0.6] × 1012/L) disease activities than in those with low activity ([3.9 ± 0.4] × 1012/L) (Fig. 1b). Notably, LY% was lower in patients with mild (16.0 [11.7–26.9]), moderate (18.5 [13.9–24.0]), and high (20.2 [10.8–25.9]) disease activities than in patients with low activity (33.5 [23.4–36.0]) (Fig. 1c). Additionally, the levels of HGB, HCT, LY#, and NE% were significantly different among the various groups (Table 1).
The distribution of SD-V-LY, RBC count, and LY% in SLE patients with different disease activities. Standard deviation of lymphocyte volume (SD-V-LY) (a), red blood cell (RBC) count (b), and lymphocyte percentage (LY%) (c) among the subgroups were differentially distributed. The 138 patients with systemic lupus erythematosus (SLE) at admission were classified into four subgroups according to the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2 K): low activity (SLEDAI-2 ≤ 4, n = 17), mild activity (5 ≤ SLEDAI-2 K ≤ 9, n = 37), moderate activity (10 ≤ SLEDAI-2 K ≤ 14, n = 44), and high activity (SLEDAI-2 K ≥ 15, n = 40). Bonferroni correction was applied to adjust for multiple comparisons. *p < 0.05; **p < 0.01.
Correlation between blood cell parameters and disease activity in patients with SLE
Disease activity in patients with SLE was assessed using SLEDAI-2 K, and the correlations between blood cell parameters and SLEDAI-2 K are displayed in Table 3. SLEDAI-2 K correlated positively with SD-V-LY (r = 0.234, p = 0.006) and NE% (r = 0.207, p = 0.015), but correlated negatively with RBC count (r = − 0.323, p < 0.001), HGB levels (r = − 0.357, p < 0.001), and HCT levels (r = − 0.357, p < 0.001). Additionally, a weak but significant negative correlation was observed between SLEDAI-2 K and LY% (r = − 0.188, p = 0.027).
Establishment and evaluation of a prediction model for distinguishing higher activity from low activity in patients with SLE
To establish a prediction model for discriminating higher activity from low activity in patients with SLE, we conducted a univariate LG analysis to compare all 26 blood cell parameters. The results revealed significant differences in the following seven indicators: RBC count, HGB, HCT, NE%, LY#, LY%, and SD-V-LY (Table 4). The SCC was calculated among these seven indicators (Supplementary Fig. 3). If the SCC value was > 0.7, then one variable was randomly eliminated. After performing feature selection, three features of the seven independent variables were used to build the model: RBC count, LY%, and SD-V-LY. Further multivariate logistic analysis (Table 4) demonstrated that RBC count (odds ratio [OR]: 0.291, 95% confidence interval [CI]: 0.113–0.754), LY% (OR: 0.913, 95% CI: 0.862–0.967), and SD-V-LY (OR: 1.354, 95% CI: 1.056–1.737) were independent risk factors for SLE activity. Among the 14 constructed machine-learning models, four demonstrated superior performance (Table 5), with the LG model exhibiting optimal efficiency in terms of AUC (0.908), sensitivity (0.811), and positive predictive value (0.938). The importance of these features was determined using a designated algorithm. Specifically, the LG model assigned the following weights to the three features: LY% had the highest weight, followed by RBC count and SD-V-LY with decreasing weights (-1, -0.869, and 0.577, respectively). The performance of external validation was considered to be satisfactory, achieving an AUC of 0.940 (95% CI: 0.884–0.998) and a sensitivity of 0.833, resulting in an accuracy of 0.850. The fundamental characteristics of the external validation dataset are presented in Supplementary Table 4.
This study established a prediction model for assessing disease activity in patients with SLE. Clinicians can access an online platform and input three feature values to predict the disease activity level of patients with SLE. The corresponding probability of outcomes can be calculated from the following website: https://dxonline.deepwise.com/prediction/index.html?baseUrl=%2Fapi%2F&id=42359&topicName=undefined&from=share&platformType=wisdom.
Correlation between SD-V-LY, RBC count, and LY% and disease indicators of SLE
The comparison results for SD-V-LY, RBC count, and LY% between different SLE disease indicator groups are presented in Supplementary Tables 5, 6, and 7. When comparing the groups, SD-V-LY was widely associated with SLE disease indicators. The 138 patients with SLE were divided into three groups according to their ANA titers: 1:80, 1:160, and 1:320. Evidently, a remarkable discrepancy in the SD-V-LY values was observed among these groups (14.0 [12.6–15.3]) vs. (15.3 [13.9–16.9]) vs. (17.4 [15.6–19.5], all p < 0.05) (Fig. 2a). SD-V-LY values were significantly higher in patients with SLE who had positive results for anti-dsDNA, anti-Smith, anti-ribosome P, and anti-nucleosome antibodies than in patients who had negative results (p < 0.01 all). Additionally, patients with SLE displaying abnormal C4 levels, C3 levels, or ESR had elevated SD-V-LY values (all p < 0.05) (Fig. 2b). Nevertheless, there was little variation in the RBC count and LY% when these indicators were aberrant, except in C3 (Supplementary Tables 5, 6, and 7).
The associations between SD-V-LY and various SLE disease indicators. Standard deviation of lymphocyte volume (SD-V-LY) is widely associated with indicators of systemic lupus erythematosus (SLE). The SD-V-LY values in patients with SLE increased as the antinuclear antibody (ANA) titer increased (a). For anti-dsDNA-, anti-Smith-, anti-ribosome P-, and anti-nucleosome-positive patients with SLE, the SD-V-LY values were significantly higher than those of negative patients. Moreover, SD-V-LY values were notably higher in patients with SLE with abnormal complement protein 4 (C4), complement protein 3 (C3), and erythrocyte sedimentation rate (ESR) (b). Bonferroni correction was applied to adjust for multiple comparisons, and the Mann-Whitney U test was employed for comparisons between the two groups.*p < 0.05; **p < 0.01; ***p < 0.001. Normal: variable results that are within the reference range or are negative. Abnormal: variable results that are outside the reference range or are positive.
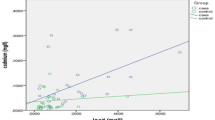
The results for Spearman’s rank correlation analysis between SD-V-LY, RBC count, LY%, and quantitative SLE disease indicators are presented in Supplementary Table 8. The associations between SD-V-LY and quantitative SLE disease indicators are shown in Fig. 3. Correlation analysis revealed a significant positive association between SD-V-LY values and ESR (r = 0.277, p = 0.001), IgG (r = 0.509, p < 0.001), IgA (r = 0.302, p < 0.001) (Fig. 3a, d, and e), and IgM (r = 0.277, p = 0.001) (Fig. 3f). Conversely, SD-V-LY values correlated negatively with C4 (r = − 0.393, p < 0.001) and C3 (r = -0.412, p < 0.001) (Fig. 3b and c). However, no significant correlation was observed between SD-V-LY values and CRP levels (r = 0.548, p = 0.052). The RBC count correlated with CRP levels (r = − 0.185, p = 0.030), C3 levels (r = 0.333, p < 0.001) and IgM levels (r = 0.259, p = 0.002), whereas LY% correlated exclusively with CRP levels (r = − 0.293, p < 0.001) and IgM levels (r = 0.279, p = 0.001) (Supplementary Table 8).
Associations of SD-V-LY with other SLE disease indicators. Associations of the standard deviation of lymphocyte volume (SD-V-LY) with the erythrocyte sedimentation rate (ESR) (a), complement protein 4 (C4) (b), complement protein 3 (C3) (c), immunoglobulin G (IgG) (d), immunoglobulin A (IgA) (e), and immunoglobulin M (IgM) (f) in patients with systemic lupus erythematosus (SLE). Spearman’s rank correlation coefficients were used to assess the associations between SD-V-LY values and these disease indicators in 138 patients with SLE. Statistical significance was set at p < 0.05.
Correlation between SD-V-LY, RBC count, LY%, and organ damage in patients with SLE
Correlations between SD-V-LY, RBC count, LY%, and major organ damage in patients with SLE are shown in Table 6. The results indicated that the RBC count was linked to impairments in the kidney (OR: 2.875, p = 0.001) and hematopoietic system (OR: 4.879, p < 0.001), whereas LY% was associated with joint/muscle involvement (OR: 1.038, p = 0.034). However, SD-V-LY did not show a significant relationship with any organ system abnormalities.
Discussion
The present study revealed notable variations in SD-V-LY, RBC count, and LY% in patients with SLE who exhibited varying disease activities. By combining SD-V-LY, RBC count, and LY%, we mark the first attempt to develop an effective prediction model for distinguishing hospitalized patients with highly active SLE. Notably, SD-V-LY is closely correlated with various disease indicators in patients with SLE.
Hematological abnormalities are among the frequently observed initial signs of SLE, nonetheless, their underlying mechanisms remain elusive. Immune-mediated bone marrow suppression may be associated with excessive destruction of peripheral blood cells and secondary infections6,12. Our findings indicated marked differences in SD-V-LY, RBC count, and LY% in patients with SLE compared with HCs. Currently, autoimmune hemolytic anemia and chronic disease anemia are the primary contributors to reduced RBC count13,14. Reduced RBC count is a common laboratory finding in patients with SLE. Li et al. reported that 63.8% of 552 patients with SLE had a decreased RBC count15. The primary factors contributing to decreased LY% in patients with SLE are anti-lymphocyte antibodies and lymphocyte apoptosis16. Previous studies reported an incidence of 62–90% for decreased LY% in adult patients with SLE17. Li et al. detected anti-lymphocyte antibodies in over 50% of patients with lymphopenia18. The abnormal increase in SD-V-LY values in patients with SLE may be associated with increased T-lymphocyte apoptosis and abnormal B-lymphocyte activation19,20. Apoptotic cells display membrane vesiculation, nuclear condensation, and DNA fragmentation, whereas activated B-lymphocytes commonly exhibit increased cell volume, elevated cytoplasmic content, and augmented basophilic cytoplasmic granules.
Various studies have demonstrated that most indicators show improvement in patients with SLE after receiving treatment21,22. The results of this study corroborate this finding. In particular, the SD-V-LY values in patients with SLE decreased upon discharge, suggesting that the treatment administered after hospital admission effectively controlled the patients’ condition. The insignificant increase in the RBC count and LY% at discharge might be attributed to the relatively short hospital stay. This further underscores the heightened sensitivity of SD-V-LY values in reflecting changes in disease status.
Our study revealed that SD-V-LY, LY%, and RBC count were closely related to SLE disease activity. This finding may be attributable to the fact that inflammation exacerbation and immune dysregulation in patients with active SLE often lead to a reduction in lymphocyte count and morphological changes23, and that the RBC count is closely associated with the degree of inflammation in patients24. The findings illustrate that blood cell parameters fluctuate with SLE progression in patients and that such fluctuation is intimately linked to disease activity. Moreno-Torres et al. also demonstrated that parameters related to lymphocytes and RBC count were strongly associated with disease activity in patients with SLE25.
In this study, three indices (SD-V-LY, RBC count, and LY%) were ultimately determined for the prediction model to distinguish SLE patients with higher disease activity from those with low disease activity. The outstanding performance of this model indicates its capability to precisely identify SLE patients with increased disease activity, assisting clinicians in effectively identifying high-risk individuals. Previous studies used other blood cell parameters, such as neutrophil-lymphocyte ratio (NLR)26, RDW27, and platelet-lymphocyte ratio (PLR)28, to evaluate disease activity, however, their efficacy was suboptimal. While newer indicators such as cytokines offer improved sensitivity and specificity in determining SLE disease activity29, numerous medical facilities in China, especially grassroots hospitals, lack the specialized equipment required to measure these indicators. In contrast, our prediction model relies solely on the measurement of blood cell parameters and offers a novel, rapid, and convenient method for predicting SLE activity.
As SLE disease activity progresses, the body synthesizes a large quantity of autoantibodies and immunoglobulins and overconsumes complements. Numerous studies have confirmed that SLE disease activity is closely related to the ESR and levels of autoantibodies and complements30,31,32. We observed that the SD-V-LY value correlated closely with these serological parameters. These findings suggest that higher SD-V-LY values may be associated with increased SLE disease activity. However, RBC counts and LY% did not correlate as well as SD-V-LY with these serologic parameters, suggesting that the value of SD-V-LY is more responsive to changes in disease status. Notably, no significant correlation was observed between SD-V-LY and CRP, possibly because CRP is more strongly linked to infections than to SLE disease activity33. This finding is consistent with findings from a previous study by Wang et al.34. Additionally, LG analysis revealed that SD-V-LY was an independent risk factor for SLE higher disease activity. Hence, we speculate that SD-V-LY could serve as an effective biomarker for predicting disease activity and evaluating the inflammatory state of patients with SLE. Furthermore, concerning organ damage assessment, we observed that SD-V-LY was not as valuable as the RBC count and LY%. Therefore, these three parameters complement each other, and incorporating them together can improve the predictive performance of the model.
Despite the novel and clinically relevant findings of this study, it has some limitations. First, our model showed satisfactory discriminative ability between cohorts. However, owing to the limited number of cases included in this single-center study, further multicenter studies are required to validate this prediction model. Second, blood cell parameters are easily influenced by other physiological conditions such as infections, pregnancy, and severe comorbidities. Thus, this model is not applicable to these populations. Third, the data in this study were obtained only from hospitalized patients with SLE, who tend to be sicker than outpatients. These findings need to be confirmed in the outpatient setting. Finally, while this study model can differentiate between higher- and low-activity phases in patients with SLE, it cannot accurately predict the specific disease activity level. Further investigations on more specific biomarkers should be conducted.
Conclusion
Our study provides evidence regarding the significant association of disease activity with SD-V-LY, RBC count, and LY%. SD-V-LY correlated with several disease indicators in patients with SLE, highlighting their involvement in the inflammatory process and their potential as indicators in patients with SLE. Notably, our model successfully distinguished patients with higher SLE disease activity from those with low disease activity, even when conducted at a single center. This study integrated machine learning with laboratory diagnostics, enhanced the accessibility of the model through online applications, and extended its applicability to a broader range of patients.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
- ANA:
-
Antinuclear antibodies
- AUC:
-
Area under the curve
- C3:
-
Complement protein 3
- C4:
-
Complement protein 4
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- dsDNA:
-
Double-stranded DNA
- DMARDs:
-
Disease-modifying anti-rheumatic drugs
- ESR:
-
Erythrocyte sedimentation rate
- HCs:
-
Healthy controls
- HCT:
-
Hematocrit
- HGB:
-
Hemoglobin
- IgA:
-
Immunoglobulin A
- IgG:
-
Immunoglobulin G
- IgM:
-
Immunoglobulin M
- IQR:
-
Interquartile range
- LG:
-
Logistic regression
- LY#:
-
Lymphocyte count
- LY%:
-
Lymphocyte percentage
- MCH:
-
Mean corpuscular hemoglobin
- MCH:
-
Mean corpuscular volume
- MN-C-LY:
-
Mean conductivity of lymphocytes
- MN-C-MO:
-
Mean conductivity of monocytes
- MN-C-NE:
-
Mean conductivity of neutrophils
- MN-V-LY:
-
Mean volume of lymphocytes
- MN-V-MO:
-
Mean volume of monocytes
- MN-V-NE:
-
Mean volume of neutrophils
- MO#:
-
Monocyte count
- MO%:
-
monocyte percentage
- NE#:
-
Neutrophil count
- NE%:
-
Neutrophil percentage
- NLR:
-
Neutrophil-lymphocyte ratio
- OR:
-
Odds ratio
- PLR:
-
Platelet-lymphocyte ratio
- PLT:
-
Platelet
- RBC:
-
Red blood cell
- RDW:
-
RBC distribution width
- ROC:
-
Receiver operating characteristic
- SCC:
-
Spearman’s correlation coefficient
- SD:
-
Standard deviation
- SD-C-LY:
-
Standard deviation of lymphocyte conductivity
- SD-C-MO:
-
Standard deviation of monocyte conductivity
- SD-C-NE:
-
Standard deviation of neutrophil conductivity
- SD-V-LY:
-
Standard deviation of volume of lymphocytes
- SD-V-MO:
-
Standard deviation of volume of monocytes
- SD-V-NE:
-
Standard deviation of volume of neutrophils
- SLE:
-
Systemic lupus erythematosus
- SLEDAI:
-
Systemic lupus erythematosus disease activity index
- Sm:
-
Smith
- WBC:
-
White blood cell
References
Pamfil, C. et al. EULAR recommendations for neuropsychiatric systemic lupus erythematosus vs usual care: results from two European centres. Rheumatology (Oxford)54, 1270–1278. https://doi.org/10.1093/rheumatology/keu482 (2015).
Fanouriakis, A. et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis.78, 736–745. https://doi.org/10.1136/annrheumdis-2019-215089 (2019).
Tanaka, Y. State-of-the-art treatment of systemic lupus erythematosus. Int. J. Rheum. Dis.23, 465–471. https://doi.org/10.1111/1756-185x.13817 (2020).
Ohmura, K. Which is the best SLE activity index for clinical trials? Mod. Rheumatol.31, 20–28. https://doi.org/10.1080/14397595.2020.1775928 (2021).
Onishi, A. et al. Comparisons of SLE-DAS and SLEDAI-2K and classification of disease activity based on the SLE-DAS with reference to patient-reported outcomes. Rheumatology (Oxford)62, 3909–3915. https://doi.org/10.1093/rheumatology/kead132 (2023).
Arathi, N., Sasidharan, P. K. & Geetha, P. Kozhikode criteria for diagnosing systemic lupus erythematosus as a hematological disorder. J. Blood Med.7, 13–18. https://doi.org/10.2147/jbm.S95839 (2016).
Newman, K., Owlia, M. B., El-Hemaidi, I. & Akhtari, M. Management of immune cytopenias in patients with systemic lupus erythematosus - old and new. Autoimmun. Rev.12, 784–791. https://doi.org/10.1016/j.autrev.2013.02.001 (2013).
Peirovy, A. et al. Clinical usefulness of hematologic indices as predictive parameters for systemic lupus erythematosus. Lab. Med.51, 519–528. https://doi.org/10.1093/labmed/lmaa002 (2020).
De Groof, A. et al. Dysregulated lymphoid cell populations in mouse models of systemic lupus erythematosus. Clin. Rev. Allergy Immunol.53, 181–197. https://doi.org/10.1007/s12016-017-8605-8 (2017).
Aringer, M. EULAR/ACR classification criteria for SLE. Semin. Arthritis Rheum.49, S14–s17. https://doi.org/10.1016/j.semarthrit.2019.09.009 (2019).
Mukaka, M. M. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med. J.24, 69–71 (2012).
Santacruz, J. C. et al. A practical perspective of the hematologic manifestations of systemic lupus erythematosus. Cureus14, e22938. https://doi.org/10.7759/cureus.22938 (2022).
Aleem, A., Al Arfaj, A. S., khalil, N. & Alarfaj, H. Haematological abnormalities in systemic lupus erythematosus. Acta Reumatol. Port39, 236–241 (2014).
Klein, A. & Molad, Y. Hematological manifestations among patients with rheumatic diseases. Acta Haematol.144, 403–412. https://doi.org/10.1159/000511759 (2021).
Li, W. G., Ye, Z. Z., Yin, Z. H. & Zhang, K. Clinical and immunological characteristics in 552 systemic lupus erythematosus patients in a southern Province of China. Int. J. Rheum. Dis.20, 68–75. https://doi.org/10.1111/1756-185x.12480 (2017).
Osman, C. & Swaak, A. J. Lymphocytotoxic antibodies in SLE: a review of the literature. Clin. Rheumatol.13, 21–27. https://doi.org/10.1007/bf02229861 (1994).
Ng, W. L., Chu, C. M., Wu, A. K., Cheng, V. C. & Yuen, K. Y. Lymphopenia at presentation is associated with increased risk of infections in patients with systemic lupus erythematosus. QJM99, 37–47. https://doi.org/10.1093/qjmed/hci155 (2006).
Li, C. et al. Antilymphocyte antibodies in systemic lupus erythematosus: association with disease activity and lymphopenia. J. Immunol. Res.2014 672126 (2014). https://doi.org/10.1155/2014/672126
Li, M. et al. Elevated apoptosis and abnormal apoptosis signaling of regulatory T cells in patients with systemic lupus erythematosus. Lupus31, 1441–1455. https://doi.org/10.1177/09612033221119455 (2022).
She, Z. et al. The role of B1 cells in systemic lupus erythematosus. Front. Immunol.13, 814857. https://doi.org/10.3389/fimmu.2022.814857 (2022).
Huang, S. P., Snedecor, S. J., Nanji, S., Lloyd, E. & Bell, C. F. Real-world effectiveness of belimumab in systemic lupus erythematosus: a systematic literature review. Rheumatol. Ther.9, 975–991. https://doi.org/10.1007/s40744-022-00454-9 (2022).
Wang, M. et al. The effectiveness and safety of total glucosides of paeony in systemic lupus erythematosus: a systematic review and meta-analysis. Medine (Baltimore)101, e32029. https://doi.org/10.1097/md.0000000000032029 (2022).
Kandane-Rathnayake, R. et al. Independent associations of lymphopenia and neutropenia in patients with systemic lupus erythematosus: a longitudinal, multinational study. Rheumatology (Oxford)60, 5185–5193. https://doi.org/10.1093/rheumatology/keab217 (2021).
Chen, Y. F. et al. Inflammatory anemia may be an indicator for predicting disease activity and structural damage in Chinese patients with rheumatoid arthritis. Clin. Rheumatol.39, 1737–1745. https://doi.org/10.1007/s10067-019-04873-y (2020).
Moreno-Torres, V. et al. Usefulness of the hemogram as a measure of clinical and serological activity in systemic lupus erythematosus. J. Transl. Autoimmun.5, 100157. https://doi.org/10.1016/j.jtauto.2022.100157 (2022).
Yu, J. et al. Neutrophil-to-C3 ratio and neutrophil-to-lymphocyte ratio were associated with disease activity in patients with systemic lupus erythematosus. J. Clin. Lab. Anal.33, e22633. https://doi.org/10.1002/jcla.22633 (2019).
Huang, Y. et al. Evaluation of systemic lupus erythematosus disease activity using anti-α-enolase antibody and RDW. Clin. Exp. Med.21, 73–78. https://doi.org/10.1007/s10238-020-00657-w (2021).
Soliman, W. M., Sherif, N. M., Ghanima, I. M. & El-Badawy, M. A. Neutrophil to lymphocyte and platelet to lymphocyte ratios in systemic lupus erythematosus: relation with disease activity and lupus nephritis. Reumatol. Clin. (Engl. Ed.). 16, 255–261. https://doi.org/10.1016/j.reuma.2018.07.008 (2020).
Ruchakorn, N. et al. Performance of cytokine models in predicting SLE activity. Arthritis Res. Ther.21, 287. https://doi.org/10.1186/s13075-019-2029-1 (2019).
Ayano, M. & Horiuchi, T. Complement as a biomarker for systemic lupus erythematosus. Biomolecules13https://doi.org/10.3390/biom13020367 (2023).
Huang, J. J., Mao, T. J., Zhang, Z. Y. & Feng, G. Systemic evaluation of lymphocyte-bound C4d and immunoglobulins for diagnosis and activity monitoring of systemic lupus erythematosus. Clin. Biochem.118, 110600. https://doi.org/10.1016/j.clinbiochem.2023.110600 (2023).
Lou, H., Ling, G. S. & Cao, X. Autoantibodies in systemic lupus erythematosus: from immunopathology to therapeutic target. J. Autoimmun.132, 102861. https://doi.org/10.1016/j.jaut.2022.102861 (2022).
Aringer, M. Inflammatory markers in systemic lupus erythematosus. J. Autoimmun.110, 102374. https://doi.org/10.1016/j.jaut.2019.102374 (2020).
Wang, J. et al. The diagnostic values of C-reactive protein and procalcitonin in identifying systemic lupus erythematosus infection and disease activity. Medicine (Baltimore)98, e16798. https://doi.org/10.1097/md.0000000000016798 (2019).
Acknowledgements
We extend our gratitude to Xialin Wang and Yuming Cheng from Beckman Coulter Commercial Enterprise (China) Co. Ltd., Shanghai, China, for their invaluable technical assistance with the construction of the predictive model.
Funding
This work was supported by the Natural Science Foundation of Hunan Province of China (no. 2023JJ40981).
Author information
Authors and Affiliations
Contributions
Juan Zhao: Methodology, Data curation, Visualization, Writing – original draft. Wanchan Peng: Methodology, Data curation. Formal analysis, Software. Siyu Wu: Methodology, Data curation, Validation, Supervision. Wei Wang: Conceptualization, Resources, Project administration, Writing – review & editing. All authors contributed to the article and approved the submitted version. Juan Zhao and Wanchan Peng contributed equally to this work and share frst authorship.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, J., Peng, W., Wu, S. et al. Evaluation of disease activity in systemic lupus erythematosus using standard deviation of lymphocyte volume combined with red blood cell count and lymphocyte percentage. Sci Rep 14, 22470 (2024). https://doi.org/10.1038/s41598-024-72977-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-72977-w
Keywords
This article is cited by
-
MS-YOLO: a multi-scale model for accurate and efficient blood cell detection
Pattern Analysis and Applications (2026)