Abstract
Critical care nurses have high workloads due to the severity of the disease and the complexity of the treatment and care. Understanding the factors that influence subjective workload as well as the association between subjective and objective workload could lead to new insights to reduce critical care nurses’ workload. (1) To describe critical care nurses’ subjective and objective workload per shift in a university-affiliated interdisciplinary adult intensive care unit in Switzerland and (2) to explore the association between objective and subjective workload. The study used a prospective longitudinal cohort design. Critical care nurses completed the adapted Questionnaire on the Experience and Evaluation of Work 2.0 (QEEW2.0) to assess the subjective workload after every shift for four weeks (0 = never loaded, 100 = always loaded). The objective workload was assessed with the Therapeutic Intervention Scoring System-28 (TISS-28), Nine Equivalents of Nursing Manpower Use Score (NEMS), Swiss Society for Intensive Care Medicine (SGI)-patients’ categories and Patient-to-Nurse Ratio (PNR). Data was analysed using multilevel mixed models. The workload of 60 critical care nurses with a total of 765 shifts were analysed. The critical care nurses experienced a subjective high mental load (66 ± 26), moderate pace and amount of work (30 ± 25) and physical load (33 ± 25), and low emotional-moral load (26 ± 22). The one-time baseline subjective workload values were higher than the day-to-day values. The mean objective shift load using the TISS-28 was 43 ± 16 points, the NEMS 36 ± 14 points, the SGI-category 1.1 ± 0.5 nurses needed per patient and the PNR 1.2 ± 0.4. We found positive associations between day-to-day objective variables with subjective pace and amount of work, with physical and mental load but not with emotional-moral load and performance. Measured objective workload is associated with only certain subjective workload domains. To promote and retain critical care nurses in the profession, nursing management should give a high priority to understanding subjective workload and strategies for reducing it.
Similar content being viewed by others
Introduction
Critical care nurses have high workloads due to the severity of the disease and the complexity of the treatment and care. A high workload for CCNs is associated with higher mortality, nosocomial infections, pressure ulcers and medication errors as well as lower patient safety and satisfaction1,2,3. CCNs’ workload consists of care demands to be done with the available resources in an intensive care unit (ICU)4. Job demands contain physical, mental and emotional-moral loads5. Permanent high-level workloads lead to stress, sleeping disorders, depression, burnout, job dissatisfaction, low work performance and intention to leave the profession5,6,7. Almost 80% of CCNs throughout the world say they bear a high burden, and 30–40% show burnout symptoms8,9. To retain CCNs in their profession, it is crucial to understand all dimensions, determinants and all the potential alleviating factors of CCNs’ workload10.
CCNs’ workload can be measured by subjective or objective approaches11,12. Subjective nursing workload is defined as “the overall perception of personal ability to perform at a level the person finds satisfying or acceptable based on personal performance and performance results”13. The perception of job demands, resources and workload as well as their impact on the CCN depend on human factors, which include individual characteristics, coping strategies and resources7,14,15. Despite its relevance to human factors (e.g. performance) and workload reduction, CCNs’ subjective workload and its stressors have scarcely been studied due to difficult, expensive and time-consuming measurements that are dynamic over time16,17.
From the objective or patient demands approach, nursing workload is defined as “the amount of time and care that a nurse can devote directly and indirectly towards patients, workplace, and professional development”18. Instruments like the Therapeutic Intervention Scoring System (TISS-28), Nine Equivalents of Nursing Manpower Use Score (NEMS), Swiss Society for Intensive Care Medicine (SGI)-category or Patient-to-Nurse Ratio (PNR) have been used to study the CCNs’ objective workload using time- and task-based models of direct patient care11. Direct patient care is defined as work that directly or indirectly benefits the patient (e.g. measuring vital signs or preparing medication)19. The objective workloads are routine measurements as they provide financial reimbursement for the services of the ICU but do not cover potentially important workload dimensions like the impact of the CCNs’ human factor or non-patient related care like training nursing students12,20,21.
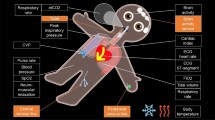
Despite the existing literature on objective workload and insights into CCNs’ subjective workload, the latter’s variation over time and association with objective workload are rarely studied22. In the absence of evidence about the comparability of subjective with objective workload, it is unclear whether and how they are associated. Based on two basic models of subjective and objective workload, we will assess and compare them with each other [see Supplementary Fig. S1].
Methods
This manuscript followed the statement checklist for cohort studies of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)23.
Aims
The aims of this study were (1) to describe CCNs’ subjective and objective workload over time and (2) to explore the association between objective and subjective workload.
Design
This is a prospective longitudinal cohort study using online questionnaires and routine data between November 2022 and January 2023.
Setting and participants
This study was conducted in a university-affiliated interdisciplinary adult ICU with 30 beds in Switzerland. In total, 154 CCNs work in this ICU in three shifts. CCNs are registered nurses who completed a 2-year post-graduate training in critical care. The recruitment was based on self-selection by the CCNs. Authors of the Questionnaire on the Experience and Evaluation of Work (QEEW2.0) recommend that at least one-quarter of a team be included in any study using the instrument (≥ 39 CCNs)24. Inclusion criteria were being a permanently employed CCN working in this ICU and having signed the informed consent.
Variables and measurements
Demographics of CCNs and patients
The CCNs’ characteristics included age, gender, skills and experience (years working in an ICU) and employment level (percentage). The patients’ characteristics including age and gender were collected by the researchers after every shift using the clinical information system.
Subjective workload
Subjective workload is based on the Job Demands and Resources (JD-R) model using three domains which interact with each other25 [see Supplementary Fig. S1]:
-
(1)
Subjective job demands include pace and amount of work, physical, mental and emotional-moral load, and interruptions.
-
(2)
Subjective job resources include staffing adequacy, support from the team and support from management.
-
(3)
Human factors include ICU experience in years, job satisfaction, motivation, work-life balance and work performance.
Each variable was assessed using the corresponding subscale of the QEEW2.0 questionnaire which contained one to six statements24. For example, job satisfaction contained: “I enjoy my work.” The statements could be rated by four answer options: Always—Often—Sometimes—Never or by five answer options: Strongly agree—Agree—Neutral—Disagree—Strongly disagree. The QEEW2.0, a reliable and valid tool to assess the employee’s subjective workload with a human factor approach, has been widely applied in studies with registered nurses and once with CCNs26,27,28,29. The QEEW2.0 was developed in the Netherlands and translated into several languages including German by the authors. The permission to use this questionnaire was obtained by the authors. We selected four of the original five domains (work perception, organisation, human resources, vitality) using 13 subscales (out of 42, e.g. physical load) and 53 questions (out of 217) to keep the effort for the CCNs within limits. We excluded the last domain “diagnostic scales” with the focus on personal physical feelings in general due to lack of alignment with the day-to-day subjective workload. The subscales in the questionnaire have a high content validity and internal consistency (Cronbach’s alpha of at least 0.7)24,26. Some of these variables (“baseline subjective workload variables”), such as CCNs’ experience, are relatively stable over time. Other variables can change on a day-to-day basis due to human factors (e.g. performance) or influences of altered external work circumstances (e.g. mental load), for which we use the term “day-to-day subjective workload variables.”
Objective workload
Objective workload is based on task- and time-based models using two domains: (1) job demands (time and task load) and (2) job resources (staffing)11 [see Supplementary Fig. S1]. Objective workload was assessed with four task- and time-based instruments:
(a) The TISS-28 contains 28 items, weighted with 1–8 points per item with a maximum of 78 points per patient per shift19. An average nurse can deliver care equal to 46.35 TISS-28 points per shift.
(b) The NEMS is a simplified tool extracted from the TISS-28 containing 9 items weighted with 3–12 points30. The maximum points per patient per shift is 56; 1 point corresponds to 10.6 min of nursing care.
(c) The SGI-categories classifies patients into four categories (1 A, 1B, 2, 3) using the NEMS and the Sedation Agitation Scale or Richmond Agitation Sedation Scale31,32,33,34. Category 1 A = 1.33 nurses per patient per shift, category 1B = one nurse per patient, category 2 = one nurse per two patients and category 3 = one nurse per three patients.
(d) The PNR, as number of total patients divided by the number of total nurses present, was calculated for the entire working shift.
NEMS and the SGI categories were used because they are mandatory and routinely collected in Switzerland.
Data sources
Three data sources were used: (a) The QEEW2.0, filled out electronically by all participating CCNs, was used to collect the demographic data and the baseline subjective JD-R (e.g. CCNs’ motivation) and the day-to-day subjective JD-R (e.g. mental load) after every CCN shift over 4 weeks; (b) The clinical information system captured the objective job demands (e.g. TISS-28) automatically as routine data; and (c) The personnel deployment planning system collected the objective job resources filled out by the head of department after every CCN shift (e.g. staffing).
Data collection
The research team informed the CCNs about the study. Interested CCNs were informed in detail about the goals of the study both orally and in writing. The data collection lasted four weeks between November 2022 and January 2023 [see Supplementary Table S2]. We chose winter because few CCNs are on holiday, supporting recruiting CCNs for the study.
During the 4 weeks of data collection, the first time point was set on each CCN’s first shift. Participants filled out the demographics questionnaire and the QEEW2.0 to capture the baseline variables of the subjective JD-R and the human factor24. The average time of completion was 15 min for the baseline questionnaire. All subsequent time points during the 4 weeks followed the working shifts of the CCN. Holidays were compensated after but not absence due to illness. Participants filled in the QEEW2.0 questionnaire retrospectively at the end of each shift to gather the day-to-day subjective variables of the shift-level subjective JD-R and the human factor24. The daily questionnaire took on average 2 min to complete. All questions without missing items were submitted electronically to finalise the questionnaire. If the questionnaire was not completed, the research team sent a reminder by email, WhatsApp or short message service to get the highest possible response rate. For the period of November 2022 until January 2023, all routine data were extracted daily from the clinical information system by the research team.
Data analysis
We performed a descriptive analysis of the demographic and the subjective and objective CCNs’ workload data. Means and standard deviations were calculated. CCNs’ subjective workload was assessed using the scaled score formula from the authors of the QEEW2.0 24. CCNs’ objective workload was assessed using the calculated objective instruments from direct patient demands. If the CCN cared for more than one patient in the same shift, the scores were summed. The workload scores TISS-28 and NEMS were multiplied by 10.6 min, resulting in the expected CCN workload per shift, as estimated by Miranda et al.19,30. Observed PNR was divided by the expected workload calculated from the TISS-28, NEMS and SGI-categories. An observed ratio > 1 (more than expected) resulted in understaffing and a ratio < 1 resulted in overstaffing4,35,36.
Association (Aim 2) was addressed by regressing subjective on objective workload with different control variables. CCNs’ shifts without direct patient care (e.g. shift manager) were excluded from the regression. The intraclass correlation coefficient 1 of the day-to-day subjective workload variables (range 0.16–0.45) indicated high between-individual variability, which led to our choosing to use multilevel regression models37 [see Supplementary Table S3]. The dependent variables of the models were each of the five day-to-day subjective workload variables (e.g. physical load). Independent variables were one of the four objective variables individually (e.g. TISS-28) in one model to each dependent variable. Therefore, there were 20 models in total [see Supplementary Table S4]. Further independent variables (work shift, CCNs’ age, baseline subjective variable of the same day-to-day variable) were chosen based on literature and statistical backward inclusion testing21. Based on the testing, CCNs’ education, working experience and level of employment were excluded as further independent variables. The estimated model results were reported with the marginal and conditional goodness of fit (R2) and their probability significance level (p< 0.05). The marginal R2 represents the fixed effects of the objective variables and the conditional R2 the fixed plus random effects. The difference between them represents the random effects representing the influence of the individual CCN human factor. To address potential influence due to multiple testing, the p-values with the false discovery rate were included in the calculation38.
We performed all analyses using R statistical software, version 4.3.0 for Windows39. For data exploring, processing and presenting, we used the packages ggplot2, dplyr, tidyverse, tableone and kableExtra40,41,42,43,44. The packages lattice, lme4 and rptR were used for the intraclass correlation 1 and model calculations45,46,47.
Results
Demographics of CCNs
Of the 154 CCNs in the ICU, 60 participated in the study (see Fig. 1). One participant dropped out due to long-term sickness and another did not fill in the questionnaire in the longitudinal data collection process. The final sample consisted of 58 CCNs (38%) who completed all day-to-day subjective questionnaires. The CCNs’ mean age was 33.5 years (SD = 7.4) and 95% (n = 57) were female (see Table 1). The 58 CCNs cared for 956 patients during 765 shifts. The patients’ demographic data are shown in the Supplementary Table S5.
Flowchart of CCNs’ sample and data collection. CCN Critical care nurses, ICU intensive care unit, QEEW2.0 Questionnaire on the Experience and Evaluation of Work, TISS-28 Therapeutic intervention scoring system, NEMS Nine equivalents of nursing manpower use score, SGI Swiss society for intensive care medicine.
Baseline subjective, day-to-day subjective and objective workload
The highest baseline subjective load was mental load with a mean of 89 (SD = 12, 0 = never loaded, 100 = always loaded) (see Table 2). Motivation on average was high (mean = 18, SD = 11, 0 = very strongly agree, 100 = absolutely disagree).
From all working shifts (n = 865), the response rate of the day-to-day subjective QEEW2.0 was 94% (n = 813). The CCNs worked on average 13 shifts (range = 1–22) during the study period, including 321 day-, 239 evening- and 253 night-shifts. Overall, mental load was considered highest (mean = 66, SD = 26, 0 = never loaded, 100 = always loaded). Ninety-four per cent (n = 765) of the shifts were linked to direct patient care. There was an overall higher workload for CCNs with direct patient care than for managers or student educators. For example, CCNs perceive the physical load on average 34 with and 20 without direct patient care (0 = never loaded, 100 = always loaded).
Overall, the CCNs rated their baseline subjective workload higher than their day-to-day workload. For example, the CCNs perceived the emotional-moral load on average 49 (SD = 11) before the study and 26 (SD = 22) after their shifts (0 = never loaded, 100 = always loaded).
The average shift load in PNR was 1.2 (SD = 0.4) and in TISS-28 43 points (SD = 15), which is equivalent to 456 min of work which a CCN should be able deliver in their 480 min shift.
Associations between day-to-day subjective and objective workload
The results of the models showed associations (FDR-p < 0.05) between all objective workload variables to day-to-day subjective pace and amount of work (physical and mental load), but none to emotional-moral load and subjective performance [see Table 3]. The marginal R2, effects from only objective workload, were highest for pace and amount of work and mental load. Mental load is highest effect, explained by objective workload including human factors (conditional R2). The difference R2, effects from only human factors, showed the lowest effect on pace and amount of work. The human factor affects all subjective workloads except pace and amount of work to a greater degree than objective workload.
Discussion
This is an observational longitudinal study of CCNs’ workload in one Swiss ICU using day-to-day questionnaires and routine data. CCNs reported a high mental load, moderate pace and amount of work and physical load, low emotional-moral load and good performance. We found positive associations between all objective workload instruments with the day-to-day subjective pace and amount of work, physical and mental load but none with emotional-moral load and performance. As the highest explainable variable, half of the mental load can be explained by objective instruments. Overall, only the pace and amount of work are explained better by objective instruments than by individual human factor influences.
The CCN’s high mental load in our study, as well as in other studies, is explained by the fact that caring for critically ill patients is complex, including not only mechanical-manual interventions and unpredictable events16,48,49 but also high responsibility for the well-being of the patient. We expected a high emotional-moral load similar to the mental load, as seen in Germany, due to the ICU setting characterized by high patient dependency or poor prognosis, conflictual ethical decisions and death8,50. However, emotional-moral load is perceived as low to moderate by our CCNs, corroborating with other studies from the United States and Italy51,52. This difference could be due to the different average staffing situations of 2.5 PNR in Germany and 1.2 PNR in our study8,50. Similar to our findings, the subjective CCNs’ performance remains good, indicating effective compensation strategies even in high workload situations53,54. Therefore, subjective performance could also be used only as a baseline variable. We expected a higher day-to-day subjective workload in all dimensions other than the baseline. However, our current findings conform with the results in a paediatric ICU in the United States, using different instruments55. The longitudinal design of our study allows a more precise assessment of the subjective workload and therefore, should be further investigated.
In our study, CCNs’ objective workload is calculated with four time- and task-based instruments showing different workload profiles. While the TISS-28, NEMS and SGI-category focus on intensity of nursing tasks based on patients’ illnesses, the PNR is a numeric count of patients and does not consider severity11. Since the SGI-category is used only in Switzerland, comparison to other studies is limited. Because the interpretation of objective workload is not fully understood11, we interpreted the workload as a quotient of the job demands and resources. According to the objective workload instruments, the number of nursing staff in our ICU is adequately adapted to the workload, but most other studies in Europe and Taiwan consider their shifts as understaffed3,56,57,58,59. In previous studies using TISS-28 and NEMS, it was rare to find CCNs often simultaneously caring for more than one patient, and comparisons of their single patients’ load to our CCNs’ cumulated shift load results could be misleading3,57. Following the international recommendation, over 75% of the CCNs in our study cared for only one patient in a shift35. Similar findings on the PNR have been reported, but these were analysed mostly in terms of adverse events like mortality1,60,61. Further it must be considered that the TISS-28 and NEMS are nearly 30 years old and have not been adapted since although there have been changes in the ICU setting. But as validated instruments, they still provide reasonable estimates of workload demands.
The associations of this study are limited compared to findings by other studies, which may have had settings other than the ICU, other instruments measuring subjective workload and different data collection designs, such as a single time point rather than longitudinal. The first study to our knowledge comparing CCNs’ subjective and objective workload, by Hoogendoorn et al. in the Netherlands, found no association but showed a tendency similar to our findings22. This discrepancy could be explained by the fact that they summed all dimensions of subjective perception and did not look into multidimensional differences. Additionally, they calculated linear mixed model associations without considering the individual CCN with the human factor, and the details of the completed subjective questionnaires are unclear. The comparability of the studies is therefore limited. The non-significant association between emotional-moral load and the TISS-28 or NEMS may be due to the exclusion in the scores of such emotionally stressful situations as patients’ delirium or intensive care for relatives5,62. According to the World Federation of Critical Care Nurses (2019), one CCN should care for one patient; this would give a constant number and not impact subjective workload35. However, practice often differs from guidelines. The PNR was statistically significantly associated with the day-to-day subjective pace and amount of work and with physical and mental load in our and other studies22,62.
As the associations show similar results using TISS-28, NEMS and SGI-category on subjective workload, further assessment needs to determine which of these three instruments brings the most insights for clinical practice. Because the results of PNR always showed weaker associations with subjective workload, its further use in this context should be evaluated.
Limitations
Strengths of this study are the longitudinal data collection (over 4 weeks), the many work shifts covered and the high response rate on the day-to-day questionnaires, as well as the completeness of the data set. The longitudinal design also allows new insights and shows trends of CCNs’ subjective workload over time, reflecting everyday practice and reality.
However, limitations exist. First, the restriction to one hospital may reduce the external validity and generalisability of our results to other hospitals. Second, the study may suffer from low validity of the QEEW2.0, TISS-28, NEMS and SGI-category as process parameters which might negatively affect the day-to-day variability of workload24,63. The results seem valid as they seem to fit our expectations. Additionally, we used only a subset of the QEEW2.0 which could lower its validity. Further, there are newer workload scores such as the Nursing Activities Score (NAS)64 which describe the nurse workload to a higher degree, but these have not been implemented in Switzerland. Third, selection bias could have occurred due to self-selection of the participants with a possible over-representation of highly motivated and more resilient CCNs65. Last, other variables than those we selected might have influenced the day-to-day subjective workload; these need to be considered in further investigations.
Recommendation for practice and research
As some subjective workload domains are clearly less represented than others by objective measures, the integration of subjective workload into daily shift management and case-based payment is recommended. We recommend the use of tools like the QEEW2.0 as it allows the perspective on subjective workload, which is a productive pathway for future research, and also integrates it into workload management. As the subjective workload is often underestimated in practice, we suggest encouraging discussion to address subjective workload on an individual and team level. The ICU management might take measures to alleviate the subjective workload and improve the organisation of uninterrupted work. This could promote CCNs’ work engagement and should be scientifically evaluated. Also, further research is suggested on other factors influencing subjective workload such as other baseline subjective variables, patients’ delirium or aggressive reactions and their weighting in subjective workload.
Conclusions
This study provides insights into the association between subjective and objective workload in a longitudinal design. The TISS-28, NEMS, SGI-category and PNR are linked with day-to-day subjective pace and amount of work, physical and mental load but not with emotional-moral load and performance. These results demonstrate that objective instruments can measure workload of direct patient care, but not all subjective workload dimensions such as emotional-moral load, which have a role in the CCN’s work. A comprehensive understanding including subjective workload and strategies for its reduction should be targeted and given a high priority in ICU management to promote and retain CCNs in the profession. Subjective workload is a main part of CCNs workload and often remains unmeasured despite high potential for interventions.
Data availability
The datasets used and analysed during the current study are available from the corresponding author and may be made accessible through a data use agreement.
Abbreviations
- CCN:
-
Critical care nurse
- CI:
-
95% confidence interval
- FDR-p:
-
False discovery rate adjusted probability-value
- ICC 1:
-
Intraclass correlation coefficient 1
- ICU:
-
Intensive care unit
- JD-R:
-
Job demand and resources
- NEMS:
-
Nine equivalents of nursing manpower use score
- PNR:
-
Patient-to-nurse ratio
- p:
-
Probability (significant p < 0.05)
- R:
-
ICC coefficient
- R2 :
-
Goodness of fit
- RN:
-
Registered nurse
- SD:
-
Standard deviation
- SE:
-
Standard error
- SGI:
-
Swiss society for intensive care medicine
- German:
-
Schweizerische Gesellschaft für Intensivmedizin
- SKB:
-
Foundation for quality promotion in occupational health care
- Dutch:
-
Stichting Kwaliteitsbevordering Bedrijfsgezondheidszorg
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- TISS-28:
-
Therapeutic intervention scoring system
- QEEW:
-
Questionnaire on the experience and evaluation of work
References
Rae, P. J. L. et al. Outcomes sensitive to critical care nurse staffing levels: a systematic review. Intensive Crit. Care Nurs. 67, 11 (2021).
Ross, P., Howard, B., Ilic, D., Watterson, J. & Hodgson, C. L. Nursing workload and patient-focused outcomes in intensive care: a systematic review. Nurs. Health Sci. https://doi.org/10.1111/nhs.13052 (2023).
Chang, L. Y., Yu, H. H. & Chao, Y. F. C. The relationship between nursing workload, quality of care, and nursing payment in intensive care units. J. Nurs. Res. 27, e8 (2019).
Intensive and Critical Care Medicine: WFSICCM World Federation of Societies of Intensive and Critical Care Medicine. (Springer, 2009). https://doi.org/10.1007/978-88-470-1436-7
Breinbauer, M. Arbeitsbedingungen Und Arbeitsbelastungen in Der Pflege: Eine Empirische Untersuchung in Rheinland-Pfalz (Springer Fachmedien, 2020). https://doi.org/10.1007/978-3-658-32021-8
Khan, N., Jackson, D., Stayt, L. & Walthall, H. Factors influencing nurses’ intentions to leave adult critical care settings: what factors influence nurses’ intentions to leave the adult critical care areas? Nurs. Crit. Care. 24, 24–32 (2019).
Bakker, A. B. & de Vries, J. D. Job demands—resources theory and self-regulation: new explanations and remedies for job burnout. Anxiety Stress Coping. 34, 1–21 (2021).
Graeb, F. Ethische Konflikte Und Moral Distress auf Intensivstationen: Eine Quantitative Befragung Von Pflegekräften (Springer Fachmedien, 2019). https://doi.org/10.1007/978-3-658-23597-0
Kumar, A. et al. Burnout and its correlates among nursing staff of intensive care units at a tertiary care center. J. Fam Med. Prim. Care. 10, 443 (2021).
Happell, B. et al. Nurses and stress: recognizing causes and seeking solutions. J. Nurs. Manag. 21, 638–647 (2013).
Hoogendoorn, M. E. et al. Workload scoring systems in the Intensive Care and their ability to quantify the need for nursing time: a systematic literature review. Int. J. Nurs. Stud. 101, 103408 (2020).
De Oliveira, J. L. C., Cucolo, F. & De Magalhães, D. Galan Perroca, M. Beyond patient classification: the hidden face of nursing workload. Rev. Esc Enferm USP. 56, e20210533 (2022).
Neill, C. D. Development of a subjective workload assessment for nurses. Graduate school of th texas woman’s university, Denton, Texas (2006).
Moghadam, K. N. et al. Nursing workload in intensive care units and the influence of patient and nurse characteristics. Nurs. Crit. Care. https://doi.org/10.1111/nicc.12548 (2020).
Palamarchuk, I. S. & Vaillancourt, T. Mental resilience and coping with stress: a comprehensive, multi-level model of cognitive processing, decision making, and behavior. Front. Behav. Neurosci. 15, 719674 (2021).
Teng, M., Yuan, Z., He, H. & Wang, J. Levels and influencing factors of mental workload among intensive care unit nurses: a systematic review and meta-analysis. Int. J. Nurs. Pract. e13167, 1–11 (2023).
Holland, P., Tham, T. L., Sheehan, C. & Cooper, B. The impact of perceived workload on nurse satisfaction with work-life balance and intention to leave the occupation. Appl. Nurs. Res. 49, 70–76 (2019).
Alghamdi, M. G. Nursing workload: a concept analysis. J. Nurs. Manag. 24, 449–457 (2016).
Reis Miranda, D., de Rijk, A. & Schaufeli, W. Simplified therapeutic intervention scoring system: the TISS-28 items–results from a multicenter study. Crit. Care Med. 24, 64–73 (1996).
Bruyneel, A. et al. Measuring the nursing workload in intensive care with the nursing activities score (NAS): a prospective study in 16 hospitals in Belgium. J. Crit. Care. 54, 205–211 (2019).
Myny, D. et al. Non-direct patient care factors influencing nursing workload: a review of the literature. J. Adv. Nurs. 67, 2109–2129 (2011).
Hoogendoorn, M. E. et al. The objective nursing workload and perceived nursing workload in intensive care units: analysis of association. Int. J. Nurs. Stud. 114, 1–7 (2021).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 4, e296 (2007).
van Veldhoven, M. J. P. M., Prins, J., van der Laken, P. A. & Dijkstra, L. QEEW2.0: 42 Short Scales for Survey Research on Work, Well-Being and Performance (SKB, 2015).
Demerouti, E., Bakker, A. B., Nachreiner, F. & Schaufeli, W. B. The job demands-resources model of burnout. J. Appl. Psychol. 86, 499–512 (2001).
van den Oetelaar, W. F. J. M., van Stel, H. F., van Rhenen, W., Stellato, R. K. & Grolman, W. Balancing nurses’ workload in hospital wards: study protocol of developing a method to manage workload. BMJ Open. 6, e012148 (2016).
Rattray, J. et al. Work-related stress: the impact of COVID-19 on critical care and redeployed nurses: a mixed-methods study. BMJ Open. 11, e051326 (2021).
Schouteten, R. Predicting absenteeism: screening for work ability or burnout. Occup. Med. 67, 52–57 (2017).
Ferramosca, F. M. P. et al. Nurses’ organization of work and its relation to workload in medical surgical units: a cross-sectional observational multi-center study. Healthcare. 11, 156–169 (2023).
Miranda, D. R., Moreno, R. & Iapichino, G. Nine equivalents of nursing manpower use score (NEMS). Intensive Care Med. 23, 760–765 (1997).
Kommission Patientenklassifizierung (KPK-CCP). Definition der SGI-Kategorien (2006).
Kommission Datensatz (KDS). Minimaler Datensatz der SGI MDSi (2021).
Riker, R. R., Picard, J. T. & Fraser, G. L. Prospective evaluation of the sedation-agitation scale for adult critically ill patients. Crit. Care Med. 27, 1325 (1999).
Sessler, C. N. et al. The Richmond agitation–sedation scale: validity and reliability in adult intensive care unit patients. Am. J. Respir Crit. Care Med. 166, 1338–1344 (2002).
World Federation of Critical Care Nurses. Position. Statements—Provision Crit. Care Nurs. Workforce (2019).
Musy, S. N. et al. The association between nurse staffing and inpatient mortality: a shift-level retrospective longitudinal study. Int. J. Nurs. Stud. 120, 103950 (2021).
McGraw, K. O. & Wong, S. P. Forming inferences about some intraclass correlation coefficients. Psychol. Methods. 1, 30 (1996).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R Stat. Soc. Ser. B Methdol. 57, 289–300 (1995).
Core Team, R. R: The R Project for Statistical Computing. (2023).
Wickham, H. Ggplot2: Elegant Graphics for Data Analysis (Springer, 2016).
Wickham, H., François, R., Henry, L., Müller, K. & Vaughan, D. dplyr: A Grammar of Data Manipulation. R package version 1.1.2. (2023). https://CRAN.R-project.org/package=dplyr
Wickham, H. et al. Welcome to the Tidyverse. J. Open. Source Softw. 4, 1–6 (2019).
Yoshida, K. et al. tableone: Create ‘Table 1’ to Describe Baseline characteristics with or without Propensity Score Weights (2022).
Zhu, H. et al. kableExtra: Construct Complex Table with ‘kable’ and Pipe Syntax. R package version 1.3.4. (2022).
Sarkar, D. Lattice: Multivariate Data Visualization with R. https://doi.org/10.1007/978-0-387-75969-2 (Springer, 2008).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67, 1–48 (2015).
Stoffel, M. A., Nakagawa, S. & Schielzeth, H. rptR: repeatability estimation and variance decomposition by generalized linear mixed-effects models. Methods Ecol. Evol. 8, 1639–1644 (2017).
Ceballos-Vásquez, P. et al. Psychosocial factors and mental work load: a reality perceived by nurses in intensive care units. Rev. Lat Am. Enfermagem. 23, 315–322 (2015).
Nasirizad Moghadam, K. et al. Nursing physical workload and mental workload in intensive care units: are they related? Nurs. Open. 8, 1625–1633 (2021).
Hartog, C. S. et al. Übertherapie und emotionale Erschöpfung in Der „end-of-life care. Anaesthesist. 67, 850–858 (2018).
Lusignani, M., Giannì, M. L., Re, L. G. & Buffon, M. L. Moral distress among nurses in medical, surgical and intensive-care units. J. Nurs. Manag. 25, 477–485 (2017).
O’Connell, C. B. Gender and the experience of moral distress in critical care nurses. Nurs. Ethics. 22, 32–42 (2015).
Saputera, B. Understanding nurse workload, work stress, and supervision on influence of clinical performance. Soc. Sci. 14 (2020).
Baethge, A., Müller, A. & Rigotti, T. Nursing performance under high workload: a diary study on the moderating role of selection, optimization and compensation strategies. J. Adv. Nurs. 72, 545–557 (2016).
Lebet, R. M. et al. Nurses’ perceptions of workload burden in pediatric critical care. Am. J. Crit. Care. 30, 27–35 (2021).
Kraljic, S. et al. Evaluation of nurses’ workload in intensive care unit of a tertiary care university hospital in relation to the patients’ severity of illness: a prospective study. Int. J. Nurs. Stud. 76, 100–105 (2017).
Riklikiene, O., Didenko, O., Ciutiene, R., Daunoriene, A. & Ciarniene, R. Balancing nurses’ workload: a case study with nurse anaesthetists and intensive care nurses. Econ. Sociol. 13, 11–25 (2020).
Simões, J. L. et al. Nursing workload assessment in an intensive care unit: a 5-year retrospective analysis. J. Clin. Nurs. 30, 528–540 (2021).
Calvo, V. Tiss-28 therapeutic intervention scoring system. IOSR J. Nurs. Health Sci. 9, 41–49 (2020).
Fasoi, G. et al. Assessment of nursing workload as a mortality predictor in intensive care units (ICU) using the nursing activities score (NAS) scale. Int. J. Environ. Res. Public. Health. 18, 1–79 (2020).
Margadant, C. et al. The nursing activities score per nurse ratio is associated with in-hospital mortality, whereas the patients per nurse ratio is not*. Crit. Care Med. 48, 3–9 (2020).
Al-Malki, M., Hawsawi, F., Mleh, R., Tabsh, L. & Mohidin, S. Factors influencing the ICU nurses workload. IOSR J. Nurs. Health Sci. 7, 1–4 (2018).
Guenther, U. et al. Pflegeaufwandsindizes TISS-10, TISS-28 und NEMS: Erhöhter Arbeitsaufwand Bei Agitation Und Delir wird nicht erfasst. Med. Klin. Intensivmed Notfallmedizin. 111, 57–64 (2016).
Miranda, D. R., Nap, R., De Rijk, A., Schaufeli, W. & Iapichino, G. Nursing activities score. Crit. Care Med. 31, 374–382 (2003).
Mazzetti, G. et al. Work engagement: a meta-analysis using the job demands-resources model. Psychol. Rep.. https://doi.org/10.1177/00332941211051988 (2021).
WMA. WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects, vol. 711–714 (World Medical Association General Assembly, 2018).
Acknowledgements
The authors thank all participating CCNs and the SKB for the provision of the QEEW.
Funding
There was no funding of the study. The QEEW2.0 was provided free of charge by the Foundation for Quality Promotion in Occupational Health Care (SKB).
Author information
Authors and Affiliations
Contributions
All authors defined the research question. SF and MTE created the study plan and, with SD, the study framework. MTE and MMJ informed and recruited the CCNs. SF created the online questionnaires and managed the data. SF analysed and interpreted the CCNs’ subjective workload data. SF and MTE collected the objective data. SF and MS carried out the statistical analysis and interpretation. All authors were major contributors in writing the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study followed the Declaration of Helsinki and the Swiss Federal Human Research Act66. In July 2022, the non-competence application was approved by the Ethics Committee in Bern, Switzerland (Req-2022-01231). All data were stored, edited, and analysed on a secured generic shared point platform from the hospital. The data were pseudonymized with a keying instruction for the researchers. All involved researchers had signed a prior confidential agreement. The CCNs’ participation was voluntary and without any advantages or disadvantages. All participating CCNs have signed the informed consent. The CCNs were able to withdraw at any time.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fischbacher, S., Exl, M.T., Simon, M. et al. A prospective longitudinal cohort study of the association between nurses’ subjective and objective workload. Sci Rep 14, 22694 (2024). https://doi.org/10.1038/s41598-024-73637-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-73637-9