Abstract
Evaluate the real-world effectiveness and safety of different treatment regimens for treatment-naïve high viral load chronic hepatitis B (CHB) patients. Between January 2021 and August 2022, CHB patients with HBV DNA ≥ 107 IU/mL were collected from four medical centers in Shenzhen. Patients treated with mono or combine antiviral therapy. The primary endpoint was the cumulative incidence of virological response at 48 weeks, and other endpoints included changes in HBsAg, HBeAg, ALT, and eGFR at 48 weeks. We used propensity score-based inverse probability of treatment weighting (IPTW) to balance the bias. Weighted logistics regression was used to estimate the factors affecting virological response. A total of 391 patients were included in the study, with 296 patients undergoing statistical analysis after IPTW. The patients were distributed into four groups: ETV (n = 62), TDF (n = 89), TAF (n = 36), TDF + LdT/ETV (n = 109). The 48-week cumulative incidence of virological response was significantly lower in ETV group (52.3%) compared to TDF (71.7%), TAF (74.2%), and TDF + LdT/ETV groups (77.9%) (P < 0.05). There were no significant differences in HBsAg loss among the four groups, but the HBeAg seroconversion rate was significantly higher in the TAF group. The ALT normalization rate was significantly higher in the TAF group (72.2%) compared to the others at 48 weeks (P < 0.05). In treatment-naïve CHB patients with high viral load, combination therapy was not superior to TDF or TAF monotherapy in virological response. Patients treated with TDF or TAF showed superior virological response compared to those treated with ETV. The TAF group demonstrated superiority in terms of ALT normalization and HBeAg seroconversion.
Similar content being viewed by others
Background
Hepatitis B virus (HBV) infection is an important global health problem, and standardized antiviral therapy for chronic hepatitis B (CHB) having been implemented for over 18 years in China1. The main goal of HBV therapy is to decrease the risk of cirrhosis, liver failure, and hepatocellular carcinoma2,3. With in-depth research on HBV antiviral therapy and the development of various nucleos(t)ide analogues (NAs), expanding antiviral therapy is imperative. Entecavir (ETV), tenofovir disoprpxil fumarate (TDF), and tenofovir alafenamide (TAF) are the recommended first-line HBV regimens due to high efficacy in suppressing HBV replication4,5,6.
However, CHB patients with high viral loads may be in an ‘immune-tolerant’, which may face challenges with antiviral treatment and have the risk of low-level viremia7. Scholars have attempted combination antiviral regimens to improve virological response rates8,9, LdT and TDF recommended by the American Association for the Study of Liver Diseases (AASLD) for high viral load cases, particularly in late pregnancy10. Notably, several studies have suggested a beneficial impact of telbivudine (LdT) on estimated glomerular filtration rate (eGFR) in CHB patients11,12. TDF + LdT/ETV combination therapy as a means to improve the efficacy and safety in CHB management has garnered attention13,14,15. While some studies have the opposite conclusion, combination therapy showed similar virological response compared to monotherapy in CHB patients16. Currently, there is an ongoing debate in clinical practice and ongoing research that compares the efficacy and safety of monotherapy with combination therapy. This study aims to investigate the real-world advantages and drawbacks of initial antiviral therapy regimens for high viral load CHB patients.
Methods
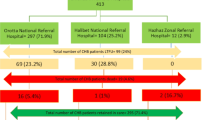
Between January 2021 and August 2022, 1350 CHB patients with HBV DNA ≥ 107IU/mL were drawn from four medical centers, including Shenzhen Nanshan People’s Hospital, Shenzhen Longhua District People’s Hospital, Shenzhen Hospital of Integrated Traditional Chinese, and Western Medicine, and Shenzhen Qianhai Shekou Free Trade Zone Hospital. 391 cases ultimately met the inclusion criteria (Fig. 1).
Ethics approval
The institutional review board of Shenzhen Nanshan People’s Hospital, Shenzhen, Guangdong, China approved the study. The accession numbers for this study are: KY-2024-003-001. All participants gave a written informed consent. The investigation conforms with the principles outlined in the Declaration of Helsinki.
Study population and variables
In our study, Participants who did not meet the criteria for analysis were excluded: (1) patients treated with nucleos(t)ide analogues; (2) patients with coinfection (hepatitis A, hepatitis C, hepatitis E, human immunodeficiency virus or/and other viral infections; (3) combined with drug-induced liver injury, alcoholic hepatitis, autoimmune liver disease, systemic disease involving the liver and other disease; (4) those who have used immunosuppressants; (5) those who have used interferon; (6) cirrhosis or hepatocellular carcinoma at baseline; (6) or pregnancy. We enrolled male or female participants (aged 18–60 years) with CHB (HBsAg positive > 6 months), high viral load (HBV DNA ≥ 107IU/ml) and initial nucleos(t)ide analogue. During the follow-up period, 132 patients were not stable dose NAs or discontinue NAs, 40 patients who switching from one treatment to other NAs (8 cases with ETV, 3 cases with TAF, 21 cases with TDF + LdT/ETV, 8 cases with TDF), and 82 patients were not complete data.
Treatment-naïve regimens
Treatment-naïve monotherapy regimens include: ETV 0.5 mg: Entecavir Dispersible Tblets, Suzhou Dawnrays Pharmaceutical Co., Ltd.; Baraclude, Bristol Myers Squibb. TDF 300 mg: Qilu Pharmaceutical Co., Ltd.; GlaxoSmithKline, Brentford, UK; Tenofovir TAF 25 mg: Qilu Pharmaceutical Co., Ltd.; Gilead (Patheon Inc). Combination regimens include: TDF + LdT/ETV (Telbivudine 600 mg, Mylan N.V.).
Demographic and clinical data collection
Demographic and clinical data of the study subjects were collected, including age, gender, HBV DNA, hepatitis B surface antigen (HBsAg), hepatitis B virus e antigen (HBeAg), alanine aminotransferase (ALT), and estimated glomerular filtration rate (eGFR) at baseline and follow-up at 12, 24, 36, and 48 weeks. HBV DNA quantitative detection reagent (30 − 5 × 109IU/ml) was provided by Hunan Shengxiang Company, and the detection instrument was ABI7500 fluorescence quantitative polymerase chain reaction (PCR) instrument. The HBV serum marker detection instrument was Abbott i2000SR automatic microparticle chemiluminescence immunoassay analyzer, and the detection reagent was provided by Abbott Company of the United States. The biochemical testing instrument was Abbott ARCHITECT c16000 automatic biochemical analyzer, and the detection reagent was provided by Abbott Company of the United States. ALT levels are expressed in absolute values (U/L) (7–40 U/L) and the above biochemical, hematological and virological tests and analyses are performed by the four central diagnostic laboratories in accordance with Good Laboratory Practice. eGFR according to the formula (140-age) * body weight * 1.23 (* 1.03 women) / serum creatinine17. According to the American Association for the Study of Liver Diseases (AASLD) guidelines for hepatitis, CHB is defined as serum HBsAg positive for six months or more4.
Outcomes
The primary endpoint was the cumulative incidence of virological response (HBV DNA < 100 IU/ml) at week 48, and secondary endpoints were (1) change from baseline in HBV DNA levels at 48 weeks; (2) HBsAg loss after NAs therapy during the follow-up period of 48 weeks; (3) HBeAg seroconversion rate during the follow-up period of 48 weeks; (4) ALT normalization rate and eGFR levels change during the follow-up period 48 weeks.
Statistical analysis
The single-sample Kolmogorov-Smirnov test is used for the continuous variables, which are expressed by means and standard deviation (SD) or medians and interquartile ranges (IQRs). The Kruskal-Wallis H rank-sum test is used for comparing multiple groups. Categorical variables are presented as percentages, and chi-square test is used for comparing between groups. Inverse probability of treatment weighting(IPTW)18was used to balance the characteristics at baseline among the four groups. Specially, the propensity of being among the four groups was estimated through a logistic regression model that included covariates such as age > 30, gender, the proportion of HBeAg negative, and baseline ALT levels. Subsequently, the propensity score (PS) was used to individually weigh each patient by the inverse probability of covariates and balance observable characteristics. Standardized mean difference (SMD) is most commonly used after PS matching to assess balancing of parameter distribution19. SMD ≥ 0.2 were regarded as showing marked difference among treatment groups20. Cumulative probabilities were estimated using Kaplan–Meier analysis and compared between groups using the log-rank test. Univariate and multivariable logistics regression analysis is used to analyze the factors influencing virological response. A two-tailed P value < 0.05 was statistically significant. SPSS 26.0 (version 26.0; IBM Corp., Armonk, NY, USA), GraphPad Prism (version 8.0; GraphPad, San Diego, CA, USA) and R (version 4.4.1) statistical software were used to analyze the data.
Results
Baseline characteristics of patients
The study enrolled a total of 1350 CHB patients with high viral load and ultimately 391 patients were tested. Patients were divided into four groups based on different antiviral treatment regimens: ETV group with 80 cases, TDF group with 128 cases, TAF group with 53 cases, and combination therapy group (TDF + LdT/ETV) with 130 cases (TDF + LdT 82 cases, TDF + ETV 48 cases). There appear to be significant differences among the four groups in age, the proportion of HBeAg negative, and baseline ALT before IPTW (P < 0.05) (Supplementary Table S1). All variables were well-balanced with SMD < 0.2 after IPTW adjustment, and 296 patients were applied in the statistical analysis, 62, 89, 36 and 109 patients received ETV, TDF, TAF, and TDF + LdT/ETV groups, respectively (Supplementary Fig. 1). The baseline characteristics of the patients after IPTW are shown in Table 1. No significant differences in age, gender, ALT level, the proportion of HBeAg negative were observed among the groups.
Comparison of virological response among different treatment regimens in CHB patients after IPTW
There were statistically significant differences in the cumulative virologic response rates among the groups at 48 weeks. The 48-week cumulative virologic response rates were 52.3%, 71.7%, 74.2%, and 77.9% for the ETV, TDF, TAF, and TDF + LdT/ETV groups, respectively (log-rank = 11.09, P = 0.011) (Fig. 2A). In the ETV group, the mean HBV DNA levels at 12, 24, 36, 48 weeks were 3.88, 2.69, 2.19, 1.77 log10 IU/mL, respectively. And in the TDF + LdT/ETV group, the mean HBV DNA levels at 12, 24, 36, 48 weeks were 3.16, 1.65, 0.97, 0.61log10 IU/mL, respectively. At weeks 12, 24, 36, and 48, the HBV DNA levels was significant difference among the four groups (all P < 0.05) (Fig. 2B). The decline in HBV DNA from baseline to 48 weeks was as follows: -7.62 log10 IU/mL in TDF + LdT/ETV group, -6.67 log10 IU/mL in the ETV group, -7.44 log10 IU/mL in the TDF group, and − 7.24 log10 IU/mL in the TAF group. ETV group had lower reduction compared to the other groups (P < 0.05), while no significant difference was observed between the latter(P > 0.05) (Fig. 2C).
Changes of HBV DNA in different antiviral regimens during the follow-up period. (A) the cumulative incidence of virological response (HBV DNA < 100 IU/ml) during the follow-up (B) change in HBV DNA decline in different time periods (C) change from baseline in HBV DNA levels at week 48. * P < 0.05 ** P < 0.01 *** P < 0.0001.
Changes in immunological indicators after IPTW
At 48 weeks, there was no significant difference in HBsAg loss among the four groups (P > 0.05) (Fig. 3A). The mean HBsAg levels was 3.48, 3.67, 3.53, and 3.5 log10 IU/mL in the TDF + LdT/ETV, ETV, TDF, and TAF groups, respectively. Due to differences in HBeAg detection methods between the four medical centers, it was not possible to precisely quantify the statistical data. Therefore, the proportion of HBeAg seroconversion was used to access the efficacy of each treatment regimen. No differences were founded at 12, 24, and 36 weeks (P > 0.05). At 48 weeks, the HBeAg seroconversion rate in the ETV, TDF, TAF and TDF + LdT/ETV groups were 12.9%, 12.4%, 16.7%, and 2.8%, respectively. The TAF group showed a statistically significant advantage compared to the other three groups (P < 0.05) (Fig. 3B).
Comparison of ALT and eGFR changes among different treatment regimens after IPTW
According to the Expert Opinion on expanding anti-HBV treatment for chronic hepatitis B, the normal threshold for ALT is 30 U/L for men and 19 U/L for women21. Four groups demonstrated significant difference in ALT renormalization at 12, 36, and 48 weeks(P < 0.05) (Fig. 4A). At 48 weeks, the ALT normalization rate of TAF group was 72.2%, which superior to TDF group (50.6%) and TDF + LdT/ETV group (45%) (P < 0.05) (Fig. 4B). With regards to the safety implications of antiviral therapy, eGFR was selected based on previous study on adverse events related to NAs22. After 48 weeks of follow-up, there was no significant decrease in eGFR compared to the baseline across the four groups, and there were no significant statistical differences among the groups (P > 0.05) (Fig. 4C).
Factors associated with virological response in treatment-naïve patients after IPTW
After IPTW, the factors influencing the virologic response of treatment-naïve patients with high viral load were analyzed. Univariate and multivariate logistic regression analyses were performed, incorporating variables such as age, gender, baseline ALT stratification, HBeAg positive at baseline, HBV DNA levels, HBsAg levels, and antiviral treatment regimens. Multivariate analysis revealed that baseline ALT1 ~ 2ULN (OR 0.267, 95%CI 0.144–0.493), baseline ALT < 1ULN (OR 0.343, 95%CI 0.131–0.897) and baseline HBV DNA levels (OR 0.285, 95%CI 0.147–0.554) were the factors influencing virological response (all P < 0.05). Furthermore, the virologic response was lower in the ETV group compared to the other groups (OR 0.348, 95%CI 0.129–0.937, P = 0.037). However, there was no statistically significant difference in the effect of baseline HBsAg levels on the 48-week virologic response (P > 0.05) (Table 2).
Discussion
Recent evidence has increasingly demonstrated the effectiveness of expanding the indications for antiviral therapy in CHB patients21,23. First-line oral antiviral agents such as ETV, TDF, and TAF have demonstrated the efficacy of high viral suppression5,24. The primary therapeutic goal is the sustained suppression of HBV DNA by antiviral therapy25. However, CHB patients who are HBeAg positive with high viral load face the risk of low-level viremia due to the high viral barrier26. Previous studies showed TDF + ETV/LdT combination therapy had superior antiviral efficacy compared to TDF monotherapy in the treatment of CHB13,15. Conversely, Cho et al.27found no significant difference between TDF monotherapy and TDF + NAs combination therapy. To determine the most beneficial agents for CHB patients, this study compared antiviral response among treatment groups including TDF + LdT/ETV, ETV, TDF, and TAF.
This study aims to explore the efficacy of first-line antiviral therapy in patients with high viral load over a 48-week period. IPTW was employed to balance the clinical characteristics of the four groups. At 48 weeks, the virological response in the ETV group (52.3%) was found to be inferior compared to the TDF + LdT/ETV group (77.9%), TDF group (71.7%) and TAF group (74.2%) (all P < 0.05). Conversely, TDF + LdT/ETV combination therapy showed comparable virological response to TDF monotherapy and TAF monotherapy (P > 0.05). Previous research reported that the efficacy of ETV plus TDF therapy surpasses that of ETV monotherapy, particularly in patients with HBV DNA exceeding 108 IU/mL at baseline (79% vs. 62%)28. Lee et al.29 similarly indicated that TDF + ETV group achieved superior virologic response than TDF group. Moreover, it was slightly better and more homogeneous in TDF + LdT combination treatment group than in the TDF or LdT monotherapy in the previous study30. Combination therapy may appears to offer a greater degree of HBV DNA inhibition compared with monotherapy31.However, Other studies also have reported that TDF monotherapy provided virological response comparable to that of TDF + ETV combination therapy16,32. In this study, we analyzed the factors related to the virologic response in CHB patients, including baseline HBV DNA and ALT levels. Specifically, ETV was identified as a factor associated with virological response (OR 0.348, 95%CI 0.129–0.937, P = 0.037). It is evident that ETV may not be the primary treatment choice for patients with high viral loads.
This study aimed to evaluate the effectiveness of antiviral regimens in CHB patients, focusing on endpoints such as HBsAg loss and HBeAg seroconversion rates over a 48-week treatment duration. And IPTW was utilized to achieve balanced bias among the four groups. Previous study has highlighted the efficacy of TDF plus LdT therapy compared to monotherapy for achieving HBsAg loss33. Similarly, studies indicated that HBsAg decline on LdT has been comparable to PegIFN-a3. In our study, there was no significant differences in HBsAg loss among the four groups over a 48-week period (P > 0.05). At the end of the 48-week follow-up period, HBeAg seroconversion rate in the TAF group (16.7%) was superior to that in the other three groups (ETV:12.9%, TDF:12.4%, TDF + LdT/ETV:2.8%) (P < 0.05). Additionally, the TAF group showed a significantly elevated proportion of ALT normalization compared to both monotherapy and combination therapy(P < 0.05). This finding is consistent with conclusions drawn from previously published global phase III clinical trials of TAF6. For the renal damage, earlier studies reported LdT had a slightly increase in eGFR after 2-year treatment, whereas TDF group had a decline34. There was no significant change in markers of renal damage in the four groups (P > 0.05). This change may be related to the relatively short observation period of 48 weeks.
Our study has the following limitations. First, this multicenter study reveals incomplete data about liver stiffness measurement or the FIB-4 index, potentially limiting the comprehensive analysis. Future follow-up study will incorporate these. Second, high-sensitivity HBV DNA testing was not conducted across all participants, this study may exhibit low level viremia. Third, regarding the cost-effectiveness of antiviral treatment, not all patients underwent bone mineral density testing, which limits the comprehensive of drug safety. Finally, this study collected clinical data from four centers, and Regional observational studies are susceptible to bias due to variations in patient enrollment criteria across participating centers, which may introduce sampling errors.
Conclusion
In the treatment-naïve CHB patients with high viral load, combination therapy was not superior to TDF monotherapy or TAF monotherapy. Patients treated with TDF or TAF showed superior virological response compared to those treated with ETV. And the TAF group demonstrated superiority in terms of ALT normalization and HBeAg seroconversion.
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding author.
References
The guideline of prevention. And treatment for chronic hepatitis B [J]. Chin. J. Clini Hepatol., (01): 3–15 (2006).
Oncology, C. S. O. C. Guidelines for Diagnosis and Treatment of Primary Liver Cancer (2020 Edition) [J]. (2020).
EASL. Clinical Practice Guidelines on the management of hepatitis B virus infection [J]. J Hepatol, 2017, 67(2): 370 – 98.DOI: (2017). https://doi.org/10.1016/j.jhep.2017.03.021
Terrault, N. A. et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance [J]. Hepatology. 67 (4), 1560–1599. https://doi.org/10.1002/hep.29800 (2018).
Chan, H. L. Y. et al. Long-term treatment with Tenofovir Alafenamide for Chronic Hepatitis B results in high rates of viral suppression and favorable renal and bone safety [J]. Am. J. Gastroenterol.119 (3), 486–496. https://doi.org/10.14309/ajg.0000000000002468 (2024).
Agarwal, K. et al. 96 weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection [J]. J. Hepatol.68 (4), 672–681. https://doi.org/10.1016/j.jhep.2017.11.039 (2018).
Zhang, Q. et al. Low-level viremia in nucleoside analog-treated chronic hepatitis B patients [J]. Chin. Med. J. (Engl). 134 (23), 2810–2817. https://doi.org/10.1097/CM9.0000000000001793 (2021).
Lim, Y-S. et al. Tenofovir monotherapy versus tenofovir and entecavir combination therapy in patients with entecavir-resistant chronic hepatitis B with multiple drug failure: results of a randomised trial [J]. Gut. 65 (5), 852–860. https://doi.org/10.1136/gutjnl-2014-308353 (2016).
Lim, S. G. et al. The scientific basis of combination therapy for chronic hepatitis B functional cure [J]. Nat. Rev. Gastroenterol. Hepatol.20 (4), 238–253. https://doi.org/10.1038/s41575-022-00724-5 (2023).
Terrault, N. A. et al. AASLD guidelines for treatment of chronic hepatitis B [J]. Hepatology. 63 (1), 261–283. https://doi.org/10.1002/hep.28156 (2016).
Gane, E. J. et al. Telbivudine improves renal function in patients with chronic hepatitis B [J]. Gastroenterology. 146 (1). https://doi.org/10.1053/j.gastro.2013.09.031 (2014).
Mak, L-Y. et al. In Vitro and in vivo Renoprotective effects of Telbivudine in Chronic Hepatitis B patients receiving Nucleotide Analogue [J]. Dig. Dis. Sci.64 (12), 3630–3641. https://doi.org/10.1007/s10620-019-05717-0 (2019).
Wang, Y-H. et al. Tenofovir monotherapy versus tenofovir plus entecavir combination therapy in HBeAg-positive chronic hepatitis patients with partial virological response to entecavir [J]. J. Med. Virol.92 (3), 302–308. https://doi.org/10.1002/jmv.25608 (2020).
Woo, H. Y. et al. Entecavir + tenofovir vs. lamivudine/telbivudine + adefovir in chronic hepatitis B patients with prior suboptimal response [J]. Clin. Mol. Hepatol.26 (3), 352–363. https://doi.org/10.3350/cmh.2019.0044n (2020).
Wu, Z-X. et al. Tenofovir and telbivudine combination therapy rapidly decreases viral loads in immune-tolerant chronic hepatitis B patients awaiting assisted reproduction: an open-label, randomized, controlled study [J]. Eur. J. Gastroenterol. Hepatol.31 (7), 832–835. https://doi.org/10.1097/MEG.0000000000001345 (2019).
Lim, Y-S. et al. Tenofovir monotherapy versus tenofovir and entecavir combination therapy in adefovir-resistant chronic hepatitis B patients with multiple drug failure: results of a randomised trial [J]. Gut. 65 (6), 1042–1051. https://doi.org/10.1136/gutjnl-2014-308435 (2016).
Shuai, F. & Xiao-Ning, L. The research development of formulas for calculating glomerular filtration rate:from Cockcroft-Gault formula to full age spectrum (FAS) formula [J]. J. Clin. Nephrol.20 (01), 73–77 (2020).
Austin, P. C. & Stuart, E. A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies [J]. Stat. Med.34 (28), 3661–3679. https://doi.org/10.1002/sim.6607 (2015).
Zhang, Z. et al. Balance diagnostics after propensity score matching [J]. Ann. Transl Med.7 (1), 16. https://doi.org/10.21037/atm.2018.12.10 (2019).
Jacob, C. Statistical Power Analysis for the Behavioral Sciences [J] (Lawrence Erlbaum Associates, 1988).
Expert opinion on expanding anti-HBV treatment for chronic hepatitis B [J]. Zhonghua Gan Zang Bing Za Zhi, 30(2): 131–136. DOI:https://doi.org/10.3760/cma.j.cn501113-20220209-00060 (2022).
Chan, H. L. Y. et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of HBeAg-positive chronic hepatitis B virus infection: a randomised, double-blind, phase 3, non-inferiority trial [J]. Lancet Gastroenterol. Hepatol.1 (3), 185–195. https://doi.org/10.1016/S2468-1253(16)30024-3 (2016).
Zhang, S. et al. Cost-effectiveness of expanded antiviral treatment for chronic hepatitis B virus infection in China: an economic evaluation [J]. Lancet Reg. Health West. Pac.35, 100738. https://doi.org/10.1016/j.lanwpc.2023.100738 (2023).
Chien, R. N. & Liaw, Y. F. Current Trend in Antiviral Therapy for Chronic Hepatitis B [J]. Viruses. 14 (2). https://doi.org/10.3390/v14020434 (2022).
You, H. et al. Guidelines for the Prevention and Treatment of Chronic Hepatitis B (version 2022) [J]. J. Clin. Transl Hepatol.11 (6), 1425–1442. https://doi.org/10.14218/JCTH.2023.00320 (2023).
Fengming, L., Bo, F. & Suzhen, Z. Current status of the research on low-level viremia in chronic hepatitis B patients receiving nucleos(t)ide analogues [J]. J. Clin. Hepatol.37 (6), 1268–1274. https://doi.org/10.3969/j.issn.1001-5256.2021.06.007 (2021).
Cho, H. J. et al. Tenofovir-based rescue therapy in chronic hepatitis B patients with suboptimal responses to adefovir with prior lamivudine resistance [J]. J. Med. Virol.87 (9), 1532–1538. https://doi.org/10.1002/jmv.24201 (2015).
Lok, A. S. et al. Efficacy of entecavir with or without tenofovir disoproxil fumarate for nucleos(t)ide-naïve patients with chronic hepatitis B [J]. Gastroenterology. 143 (3). https://doi.org/10.1053/j.gastro.2012.05.037 (2012).
Lee, S. et al. Tenofovir versus tenofovir plus entecavir for chronic hepatitis B with lamivudine resistance and entecavir resistance [J]. J. Viral Hepat.24 (2), 141–147. https://doi.org/10.1111/jvh.12623 (2017).
Leung, N. W. Y. et al. Early viral kinetics with Telbivudine, tenofovir or combination of both in Immunotolerant patients with Hepatitis B E Antigen-positive chronic Hepatitis B [J]. Infect. Dis. Ther.3 (2), 191–202. https://doi.org/10.1007/s40121-014-0039-5 (2014).
Terrault, N. A. Benefits and risks of combination therapy for hepatitis B [J]. Hepatology. 49 (5 Suppl), S122–S8. https://doi.org/10.1002/hep.22921 (2009).
Shang, J. et al. Efficacy of different nucleoside analog rescue therapies for entecavir-resistant chronic hepatitis B patients [J]. BMC Infect. Dis.21 (1), 912. https://doi.org/10.1186/s12879-021-06554-1 (2021).
Jindal, A. et al. A randomized open label trial of tenofovir monotherapy versus tenofovir plus telbivudine in spontaneous reactivation of hepatitis B [J]. Saudi J. Gastroenterol.25 (5), 319–326. https://doi.org/10.4103/sjg.SJG_537_18 (2019).
Tsai, M. C. et al. Does Nucleos(t)ide Analogues Treatment affect renal function in Chronic Hepatitis B patients who have already decreased eGFR? A longitudinal study [J]. PLoS One. 11 (3), e0149761. https://doi.org/10.1371/journal.pone.0149761 (2016).
Author information
Authors and Affiliations
Contributions
Concept and design of the study (QY, XW), acquisition of the data (Cm J, Rs F, Sl L, QY), analysis and interpretation of the data (XW), drafting of the manuscript (XW, QY), and critical revision of the manuscript for important intellectual content (XW, QY). All authors made significant contributions to this study and have approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
This research was approved by the ethics Committee of Shenzhen Nanshan People’s hospital (number: KY-2024-003-01), and patients are exempted from informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, X., Yan, Q., Jiang, C. et al. Real-world study on the efficacy and safety of different treatment regimens in treatment-naïve CHB patients with high viral load. Sci Rep 14, 21656 (2024). https://doi.org/10.1038/s41598-024-72986-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72986-9