Abstract
A single-center, prospective, observational pilot study was performed to evaluate wound healing endpoint and recurrence by measuring transepidermal water loss (TEWL) post-closure at the site of wound repair. Patients with clinically-defined chronic wounds (such as pressure ulcers, diabetic ulcers, and trauma wounds) who visited the Plastic Surgery outpatient department or were in-patients at the All India Institute of Medical Sciences, Rishikesh, India, and were referred for chronic wound management, were enrolled. Non-invasive point-of-care TEWL measurements were obtained, from closed wound-site and contralateral healthy skin site, starting from confirmation of closure (post-closure, V0) continuing every 2 weeks for a maximum of five visits or until the wound recurred. Statistical analyses of the data involved logistic regression and likelihood ratio chi-square tests to assess differences in TEWL at visit 0 (V0) between the closed wound site and reference skin, with the TEWL score as the sole predictor of recurrence. Of the 72 subjects that completed the study, 44 (61%) showed no recurrence and 28 (39%) had wounds that recurred over a period of 12 weeks. A significant association was found between the V0 (post-closure) TEWL score and the odds of wound recurrence, both in univariate analysis (OR [95%CI] = 1.26[1.14,1.42] (p < 0.001) and after adjusting for covariates in multivariable analysis (OR [95%CI] = 1.34[1.19,1.61] (p < 0.001). The likelihood ratio chi-square analysis demonstrated that the V0 TEWL score is a significant universal predictor of recurrence across all wound types studied. Cases of closed wounds with subsequent recurrence showed an overall higher post-closure V0 TEWL score, compared to those who did not have a wound recurrence, across visits. The TEWL score cut-off value predictive of recurrence was 24.1 g.m–2.h–1 (AUC = 0.967). The outcome of this pilot study on a wide range of chronic wounds leads to the hypothesis that post-closure TEWL at the site of wound healing is a reliable biomarker of wound recurrence. It also raises the question whether the clinical endpoint of wound closure should include re-establishment of skin barrier function as additional criterion. The current standard of care wound closure endpoint calls for re-epithelialization of the wound with no discharge for two consecutive weeks disregarding the functional parameter of restoration of skin barrier function at the wound-site.
Similar content being viewed by others
Introduction
Chronic wounds, such as pressure ulcers (PU), diabetic foot ulcers (DFU), venous ulcers, and arterial ulcers, are those that has been open for at least one month1,2. Acute wounds such as burns, traumatic wounds and surgical wounds that progress to chronicity are typically confounded by pathophysiological complications such as infection, immune dysregulation or other factors3. A 2005 community-based epidemiological study identified the prevalence of chronic wounds in India to be 4.5 per 1000 of the population, with lower extremity wounds being the most common4. The situation is further exacerbated in India because of poor access to healthcare, lack of medical insurance, and inadequate healthcare infrastructure4. In the US, the population with chronic wounds (Medicare data) increased by 2.3 million in 2019 compared to 2014. This primarily included PU, DFU and infected surgical wounds5.
Chronic wounds are difficult to heal, and post-closure recurrence pose significant threat1,5,6. The US Food and Drug Administration defines complete wound closure as skin re-epithelialization without drainage or dressing requirements confirmed at two consecutive study visits two weeks apart7. A recurring wound therefore is one that reopens after the two-week window between two consecutive study visits. Several factors contribute to wound recurrence including underlying health conditions such as diabetes, peripheral vascular disease, history of biofilm infection, inadequate wound care, poor nutrition, mechanical stress, and medications such as immunosuppressants that impair wound healing8,9. In the case of DFU it is estimated that 40% of patients have a recurrence within one year after ulcer healing, almost 60% within 3 years, and 65% within 5 years post healing10. A recent systematic review and meta-analysis of 49 studies show that the recurrence rate of diabetic foot ulcers was about 22.1% on average globally11. The clinical significance of wound recurrence is multifaceted and can impact an individual’s health and quality of life significantly. Recurring wounds may lead to extended morbidity, amputation, decreased mobility and decreased quality of life12. It can take a toll on the individual’s mental health leading to diminished overall psychological well-being which in turn impacts their ability to engage in work, social and other activities. Problematic chronic wounds lead to increased risk of complications resulting in limb amputations13which adds significant economic burden14.
Previous studies from our group identified that poor quality of wound closure may contribute to wound recurrence15,16. Wounds infected with bacterial biofilm are likely to close without complete restoration of skin barrier function15,16,17. Transepidermal water loss (TEWL) represents the amount of core body water (as vapor) that escapes from the stratum corneum per area of skin and has historically been used as a dermatological measure of skin barrier integrity15,17,18,19,20,21,22,23. This is a validated measurement used in the context of other skin diseases such as psoriasis and atopic dermatitis, where skin barrier integrity is known to be compromised24. TEWL measurement has been employed to study the progress of epidermal wound healing in pre-clinical15and clinical studies in combination with SoC25,26,27,28,29,30,31. However, the notion that restoration of skin barrier function may be a reasonable functional criterion to define clinical wound closure has not been tested in a clinical setting. The current study utilizes TEWL measurement of repaired skin at the site of wound closure using the DermaLab TEWL open chamber unit (Cortex Technologies, Denmark) as a surrogate marker to study post-closure cutaneous functionality of closed human chronic wounds. The significance of closure associated restoration of barrier function was evaluated as part of a quality index to assess the quality of wound closure. Furthermore, the significance of elevated TEWL at the site of wound closure has been directly tested as a predictor of wound recurrence/recidivism.
Results
Patient demographics: A total of 88 subjects with chronic wounds were recruited for the study between January 2019 and went on till March 2020, with the follow up of patients being done till October 2020. A total of 16 subjects were excluded from the analysis (Fig. 1A). All the remaining (n = 72) subjects completed the study and their data was analyzed. The flowchart of the study design is shown in Fig. 1. Demographics of the subjects are listed in Table 1. A fifth (20.8%) of the 72 subjects who completed the study were female. Almost a quarter (23.6%) were diabetic. Pressure ulcers (55.5%) were the most common type of wound in the cohort studied.
High TEWL score (difference between healed and reference site TEWL values) is associated with wound recurrence
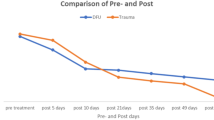
The study design comprised of five visits post-closure of wound (Fig. 1). TEWL measurement was obtained using the DermaLab TEWL open chamber unit. A calibrated DermaLab TEWL probe was placed on the skin and each measurement required about one minute and can be conducted clinical staff with brief prior training. Five measurements were obtained over the healed wound site, at 12, 3, 6, and 9 o’clock around the wound edge, as well as one at the center. Pair-matched reference (control) TEWL measurement was collected from the intact skin at an anatomically matched site or from the patient’s contralateral side. In the study, the center reading was used for calculating TEWL score. TEWL value at the clinically healed site and reference site was collected at each visit or wound recurrence, whichever was earlier. The difference of reading at healed site vs pair-matched reference site TEWL was measured as TEWL score. Over the five visits designed in the study, a decrease in healed site TEWL score was observed in patients with no recurrence compared to those with recurrence (Fig. 2). In subjects with no recurrence, as functional wound closure involving restoration of skin barrier function was achieved, TEWL reading at the healing site decreased approaching reference TEWL. This resulted in TEWL score approaching zero. Such near-zero TEWL score was not common in patients with wound recurrence (Fig. 2A). The box plot data in Fig. 2B showed that there was a clear segregation of subjects into two groups, based on the TEWL score (**p < 0.001; Wilcoxon Rank sum test). In general, the wounds that recurred showed an overall higher TEWL score compared to non-recurring wounds.
High TEWL score at first visit post-closure predicted wound recurrence
Figure 2 supports the contention that closed wounds with higher wound-site TEWL score was predictive of wound recurrence. To test if TEWL score at first-visit post-closure (V0 in Fig. 1B) may predict wound recurrence, a simple logistic regression analyses of wound recurrence was performed. A significant association was observed between the V0 wound site TEWL score and the odds of wound recurrence (OR [95%CI] = 1.26[1.14,1.42] (p < 0.001) in univariate logistic regression (Table 2C). A 1-unit increase in the TEWL score was associated with approximately a 26% increase in the odds of wound recurrence. Multiple regression analysis (OR [95%CI] = 1.34[1.19,1.61] (p < 0.001) also recognized TEWL as a significant predictor of wound recurrence odds (Table 2C). After controlling for covariates (age, gender, BMI, and diabetic status), the odds of wound reopening increase by approximately 34% for every 1-unit increase in the TEWL score (Table 2C). The bigger the initial gap between wound and reference TEWL, the higher were the odds of recurrence (Fig. 3A&B). Initial-visit TEWL scores were analyzed to determine a cutoff value for the purposes of predicting wound recurrence. The optimal cutoff value was determined by finding the mean value with the maximum Youden’s J statistic among 1000 bootstrapped samples of the data. The TEWL score predictive of recurrence was identified as 24.1 g.m–2.h–1 with a sensitivity of 0.928 and specificity of 0.909 (AUC = 0.967) (Fig. 3C). Wound-site TEWL score greater than 24.1 g.m–2.h–1 predicted wound recurrence. In the interest of rigor and reproducibility of the findings, four additional TEWL measurements were taken around the closed wound site at the 12, 3, 6, and 9 o’clock positions along the wound edge, in addition to the measurement at the center, as previously described (Table 3). Spearman correlation analysis showed that the V0 TEWL central value was highly positively correlated with all TEWL values recorded (p < 0.001). Thus, the measurement at the center of the wound was representative of TEWL at 12, 3, 6, 9, o’clock positions.
Difference Between Healed Wound and Reference Site TEWL at First Visit Post-Closure is a Good Predictor of Wound Recurrence. (A) Plot showing estimated recurrence probability based on the difference between wound site and reference site TEWL at visit 0. (B) Chart exhibited increase in probability of recurrence for incremental difference of 10 TEWL values (C) Optimal cut point difference in TEWL for wound site vs reference site at visit 0 post-closure using Youden’s J statistics.
Diabetes and TEWL score are independent predictors of wound recurrence
The study observed that the median (\({Q}_{1}, {Q}_{3}\)) days required for the closed wound to recur was 40 (29.25, 47.0), based on the descriptive statistics in Table 1. Subjects with and without recurrence showed significant differences in clinically recorded wound infections (based on culture results) and the diagnosis of diabetes. Whether these factors may predict wound recurrence odds directly (Table 2A) or through V0 wound site TEWL score as a mediator were tested (Table 2B). Logistic regression models predicting wound recurrence, incorporating clinically tested wound infection and diabetes along with TEWL score as predictors, were evaluated using likelihood ratio chi-square statistics, and statistical significance was determined (Table 2A). The results indicate that both diabetes (p < 0.002) and TEWL (p < 0.0001) (Table 2A) were significant independent predictors of wound recurrence, whereas clinical infection was not a significant predictor (Table 2).
Discussion
The human skin serves the primary function of barrier defense23,32,33,34. Any breach of skin integrity which compromises skin barrier function but does not cause overt structural damage to the skin may be viewed as an invisible wound20. Compromised skin barrier function, with or without overt structural damage to the skin, increases vulnerability to infection and allergens35,36,37,38,39. Several skin diseases such as atopic dermatitis, psoriasis, contact dermatitis, and some specific genetic disorders have been shown to be associated with loss of functional skin barrier24,36. By definition, a skin wound is characterized by structural (defect) and functional (compromised barrier function) loss of skin cover. Typically, wound healing is thought of skin reepithelization with no discharge, i.e. structural recovery. However, functional wound closure23would require that the disrupted barrier function be restored during the course of wound healing. Restoration of skin barrier is critical to enabling host defense15,17. The barrier function of the skin is mediated via junctional proteins and cutaneous lipids32,33,34. Other factors that effect this barrier function of skin are sex, age, skin health, and environmental factors including temperature and humidity40,41,42. Multiple reports have documented that a history of wound biofilm infection leads to compromised restoration of skin barrier function15,17,19,20. Measurement of TEWL to determine the restoration of skin barrier is not common as standardized wound care practice, although it has been employed in clinical studies with patients of psoriasis and atopic dermatitis to assess disease severity24. Non-invasive TEWL measurement can enhance standard care practices in the management of both acute and chronic wounds. Levy et al., studied acute wounds in healthy volunteers using TEWL measurement to evaluate the efficacy of treatments on epidermal regeneration30. In chronic wounds, TEWL measurements have been effective in quantitative assessments of peri-wound skin health as a marker for quality of healing25,28. TEWL has also been shown to be effective in the evaluation of skin barrier function which is critical to limit skin infection and inflammation by inhibiting irritant and immunogen invasion27,29,31. TEWL measurement using appropriately calibrated probes can be done at the point-of-care and could include a single measurement at the wound center. It is simple, rapid and provides an objective assessment of skin health15,18,43. The device is portable and can be deployed across hospitals and even in rural clinics which is critical in a developing country like India. In this pilot study, a qualified wound care provider used a clinically validated device to measure the TEWL score at closed wound sites.
Findings of this pilot study show that wounds that are clinically recognized to be closed do not necessarily restore skin barrier function at the site of repair. Of the 72 patients with chronic wounds studied, 39% of the wounds did not achieve functional wound closure. This questions current standards of clinical wound closure endpoint lending support to the notion that the diagnosis of wound closure should require restoration of barrier function at the wound site. This study supports that TEWL measurement at the site of wound repair is useful in ascertaining the quality of wound closure. To minimize confounding factors such as age, sex and environmental factors, matched reference reading from a non-wounded area of the same subject is useful to determine the TEWL score. TEWL values vary in different anatomical sites of the human body41. For example,the groin area exhibits a higher TEWL compared to the foot44. Baseline TEWL values collected from comparable sites of different individuals may markedly vary because of factors such as age and other factors including skin characteristics of different individuals41,42,44. The approach of using pair-matched reference readings allowed us to account for the variability in wound location. The current study is limited by its small sample size. The study’s post-closure duration was limited to three months, so any wound recurrence occurring beyond this period was not recorded. As the post-closure tissue remodeling phase of wound healing may continue over a year post wound closure45, longer follow up studies should be of value. We posit that bacterial colonization without overt signs of infection is a common but unrecognized contributor to wound chronicity and could be attributed to biofilm infection46. Under such conditions, clinical wound culture may grossly underestimate the microbial bioburden in wounds. The incidence of biofilm in the current cohort of patients was beyond the scope of study and remains unknown. However, mechanistic studies leading to this study clearly showed a direct contribution of biofilm infection to elevated wound-site TEWL15,20. False negative cultures in samples from recurring wounds compared to non-recurring wounds could explain the apparently fewer infections in the recurrent cohort. This is a limitation of the current study but would be an important element to address in future studies. In conclusion, TEWL score of closed wounds predicts recurrence. Results of this study warrant longer multi-site studies involving larger sample size.
Methods
Study design
The study was designed as a single-center, prospective, observational pilot study to evaluate wound healing endpoint and recurrence by post-closure trans epidermal water loss. The study protocol was designed by the authors. The study was done with approval from the Institutional Ethics Committee (AIIMS/IEC/19/1014) at All India Institute of Medical Sciences, Rishikesh, India. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian(s) for study participation and publication. The study was registered in Clinical Trial Registry of India (CTRI/041,766). All original records and data are the property of this institution and therefore under the custody of investigators and wound care providers affiliated to that institution.
Study setting
The study was conducted in the Department of Burns & Plastic Surgery of All India Institute of Medical Sciences, Rishikesh. The overall study duration was around one and a half years. Patient enrolment began in January 2019 and went on till March 2020, with the follow up of patients being done till October 2020. Each patient enrolled with a wound was followed up for a maximum period of 16 weeks (verification of wound chronicity) or until wound healing occurred (Phase A of study). TEWL recordings were started 10 days after wound closure which was marked as Visit 0 (Fig. 1B). The readings were then taken at 2-week intervals (V0-4; phase B of the study) (Fig. 1B). A final study closure visit occurred at 2 weeks post-final TEWL reading (V5). Phase B was for a total of ~ 12 weeks.
Participants
Patients with open wounds visiting the Plastic Surgery out-patient department and in-patients of AIIMS Rishikesh referred for wound management were enrolled. Patients enrolled in the study were subjected to Standard of Care (SoC) until wound closure. Most of the patients achieved wound closure within 16 weeks (following wound chronicity definition, i.e., open at 16 weeks), which was proposed as phase A of the study. Phase B of the study began 10 days after closure of the wound. The total length of this phase was ~ 12 weeks (Fig. 1B). Measurement of TEWL at the post-closure wound site and corresponding normal unaffected skin of the same individual were performed every 2 weeks for a maximum of five visits (V0-4; Fig. 1B) or until the wound recurred. The subjects returned for a final visit (V5; Fig. 1B) 2 weeks after the final TEWL measurement was taken.
Inclusion criteria
-
(1)
Chronic wound of multiple etiologies open for at least 30 days, including:
-
(i)
Diabetic foot ulcers, Wagner grade 1–3
-
(ii)
Pressure ulcers, stage 1–3
-
(iii)
Venous leg ulcers, confirmed by venous duplex
-
(iv)
Burn wounds
-
(v)
Other etiology
-
(i)
-
(2)
In cases where wounds were located below the knee, Ankle Brachial Index should be greater than 0.7.
Exclusion criteria
-
(1)
Individuals who are deemed unable to provide informed consent
-
(2)
Diabetics with Hemoglobin A1c > 10%
-
(3)
Subjects with marked immunodeficiency (HIV/AIDS, organ transplant patients and cancer patients and patients with autoimmune disease on immunosuppressive medications)
-
(4)
Wounds closed or to be closed by flap or graft coverage—including stage 4 pressure ulcers and Wagner grade 4 or 5 diabetic foot ulcers
-
(5)
Prisoners
Study procedure
-
1.
Phase A
In the initial visit, after wound assessment, HbA1c and ABI were determined to confirm inclusion into the study. Once inclusion criteria were determined, the patient was explained the study procedure and informed consent along with demographic data were recorded. Wound data was recorded regarding etiology, size, location, duration, erythema, and drainage. During the 16 weeks of this phase of the study the number of debridement, culture and sensitivity reports of wound swab were also recorded. Once the wound healed on visual inspection by the plastic surgeon the patient was shifted to phase B of the study (Fig. 1B). All patients enrolled in this study (except for the 16 who were excluded (Fig. 1A) had their wounds close within 16 weeks and continued to phase B.
-
2.
Phase B (Fig. 1B)
This phase began 10 days after the plastic surgeon deemed the wound closed on visual inspection. During this phase TEWL measurements were obtained every 2 weeks (V0-4). The total duration of phase B was 80 days. In cases where the wound recurred within 80 days, the participant was recorded under ‘wound recurrence’ group. In cases where no recurrence occurred for the duration of phase B the participant was classified as ‘no recurrence’ group. The primary outcome was to evaluate whether TEWL score at the wound-site post-closure may detect a faulty barrier of the skin in clinically closed wounds.
Sample size
As evident in CONSORT diagram (Fig. 1), a total of 88 subjects with chronic wounds were enrolled at the All India Institute of Medical Sciences, Rishikesh, India under the institutional approved protocol # AIIMS/IEC/19/1014. Of these, 15 subjects were excluded as they were lost to follow up. One subject was excluded because the wound recurred within the 2-week window post closure (following FDA definition7). The statistical analysis therefore was performed on data from 72 subjects of which 44 did not have recurrence and 28 had wounds that recurred. Descriptive statistics are shown in Table 1.
Trans-epidermal water loss (TEWL) measurement: TEWL is defined as the flux of water, which diffuses from the epidermis through the stratum corneum to the skin surface. DermaLab Combo™ (Cortex technologies, Denmark) was used to measure the trans-epidermal water loss from the healed wounds. It is based on open chamber TEWL measurement. TEWL was measured in g (m2)-1 h-1. Dermalab Combo comprises a measuring unit with a computer and a sensor probe. The TEWL probe has hygro sensors located in perpendicular orientation, TEWL is determined from the humidity gradient between the sensors. The probe is placed on the skin surface. The evaporated water released from the skin is detected by the sensors in the probe and measured to provide the TEWL value. The probe must be routinely calibrated and such calibration may be perturbed by accidently dropping the probe on the floor or such as mechanical shock.
Statistical analyses
The statistical analysis was performed using the R Software version 4.2.2. The frequency and percentage were calculated for categorical values, whereas median and \({Q}_{1}\& {Q}_{3}\) were calculated for continuous values. The inferential statistics with Chi-square/Wilcoxon rank sum test was conducted with p-value set at p < 0.05 for the following variables: age in years, gender, wound culture, diabetic status, would closure to reopening time with and without recurrence. Correlation method used for different location measurement of TEWL for V0. Analysis was done using TEWL score i.e. the difference in TEWL of the healed wound vs reference site. Univariate analysis was conducted to identify significant differences wound recurrences with visit 0 TEWL score as the sole predictor. The multivariable logistic regression analysis was performed to test significance of TEWL score in predicting wound recurrence produced under conditions where the following variables were controlled: patient age, gender, BMI and diabetic status. Logistic regression analysis results are expressed as odds ratio (OR) value, 95% confidence interval (95% CI), p value. All results, univariate and multivariable, are statistically significant with p< 0.05. Significant predictor variables were determined using the likelihood ratio Chi-square statistics for logistic regression models47,48. An optimal cutoff value was estimated for the purposes of predicting wound recurrence using mean value with the maximum Youden’s J statistic49 (which is just sensitivity + specificity—1) among 1000 bootstrapped samples of data.
Data availability
The datasets generated and/or analyzed during the current study supporting are not publicly available to protect patient privacy but are available from the corresponding author on reasonable request.
References
Frykberg, R. G. & Banks, J. Challenges in the treatment of chronic wounds. Adv. Wound Care (New Rochelle) 4, 560–582. https://doi.org/10.1089/wound.2015.0635 (2015).
Kottner, J. et al. Prevention and treatment of pressure ulcers/injuries: The protocol for the second update of the international Clinical Practice Guideline 2019. J. Tissue Viability 28, 51–58. https://doi.org/10.1016/j.jtv.2019.01.001 (2019).
Liu, Y. F., Ni, P. W., Huang, Y. & Xie, T. Therapeutic strategies for chronic wound infection. Chin. J. Traumatol. 25, 11–16. https://doi.org/10.1016/j.cjtee.2021.07.004 (2022).
Shukla, V. K., Ansari, M. A. & Gupta, S. K. Wound healing research: a perspective from India. Int. J. Low. Extrem. Wounds 4, 7–8. https://doi.org/10.1177/1534734604273660 (2005).
Sen, C. K. Human wound and its burden: Updated 2022 compendium of estimates. Adv. Wound Care (New Rochelle) 12, 657–670. https://doi.org/10.1089/wound.2023.0150 (2023).
Darwin, E. & Tomic-Canic, M. Healing chronic wounds: Current challenges and potential solutions. Curr. Dermatol. Rep. 7, 296–302. https://doi.org/10.1007/s13671-018-0239-4 (2018).
US Department of Health and Human Services, F. Guidance for industry: Chronic cutaneous ulcer and burn wounds-developing products for treatment, <http://www.fda.gov/ucm/groups/fdagov-public/@fdagov-drugs-gen/documents/document/ucm071324.pdf> (2006).
Diban, F. et al. Biofilms in chronic wound infections: Innovative antimicrobial approaches using the in vitro lubbock chronic wound biofilm model. Int. J. Mol. Sci. https://doi.org/10.3390/ijms24021004 (2023).
Anderson, K. & Hamm, R. L. Factors that impair wound healing. J. Am. Coll. Clin. Wound Spec 4, 84–91. https://doi.org/10.1016/j.jccw.2014.03.001 (2012).
Armstrong, D. G., Boulton, A. J. M. & Bus, S. A. Diabetic foot ulcers and their recurrence. N. Engl. J. Med. 376, 2367–2375. https://doi.org/10.1056/NEJMra1615439 (2017).
Fu, X. L. et al. Global recurrence rates in diabetic foot ulcers: A systematic review and meta-analysis. Diabetes Metab. Res. Rev. 35, e3160. https://doi.org/10.1002/dmrr.3160 (2019).
Sen, C. K. Human wound and its burden: Updated 2020 compendium of estimates. Adv. Wound Care (New Rochelle) 10, 281–292. https://doi.org/10.1089/wound.2021.0026 (2021).
Madsen, U. R., Hyldig, N. & Juel, K. Outcomes in patients with chronic leg wounds in Denmark: A nationwide register-based cohort study. Int. Wound J 19, 156–168. https://doi.org/10.1111/iwj.13607 (2022).
Olsson, M. et al. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen. 27, 114–125. https://doi.org/10.1111/wrr.12683 (2019).
Roy, S. et al. Mixed-species biofilm compromises wound healing by disrupting epidermal barrier function. J. Pathol. 233, 331–343. https://doi.org/10.1002/path.4360 (2014).
Roy, S. et al. Staphylococcus aureus biofilm infection compromises wound healing by causing deficiencies in granulation tissue collagen. Ann. Surg. 271, 1174–1185. https://doi.org/10.1097/sla.0000000000003053 (2020).
Sinha, M. et al. Pseudomonas aeruginosa theft biofilm require host lipids of cutaneous wound. Ann. Surg. 277, e634–e647. https://doi.org/10.1097/SLA.0000000000005252 (2023).
Alexander, H., Brown, S., Danby, S. & Flohr, C. Research techniques made simple: Transepidermal water loss measurement as a research tool. J. Invest. Dermatol. 138, 2295-2300 e2291. https://doi.org/10.1016/j.jid.2018.09.001 (2018).
Barki, K. G. et al. Electric field based dressing disrupts mixed-species bacterial biofilm infection and restores functional wound healing. Ann. Surg. 269, 756–766. https://doi.org/10.1097/sla.0000000000002504 (2019).
El Masry, M. et al. Swine model of biofilm infection and invisible wounds. J. Vis. Exp. https://doi.org/10.3791/65301 (2023).
Ghatak, S. et al. Barrier function of the repaired skin is disrupted following arrest of dicer in keratinocytes. Mol. Ther. 23, 1201–1210. https://doi.org/10.1038/mt.2015.65 (2015).
Li, J. et al. Topical lyophilized targeted lipid nanoparticles in the restoration of skin barrier function following burn wound. Mol. Ther. 26, 2178–2188. https://doi.org/10.1016/j.ymthe.2018.04.021 (2018).
Sen, C. K. & Roy, S. The hyperglycemia stranglehold stifles cutaneous epithelial-mesenchymal plasticity and functional wound closure. J. Invest. Dermatol. 141, 1382–1385. https://doi.org/10.1016/j.jid.2020.11.021 (2021).
Montero-Vilchez, T. et al. Skin barrier function in psoriasis and atopic dermatitis: Transepidermal water loss and temperature as useful tools to assess disease severity. J. Clin. Med. https://doi.org/10.3390/jcm10020359 (2021).
Bernatchez, S. F. & Bichel, J. The science of skin: Measuring damage and assessing risk. Adv. Wound Care (New Rochelle) 12, 187–204. https://doi.org/10.1089/wound.2022.0021 (2023).
Czaika, V. et al. Comparison of transepidermal water loss and laser scanning microscopy measurements to assess their value in the characterization of cutaneous barrier defects. Skin Pharmacol. Physiol. 25, 39–46. https://doi.org/10.1159/000330486 (2012).
Danielsen, P., Jørgensen, B., Karlsmark, T., Jorgensen, L. N. & Ågren, M. S. Effect of topical autologous platelet-rich fibrin versus no intervention on epithelialization of donor sites and meshed split-thickness skin autografts: a randomized clinical trial. Plast. Reconstr. Surg. 122, 1431–1440. https://doi.org/10.1097/PRS.0b013e318188202c (2008).
Dini, V., Salibra, F., Brilli, C. & Romanelli, M. Instrumental evaluation of the protective effects of a barrier film on surrounding skin in chronic wounds. Wounds 20, 254–257 (2008).
Koskela, M. et al. Epidermal wound healing in severe sepsis and septic shock in humans. Crit. Care 13, R100. https://doi.org/10.1186/cc7932 (2009).
Lévy, J. J., von Rosen, J., Gassmüller, J., Kleine Kuhlmann, R. & Lange, L. Validation of an in vivo wound healing model for the quantification of pharmacological effects on epidermal regeneration. Dermatology 190, 136–141. https://doi.org/10.1159/000246663 (1995).
Maarouf, M., Maarouf, C. L., Yosipovitch, G. & Shi, V. Y. The impact of stress on epidermal barrier function: An evidence-based review. Br. J. Dermatol. 181, 1129–1137. https://doi.org/10.1111/bjd.17605 (2019).
Lee, S. H., Jeong, S. K. & Ahn, S. K. An update of the defensive barrier function of skin. Yonsei Med. J. 47, 293–306. https://doi.org/10.3349/ymj.2006.47.3.293 (2006).
Natsuga, K. Epidermal barriers. Cold Spring Harb. Perspect. Med. 4, a018218. https://doi.org/10.1101/cshperspect.a018218 (2014).
Proksch, E., Brandner, J. M. & Jensen, J.-M. The skin: An indispensable barrier. Exp. Dermatol. 17, 1063–1072. https://doi.org/10.1111/j.1600-0625.2008.00786.x (2008).
De Benedetto, A., Kubo, A. & Beck, L. A. Skin barrier disruption: A requirement for allergen sensitization?. J. Invest. Dermatol. 132, 949–963. https://doi.org/10.1038/jid.2011.435 (2012).
Agrawal, R. & Woodfolk, J. A. Skin barrier defects in atopic dermatitis. Curr. Allergy Asthma. Rep. 14, 433. https://doi.org/10.1007/s11882-014-0433-9 (2014).
Goleva, E., Berdyshev, E. & Leung, D. Y. M. Epithelial barrier repair and prevention of allergy. J. Clin. Investig. 129, 1463–1474. https://doi.org/10.1172/JCI124608 (2019).
Knaysi, G., Smith, A. R., Wilson, J. M. & Wisniewski, J. A. The skin as a route of allergen exposure: Part II. Allergens and role of the microbiome and environmental exposures. Curr. Allergy Asthma Rep. 17, 7. https://doi.org/10.1007/s11882-017-0675-4 (2017).
Smith, A. R., Knaysi, G., Wilson, J. M. & Wisniewski, J. A. The skin as a route of allergen exposure: Part I. immune components and mechanisms. Curr. Allergy Asthma Rep. 17, 6. https://doi.org/10.1007/s11882-017-0674-5 (2017).
Firooz, A. et al. Variation of biophysical parameters of the skin with age, gender, and body region. Sci. World J. 2012, 386936. https://doi.org/10.1100/2012/386936 (2012).
Honari, G. & Maibach, H. in Applied Dermatotoxicology (eds Howard Maibach & Golara Honari) 1–10 (Academic Press, 2014).
Green, M., Kashetsky, N., Feschuk, A. & Maibach, H. I. Transepidermal water loss (TEWL): Environment and pollution-A systematic review. Skin Health Dis. 2, e104. https://doi.org/10.1002/ski2.104 (2022).
Uehara, O., Kusuhara, T. & Nakamura, T. transepidermal water loss estimation model for evaluating skin barrier function. Adv. Biomed. Eng. 12, 1–8. https://doi.org/10.14326/abe.12.1 (2023).
Bhargava, P., Singdia, H., Nijhawan, S., Mathur, D. K. & Bhargava, R. K. A study of biophysical profile of inguinal skin: An implication for health and disease. Indian J. Sex. Transm. Dis. AIDS 42, 7–13. https://doi.org/10.4103/ijstd.IJSTD_101_19 (2021).
Spielman, A. F. et al. Beyond the scar: A basic science review of wound remodeling. Adv. Wound Care (New Rochelle) 12, 57–67. https://doi.org/10.1089/wound.2022.0049 (2023).
Sen, C. K., Roy, S., Mathew-Steiner, S. S. & Gordillo, G. M. Biofilm management in wound care. Plast. Reconstr. Surg. 148, 275e–288e. https://doi.org/10.1097/prs.0000000000008142 (2021).
Bewick, V., Cheek, L. & Ball, J. Statistics review 14: Logistic regression. Crit. Care 9, 112–118. https://doi.org/10.1186/cc3045 (2005).
Hosmer, D. W., Taber, S. & Lemeshow, S. The importance of assessing the fit of logistic regression models: A case study. Am. J. Public Health 81, 1630–1635. https://doi.org/10.2105/ajph.81.12.1630 (1991).
Youden, W. J. Index for rating diagnostic tests. Cancer 3, 32–35. https://doi.org/10.1002/1097-0142(1950)3:1%3c32::aid-cncr2820030106%3e3.0.co;2-3 (1950).
Acknowledgements
The clinical study was performed at the All-India Institute of Medical Sciences (AIIMS), Rishikesh, Uttarakhand, India. All original records and data are the property of this institution and therefore requests related to the study itself can be addressed to the co-corresponding author – Dr. Chattopadhyay. The authors acknowledge the initial efforts of Cameron Colgate in statistical analysis conducted on the data.
Author information
Authors and Affiliations
Contributions
The contribution of the authors was as follows: study concept and design: D.C, M.S, C.K.S acquisition of data: D.C, A.K.; data analysis: M.K, interpretation of data: M.S, C.K.S, S.M.S, K.S, M.K, and manuscript draft: S.M.S, M.S, D.C, A.K, M.K, K.S, C.K.S.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chattopadhyay, D., Sinha, M., Kapoor, A. et al. Deficient functional wound closure as measured by elevated trans-epidermal water loss predicts chronic wound recurrence: An exploratory observational study. Sci Rep 14, 23593 (2024). https://doi.org/10.1038/s41598-024-74426-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-74426-0