Abstract
Lung cancer is a malignant tumor originating from the bronchial mucosa or gland of the lung. Recently, lidocaine, a widely used amide local anesthetic, was demonstrated to inhibit many cancer progression. This research was performed to explore the specific mechanism of lidocaine in the lung cancer progression. The human normal lung epithelial cells (BEAS-2B), and NSCLC cell lines (A549 and H1299) were used and treated with lidocaine in this study. The cell biological behaviors were detected by CCK-8, wound healing and transwell assay. Besides, the mRNA and protein levels of related genes were detected by western blot. The results showed that lidocaine treatment significantly decreased the cell viability and migration of the A549 and H1299 cells. Furthermore, the lidocaine treatment significantly decreased the succinylation and protein levels of HIST1H2BL, which was reversed after SIRT5 knockdown. Additionally, HIST1H2BL knockdown decreased the cell viability and migration of the A549 and H1299 cells, while HIST1H2BL overexpression reversed the effects of lidocaine on the cell viability and migration of the A549 and H1299 cells. In conclusion, lidocaine treatment might inhibited the lung cancer progression through decreasing the SIRT5 mediated succinylation of HIST1H2BL.
Similar content being viewed by others
Introduction
Lung cancer is a malignant tumor originating from the bronchial mucosa or gland of the lung. The mortality rate of lung cancer patients remains high, and about 1.6 million people die of lung cancer every year1,2. Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are two subtypes of lung cancer. NSCLC includes adenocarcinoma, squamous cell carcinoma and large cell carcinoma, accounting for about 85% of all lung cancer patients3. Although the techniques and strategies for treating NSCLC have improved in recent years, the prognosis of the disease is still poor. The 5-year survival rate of NSCLC is only about 15%4. Therefore, finding new drugs and clarifying their potential mechanisms are the basis for developing new therapies for NSCLC.
More and more studies have found that multiple anesthetic drugs can affect the prognosis of tumor patients5,6,7. Lidocaine is a widely used amide local anesthetic. Research showed that lidocaine still has the function of stabilizing the cell membrane, which can play the role of reducing the nerve cell activity by inhibiting the sodium ion channel of the nerve cell membrane, thus protecting the postoperative nerve function of patients8,9. Recently, the research on the effect of intravenous infusion of lidocaine on tumor cells and the acceleration of postoperative rapid recovery has received wide attention10,11. The antitumor role of lidocaine has been demonstrated in vitro, such as in liver cancer12 and cervical cancer13. However, the specific mechanism of lidocaine in lung cancer cells remains unclear.
Succinylation is a newly discovered protein post-translational modifications, which widely exists in cells and can participate in a variety of life activities by regulating protease activity and gene expression14. In the nucleus, more than 1/3 of the nucleosomes have lysine succinylation modifications, including histones and non-histones15. Sirtuin (SIRT) family belongs to nicotinamide adenine dinucleotide (NAD+) - dependent class III deacetylase, which contains seven members of SIRT 1 to 716. Compared with other members of the sirtuin family, SIRT5 not only has weak deacetylase activity, but also has strong desuccinylation due to its larger lysine acyl-binding pocket structure17,18. Recently, SIRT5 has been demonstrated to participate in the lung cancer progression through regulating the cell growth and metastasis19,20. However, whether lidocaine can participate in the occurrence and development of lung cancer by regulating SIRT5-mediated succinylation is still unknown.
Previous study demonstrated that many genes (LTF, ENO1, HSPD1, G6PD, HSPA9, PGD, AIF1, HIST1H2BL and RRBP1) with succinylation sites were abnormally expressed and in the lung cancer21. Here, we found that lidocaine treatment significantly decreased the succinylation and expression of HIST1H2BL. Therefore, we hypothesized that lidocain treatment inhibited the malignant behavior of lung cancer cells through regulating the SIRT5-mediated succinylation of HIST1H2BL.
Materials and methods
Cell culture and treatment
The human normal lung epithelial cells (BEAS-2B), and NSCLC cell lines (A549 and H1299) were obtained from Chinese Academy of Sciences (Shanghai, China). All cells were cultured in the DMEM medium supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin. According to previous22,23 with some modifications. The BEAS-2B, A549 and H1299 cells were treated with 1, 2, 4 mM lidocaine for 24 h to select the appropriate concentration .
Cell transfection
The overexpression vectors (pcDNA 3.1 containing KAT3B, KAT2A, CPT1A, HIST1H2BL), short hairpin RNAs (sh-SIRT5, sh-SIRT7, sh-HIST1H2BL) and their controls were purchased from RiboBio (Guangzhou, China). All these vectors and shRNAs were transfected into the cells using Lipofectamine 2000 (Invitrogen, USA). The transfection efficiency was tested by RT-qPCR assay. The cells were collected for next experiments after 24 h transfection.
Cell viability assay
The cells of each group after treatment were seeded in 96 well plates with a cell density of 4 × 103/well. After 24 h of culture, 10 µL CCK-8 solution (Beyotime, Beijing, China) were added to the each well. After incubation at 37 ℃ for 1.5 h, the absorbance of the cells at the wavelength of 450 nm was detected by a microplate reader.
Wound healing assay
A549 and H1299 cells were cultured in a 6-well plate were scratched with a 100 µL pipette tip to create wounds and cultivated. After 24 h, the wounds were observed using optical microscopy, and the migration distance was calculated.
Transwell assay
A total of 500 µL medium containing 10% FBS was placed in the lower chamber, whereas 200 µL of the cell suspension was placed in the upper chamber. After 24 h, A549 and H1299 cells at the bottom of the transwell membrane were fixed with 4% paraformaldehyde and stained with 0.5% crystal violet. The average number of A549 and H1299 cells in five randomly selected fields under the microscope represented the number of migrated cells.
RT-qPCR
The RNA of cells was extracted using the TRIzol reagent (Invitrogen) according to the reagent guidelines. Then the cDNAs were synthesized using the Prime Script Reverse Transcription Kit (Takara, Tokyo, Japan). SYBR Premix Ex Taq (Takara) was utilized for RT-qPCR analysis in a CFX96 qPCR detection system (Bio-Rad, CA, USA). For mRNA expression levels calculation, glyceraldehyde-3-phosphate dehydrogenase (GAPDH) were used as internal parameters. The relative expression was calculated using the 2-ΔΔCt method. The primers were as follows (5’ -> 3’):
KAT2A, Forward Primer GCAAGGCCAATGAAACCTGTA, Reverse Primer TCCAAGTGGGATACGTGGTCA;
KAT3B, Forward Primer CGAATCGCCGTGAAGAAAGC, Reverse Primer CTTGCAGGCGGAGTACACT;
CPT1A, Forward Primer TCCAGTTGGCTTATCGTGGTG, Reverse Primer TCCAGAGTCCGATTGATTTTTGC;
SIRT5, Forward Primer GCCATAGCCGAGTGTGAGAC, Reverse Primer CAACTCCACAAGAGGTACATCG;
SIRT7, Forward Primer ACGCCAAATACTTGGTCGTCT, Reverse Primer AGCACTAACGCTTCTCCCTTT;
HIST1H2BL, Forward Primer TACAACAAGCGCTCGACCAT, Reverse Primer ATGGTCGAGCGCTTGTTGTA.
GAPDH, Forward Primer TGTGGGCATCAATGGATTTGG, Reverse Primer ACACCATGTATTCCGGGTCAAT.
Western blot
Total protein was extracted using a radioimmunoprecipitation assay buffer and the protein concentration was determined using a BCA kit (Beyotime). After sodium dodecyl sulfate-polyacrylamide gel electrophoresis protein transfer, the transferred membrane was incubated with 5% skimmed milk powder for 1 h; the primary antibodies (succinyl lysine antibody, 1:1200, PTM Bio, Hangzhou, China; anti-LTF, 1:1500, Abcam, USA; anti-ENO1, 1:1000, Abcam; anti-HSPD1, 1:800, Abcam; anti-G6PD, 1:1000, Abcam; anti-HSPA9, 1:1200, Abcam; anti-PGD, 1:600, Abcam; anti-AIF1, 1:1500, Abcam; anti-HIST1H2BL, 1:600, Abcam; anti-RRBP1, 1:1000, Abcam; anti-KAT3B, 1:1000, Abcam; abti-KAT2A, 1:12000, Abcam; anti-CPT1A, 1:1200, Abcam; anti-SIRT5, 1:800, Abcam; anti-SIRT7, 1:1000, Abcam; anti-GAPDH, 1:2500, Abcam) were added and cell were incubated at 4 °C overnight. Then, horseradish peroxidase-labeled rabbit anti mouse secondary antibody (1:2000; Abcam, Cambridge, MA, USA) was added and incubated at 37 °C for 2 h. The images were captured using an ECL detection system (Bio-Rad Laboratories, USA) and quantified using the ImageJ software.
Statistical analysis
The statistical software SPSS 26.0 was used for statistical analysis. The measurement data were expressed as mean ± SD. Each experiment is carried out three times independently. The comparison between the means of multiple samples adopted one-way analysis of variance followed by Tukey’s test, with P < 0.05 indicating a statistically significant difference.
Results
Lidocaine decreased the cell viability of the lung cancer cells
The molecular formula of lidocaine was shown in Fig. 1A. Then the BEAS-2B, A549 and H1299 cells were treated with lidocaine at a dose of 1, 2, 4 mM. The results showed that lidocaine had no effect on cell viability of BEAS-2B cells, which indicated that lidocaine had no side effects on the growth and development of lhuman normal lung epithelial cells (Fig. 1B). However, lidocaine treatment significantly decreased the cell viability of the A549 (Fig. 1C) and H1299 (Fig. 1D) cells in a dose dependent manner. Therefore, 4 mM lidocaine was selected for the next experiment.
Lidocaine decreased the cell viability of the lung cancer cells. BEAS-2B, A549 and H1299 cells were treated with different dose of ldocaine, and cell viability of cells were detected by CCK-8 assay. (A) The molecular formula of ldocaine. The cell viability of the BEAS-2B (B), A549 (C) and H1299 (D) cells were detected by CCK-8 assay after lidocaine (1, 2, 4 mM) treatment. *P < 0.05, **P < 0.01 vs. 0 mM group.
Lidocaine treatment inhibited the cell migration of the lung cancer cells
Then, the transwell and wound healing assays were performed to determine the cell migration ability of the lung cancer cells after lidocaine treatment. We found that lidocaine treatment significantly decreased the wound healing and migrated cells of the A549 (Fig. 2A) and H1299 (Fig. 2B) cells. These results indicated that lidocaine might inhibited the cell metastasis in the lung cancer progression.
Lidocaine treatment inhibited the cell migration of the lung cancer cells. A549 and H1299 cells were treated with 4 mM lidocaine, and cell migration was detected by wound healing and transwell assays. The wound healing (A) and transwell (B) assays were performed to determine the cell migration ability of the lung cancer cells after lidocaine treatment. **P < 0.01 vs. Control group.
Lidocaine decreased the HIST1H2BL levels through regulating the SIRT5 mediated succinylation
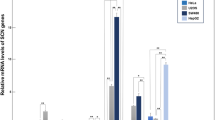
Subsequently, we found that lidocaine treatment significantly decreased the total succinylation levels in the A549 and H1299 cells (Fig. 3A). Previous study demonstrated that many genes (LTF, ENO1, HSPD1, G6PD, HSPA9, PGD, AIF1, HIST1H2BL and RRBP1) with succinylation sites were abnormally expressed and in the lung cancer21. Here, we found that lidocaine treatment significantly significantly decreased the succinylation of HIST1H2BL in the A549 and H1299 cells, while showed no effects on the succinylation of other genes (Fig. 3B). Additionally, the protein expression of HIST1H2BL was significantly decreased in the A549 and H1299 cells after lidocaine treatment (Fig. 3C). Then, the effects of lidocaine on the protein levels of succinyltransferase (KAT3B, KAT2A, CPT1A) and desuccinyltransferase (SIRT5, SIRT7) in A549 and H1299 cells were detected by western blot, which showed that lidocaine had no effects on the protein levels of these genes (Fig. 3D). Furthermore, the transfection efficiency of KAT2A (Fig. 3E), KAT3B (Fig. 3F) and CPT1A (Fig. 3G) overexpressed vector, and sh-SIRT5 (Fig. 3H) and sh-SIRT7 (Fig. 3I) was confirmed by RT-qPCR. After these vectors and shRNAs transfection, we found that just sh-SIRT5 significantly enhanced the protein levels of HIST1H2BL in the lidocaine treated A549 and H1299 cells (Fig. 3J and K). These results indicated that lidocaine decreased the HIST1H2BL protein levels through interacting with SIRT5, which further decreased the succinylation of HIST1H2BL.
Lidocaine decreased the HIST1H2BL levels through regulating the SIRT5 mediated succinylation. A549 and H1299 cells were treated with 4 mM lidocaine. The LTF, ENO1, HSPD1, G6PD, HSPA9, PGD, AIF1, HIST1H2BL and RRBP1 expressions, succinylation related genes expressions, and succinylation levels in cells were detected by western blot assay. (A) The total succinylation of the A549 and H1299 were detected by western blot after lidocaine treatment. (B) The succinylation of LTF, ENO1, HSPD1, G6PD, HSPA9, PGD, AIF1, HIST1H2BL and RRBP1 in the A549 and H1299 were detected by western blot after lidocaine treatment. (C) The protein levels of HIST1H2BL in the A549 and H1299 cells were detected by western blot after lidocaine treatment. (D) The protein levels of succinylation related genes in the A549 and H1299 cells were detected by western blot after lidocaine treatment. (E-I) The transfection efficiency was tested by RT-qPCR. (J-K) The protein levels of HIST1H2BL in the lidocaine treated A549 and H1299 cells were detected by western blot after transfection. **P < 0.01.
HIST1H2BL knockdown decreased the cell viability and migration of the lung cancer cells
Next, the role of HIST1H2BL in the lung cancer cells was further analyzed. The transfection of sh-HIST1H2BL #1 and #2 were detected by RT-qPCR, which showed that HIST1H2BL was significantly decreased after transfection and sh-HIST1H2BL #2 was selected for the next experiments (Fig. 4A). After HIST1H2BL knockdown, the cell viability (Fig. 4B), wound healing (Fig. 4C) and migrated cells (Fig. 4D) were significantly decreased in the A549 and H1299 cells.
HIST1H2BL knockdown decreased the cell viability and migration of the lung cancer cells. A549 and H1299 cells were transfected with sh-HIST1H2BL. CCK-8, wound healing and transwell assays were performed to detect the cell viability and migration. (A) The transfection efficiency of sh-HIST1H2BL #1 and #2 was tested by RT-qPCR. After HIST1H2B knockdown, (B) the cell viability of the A549 and H1299 cells was detected by CCK-8 assay. The wound healing (C) and transwell (D) assays were performed to determine the cell migration ability of A549 and H1299 cells. **P < 0.01.
HIST1H2BL overexpression reversed the role of lidocaine in the lung cancer cells
Finally, the rescue experiments were performed to explore the specific mechanism of lidocaine in A549 and H1299 cells. The transfection of HIST1H2BL was detected by RT-qPCR, which showed that HIST1H2BL was significantly increased after HIST1H2BL overexpressed vector transfection (Fig. 5A). Then we found that HIST1H2BL overexpression significantly enhanced the cell viability (Fig. 5B), wound healing (Fig. 5C & D) and migrated cells (Fig. 5C & E) in the lidocaine treated A549 and H1299 cells.
HIST1H2BL overexpression reversed the role of lidocaine in the lung cancer cells. A549 and H1299 cells were treated with 4 mM lidocaine and transfected with HIST1H2BL overexpressed vectors. CCK-8, wound healing and transwell assays were performed to detect the cell viability and migration. (A) The transfection efficiency of HIST1H2BL overexpressed vector was tested by RT-qPCR. After HIST1H2B overexpression and lidocaine treatment, (B) the cell viability of the A549 and H1299 cells was detected by CCK-8 assay. The wound healing (C & D) and transwell (C & E) assays were performed to determine the cell migration ability of A549 and H1299 cells. **P < 0.01 vs. Control group. ##P < 0.01 vs. lidocaine + vector group.
Discussion
In this study, we found that lidocaine treatment inhibited the cell viability and migration of the lung cancer cells, which was reversed after HIST1H2BL overexpression. Mechanistically, lidocaine decreased the succinylation levels of HIST1H2B through interacting with SIRT5.
Although the therapeutic methods of lung cancer are has gradually improved, with the aging of the population, the incidence rate and mortality of lung cancer are still increasing year by year. Surgical resection is still the main method for the treatment of solid tumors, but the recurrence and metastasis of tumors after surgery are still common24. Recently, Multiple local anesthetics, such as propofol25 and sufentanil26, was found to exhibit the anti-tumor role in many cancers. Lidocaine, a local anesthetic drug derived from cocaine, has also been demonstrated to affect the development of multiple tumors. For example, Sun et al.27 found that lidocaine induced the occurrence of ferroptosis in ovarian as well as breast cancer cells, which revealed the clinical value of lidocaine in ovarian and breast cancer. Besides, Teng et al.28 found that lidocaine suppressed the cell growth and induced the cell apoptosis of the bladder cancer cells through decreasing the isoprenylcysteine carboxylmethyltransferase expression. However, the role of lidocaine in lung cancer has not been reported. In this study, we found that lidocaine treatment showed no side effects on the growth of normal lung epithelial cells, while significantly inhibited the cell viability and migration of lung cancer cells. Similarly, Zhang et al. Also conformed that lidocaine repressed the cell growth of the lung cancer cells through downregulating the golgi transport 1 A expression. These results preliminarily indicated the anticancer effect of lidocaine in lung cancer.
Succinylation modification is a newly discovered post translational modification of proteins, and the research field has developed rapidly in recent years. SIRT5, as a member of the Sirtuins family, was first discovered by Frye et al. in 1999. With the continuous deepening of research, SIRT5 has been found to have the ability to hydrolyze succinyl on lysine in addition to its NAD + dependent deacetylation activity. Recently, SIRT5 mediated succinylation has been demonstrated to participate in multiple cancers progression. For instance, chen et al.29 found that SIRT5 decreased the ACOX1 activity through inhibiting the succinylation, which further suppressed the oxidative stress in the liver cancer development. Kwon et al.30 demonstrated that SIRT5 was decreased in the prostate cancer, and SIRT5 overexpression significantly decreased the lysine 118 succinylation of LDHA, which further decreased the LDHA levels and inhibited the migration and invasion of prostate cancer cells. In our study, we found that lidocaine significantly decreased the total succinylation of the lung cancer cells. Wu et al.21 found that lysine succinylation might be the potential therapeutic target for lung cancers, and they found 9 up-regulated proteins with succinylation sites in lung cancer progression. Therefore, we further analyzed the effects of lidocaine on the succinylation of these proteins in lung cancer cells. Interestingly, we found that lidocaine just decreased the succinylation of HIST1H2BL, and the subsequent experiment further conformed that HIST1H2BL levels were significantly decreased after lidocaine treatment. Then, we found that lidocaine showed no effects on the protein expressions of succinylation related genes, while SIRT5 knockdown reversed the effects of lidocaine of the HIST1H2BL protein levels. There results indicated that lidocaine regulated the HIST1H2BL levels through interacting with SIRT5 instead of modulating it’s expression levels. Additionally, we also demonstrated that HIST1H2BL knockdown inhibited the cell viability and migration of the lung cancer cells and HIST1H2BL overexpression reversed the role of lidocaine in the lung cancer cells.
This study has made innovative discoveries regarding the role of lidocaine in lung cancer. Previous studies have explored the anti-cancer effects of lidocaine, but our work is the first to identify the SIRT5-dependent succinylation pathway as a critical mechanism underlying its action in lung cancer cells. This finding not only elucidates a novel biological pathway but also opens up new therapeutic targets for intervention. In addition, while prior studies have contributed to the basic understanding of lidocaine’s anti-cancer effects, our work bridges the gap between mechanistic insights and clinical implications. By elucidating the precise molecular mechanisms, we pave the way for translating these findings into potential therapeutic strategies for lung cancer patients.
In terms of clinical significance, our research uncovers a novel role for lidocaine, a common local anesthetic, in suppressing the malignancy of lung cancer cells. Basing on chemical structure of the lidocaine, one may design other drugs in future that may achieve the effect of treating lung cancer without anesthetic effect. In addition, our identification of the SIRT5-HIST1H2BL pathway as a target for lidocaine’s anti-cancer action opens doors for personalized medicine. Patients whose lung cancer displays high levels of HIST1H2BL or SIRT5 activity might particularly benefit from lidocaine-based interventions. This could lead to more targeted and effective treatment plans, tailored to the specific genetic and biochemical profiles of individual patients. In furture, we will conduct more animal experiments to further demonstrate the role of lidocaine in NSCLC progression, providing more reliable evidence for the clinical application of lidocaine.
However, there were still some limitations in this study. This study was confined to in vitro cellular experiments aimed at elucidating how lidocaine modulates the aggressive behaviors of lung cancer cells and identifying its molecular targets. While our findings suggest a potential role for lidocaine in regulating the SIRT5/HIST1H2BL signaling pathway, the clinical relevance and specificity of this interaction warrant further exploration. Moreover, the potential for lidocaine to induce off-target effects in non-cancerous cells remains to be thoroughly evaluated.
In conclusion, our study demonstrated that lidocaine might inhibit the lung cancer progression through decreasing the SIRT5 mediated succinylation of HIST1H2BL. The lidocaine/SIRT5/HIST1H2BL axis deserves to be proved in detail for lung cancer treatment.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Bade, B. C. & Dela Cruz, C. S. Lung Cancer : Epidemiology, Etiology, and Prevention. Clin. Chest Med. 41, 1–24 (2020). (2020).
Jonna, S. & Subramaniam, D. S. Molecular Diagnostics and targeted therapies in Non-small Cell Lung Cancer (Nsclc): an update. Discov Med.27, 167 (2019).
Xie, X., Li, X., Tang, W., Xie, P. & Tan, X. Primary Tumor Location in Lung Cancer: the evaluation and administration. Chin. Med. J.135, 127–136 (2021).
Wightman, S. C. et al. Adjuvant chemotherapy for visceral Pleural Invasion in 3-4-Cm non-small-cell lung Cancer improves survival. Eur. J. Cardio-Thorac Surg.62, (2022).
Wang, X. & Li, T. Ropivacaine inhibits the Proliferation and Migration of Colorectal Cancer cells through Itgb1. Bioengineered. 12, 44–53 (2021).
Li, H. et al. Ketamine suppresses proliferation and induces ferroptosis and apoptosis of breast Cancer cells by targeting Kat5/Gpx4 Axis. Biochem. Biophys. Res. Commun.585, 111–116 (2021).
Bai, Z. M. et al. Propofol Inhibited Gastric Cancer Proliferation Via the Hsa-Mir-328-3P/Stat3 pathway. Clin. Transl Oncol.23, 1866–1873 (2021).
Hesketh, L. M. et al. Oct2013, an ischaemia-activated antiarrhythmic Prodrug, devoid of the systemic side effects of Lidocaine. Br. J. Pharmacol.179, 2037–2053 (2022).
Riera, R. et al. Lidocaine for systemic sclerosis: a double-blind Randomized Clinical Trial. Orphanet J. Rare Dis.6, 5 (2011).
Wall, T. P., Crowley, P. D. & Buggy, D. J. The Effect of Lidocaine and Bosutinib on 4T1 murine breast Cancer Cell Behaviour in Vitro. Anticancer Res.41, 2835–2840 (2021).
Guan, E., Liu, H. & Xu, N. Lidocaine suppresses gastric Cancer Development through Circ_Ano5/Mir-21-5P/Lifr Axis. Dig. Dis. Sci.67, 2244–2256 (2022).
Zhao, L. et al. Lidocaine inhibits Hepatocellular Carcinoma Development by modulating Circ_Itch/Mir-421/Cpeb3 Axis. Dig. Dis. Sci.66, 4384–4397 (2021).
Zhu, J. & Han, S. Lidocaine inhibits cervical Cancer Cell Proliferation and induces cell apoptosis by modulating the Lncrna-Meg3/Mir-421/Btg1 pathway. Am. J. Transl Res.11, 5404–5416 (2019).
Yang, Y. & Gibson, G. E. Succinylation Links metabolism to protein functions. Neurochem Res.44, 2346–2359 (2019).
Liu, J., Shangguan, Y., Tang, D. & Dai, Y. Histone succinylation and its function on the nucleosome. J. Cell. Mol. Med.25, 7101–7109 (2021).
Wu, Q. et al. The Sirtuin Family in Health and Disease. Signal. Transduct. Target. Ther.7, 402 (2022).
Sadhukhan, S. et al. Metabolomics-assisted Proteomics identifies Succinylation and Sirt5 as important regulators of cardiac function. Proc. Natl. Acad. Sci. U S A. 113, 4320–4325 (2016).
Kumar, S. & Lombard, D. B. Functions of the Sirtuin Deacylase Sirt5 in normal physiology and pathobiology. Crit. Rev. Biochem. Mol. Biol.53, 311–334 (2018).
Li, Z. et al. Sirt5 promotes Non-small Cell Lung Cancer Progression by reducing Fabp4 Acetylation Level. Neoplasma. 69, 909–917 (2022).
Lu, W., Zuo, Y., Feng, Y. & Zhang, M. Sirt5 facilitates Cancer Cell Growth and Drug Resistance in Non-small Cell Lung Cancer. Tumor Biology. 35, 10699–10705 (2014).
Wu, J. et al. Proteomic Quantification of Lysine Acetylation and Succinylation Profile alterations in lung adenocarcinomas of non-smoking females. Yonago Acta Med.65, 132–147 (2022).
Liu, H., Dilger, J. P. & Lin, J. Lidocaine suppresses viability and Migration of human breast Cancer cells: Trpm7 as a target for some breast Cancer cell lines. Cancers. 13, 234 (2021).
Sun, D., Li, Y. C. & Zhang, X. Y. Lidocaine Promoted Ferroptosis by Targeting Mir-382-5P /Slc7a11 Axis in ovarian and breast Cancer. Front. Pharmacol.12, 681223 (2021).
Chen, Z. et al. Surgical stress and Cancer progression: the twisted Tango. Mol. Cancer. 18, 132 (2019).
Zhao, M. Y., Liu, P., Sun, C., Pei, L. J. & Huang, Y. G. Propofol augments Paclitaxel-Induced Cervical Cancer Cell Ferroptosis in Vitro. Front. Pharmacol.13, 816432 (2022).
Guan, M., Huang, Y. & Lin, X. Sufentanil inhibits the proliferation and epithelial mesenchymal transition of Lung Cancer cells through Wnt/Beta-Catenin signaling pathway. Bioengineered. 13, 10857–10865 (2022).
Sun, D., Li, Y. & Zhang, X. Lidocaine Promoted Ferroptosis by Targeting Mir-382-5P /Slc7a11 Axis in ovarian and breast Cancer. Front. Pharmacol.12, 681223 (2021).
Teng, X., Liu, Y., Wang, L. & Wang, G. Lidocaine exerts anticancer activity in bladder Cancer by Targeting Isoprenylcysteine Carboxylmethyltransferase (Icmt). Transl Androl. Urol.10, 4219–4230 (2021).
Chen, X. F. et al. Sirt5 inhibits peroxisomal Acox1 to prevent oxidative damage and is downregulated in Liver Cancer. Embo Rep.19, (2018).
Kwon, O. K. et al. Sirt5 is the desuccinylase of Ldha as Novel Cancer metastatic stimulator in aggressive prostate Cancer. Genom. Proteom. Bioinform. (2022).
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors participated in the design, interpretation of the studies and analysis of the data and review of the manuscript. X.Chen drafted the work and revised it critically for important intellectual content; ZB.Li and XJ.Yi were responsible for the acquisition, analysis, or interpretation of data for the work; CY Jin made substantial contributions to the conception or design of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, X., Li, Z., Yi, X. et al. Lidocaine inhibits the lung cancer progression through decreasing the HIST1H2BL levels via SIRT5 mediated succinylation. Sci Rep 14, 23310 (2024). https://doi.org/10.1038/s41598-024-73966-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-73966-9
Keywords
This article is cited by
-
Effect of perioperative lidocaine application on inflammatory factors, immune function, and quality of early postoperative recovery in patients undergoing video-assisted thoracoscopic surgery: a randomized controlled trial
European Journal of Medical Research (2025)
-
SIRT5 Inhibits Mitophagy and Inflammation of Hypoxia-Induced Pulmonary Hypertension by Regulating the Desuccinylation of PDK1
Molecular Biotechnology (2025)