Abstract
To analyze the prevalence and influencing factors of myopia among children and adolescents in Hangzhou city, and provide ideas for the formulation of myopia prevention and control measures. A cross-sectional school-based study using stratified cluster random sampling method was used to select 31,880 students from 113 schools in Hangzhou city. Myopia screening and questionnaires on the influencing factors of poor visual acuity were carried out. Univariate and multivariate logistic regression were used to screen possible risk factors of myopia. The overall prevalence of myopia was found to be 55.3% (17,630/31,880), with the myopia rates observed among students in kindergarten, primary school, junior high school, and senior high school, at 5.8%, 34.9%, 74.2%, and 85.0%, respectively. As the academic year progresses, there has been an observable increase in the prevalence of myopia (χ2 = 8676.748, P<0.001), low myopia (χ2 = 5444.040, P<0.001) and high myopia (χ2 = 2171.073, P<0.001) among students, with the difference between the three groups being statistically significant. The myopia prevalence in girls is higher than that in boys (χ2 = 119.917, P<0.001); the prevalence of myopia in urban students is higher than that in suburban students (χ2 = 4.603, P = 0.032). The time spent on homework after school, the correctness of reading and writing postures, the duration of exposure to electronic screens, and the use of lighting in an appropriate manner all have an impact on the development of myopia (all P<0.05). The overall prevalence of myopia and high myopia in schools in eastern China, is notably high. The prevalence of myopia and high myopia increases with grade or age. Myopia is associated with increased age, parental myopia, extended periods of homework after school, poor reading and writing posture, prolonged exposure to electronic screens and inappropriate lighting. In light of the findings of the present survey, it is recommended that a comprehensive prevention and control intervention model for myopia in children and adolescents based on society-hospital-school-family-individual students with a view to preventing and controlling myopia.
Similar content being viewed by others
Introduction
In recent years, the prevalence of myopia has been increasing worldwide, reaching a point where it has become a significant global public health concern1. Significant ethnic and geographic differences are evident in the distribution of myopia prevalence2. The prevalence of myopia is increasing every year, with a younger and more severe trend, and young people aged 10–25 years are the fastest growing myopia population3. Many East and Southeast Asian countries are particularly affected, such as China (37.7%)4. In China, the myopic population reached 750 million in 2020, accounting for about 47% of the total Chinese population. Among them, the overall prevalence of myopia in children and adolescents was 53.6%, and the overall prevalence of myopia in college students exceeded 90%1,5. In contrast, the lowest prevalence is seen in black Africans, with a figure of 4.7%6. White Europeans exhibit an intermediate prevalence, with figures reaching 13.4% in Norway7, 11.4% in Germany8, and 19.9% in Ireland9. The prevalence of myopia in East Asians has increased by 23% over the past decade, with a slow increase in the prevalence of myopia in South Asians and minimal change in the prevalence of myopia in whites10. It is expected that by 2050, the global myopic population will reach 4.758 billion, or about 50% of the total population, and the number of people with high myopia will reach 938 million (about 9.8%)3.
Public health interventions are needed to help stem the growing myopia epidemic. Additionally, the pathological myopia prevalence was also increasing over the years. Early detection and potential myopia control treatments are essential to prevent the progression to pathological myopia11. Understanding risk factors is crucial for formulation of preventive measures. Although genetic factors play a role in the development of myopia, the rapid growth in prevalence is likely attributable to environmental and lifestyle factors3. Prior studies have demonstrated an association between myopia and near-work activities such as studying, reading, outdoor activities, and screen time among children12,13. However, among the above factors, only the causal relationship between education and outdoor activity time and the occurrence of myopia in school-aged children has been confirmed11, and other factors still need to be further validated by high-quality studies and clinical randomized trials.
Currently, large-scale studies investigating the influence of lifestyle and learning factors on myopia incidence and progression in children are limited. This study evaluates the prevalence and risk factors for myopia in paediatric patients in a large, diverse and real-world population in eastern China to provide direction and theoretical basis for the development of myopia interventions in children and adolescents and to reduce the social and economic burden of the disease.
Methods
Study population
This is a school-based cross-sectional study that employs a stratified whole cluster random sampling method. The study was conducted among all 13 districts and counties in Hangzhou city from September to November 2021. A total of eight or nine educational institutions were selected from each district and county, comprising two kindergartens, two primary schools, two junior high schools, and two to three senior high schools. The distribution of selected schools is provided in Fig. 1. Primary education lasts for six years, junior high for three years and senior high for three years. In the kindergarten phase, children aged 5.5 to 6.5 years old in the larger class were selected. In the primary, junior high and senior high school phases, surveys were conducted by class. Three classes of students were randomly selected from each grade to participate in this study, with a minimum of 80 students per grade. Those diagnosed with eye diseases such as leukoplakia, cataracts, glaucoma and retinal disease were excluded. This dataset is the original data collected by the researcher’s team. The final effective sample size of the survey is 31,880 (5 students were excluded due to missing gender information), including 2,212 kindergarten children, 13,900 primary school students, 6,984 junior high school students, and 8,784 senior high school students.
Ethical clearance
The study adhered to the tenets of the Declaration of Helsinki, and was approved by the Medical Ethics Committee of Hangzhou Centre for Disease Control and Prevention (approval no. Declared 2019-17). Ophthalmology formally requests approval in writing, detailing the study objectives and procedures, and obtaining consent from the local education board to conduct the study in schools. Prior to the commencement of the study, verbal informed consent was obtained from all participants and their parents. In the case of a child under 12 years of age, the consent form was signed by the child’s parents. In the case of children aged 13 and above, the consent form was signed by both the child and their parents. The participants and their parents were provided with a comprehensive explanation of the study’s objectives and methodology. At any point, participants were permitted to withdraw from the research without providing justification to the investigators. The confidentiality of individual research data has been maintained by the investigators, and the data have been de-identified prior to analysis.
Methodology and criteria for the identification of myopia
All selected students were examined for visual acuity (VA) and refraction, according to the “Children and Adolescents Myopia Screening Standards” recommended by the National Health Commission of the People’s Republic of China in 201814. The VA of all students was evaluated without refractive correction, employing a logarithmic far visual acuity chart with a 5-point recording at a distance of 5 m14. Binocular refraction was measured by an ophthalmologist using an automated computer refractometer (TOPCN) in a non-cycloplegic state. Each eye was measured three times and averaged, and the sphere (S), cylinder (C), and axis were recorded. Spherical equivalent (SE) was sphere + 1/2cylinder15. As the refractive error was measured using a non-cycloplegic autorefractor, which has been demonstrated to overestimate the magnitude of myopia, at the same time, with reference to the work of the International Myopia Institute (IMI), we finally defined myopia using a combination of SE and VA16,17,18. In the present study, myopia was defined as VA<5.0 and SE≤-0.5 diopters (D) in at least one eye. Additionally, students who wore orthokeratology were classified as the myopic population. Further, low myopia was defined as VA<5.0 and − 6.00D< SE≤-0.5D in at least one eye, high myopia was defined as VA<5.0 and SE≤-6.00D in at least one eye.
Questionnaire surveys
Using evidence from the literature19,20,21,22,23, we designed a questionnaire to identify the associated risk factors of myopia. To test the questionnaire, a total of 120 students were selected for the study from grades 4, 5, and 6 of primary school, grades 1, 2, and 3 of middle school, and grades 1, 2, and 3 of high school, which were not included in the study. The students were asked to give feedback on how well the questionnaire was understood and how easy it was to fill out. The final version of the questionnaire was also determined by combining expert opinion and parental opinion.
The questionnaire encompassed 42 items across eight dimensions, including general information (gender, grade, ethnic group), the environment in which eyes are used at school (desk and chair transfers, eye exercises, activity sites), the context in which eyes are used outside of school (time spent doing homework, attending tutorial classes, etc.), posture when reading and writing (when reading and writing, 10 cm from the chest to the table, 33 cm from the eye to the book and 3.3 cm from the tip of the pen to the finger), the usage of electronic screens (television and computer game consoles), the habit of using the eyes at close distance (reading a book while travelling on public transport, light intensity, etc.), the situation of outdoor activities and sleep, and the situation of myopia inspection and correction. The original questionnaire has been included in the supplementary material for further examination. Students who had undergone vision screening in grades 4, 5 and 6 of primary school, grades 1, 2, 3 of middle school students and grades 1, 2, 3 of high school students in two districts (Shangcheng district and Gongshu district) and two counties (Jiande county and Chunan county) participate in the questionnaire.
Quality control
The investigators underwent uniform training prior to the fieldwork. This training enabled them to gain a full understanding of the content of the questionnaires and the instructions for completing them. Questionnaires were double-entered, and any discrepancies or inaccuracies in the data entered by the two individuals were resolved through calibration and correction based on the questionnaires. Questionnaires with more missing content were excluded. Medical examiners receive uniform training from experts invited by the Health Commission. All instruments and equipment are calibrated before use. In addition, 5% of the population is randomly selected for on-site medical examinations to ensure the homogeneity and reliability of the results.
Statistical analysis
Statistical description and analyses were conducted using MS Excel and SPPS version 25. Single factor statistical analysis method: enumeration data were described by rate and composition ratio, and the comparison was performed by chi-square test or Fisher probabilities method. Univariate or multivariate logistic regression is used to analyze the occurrence of myopia between different groups. Meanwhile, the odds ratio (OR) and 95% confidence interval (CI) were used to describe and compare the associations between factors at different levels. Statistical tests were declared significant for a two-tailed P value not exceeding 0.05, except where otherwise specified.
Results
General characteristics of the study population
The demographic information of the study population is presented in Table 1. The mean age of the kindergarten, primary school, junior high school and senior high school students was 5.86 ± 1.96, 9.12 ± 1.74, 13.67 ± 0.90 and 16.73 ± 0.92 years (F = 19382.45, P < 0.001), respectively. No statistically significant difference was observed in the sex ratio across the four school segments (χ2 = 1.628, P = 0.653). The mean age of urban and suburban students was 12.00 ± 3.87 and 11.86 ± 3.83 years (F = 6.452, P = 0.142), respectively. There was no statistically significant difference was observed in the sex ratio between the urban and suburban students (χ2 = 2.482, P = 0.115).
Distribution characteristics of myopia
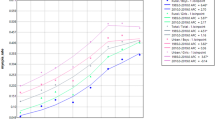
The study population comprised 31,880 individuals for whom both complete visual acuity data and demographic data were available. The overall prevalence of myopia was found to be 55.3% (17,630/31,880), with the myopia rates observed among students in kindergarten, primary school, junior high school, and senior high school, at 5.8%, 34.9%, 74.2%, and 85.0%, respectively (Table 2). As age increased, both male and female students demonstrated a rising prevalence of myopia. In the majority of age groups, the myopia rate was higher among female students than among male students (Fig. 2). As the academic year progresses, there has been an observable increase in the prevalence of myopia (χ2 = 8676.748, P<0.001), low myopia (χ2 = 5444.040, P<0.001) and high myopia (χ2 = 2171.073, P<0.001) among students, with the difference between the three groups being statistically significant. The prevalence of overall myopia, low myopia, and high myopia was higher in girls (58.5%, 52.5% and 6.0%) than in boys (52.3%, 46.9% and 5.4%). The overall prevalence of myopia and low myopia was higher in urban areas (55.6% and 49.9%) than in the suburban areas (54.1% and 48.4%). However, the difference in the prevalence of high myopia between the two areas was not statistically significant (χ2 = 0.004, P = 948).
Univariate analysis of related factors of myopia
Ultimately, a total of 6,037 students participated in the questionnaire survey. Following the exclusion of questionnaires with a missing information rate exceeding 5%, 5,652 valid questionnaires were obtained. Univariate analysis indicated that height of desks/chairs adjusted to students’ height, location of inter-class activities, homework time per day in the past week, parents restrict children watching electronics, the distance between chest and the edge of table was more than one fist when reading/writing, the distance between the eyes and book was more than one foot (33 cm) when reading/writing, the distance between the finger and the tip was more than 3 cm when reading/writing, teacher points out incorrect reading/writing posture, average daily TV viewing time, average daily computer time, lying down to read books or electronic screens, reading books or electronic screens while walking or on the bus, types of lights used for reading and writing at night, using a computer more than 66 cm from the screen, duration of using eyes at a short distance, time spent outside in the past one week, myopia in parents are the influencing factors of myopia in children and adolescents (all P<0.05). The univariate analysis of related factors of myopia are summarized in Table 3.
Multiple logistic regression analysis of related factors of myopia
Taking myopia as dependent variable, the statistically significant factors in the univariate analysis as independent variables into the binary logistic regression model, with adjustments for age, gender, and area. The results showed that, homework time ≥ 2 h in the past week, use table and roof lamps simultaneously when reading/writing at night, average daily TV viewing time ≥ 2 h, and one or both of the parents suffered myopia are significantly increase the risk of myopia in students. However, distance between the eyes and book was more than one foot (33 cm) when reading/writing is protective factors for myopia in children and adolescents. The results of the multiple logistic regression analysis of the related factors are presented in Table 4.
Discussion
Variation in myopia prevalence by geographic location has been well documented in the literature24.The overall myopia rate observed in this study among children and adolescents was 55.30%, which is comparable to that documented in developed countries in East Asia10, but higher than that reported in previous studies conducted in China2. In comparison to the National Childhood and Adolescent Myopia Survey of 2020, the prevalence of myopia in kindergartens and primary schools was found to be slightly lower, while a higher prevalence of myopia was observed in junior high schools and high schools17,25. The prevalence of myopia among high school students reached 85.0%, which consistent with the previously reported prevalence levels for the same age group in East Asian countries10.
The overall myopia prevalence and high myopia prevalence among students showed an obvious upward trend with the increase of the school segments. In particular, it should be noted that the period from fourth grade of primary school to the second grade of junior high school is a period that myopia prevalence increased rapidly. At the same time, both increased education burden on students and puberty growth spurt are happening in this period, two superimposed effects resulting in a rapid increase of myopia prevalence, prompting that the occurrence and progression of myopia is related to education level24,26. It is essential that adjustments be made to the pattern of learning in the senior school years and alleviate the considerable pressure that students face in their studies. The primary school stage represents a critical period for the prevention of new-onset myopia27. During the transition period between primary school and junior high school, as well as between junior high school and high school, it is of paramount importance to prioritise the prevention and control of the progression of myopia and the prevention of pathological myopia28.
Differences in myopia prevalence among children and adolescents found between genders, which is consistent with the results of most literature studies20,29,30. Some scholars believe that girls’ puberty growth and development is faster than that of boys, their eyeball development is also relatively fast and susceptible to environmental factors31. Some studies also pointed out that girls spend more time using their eyes at close environment than boys, so that having less time on outdoor activities and sports activities in recess and spare time32. Education on vision protection for girls should be strengthened in the daily teaching process. The prevalence of myopia among students in urban areas is higher than that in suburban, which may be related to the premature use of electronic products, education advance, less outdoor activities or living in high-rise residential buildings among children and adolescents in urban areas30,33,34.
The aetiology of myopia is multifactorial. Similar to previous studies, genetic factors play a crucial role in the prevalence of myopia35,36, especially in the occurrence of high myopia37. The findings of this study indicate that the time spent on homework after school, the correctness of reading and writing postures, the duration of exposure to electronic screens, and the use of lighting in an appropriate manner all have an impact on the development of myopia. A systematic review and meta-analysis of 27 articles also found that near-work activities (e.g., watching TV, reading, playing video games, etc.) increase the risk of developing myopia especially for high-degree myopia38. For this, the authors recommended controlling time spent on near-work activities, reducing exposure to electronic screens and choosing the right lights to reduce the risk of developing myopia among children. The findings of this study indicate that the distance between the eyes and the book was more than one foot (33 cm) when reading or writing was associated with a reduction in myopia prevalence among children and adolescents. This may be due to the fact that distance affects axial length and corneal curvature39. At present, the association between working distance and myopia is still controversial, this may be due to the fact that most studies on distance are based on student-filled questionnaires or parental questionnaires, with large recall bias or cognitive differences, and lack unitive measure indicators40.
We conducted a study on the latest prevalence and risk factors for myopia and high myopia in schools in eastern China. One advantage of the current study is that a large sample size of students at all grade levels was selected, thereby allowing for an assessment of the relationship between myopia and high myopia and age, grade level and gender. However, there are some limitations. First, the cross-sectional design of this study does not permit the establishment of causal relationships. Second, the refraction of each student was assessed by non-cycloplegic autorefraction, which could result in an overestimation of myopia prevalence. We tried to reduce the overestimated prevalence by basing the definitions of myopia on the combination of SE and VA. This should reduce the number of emmetropes incorrectly classified as low myopia. Nevertheless, our estimates of myopia and high myopia remain subject to bias. Third, most risk factors were obtained through the completion of questionnaires. It should be noted that the assessment of time spent on specific activities may vary somewhat from person to person, which could introduce a degree of confounding bias and recall bias. Fourth, some important myopia risk factors were not analyzed including environment, diet, family economic status, and genetic factors such as inherited gene polymorphisms.
Myopia has a considerable detrimental effect on the health of children and adolescents. In light of the findings of the present survey, it is recommended that comprehensive measures be taken with regard to the prevention and control of myopia. Firstly, it is important to acknowledge the role of genetic factors in the development of myopia. Therefore, it is recommended that children and teenagers who have a parent with myopia should carry out early prevention and control of their vision, undergo regular screening, assess their distant vision reserves. Secondly, it is imperative that schools, families and society at large collaborate to foster the development of positive learning and living habits in children and adolescents, such as adjust the pattern of learning in the senior school years, strengthen the education on vision protection for girls, regulate the time spent on homework and electronic screen exposure, select appropriate lighting, and provide guidance to children on maintaining proper postures when reading and writing. Finally, it is recommended that parents encourage their children to participate in a greater number of outdoor sports activities and ensure that they spend a minimum of one hour outdoors each day. In future studies, it is expected that the construction of a comprehensive prevention and control intervention model for myopia in children and adolescents based on society-hospital-school-family-individual students will help to alleviate the problem of the continuous increase in the prevalence of myopia.
Conclusions
This is a cross-sectional study based on key school discovery. The overall prevalence of myopia and high myopia in schools in Hangzhou, China, is notably high. The prevalence of myopia and high myopia increases with grade or age. Myopia is associated with increased age, parental myopia, extended periods of homework after school, poor reading and writing posture, prolonged exposure to electronic screens and inappropriate lighting. In light of the findings of the present survey, it is recommended that a comprehensive prevention and control intervention model for myopia in children and adolescents based on society-hospital-school-family-individual students with a view to preventing and controlling myopia.
Data availability
The data that support the findings of this study are available on request from the corresponding author, Hong Xu. The data are not publicly available due to containing a wealth of adolescent health information that could compromise the privacy of research participants.
References
Dolgin, E. The myopia boom. Nature 519(7543), 276–278 (2015).
Morgan, I. G. et al. The epidemics of myopia: Aetiology and prevention. Prog. Retin. Eye Res. 62, 134–149 (2018).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016).
Dong, L. et al. Prevalence and time trends of myopia in children and adolescents in China: A Systemic Review and Meta-Analysis. Retina 40(3), 399–411 (2020).
National Health Commission of the People’s Republic of China. Transcript of the press conference of "China’s White Paper on Eye Health" [EB/OL]. [2020–06–05]. http://www.nhc.gov.cn/xcs/s3574/202006/1f519d91873948d88a77a35a427c3944.shtml
Kobia-Acquah, E. et al. Regional variations and temporal trends of childhood myopia prevalence in Africa: A systematic review and meta-analysis. Ophthalmic. Physiol. Opt. 42(6), 1232–1252 (2022).
Hagen, L. A. et al. Prevalence and possible factors of myopia in norwegian adolescents. Sci. Rep. 8(1), 13479 (2018).
Schuster, A. K. et al. Prevalence and time trends in myopia among children and adolescents. Dtsch. Arztebl. Int. 117(50), 855–860 (2020).
Harrington, S. C. et al. Refractive error and visual impairment in Ireland schoolchildren. Br. J. Ophthalmol. 103(8), 1112–1118 (2019).
Rudnicka, A. R. et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: Implications for aetiology and early prevention. Br. J. Ophthalmol. 100(7), 882–890 (2016).
Morgan, I. G. et al. IMI risk factors for myopia. Invest. Ophthalmol. Vis. Sci. 62(5), 3 (2021).
Saw, S. M. et al. Nearwork in early-onset myopia. Invest. Ophthalmol. Vis. Sci. 43(2), 332–339 (2002).
Chen, X. et al. Prevalence, incidence, and risk factors for myopia among urban and rural children in southern China: protocol for a school-based cohort study. BMJ Open. 11(11), e049846 (2021).
National Health Commission of the People’s Republic of China. Notice on the Children and Adolescent Myopia Survey, which is jointly issued by the General Office of the National Health Commission, the General Office of the Ministry of Education, and the General Office of the Ministry[EB/OL]. [2018–10–26]. http://www.nhc.gov.cn/jkj/s5898bm/201810/08e2b45092d346a8a8c960d3e3d98b62.shtml
Liu, M. et al. Refractive Errors and Risk Factors for Myopia in Primary School Students in Urumqi. Appl. Bionics Biomech. 2022, 2657455 (2022).
Wang, N. L. & Wei, S. F. Emphasizing the standardized use of cycloplegics in the epidemiological studies of myopia. Zhonghua. Yan. Ke. Za. Zhi. 55(8), 561–564 (2019).
Zhao, X. et al. Prevalence of myopia and associated risk factors among key schools in Xi’an, China. BMC Ophthalmol. 22(1), 519 (2022).
Flitcroft, D. I. et al. IMI - Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Invest. Ophthalmol. Vis. Sci. 60(3), M20–M30 (2019).
National Health Commission of the People’s Republic of China. Notice on printing and distributing the National Student Common Diseases and Health Influencing Factors Monitoring and Intervention Program [EB/OL]. [2019–03–26]. http://www.nhc.gov.cn/jkj/s5898bm/201903/1bcbac21e1864377ad24984fac014c7d.shtml
Xie, Z. et al. Prevalence of myopia and associated risk factors among primary students in Chongqing: multilevel modeling. BMC Ophthalmol. 20(1), 146 (2020).
Huang, L. et al. The prevalence of myopia and the factors associated with it among university students in Nanjing: A cross-sectional study. Med. (Baltimore) 98(10), e14777 (2019).
Dragomirova, M. et al. Myopia in Bulgarian school children: prevalence, risk factors, and health care coverage. BMC Ophthalmol. 22(1), 248 (2022).
Jing, S. et al. Prevalence and risk factors for myopia and high myopia: A cross-sectional study among Han and Uyghur students in Xinjiang, China. Ophthalm. Physiol. Opt. 42(1), 28–35 (2022).
Pan, C. W., Ramamurthy, D. & Saw, S. M. Worldwide prevalence and risk factors for myopia. Ophthalm. Physiol. Opt. 32(1), 3–16 (2012).
Central People’s Government of the People’s Republic of China. The overall myopia prevalence of children and adolescents in China is 52.7% in 2020, and the problem of myopia at a younger age is still prominent[EB/OL]. [2021–07–13]. http://www.gov.cn/xinwen/2021-07/13/content_5624709.htm
Mountjoy, E. et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ 361, k2022 (2018).
Tao, F. Expert interpretation on appropriate technical guidelines for prevention and control of myopia in children and adolescents. Chin. J. Sch. Health 41(02), 166–168 (2020).
Luo, C.-Y. et al. Analysis of low vision monitoring among primary and secondary school students in Shanghai during 2011–2015 academic year. Capital J. Publ. Health 11(03), 106–108 (2017).
Gebru, E. A. & Mekonnen, K. A. Prevalence and factors associated with myopia among high school students in Hawassa City, South Ethiopia, 2019. Clin. Optom. (Auckl) 14, 35–43 (2022).
Karthikeyan, S. K. et al. Physical activity, time spent outdoors, and near work in relation to myopia prevalence, incidence, and progression: An overview of systematic reviews and meta-analyses. Indian J. Ophthalmol. 70(3), 728–739 (2022).
Zhao, H., Yu, J. & Xu, H. Prevalence and associated factors of myopia among third-grade primary school students in the Gongshu District of Hangzhou. Chinese Journal of Optometry Ophthalmology 5, 321–326. https://doi.org/10.3760/cma.j.issn.1674-845X.2019.05.001 (2019).
Long, P. et al. Prevalence of myopia and associated factors among primary and secondary school students in Chongqing. Chin. J. Sch. Health 36(01), 109–112. https://doi.org/10.16835/j.cnki.1000-9817.2015.01.033 (2015).
Zhou, J. et al. Prevalence of myopia and influencing factors among primary and middle school students in 6 provinces of China. Zhonghua Liu Xing Bing Xue Za Zhi 37(1), 29–34 (2016).
Wu, P. C. et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 120(5), 1080–1085 (2013).
Tian, X. et al. Retinal changes following rapid ascent to a high-altitude environment. Eye (Lond) 32(2), 370–374 (2018).
Wenbo, L., Congxia, B. & Hui, L. Genetic and environmental-genetic interaction rules for the myopia based on a family exposed to risk from a myopic environment. Gene 626, 305–308 (2017).
Robboy, M. W. et al. Assessment of clinical trials for devices intended to control myopia progression in children. Eye Contact Lens 44(4), 212–219 (2018).
Huang, H. M., Chang, D. S. & Wu, P. C. The association between near work activities and myopia in children-a systematic review and meta-analysis. PLoS One 10(10), e0140419 (2015).
Liang, Y. & Kee, C. S. Risk factors for myopia in 2 Hong Kong school systems: A pilot study. Asia Pac. J. Ophthalmol. (Phila) 11(1), 19–26 (2022).
Liu, Y. L. et al. Influence of parental behavior on myopigenic behaviors and risk of myopia: Analysis of nationwide survey data in children aged 3 to 18 years. BMC Public Health 22(1), 1637 (2022).
Acknowledgements
The authors would like to thank all the students and teachers who participated in this survey and thank all of the project team staff, including fieldworkers, administrative staff, computer and data management staff, and the trainers who provided teacher training. They also thank Mr. Lizhang Wang (Strategic Director for Children, Youth and Skills, Fuyang College: Zhejiang Open University), Mr Mingming Shen (Director of Academic Affairs, Fuyang College: Zhejiang Open University) and Mrs Hanhan Fang (Director of Academic Affairs, Fuyang College: Zhejiang Open University) for their support to the project. They thank the Medical and Health Science and Technology Project of Hangzhou (grant number: A20220246) and Scientific Research Project on Agricultural and Social Development in Hangzhou (grant number: 2024ZDSJ0150) for its financial support.
Author information
Authors and Affiliations
Contributions
All authors listed have made substantial contributions to the work. L.Z., B.Z., H.X. and X.J. contributed to the conception or design of the work. L.Z., X.J., W.Z., L.H., Y.Z. and S.W. contributed to the acquisition, analysis or interpretation of data for the work. L.Z. and B.Z. drafted the manuscript. B.Z., H.X. and X.J. critically revised the manuscript. All agreed on the journal to which the article will be submitted. All have reviewed and agreed on all versions of the article prior to submission, during revision, the final version accepted for publication, and any substantial changes made at the proofreading stage. Agreed to take responsibility and accountability for the content of the article and to share responsibility for resolving any questions raised about the accuracy or integrity of the published work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, L., Jiang, X., Zhang, W. et al. Prevalence and risk factors of myopia among children and adolescents in Hangzhou. Sci Rep 14, 24615 (2024). https://doi.org/10.1038/s41598-024-73388-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-73388-7
Keywords
This article is cited by
-
Association of physical activity, sedentary behaviour, sleep and myopia in children and adolescents: a systematic review and dose-response meta-analysis
BMC Public Health (2025)
-
Predicting myopia risk using a machine learning model based on fundus imageomics
Scientific Reports (2025)
-
Repeated low-level red-light therapy vs. conventional treatments for myopic control in children: a systematic review and meta-analysis
Scientific Reports (2025)
-
Exploring the interrelationship between myopia, psychological resilience, and emotion regulation in adolescents using a network analysis
Scientific Reports (2025)