Abstract
Reportedly, nausea or vomiting after heavy exercise was associated with post-exercise increased blood calcium (Ca) levels, which was correlated with enhanced bone resorption. We conducted a randomized, double-blind, placebo-controlled trial, enrolling 104 healthy trained male members of the Japan Ground Self-Defense Forces. Risedronate (17.5 mg) or placebo was prescribed 3 and 10 days before heavy exercise lasting approximately 5 h. The primary outcome was the severity of nausea or vomiting assessed by a visual analog scale during or post-exercise. The secondary outcomes included clinical symptoms associated with heat illness, post-exercise serum total Ca (tCa), whole blood ionized Ca (iCa), and serum tartrate-resistant acid phosphatase 5b (TRACP-5b) levels. The mean age was 26 years. The exercise resulted in a 4.5% weight loss. The two groups were comparable in terms of the symptoms, including primary outcome. However, post-exercise tCa and TRACP-5b were significantly lower with risedronate. A similar result was observed for iCa. The post-exercise urinary Ca/Magnesium ratio and the incidence of hypercalcemia (defined as tCa or iCa levels ≥ each median value of all subjects) were significantly lower with risedronate (78.0% vs. 58.5%). A stronger treatment effect of risedronate on blood Ca levels was observed in participants who lost substantial body weight. Post-exercise hypercalcemia is attributed to enhanced bone resorption but not the cause of nausea.
Similar content being viewed by others
Introduction
Gastrointestinal symptoms, such as nausea or vomiting, are commonly related to heavy exercise1. These symptoms have often been attributed to dehydration from heavy physical exertion. Besides, another potential mechanism might include exercise-induced hypercalcemia since we reported an association between exercise-induced hypercalcemia and symptoms of nausea or vomiting2; however, a causal relationship between the symptoms and this phenomenon has not been confirmed.
Exercise-induced hypercalcemia is an increase in blood calcium (Ca) levels during exercise, and it is reportedly associated with bone metabolism3 and hemoconcentration4 in vertebrates. Recently, we reported an association between exercise-induced hypercalcemia and enhanced bone resorption in humans in an observational study2. However, since it was an observational study, a causal relationship could not be proved. Truly, most research reported a decrease in ionized Ca (iCa) after exercise5,6, however, these exercises were not so intensive as our heavy workout.
Accordingly, we postulated that enhanced bone resorption due to heavy exercise7,8,9 may cause hypercalcemia, and this exercise-induced hypercalcemia may be partially responsible for the symptoms of nausea or vomiting during heavy exercise. To evaluate these hypotheses, we conducted an experimental study using the drug risedronate, which inhibits bone resorption. We hypothesized that risedronate may prevent exercise-induced hypercalcemia and the resultant gastrointestinal symptoms. For exercise-induced gastrointestinal symptoms, there are reports of improvement with dietary interventions10,11, but no drug intervention trials. If risedronate improves nausea or vomiting during exercise, it could significantly improve performance and might be a more convenient preventive strategy than just drinking water in a setting of severe exercise soldiers would experience. Notably, the dose of risedronate in this study was set to be a dose not to lower blood Ca levels in healthy subjects12.
A study reported that the incidence of urinary stone formation in New York City marathon runners was 4.5 times greater than in the matched population13. Furthermore, Irving et al. reported that physicochemical properties of calcium crystals in the urine of marathon runners were similar to those of urinary stone formers14. Alendronate was reported to demonstrate a preventive effect on bone loss15 and an increase in urinary Ca16 in astronauts who experience enhanced bone resorption during their stay in space, and it is expected to exhibit a urinary stone-preventive effect. In addition, two RCTs reported the preventive effect of pamidronate on long-term bed-rest-induced urinary stone formation17,18. Risedronate might also contribute to a reduction in urinary Ca/Magnesium (Mg) ratio, which is related to urinary stone formation19,20, via the improvement of exercise-induced hypercalcemia.
Methods
Study design, participants, and protocol
A randomized, double-blind, placebo-controlled, parallel-group trial was conducted, which consisted of three waves (Wave 1–3) to enroll 34, 35, and 35 healthy trained male members (aged 20–39 years) of the Japan Ground Self-Defense Forces, respectively. In each wave, all participants underwent the same training program, which consisted of several sets of 5-day workout drills. On the third day of each set, the participants carried out heavy exercise that was progressively increased in intensity as the set progressed. During the fourth set, the exercise intensity was increased to the maximum level of the training program. The maximum level of heavy exercise began one hour after lunch and lasted for approximately 5 h. The heavy exercise consisted of four different types of workouts with a 15-min interval in between. First, the participants performed a full-body workout and resistance training including push-ups and squats (300 to 400 times each). Second, they ran full seven laps of the 300-m track with obstacles including hurdles, barriers, bunkers, rope climbing, belly crawling, hedgerows, parallel bars, and net climbing. Third, they ran approximately 7 km with a rifle weighing 3.5 kg in their hands. Lastly, they performed a route march with a knapsack weighing 30 kg for an hour. The participants were permitted to take up to 450 mL of water and an unlimited amount of salt during the whole course of heavy exercise by the administrative board2. For the present study, the observation period was from the beginning of set 1 to the morning of the fourth day of set 4 (25th day). All participants ate similar diets at the same time during this period. Baseline blood collection and randomization were performed before the beginning of set 1. The medication was given upon early morning awakening (before breakfast) on the 14th and 21st days, and blood and urine samples were collected before dinner (around 6:00 p.m.) on the 22nd day (8 days after the 1st medication) and within 2.5 h after the maximal level of heavy exercise on the 24th day (10 days after 1st medication). Urine samples were also collected early on the morning (around 6:00 a.m.) of the 25th day (11 days after the 1st medication) (Fig. 1a). This trial was approved by the ethics committee of the Japanese Self-Defense Forces Central Hospital (IRB approval number: 30 − 002) and registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (ID: UMIN000032110) on 4 April 2018 (04/04/2018). (https://www.center6.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000036632) All participants provided written informed consent, and the study was carried out as per the Declaration of Helsinki.
Randomization and intervention
We performed stratified randomization throughout each wave without blocking before the beginning of set 1. An allocation ratio of 1:1 was maintained to receive oral medication either as a risedronate sodium tablet of 17.5 mg or a matching placebo (lactose) tablet on the 14th and 21st days (Fig. 1a). Placing risedronate or placebo in the same white capsule helped prevent identification by both physicians and participants. The manufacturer of risedronate tablets is NIPRO Corp. (Osaka, Japan), and the dosage of risedronate was set to the dose reported not to lower serum Ca levels in healthy subjects12.
Outcomes
The primary study outcome was the severity of nausea or vomiting during or after heavy exercise on the 24th day (10 days after 1st medication). The severity was assessed by a visual analog scale (VAS) (Fig. 1b). The secondary outcomes were clinical symptoms associated with heat illness, levels of serum total Ca (tCa), whole blood iCa, serum tartrate-resistant acid phosphatase-5b (TRACP-5b), and estimated glomerular filtration rate (eGFR) on the 24th day.
Measurements
We collected blood and spot urine samples; the iCa levels of whole blood were measured immediately with Stat Profile® pHOx® Ultra (NOVA Biomedical Corp., Waltham, MA, USA) at the medical office of the participants’ camp. Then, we transferred the centrifuged samples to the Japan Self-Defense Forces Central Hospital for measurement of analytes, except for iCa, by standard automated techniques. Serum tCa and urinary Ca levels were measured using the Arsenazo-III method (coefficient of variation: 5%21). Serum and urinary Mg levels were measured by the xylidyl blue method. TRACP-5b levels were measured with Osteolinks® (SB Bioscience Corp., Tokyo, Japan). Residual samples were stored at − 80 °C until being used for further analyses. Glomerular filtration rate was estimated using the Japanese formula22: 194 × creatinine− 1.094 × age− 0.287. Exercise-induced hypercalcemia was defined as post-exercise tCa or iCa levels above their median values for all participants. Since blood calcium (tCa/iCa) levels decrease within minutes of ending the exercise23, we recorded the time from the end of the exercise to blood collection and examined the correlation between blood Ca levels and the recorded time. Using the coefficient of these correlations, we estimated blood calcium (estimated tCa/iCa) levels immediately after the heavy exercise for a sensitivity analysis.
Sample size calculation
Reportedly, the symptoms of nausea or vomiting during or after heavy exercise were associated with elevated iCa levels, and the probability of nausea or vomiting of 20% (observed prevalence of nausea or vomiting in the previous study) and 5% corresponded to iCa levels of 1.26 and 1.22 mmol/L, respectively, after adjusting for venous blood pH2. In tumor-related hypercalcemia, aminohydroxypropylidene bisphosphonate (APD) has been reported to reduce iCa levels by about 2 mg/dL (0.05 mmol/L) in 7 to 10 days24. Assuming that risedronate reduces the iCa levels after heavy exercise from 1.26 to 1.22 mmol/L, we presume that the incidence of nausea or vomiting will be reduced from 20 to 5%. Based on this assumption, the required sample size to achieve 1:1 randomization was 92 participants (46 in each group) to obtain > 70% power with an alpha level of 0.05. Assuming a dropout rate of 8% from the hard training program, we set a target of 50 participants in each group.
Statistical analysis
Continuous data were presented either as mean and standard deviation or median and interquartile range (IQR), as appropriate. The proportions of participants with clinical symptoms were compared using the Chi-squared or Fisher’s exact test. The VAS scores of nausea or vomiting and serum TRACP-5b were compared using the Mann-Whitney U test. The tCa/iCa levels and eGFR were compared using Student’s t-test.
We conducted several post hoc analyses. We employed linear regression and multivariable linear regression models, incorporating restricted cubic splines with three knots to confirm the associations among plasma arginine vasopressin (AVP), enhanced bone resorption, and exercise-induced hypercalcemia. The urinary Ca/Mg ratio was compared using the Mann-Whitney U test. We employed a mixed-effects linear regression model25 to evaluate the efficacy of risedronate on time-varying urinary N-acetyl-beta-D-glucosaminidase (NAG)/Cr ratio and beta2-microglobulin (beta2MG) levels, which were measured at three time points (Fig. 1a). Additionally, we used a multivariable fractional polynomial interaction (MFPI) analysis to assess the treatment effects of risedronate on tCa/iCa levels26.
All p-values were two-sided, except for the one-sided comparison for the incidence of nausea and vomiting. A p-value of < 0.05 was considered statistically significant. The statistical analyses were performed with Stata/SE 13.0 software (Stata Corp., College Station, TX, USA).
Results
Study participants
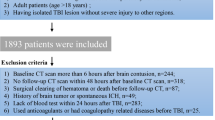
A total of 104 participants were randomized to receive either risedronate (n = 53) or placebo (n = 51). Of these, one participant in the placebo group dropped out before taking medication, leaving 103 participants eligible for an intention-to-treat (ITT) analysis (53 in the risedronate group and 50 in the placebo group) (Fig. 2a,b). There were no significant differences in the baseline data between the two groups (Table 1). During wave 2, six participants missed the 2nd medication (five in the risedronate group and one in placebo). Accordingly, in the per-protocol (PP) analysis, we enrolled 97 participants, excluding these six subjects.
Both study groups demonstrated comparable baseline characteristics (Table 1). The mean age of the participants was 26 (3) years. The maximal level of heavy exercise was carried out when it was sunny and sometimes cloudy with a Wet-Bulb Globe Temperature index of 20–26 °C, 19–24 °C, and 18–21 °C in waves 1, 2, and 3, respectively. After the heavy exercise, the participants experienced a 4.5% (SD: 2.0%) loss of body weight (4.2 [1.9] % with placebo vs. 4.8 [2.1] % with risedronate, p = 0.13 [ITT]), and 95% of participants (n = 98) experienced hypernatremia. The median (IQR) time from the end of the exercise to blood collection was 46 (31–63) minutes, with no difference between the two groups (46.5 [34–66] minutes with placebo vs. 45 [28–60] minutes with risedronate, p = 0.45).
Symptoms associated with heat illness
In the ITT analysis, nausea or vomiting during or after the heavy exercise on the 24th day was observed in 58.0% (29/50) of the placebo group participants and 60.4% (32/53) in the risedronate group; these values exceeded our expected values of 5–20%. However, the median VAS scores for nausea or vomiting indicated mild symptoms (10/100 in placebo and 12/100 in risedronate groups, respectively). Both the prevalence of nausea or vomiting and the VAS scores were not significantly different between the two groups as observed in the ITT analysis (Fig. 3a,b). Similar results were seen in the PP analysis. No significant difference was found between the two groups regarding other symptoms associated with heat illness (Supplementary Information [SI], Table S1).
(a, b) Comparison of (a) the incidence and (b) visual analog scale (VAS) scores of nausea or vomiting during or after the heavy exercise between the two groups in the intention-to-treat (ITT) analyses. (c,d) Comparison of serum total calcium (tCa) levels after the heavy exercise between the two groups in the (c) ITT and (d) per-protocol (PP) analyses.
Ca, TRACP-5b, and eGFR levels
In the ITT analysis, the post-exercise mean (SD) tCa level in the risedronate group was 9.7 (0.5) mg/dL, which was significantly lower than the placebo group (9.9 (0.5) mg/dL, p < 0.05). This result was comparable to the PP analysis (p < 0.01) (Fig. 3c and d). The post hoc analysis showed that exercise-induced hypercalcemia was observed in 78% (39/50) and 58.5% (31/53) in the placebo and risedronate groups, respectively, in the ITT analysis (p < 0.05). A similar result was observed for iCa levels (Table 2).
In a sensitivity analysis, both tCa and iCa levels after the heavy exercise on the 24th day (10 days after 1st medication) were negatively associated with time from the end of the exercise to blood collection (SI, Fig. S1). Using the coefficient of these correlations, we estimated tCa/iCa levels “immediately” after the exercise. The incidence of exercise-induced hypercalcemia in the placebo group was higher when using estimated values than the analysis using raw values (86% [43/50] in the estimated values vs. 78% [39/50] in the raw values). We found similar results regarding group difference for the estimated blood Ca levels immediately after the exercise (Mean [SD]: 10.2 [0.5] mg/dL with placebo vs. 10.0 [0.5] mg/dL with risedronate, p < 0.05 [ITT]) (Table 2).
Serum TRACP-5b levels after heavy exercise were significantly lower in the risedronate group than in the placebo (p = 0.002 for ITT and < 0.001 for PP, respectively) (Table 2). No significant difference was found in the eGFR between the two groups in the ITT or PP analyses (Table 2).
Post hoc analyses
All post hoc analyses were performed using a full analysis set (ITT-based analyses) and estimated blood Ca levels immediately after the exercise. A per-protocol analysis was also performed to compare the post-exercise urinary Ca/Mg ratio. Plasma AVP levels after the heavy exercise were extremely high in both groups and were not significantly different between the two groups (Median: 18.7 [IQR: 12.4–32.2] pg/mL with placebo vs. 20.7 [13.3–26.3] pg/mL with risedronate, p = 0.73). Similar to the previous report2, positive associations were found among plasma AVP levels, percent change in the serum TRACP-5b levels (%∆TRACP-5b), and change in the serum tCa levels (∆tCa) (SI, Fig. S2a and b). Furthermore, the AVP levels were positively associated with the estimated tCa levels immediately after the exercise (p < 0.01) and VAS scores of nausea or vomiting (p < 0.05) in participants experiencing nausea or vomiting (SI, Fig. S2c and d).
The urinary Ca/Mg ratio after heavy exercise on the 24th day was significantly lower in the risedronate group than in placebo (p < 0.05 for ITT and p < 0.01 for PP, respectively) (Fig. 4a and b). No difference was found in the time-varying urinary NAG/Cr ratio or beta2MG levels between the two groups (SI, Table S2).
(a,b) Comparison of urinary calcium/magnesium (Ca/Mg) ratio just after the heavy exercise between the two groups in the (a) ITT and (b) per-protocol (PP) analyses. (c,d) The treatment effects of risedronate on post-exercise blood Ca levels (c: serum total Ca [tCa], d: whole blood ionized Ca [iCa]) against percent change of body weight (%ΔBW). Data were adjusted for wave type and each value before the heavy exercise (8 days after 1st medication). P-values are shown for interaction between %ΔBW and treatment effect. The black lines represent the estimated point at a given level of %ΔBW and the gray areas represent the 95% confidence interval (CI). The cut-offs of (A) and (B) (corresponding to the upper boundary of 95% CI) show the %ΔBW below which risedronate significantly reduced blood Ca levels as compared to placebo.
The MFPI analyses showed a pronounced treatment effect of risedronate on tCa/iCa in participants with substantial bodyweight loss after the heavy exercise on the 24th day (Pinteraction < 0.001 for tCa and < 0.05 for iCa, respectively). A significant effect of risedronate was observed on tCa/iCa levels in participants with weight loss > 6% (Fig. 4c,d), which constituted 21% of total participants.
Adverse effects
During the study period, one participant in the risedronate group experienced gastric discomfort, which resolved spontaneously. There was no incidence of any serious adverse effects.
Discussion
In this double-blind randomized controlled trial, we successfully corroborated the causal relationship between exercise-induced hypercalcemia and enhanced bone resorption since risedronate attenuated the increase in serum total Ca levels significantly after the heavy exercise. Additionally, risedronate decreased urinary Ca/Mg ratio after heavy exercise. However, we could not prove a preventive effect of risedronate on nausea or vomiting by inhibition of exercise-induced hypercalcemia.
Risedronate did not affect nausea or vomiting symptoms. One reason for this may be that the decrease in the serum calcium levels was smaller than anticipated. We presumed that the iCa levels after heavy exercise in the risedronate group would be ~ 0.04 mmol/L lower than that in the placebo group. However, the actual difference in iCa levels was 0.02 mmol/L. At least in the setting of our study, risedronate does not seem to be effective at the dose used for osteoporosis. Perhaps if a more potent antiresorptive had been used, a certain effect might have been observed. Another explanation of this could be that nausea or vomiting observed in the study participants was caused by factors other than elevated blood Ca levels. Four pathways have been reported for the development of nausea or vomiting: stimulation of (1) chemoreceptor trigger zone (CEZ), (2) cerebral cortex, (3) peripheral pathways, or (4) the vestibular system27. Of these, the hypercalcemia causes nausea or vomiting through the CEZ pathway. Heavy exercise also stimulates the peripheral pathway or vestibular system27, and these stimuli may have been more pronounced than the CEZ pathway stimulation caused by elevated blood Ca levels.
Another reason risedronate was ineffective for nausea or vomiting may be the fact that risedronate did not decrease AVP levels. The post hoc analyses showed a positive association between plasma AVP levels and VAS scores of nausea or vomiting in participants with nausea or vomiting during or after heavy exercise. Researchers reported that intravenous AVP causes gastric arrhythmia and nausea in humans28,29. Conversely, some reports exist of AVP secretion in response to artificially-induced nausea by ipecacuanha30 and illusory self-motion31. Thus, the relationship between AVP and nausea seems to be bidirectional, and determining which is the index event is difficult. Further studies are required to explore the causal relationship between AVP and nausea.
In the post hoc analyses, urinary Ca/Mg ratio after heavy exercise on the 24th day was significantly lower in the risedronate group than in placebo (Fig. 4a and b). The urinary Ca/Mg ratio was reported to be higher in stone-formers compared to healthy controls19,20. In addition, it is reported that the urinary Ca/Mg ratio is a better risk factor for silent nephrolithiasis than hypercalciuria in terms of sensitivity and positive predictive value32. Therefore, we compared the urinary Ca/Mg ratio as a stone-related indicator instead of urinary Ca levels. Based on our study, risedronate may be expected to exhibit a preventive effect against urolithiasis in subjects exposed to heavy exercise leading to enhanced bone resorption.
Long-term use of risedronate may be harmful. However, the use in this study was short-term. Some reports showed that bisphosphonate does not affect bone healing time or bone repair in the acute phase of fracture33,34. Although we could not find any rationale for risedronate administration for the improvement of clinical symptoms, it did decrease blood and urinary Ca levels, which may have a preventive effect on renal stones, especially in a setting of enhanced bone resorption sometimes occurring in a heavy workout.
Our study exhibits several limitations. First, we could not measure blood Ca levels just after the heavy exercise. Therefore, we estimated blood calcium levels using coefficients between blood Ca levels and time from the end of heavy exercise. We confirmed similar results in this sensitivity analysis. Second, the enrolled participants were only healthy trained male officers, thereby limiting generalizability to untrained individuals, women, or children. However, this criterion for inclusion precluded the need to consider the effects of female hormones and growth in children. Despite these limitations, our study is the first report to prove the causal relationship between enhanced bone resorption and exercise-induced hypercalcemia. Moreover, we showed that bone resorption was increased in the severe workout. This suggests that fatigue fracture often observed in athletes might be the consequence of repeated enhanced bone resorption. Furthermore, although no significant effect of risedronate was found on the symptoms, this is the first interventional study using bisphosphonate targeting gastrointestinal symptoms during exercise. The double-blind, placebo-controlled design is another strength of this study.
Conclusions
In conclusion, post-exercise hypercalcemia is attributed to enhanced bone resorption but not the cause of nausea or vomit. Risedronate may help decrease the incidence of urinary stones in the setting of heavy exercise via the reduction of urinary Ca/Mg ratio.
Data availability
The dataset of this study is not open to the public due to the data protection policy of the Self-Defense Forces Central Hospital. However, the data can be obtained from the corresponding author upon reasonable request.
References
Costa, R. J. S., Snipe, R. M. J., Kitic, C. M. & Gibson, P. R. Systematic review: Exercise-induced gastrointestinal syndrome—implications for health and intestinal disease. Aliment. Pharmacol. Ther. 46, 246–265 (2017).
Senda, M. et al. Exercise-induced hypercalcemia and vasopressin-mediated bone resorption. Osteoporos. Int. 32, 2533–2541 (2021).
Ruben, J. A. & Bennett, A. F. Intense exercise, bone structure and blood calcium levels in vertebrates. Nature 291, 411–413 (1981).
Aloia, J. F., Rasulo, P., Deftos, L. J., Vaswani, A. & Yeh, J. K. Exercise-induced hypercalcemia and the calciotropic hormones. J. Lab. Clin. Med. 106, 229–232 (1985).
Convertino, V. A., Morey, E. R. & Greenleaf, J. E. Reduction in plasma calcium during exercise in man. Nature 299, 658 (1982).
Kohrt, W. M. et al. Maintenance of serum Ionized Calcium during Exercise attenuates parathyroid hormone and bone resorption responses. J. Bone Min. Res. 33, 1326–1334 (2018).
Langberg, H., Skovgaard, D., Asp, S. & Kjær, M. Time pattern of exercise-induced changes in type I collagen turnover after prolonged endurance exercise in humans. Calcif Tissue Int. 67, 41–44 (2000).
Tsuchiya, Y., Sakuraba, K. & Ochi, E. Effect of eccentric contractions of elbow flexor on bone formation and resorption markers. J. Sports Med. Phys. Fit. 54, 651–657 (2014).
Tsuchiya, Y., Sakuraba, K. & Ochi, E. High force eccentric exercise enhances serum tartrate-resistant acid phosphatase-5b and osteocalcin. J. Musculoskelet. Neuronal Interact. 14, 50–57 (2014).
Lis, D. M., Stellingwerff, T., Kitic, C. M., Fell, J. W. & Ahuja, K. D. K. Low FODMAP: A preliminary strategy to reduce gastrointestinal distress in athletes. Med. Sci. Sports Exerc. 50, 116–123 (2018).
Wiffin, M. et al. Effect of a short-term low fermentable oligiosaccharide, disaccharide, monosaccharide and polyol (FODMAP) diet on exercise-related gastrointestinal symptoms. J. Int. Soc. Sports Nutr. 16, 1–9 (2019).
Mitchell, D. Y. et al. Effect of renal function on risedronate pharmacokinetics after a single oral dose. Br. J. Clin. Pharmacol. 49, 215–222 (2000).
Milvy, P., Colt, E. & Thornton, J. A high incidence of urolithiasis in male marathon runners. J. Sports Med. Phys. Fit. 21, 295–298 (1981).
Irving, R. A., Noakes, T. D., Rodgers, A. L. & Swartz, L. Crystalluria in marathon runners. 1. Standard marathon–males. Urol. Res. 14, 289–294 (1986).
LeBlanc, A. et al. Bisphosphonates as a supplement to exercise to protect bone during long-duration spaceflight. Osteoporos. Int. 24, 2105–2114 (2013).
Okada, A. et al. Bisphosphonate use may reduce the risk of Urolithiasis in astronauts on long-term spaceflights. JBMR Plus 6, 1–10 (2022).
Watanabe, Y. et al. Intravenous pamidronate prevents femoral bone loss and renal stone formation during 90-day bed rest. J. Bone Min. Res. 19, 1771–1778 (2004).
Okada, A. et al. Risk of renal stone formation induced by long-term bed rest could be decreased by premedication with bisphosphonate and increased by resistive exercise. Int. J. Urol. 15, 630–635 (2008).
Schwille, P. O., Schlenk, I., Samberger, N. M. & Bornhof, C. Fasting urine excretion of magnesium, calcium, and sodium in patients with renal calcium stones. Urol. Res. 4, 33–43 (1976).
Leskovar, P., Hartung, R., Siebert, A. & Wellnhofer, E. Urinary magnesium and its relationship to calcium in recurrent stone-formers and controls. Urologe A 19, 214–219 (1980).
Ovsiannikov, A. I. et al. Measurement of calcium content in the blood and other biological fluids by Arsenazo III Complexone. Klin. Lab. Diagn. 1, 16–18 (1999).
Imai, E. et al. Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin. Exp. Nephrol. 11, 41–50 (2007).
Ljunghall, S. et al. Effects of physical exercise on serum calcium and parathyroid hormone. Eur. J. Clin. Invest. 14, 469–473 (1984).
Body, J. J., Magritte, A., Seraj, F., Sculier, J. P. & Borkowski, A. Aminohydroxypropylidene bisphosphonate (APD) treatment for tumor-associated hypercalcemia: A randomized comparison between a 3‐day treatment and single 24‐hour infusions. J. Bone Min. Res. 4, 923–928 (1989).
StataCorp Stata Multilevel mixed-effects Reference Manual (StataCorp LP, 2013).
Royston, P. & Sauerbrei, W. Two techniques for investigating interactions between treatment and continuous covariates in clinical trials. Stata J. 9, 230–251 (2009).
Markowitz, A. J. & Rabow, M. W. Management of intractable nausea and vomiting in patients at the end of life: ‘I was feeling nauseous all of the time… nothing was working’. JAMA - J. Am. Med. Assoc. 299, 1826 (2008).
Kim, M. S., Chey, W. D., Owyang, C. & Hasler, W. L. Role of plasma vasopressin as a mediator of nausea and gastric slow wave dysrhythmias in motion sickness. Am. J. Physiol. Gastrointest. Liver Physiol. 272 (1997).
Caras, S. D., Beverly, V., Lin, Z. & McCallum, R. W. The effect of intravenous vasopressin on gastric myoelectric activity and symptoms in normal subjects. J. Investig. Med. 44, 151–156 (1996).
Page, S. R. et al. The responses of arginine vasopressin and adrenocorticotrophin to nausea induced by ipecacuanha. Clin. Endocrinol. 33, 761–770 (1990).
Koch, K. L., Summy-Long, J., Bingaman, S., Sperry, N. & Stern, R. M. Vasopressin and oxytocin responses to illusory self-motion and nausea in man. Clin. Endocrinol. Metab. 71, 1269–1275 (1990).
Saponaro, F. et al. Hypomagnesuria is Associated with nephrolithiasis in patients with asymptomatic primary hyperparathyroidism. J. Clin. Endocrinol. Metab. 105, 2789–2795 (2020).
Xue, D., Li, F., Chen, G., Yan, S. & Pan, Z. Do bisphosphonates affect bone healing? A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 9, 1–7 (2014).
Gao, Y. et al. The effect of bisphosphonates on fracture healing time and changes in bone mass density: A meta-analysis. Front. Endocrinol. (Lausanne) 12 (2021).
Acknowledgements
We would like to thank members of Japan Self-Defense Forces Central Hospital: Research Department (especially Mrs. Seiji Fujimura, Kenji Okuyama, Michio Nakai, Naoto Onodera, Shigeru Kashiwabara, Masao Chiba, Takashi Suzuki, Ms. Akiko Tanigama, Asumi Kitamura, Drs. Hiroki Omura, Yasunori Mizuguchi, and Shigeto Takeshima) for planning and collecting samples, Clinical Laboratory (especially Mrs. Makoto Nemoto, Tadakazu Osaka, Nobuyoshi Kaito, Daisuke Izumiyama, Akio Nagashima, Ms. Tomomi Hori, Tomoko Takahashi, and Dr. Takao Kubota) for laboratory measurement, Pharmaceutical Department (especially Ms. Hisae Ida and Mr. Kengo Okabe) for medicine preparation, Health Care Center (especially Mr. Masahiro Kato, Ms. Akemi Yagi, and Dr. Susumu Matsukuma) for paperwork, and Department of Gastroenterological Medicine (especially Dr. Shigeaki Aono) for collaboration. We are deeply grateful to members of the Education Department, Japan Ground Self-Defense Forces Medical Serves School (especially Drs. Satoshi Mimura, Mikio Takeshima, and Yoshitaro Matsushita) for their advice. Finally, we would like to express our deepest gratitude and respect to all study participants.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study conceptualization: M.S, T.H, N.F, T.I, Y.I, and T.M. Study design: M.S, T.H, and T.I. Data curation: M.S. Formal analysis: M.S, T.H, and N.F. Manuscript drafting: M.S, T.H, and N.F. Manuscript review/editing: T.H, T.I, Y.I, and T.M. Overall principal investigator of the study: T.H. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Senda, M., Fujii, N., Ito, T. et al. Risedronate prevents exercise-induced hypercalcemia but not nausea or vomit in humans: a double blind randomized controlled trial. Sci Rep 14, 22534 (2024). https://doi.org/10.1038/s41598-024-73985-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-73985-6