Abstract
Hormone receptor-positive breast cancer (BC) is the most prevalent subtype of BC and is generally correlated with a favorable prognosis. This study aimed to determine the incidence and survival trends among women diagnosed with hormone receptor-positive BC between 1990 and 2019. Female patients with hormone receptor-positive BC for calendar years 1990–2019 were obtained from the Surveillance, Epidemiology, and End Results (SEER) database and categorized into six diagnostic groups according to the year of diagnosis. Age-adjusted incidence rates (IRs) were calculated using joinpoint regression. We used the Kaplan–Meier method and multivariate Cox regression analyses to determine the association between diagnostic groups, and overall survival (OS) and BC-specific survival (BCSS). The final analysis included 370,729 women, among whom 37,943 (10.2%), 49,266 (13.3%), 55,652 (15.0%), 64,451 (17.4%), 77,127 (20.8%), and 86,290 (23.3%) were diagnosed between 1990 and 1994, 1995–1999, 2000–2004, 2005–2009, 2010–2014, and 2015–2019, respectively. Within the overall cohort, IRs gradually increased from 70 per 100,000 in 1990 to 113 per 100,000 in 2019 (average annual percent change, 1.59%; 95% CI, 1.18–1.99). Multivariate Cox regression analysis revealed that the survival outcomes gradually improved over nearly three decades among hormone receptor-positive BC patients, with a 0.8% and 1.3% decrease in risk for all-cause and BC-specific mortality each year, respectively. Compared to 1990–1994, hormone receptor-positive BC patients diagnosed in 2015–2019 had a 22% lower risk of all-cause death (hazard ratio [HR], 0.78; 95% CI, 0.76–0.81) and a 27% lower risk of BC-specific death (HR, 0.73; 95% CI, 0.70–0.76). The development of treatment strategies within the past three decades, especially endocrine therapy, may contribute to the continuous improvement of clinical outcomes in patients with hormone receptor-positive BC.
Similar content being viewed by others
Introduction
Breast cancer (BC) is the most frequent cancer worldwide, and BC alone accounts for 30% of all cancers in women1. According to the latest statistics for the US populations, women have a 13% risk of developing BC in their lifetime, and approximately 287,850 new cases of BC are expected in 20222. The overall BC incidence has had a steep increase over the present decade3. Indeed, the increasing trends have largely been driven by increases in hormone receptor-positive tumors3, which are the most common subtype of BC and account for approximately 70% of all BCs3,4,5,6,7. Therefore, hormone receptor-positive BC is a significant public health concern, especially among the female population.
The steroid hormone receptor status, including expression of the estrogen receptor (ER) and progesterone receptor (PR), is a crucial factor predicting the benefit of endocrine therapy (ET) among BC patients8,9,10,11,12. BC is categorized into three major clinical subtypes based on the presence or absence of molecular markers for ER/PR and human epidermal growth factor 2 (HER2), all of which have different treatment approaches, as follows: hormone receptor-positive/HER2-negative, HER2-positive, and hormone receptor-negative/HER2-negative (triple negative breast cancer)13. Adjuvant tamoxifen for at least 5 years is the standard adjuvant ET strategy for low-risk peri- and pre-menopausal hormone receptor-positive BC patients14,15. There is an approximate 50% reduction in risk of recurrence and a 30% risk of BC mortality after the first 5 years (the treatment period) of diagnosis using this standard strategy among hormone receptor-positive patients compared to no ET16.
Over the past several decades, advances in therapies have resulted in survival benefits for patients with hormone receptor-positive BC. The Breast International Group 1–98 trial demonstrated that postmenopausal women who received third-generation aromatase inhibitors, including anastrazole, exemestane, and letrozole, had a significantly higher 5-year disease-free survival compared with tamoxifen (84.0% vs. 81.4%) and a 27% reduction in the risk of distant recurrence17. The addition of fulvestrant, an ER down-regulator, to anastrozole prolonged the overall survival by 7.8 months compared with anastrozole alone18. With the advent of targeted therapy, the combination of palbociclib, a cyclin-dependent kinase 4/6 (CDK 4/6) inhibitor, with ET significantly extended the progression-free survival (PFS) by 10 months in hormone receptor-positive/HER2-negative BC19. Furthermore, the phosphatidylinositol 3-kinase (PI3K)/AKT (known as protein kinase B)/mammalian target of rapamycin (mTOR) pathway is involved in the maintenance of ET resistance and has become the target for many new drugs in the treatment of ER-positive BC20. These data indicate that the prognosis for patients with hormone receptor-positive BC has improved with advances in ET and the introduction of targeted drugs (i.e., CDK 4/6, mTOR, AKT, vascular endothelial growth factor receptors [VEGF], and PI3K inhibitors) over the past several decades;21,22 however, the pattern of long-term survival outcomes among patients with hormone receptor-positive BC have not been systematically described so far.
In this retrospective study, we determined whether there has been a stepwise improvement in the prognosis among patients with hormone receptor-positive BC from 1990 to 2019 based on the Surveillance, Epidemiology, and End Results (SEER) database population, reflecting the advances in ET and the introduction of targeted drugs regimens that have been approved by the United States Food and Drug Administration (US FDA). We believe that these findings are helpful for enhancing physicians’ and patients’ understanding to the survival pattern of hormone receptor-positive breast cancer, and may also provide critical evidence for the development of treatment strategies for hormone receptor-positive breast cancer.
Methods
Patient population
We used data extracted from population registries participating in the National Cancer Institute (NCI) SEER database (Incidence-SEER Research Plus Data, 8 Registries, Nov 2021 Sub [1975–2019], the most years available) registry that was released in April 2022 (SEER ∗Stat, 8.4.0.1) and represents approximately 8.3% of the US population23. Given that the SEER is a public database that can be freely accessed by researchers worldwide, the Institutional Ethics Committee of the First Affiliated Hospital of Chongqing Medical University Review Board deemed this study exempt from approval and written informed consent from patients. The date of data analysis began on 1 November 2022 and ended on 10 September 2023.
Participants were restricted to female patients with hormone receptor-positive BC diagnosed between 1975 and 2019. Because information on hormone receptor status was first documented by SEER registries in 1990, and we thus excluded patients who were diagnosed with BC before 1990. A total of 508,283 females residing in the San Francisco-Oakland SMSA, Connecticut, Hawaii, Iowa, New Mexico, Seattle, Utah, and Atlanta areas were originally identified. The information on year of diagnosis, age at the time of diagnosis, race, marital status at the time of diagnosis, ER status, PR status, tumor grade, stage, lymph node status, radiation therapy status, chemotherapy status, cause of death, and duration of survival in months were extracted from the SEER database. We focused on the hormone receptor-positive BC subgroups, excluding a total of 132,949 patients with missing ER or PR (not both) status and diagnosed as ER-negative/PR-negative BC. In parallel, patients without a SEER cause-specific death classification (n = 1861) and 2744 patients with 0 months or an unknown duration of survival were excluded from final analysis (Fig. 1). Finally, data from 370,729 female patients with hormone receptor-positive BC were included in this retrospective population-based study. The American Society of Clinical Oncology (ASCO) and the American Society of Pathologists (CAP) guidelines proposed to redefine hormone receptor-positive as > 1% tumor expressing positive nuclei in 201021,24. Because tumor cell nucleus information was not collected in the SEER database, all female BC patients with a molecular subtype described as ER-negative/PR-positive, ER-positive/PR-negative, or ER- and PR-positive were defined as hormone receptor-positive patients8. Therefore, we divided the patients into ER-positive/PR-positive (n = 308,672), ER-positive/PR-negative (n = 54,709), and ER-negative/PR-positive (n = 7348) according to ER/PR status. We categorized the year of diagnosis based on 5-year intervals; thus, all female patients diagnosed with hormone receptor-positive BC were divided into six diagnostic groups according to the year of diagnosis, as follows: (a) 1990–1994, (b) 1995–1999, (c) 2000–2004, (d) 2005–2009, (e) 2010–2014, and (f) 2015–2019. A systematic comparison was made of survival trends among hormone receptor-positive BC subtypes according to the 30-year study period from 1990 to 2019.
Statistical analysis
The changes in demographic and clinicopathologic characteristics of patients with hormone receptor-positive BC were compared according to the year of diagnosis group using the Mantel–Haenszel test. The annual mean age-adjusted standardized incidence rate (IR) per 100,000 population (i.e., 2000 US standard population) for women with hormone receptor-positive BC was calculated using SEER*Stat (version 8.4.0.1), the 95% confidence interval (CI) was calculated using the Tiwari et al. modification25, and the corresponding P values were reported as significance tests for the difference between IRs. NCI joinpoint software (version 4.9.1.0) quantified the yearly average annual percent change (AAPC) trends in IRs per 100,000 person-years for hormone receptor-positive BC patients for the whole study period stratified by age group. A Monte Carlo permutation method was used in combination with provided standard errors from SEER*Stat to determine the significance of AAPCs. IRs were not analyzed for women < 20 years of age because of the small number of patients diagnosed with hormone receptor-positive BC. Moreover, IRs were analyzed for 5-year age translations (i.e., 20–24, 25–29…80+) to determine the changes in trends as a function of age.
The main study outcomes were OS and BCSS. The OS was defined as the time elapsing from the date of BC diagnosis to the date of death from any cause or the follow-up cut-off and BCSS was calculated from the date of diagnosis to the date of death from BC. Survival outcomes were calculated using Kaplan–Meier survival curves and the statistical difference was examined across the 6-year groups using the log-rank statistic. Specifically, the 5-year OS and BCSS rates for each individual year was estimated and plotted with 95% CIs, and the group year survival estimate was predicted by the mean survival results of all patients in that year group. The individual year estimates were used to fit the locally weighted least squares (LOWESS) curve without specifying a parametric model. Furthermore, we perpetrated a series of expected subgroup analyses stratified by race (white and black patients), different subtypes of hormone receptor-positive and age group according to the year of diagnosis. Women who were later diagnosed with BC in the study had a short period of follow-up, so our main outcomes (5-year OS and BCSS) were only available in patients diagnosed before 2014. The significance level was tested, and the P value is shown as the log-rank test of survival results according to year group. For multigroup comparisons, the log-rank P-value with a Bonferroni correction (0.05/15 [number of possible pairs]) was used to obtain group-specific 95% CIs for hazard ratios (HRs) and indicate statistically significant differences.
Univariable Cox proportional hazards regression was performed to calculate the HRs and 95%CIs for OS and BCSS. Multivariate Cox proportional hazards regression analysis was evaluated to determine the association between year of diagnosis and survival outcomes adjusted for age, race, marital status, hormone receptor status, grade, stage, node status, chemotherapy, and radiation. Furthermore, we also performed a multivariate Cox analysis with year of diagnosis as a continuous variable to further determine whether the survival outcomes improved over time. The results are expressed in HRs and 95% CIs. All statistical tests were two-sided, and a P-value ≤ 0.05 was considered statistically significant. All statistical analyses were carried out using IBM SPSS (version 22; IBM Corporation, Armonk, NY, USA) and GraphPad Prism (version 9.5.0; GraphPad Software, Inc., La Jolla, CA, USA).
Ethics Committee
Ethical review and approval were waived for this study due to the data was accessed from the SEER publicly database and no intervention on patients was performed.
Results
Patient characteristics
Table 1 presents the main demographic and clinicopathologic characteristics of patients based on the year of diagnosis. The final analysis involved 370,729 hormone receptor-positive BC patients, of whom 37,943 (10.2%), 49,266 (13.3%), 55,652 (15.0%), 64,451 (17.4%), 77,127 (20.8%), and 86,290 (23.3%) were diagnosed between 1990 and 1994, 1995–1999, 2000–2004, 2005–2009, 2010–2014, and 2015–2019, respectively. Among the included patients, a total of 308,672 (83.3%) were diagnosed with ER-positive/PR-positive, 54,709 (14.8%) were ER-positive/PR-negative, and 7348 (1.9%) were ER-negative/PR-positive tumors. Patients between 60 and 69 years of age (25.2%) were most frequent, followed closely by those 50–59 years of age (22.5%), and patients < 30 years of age were least common (0.4%). The racial distribution showed that 306,153 women (82.6%) were white, 24,092 women (6.5%) were black, 39,217 women (10.6%) were classified as another race (American Indian/Alaska native or Asian/Pacific Islander), and the race of 1267 women (0.3%) was not reported by SEER.
The frequency of hormone receptor-positive BC increased significantly in black patients over the interval study (1990–1994, 4.4%; 1995–1999, 4.8%; 2000–2004, 5.3%; 2005–2009, 6.5%; 2010–2014, 7.6%; and 2015–2019, 8.2%; P for trend < 0.0001), whereas the frequency of hormone receptor-positive BC decreased in white patients (1990–1994, 88.6%; 1995–1999, 87.0%; 2000–2004, 85.2%; 2005–2009, 82.8%; 2010–2014, 80.1%; and 2015–2019, 77.8%; P for trend < 0.0001). The proportion of patients with ER-positive/PR-positive BC increased stepwise from 78.2% during the 1990–1994 time period to 85.3% during the 2015–2019 time period (7.1% increase). In contrast, the ER-positive/PR-negative and ER-negative/PR-positive disease rates steadily decreased from 16.8 to 13.7% (3.1% decrease) and 5.0–2.0% (3.0% decrease), respectively. The frequency of low grade (I and II) hormone receptor-positive BC increased from 43.9 to 71.7%, while the frequency of high grade (III and IV) decreased from 27.0 to 17.9% between 1990 and 2019. The prevalence of early stage (Tis and I) hormone receptor-positive BC increased 19.5%, stage II–III decreased 12.6%, and stage IV remained low (2.8–4.2%) in the 6 diagnostic groups. The deaths attributed to BC among women diagnosed with hormone receptor-positive BC decreased from 26.3% in 1990–1994 to 3.3% in 2015–2019.
Incidence rates for hormone receptor-positive BC
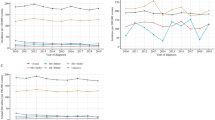
Age-adjusted IRs of hormone receptor-positive BC increased from 70 per 100,000 women-years in 1990 to 113 per 100,000 women-years in 2019, with an AAPC of 1.59% (95% CI, 1.18–1.99; Fig. 2). The AAPCs were 1.95% (95% CI, 1.56–2.35), 0.62% (95% CI, 0.38–0.85), and − 4.83% (95% CI, − 7.24 to − 2.36) for ER-positive/PR-positive, ER-positive/PR-negative, and ER-negative/PR-positive BC, respectively (Fig. 2).
There was an age heterogeneity in the incidence of hormone receptor-positive BC. The highest IR (362.5 per 100,000 women-years) occurred among all hormone receptor-positive women 75–79 years of age. ER-positive/PR-positive women, 70–74 years of age, had the highest IR (300.5 per 100,000 women-years), ER-positive/PR-negative women, 75–79 years of age, had the highest IR (58.3 per 100,000 women-year), and ER-negative/PR-positive women, 65–69 years of age, had the highest IR (4.7 per 100,000 women-year; Supplementary Fig. 1). Nearly all age groups had an increase in trends (0.5–4.0%) from 1990 to 2019, and a statistically significantly difference except women > 85 years of age (Supplementary Table 1) for the AAPC in each age group.
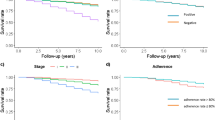
Survival analysis
The cut-off for follow-up was 31 December 2019. The median follow-up among all patients was 108 months (range, 1–359 months). The mean OS and BCSS was 208.9 (95% CI, 208.4–209.5 months) and 294.8 months (95% CI, 294.3–295.4 months) for hormone receptor-positive BC, respectively. A total of 128,714 patients (34.7%) died from all causes and 49,018 patients (13.2%) died from BC. We used the Kaplan-Meier algorithm to estimate the 5-year survival rates (OS and BCSS) for hormone receptor-positive BC patients. A LOWESS curve was used to fit the individual survival estimates reflecting the variation trends (Fig. 3). The 5-year OS rate increased from 78.5% (95% CI, 77.5–79.4%) among patients diagnosed in 1990 to 86.1% (95% CI, 85.6–86.7%) among patients diagnosed in 2014, and the 5-year BCSS rate increased from 87.7% (95% CI, 86.8–88.5%) in 1990 to 92.7% (95% CI, 92.3–93.1%) in 2014 (P < 0.0001 for both OS and BCSS). Similar trends were observed for the 2-year OS and BCSS in hormone receptor-positive patients, with the 2-year OS rate increasing from 92.7% (1990–1994) to 95.1% (2015–2019) and the 2-year BCSS rate increasing from 95.9% (1990–1994) to 97.2% (2015–2019; Supplementary Fig. 2). The survival curves for OS and BCSS stratified by diagnostic group, as well pairwise comparisons among each of two diagnostic groups and along with log-rank P-value are provided in Fig. 4. Patients diagnosed during 2015–2019 had the best OS and BCSS, followed by 2010–2014, 2005–2009, 2000–2004, 1995–1999, and 1990–1994 (P < 0.0001; Fig. 4A and B). The 5-year OS and BCSS rates were highest for hormone receptor-positive BC patients diagnosed in 2010–2014 (85.5% and 92.4%), followed closely by 2005–2009 (85.2% and 92.3%), 2000–2004 (84.6% and 92.3%), 1995–1999 (82.3% and 91.0%), and 1990–1994 (79.3% and 88.5%). Similarly, there was a significantly increased trend for 2- and 5-year relative survival (OS and BCSS) for ER-positive/PR-positive BC and ER-positive/PR-negative BC (Supplementary Figs. 3–6). However, although the relative survival rate among ER-negative/PR-positive BC differed statistically significantly over the study period, no apparent trend was observed.
5-year overall survival (OS) and 5-year breast cancer -specific (BCSS) for hormone receptor-positive female breast cancer patients between 1990 and 2014. (A)OS; (B)BCSS. Note: Inserts show FDA approvals of various endocrine therapy and targeted therapy agents for treatment of hormone receptor-positive tumors.
Overall survival (A) and breast cancer-specific survival (B) for hormone receptor-positive breast cancer. Note: * mean P ≤ 0.05, ** mean P ≤ 0.01, *** mean P ≤ 0.001, **** mean P ≤ 0.0001. P value < 0.0033 was considered statistically significant in pairwise-comparison analysis with Bonferroni adjusted.
Subgroup analyses were performed based on age at diagnosis, race, stage, radiation, and chemotherapy (Supplementary Figs. 7–11). In patients first diagnosed with hormone receptor-positive BC < 60 years of age, those who were diagnosed between 1990 and 1994 had the significantly worst OS and BCSS, followed by 1995–1999, 2000–2004, and 2005–2009. There was no significant difference in OS and BCSS between 2005 and 2009, 2010–2014, and 2015–2019 (Supplementary Fig. 7A-D and Supplementary Tables 2–3). For patients > 60 years of age, the OS increased significantly between 1990 and 2019; however, no significant difference in BCSS was detected in pairwise comparisons of the two diagnostic groups in 2005–2009 versus 2000–2004, and 2010–2014 versus 2000–2004 (Supplementary Fig. 7E-F and Supplementary Tables 2–3). Among white patients with stage 0–II tumors, the OS did not differ statistically significantly between 2005 and 2009 and 2010–2014, and the BCSS did not differ statistically significantly between 2000 and 2004, 2005–2009, 2010–2014, and 2015–2019 (Supplementary Figs. 8–9 and Supplementary Tables 2–3). Among patients who received radiation therapy, both OS and BCSS improved significantly over the entire study period, except for the pairwise comparisons between 2005 and 2009 and 2010–2014 (Supplementary Fig. 10 and Supplementary Tables 2–3). Among hormone receptor-positive BC patients between 2000 and 2019 who underwent chemotherapy, no statistically significant differences for pairwise comparison of 2010–2014 vs. 2000–2004, 2015–2019 vs. 2000–2004, 2010–2014 vs. 2005–2009, and 2015–2019 vs. 2010–2014 were observed (Supplementary Fig. 11 and Supplementary Tables 2–3).
In univariable analysis, receiving chemotherapy was associated with lower BCSS; however, after adjustment for confounding variables with multivariable analysis, receiving chemotherapy was proved to have no significant impact on BCSS (HR, 0.98; 95% CI, 0.96-1.00; P = 0.157, Table 2 and Supplementary Table 4). Based on multivariate Cox proportional hazards regression analysis, the risk of all-cause mortality decreased 5% (HR, 0.95; 95% CI, 0.94–0.97), 6% (HR, 0.94; 95% CI, 0.92–0.96), 10% (HR, 0.90; 95% CI, 0.88–0.92), 15% (HR, 0.85; 95% CI, 0.83–0.87), and 22% (HR, 0.78; 95% CI, 0.76–0.81) for patients diagnosed with hormone receptor-positive BC during 1995–1999, 2000–2004, 2005–2009, 2010–2014, and 2015–2019, respectively, when compared to patients diagnosed during 1990–1994 (P < 0.0001). The risk of BC-specific mortality decreased 9% (HR, 0.91; 95% CI, 0.88–0.93), 16% (HR, 0.84; 95% CI, 0.81–0.86), 21% (HR, 0.79; 95% CI, 0.76–0.81), 25% (HR, 0.75; 95% CI, 0.73–0.78), and 27% (HR, 0.73; 95% CI, 0.70–0.76) for patients diagnosed with hormone receptor-positive BC during 1995–1999, 2000–2004, 2005–2009, 2010–2014, and 2015–2019, respectively, compared to patients diagnosed during 1990–1994 (P < 0.0001). By setting the year of diagnosis as a continuous variable, the risk of all-cause and BC-specific mortality decreased 0.8% (HR, 0.992; 95% CI, 0.991–0.993; P < 0.0001) and 1.3% (HR, 0.987; 95% CI, 0.985–0.988; P < 0.0001) each year since 1990, respectively (Table 2).
Discussion
The status of hormone receptor expression, especially ER status, is one of the most critical molecular markers for evaluating the reaction and benefits of BC therapy. The level of ER expression is closely associated with endocrine responsiveness and recurrence-free survival (ERhigh > ERlow) and therefore the ER-negative population does not benefit from hormonal therapy16,26,27. Over the past several decades, many new drugs based on the hormone receptor pathway have been developed for hormone receptor-positive BC patients, including anastrazole, fulvestrant, and palbociclib. Although the mortality rates have been dramatically reduced by 43% among BC patients overall, with > 460,000 cancer survivors from 1989 to 20203, the survival patterns of hormone receptor-positive BC is poorly understand. In the present study, the trends in IRs and survival outcomes of patients with hormone receptor-positive BC were evaluated using a nearly 30-year population-based cohort.
The overall increase in the incidence of BC in the US has mainly been due to an increase in the incidence of hormone receptor-positive BC3,28. In this present study, we showed that the incidence of hormone receptor-positive BC steadily increased over the past three decades. During the entire interval of data collection (1990–2019), the IR for hormone receptor-positive BC increased by 1.59% annually and was mostly driven by the subtype of ER-positive/PR-positive BC. The decrease in thresholds for positivity of immunohistochemistry determinations of ER and PR testing from 10 to 1% in 2010 might result in approximately 20% of the previous ER-positive and/or PR-positive results misclassified as ER-negative and/or PR-negative29. Some patients previously classified as hormone receptor-negative BC will be diagnosed as hormone receptor-positive BC as the new threshold is incorporated into clinical practice. We do not have an explanation for none sharp increase in the incidence of hormone receptor-positive BC since 2010 based on a decrease in the threshold. In contrast, the progressive decline in the incidence of ER-negative/PR-positive BC from 1990 to 2019 may be due to advances in immunohistochemical techniques, which modified ER-negative and/or PR-negative BC classification into ER-positive and/or PR-positive BC30. However, there was no information from the SEER database on the methods of hormone receptor detecting for BCs, and their sensitivity and specificity. Another important potential confounder for this increased incidence trend was the detection of more new hormone receptor-positive BC cases with the advent and increasing availability of mammographic screening programs28,31. Thus, it has been suggested that development of immunohistochemical and access to health examinations might have a notable influence on the increase in the incidence of hormone receptor-positive BC. Because of the existent discordance between the primary tumor and metastasis in ER, PR and HER2 status in portions of advanced BCs32, the unequivocal recommendations for biopsy when metastases are suspected as follow: solitary metastasis, unusual clinical course, and research33.
In addition to immunohistochemical technique and health access, the divergent IR trend may reflect changes in risk factors for subtype-specific BC. Importantly, multiparity is strong associated with an approximate 25% lower risk of developing hormone receptor-positive BC34,35. The fertility rate in the US has dropped from a high of 118 births per 1000 women 15–44 years of age to a historic nadir of 56.6 births per 1000 women in 20213. The birth rate has declined steadily since 2007 when the birth rate was recorded at 69.4 births per 1000 women3, representing a significant decrease in the average number of children per woman over the past few decades35. In contrast, the IR for hormone receptor-positive BC has been increasing. Ritte et al.36 reported that the current use of hormone replacement therapy (HRT) for postmenopausal women is correlated with an increased risk of hormone receptor-positive BC (treatment vs. no treatment: HR, 1.74; 95% CI, 1.56–1.95). Nevertheless, HRT has been increasingly promoted in the past 40 years to improve quality of life and reduce the risk of osteoporotic fractures and coronary heart disease37. Data obtained from the First National Health and Nutrition Examination Survey documented that the percentage of postmenopausal women in the US who used HRT for ≥ 5 years increased from 20% in the early 1970s to 31% in the late 1980s and early 1990s38. It is well-known that obesity is also associated with a higher risk of developing hormone receptor-positive BC, especially among postmenopausal women39,40,41,42. Interestingly, the US has the highest incidence of obesity globally, and the incidence of obesity in the US has increased since the 1970s43,44.
Although the incidence of hormone receptor-positive BC has gradually increased over the past three decades, we found that the earlier year of diagnosis was independently associated with an increased risk of overall mortality and BC-specific mortality since 1990. Specifically, the 5-year OS and BCSS improved by 7.6% from 78.5% in 1990 to 86.1% in 2014, and by 5.0% (from 87.7% in 1990 to 92.7% in 2014), respectively. Jatoi et al.45 conducted a study involving a cohort of 147,289 women with ER-positive BC diagnosed between 1990 and 2003 and reported that the incidence-based mortality significantly declined 13% from 6.1 to 5.3 per 100,000 women-years (P < 0.0001). Chen et al.46 reported that the 2- and 5-year BCSS rates significantly improved across ER-positive/PR-positive and ER-positive/PR-negative subtypes between 1992 and 2008. Yamada et al.47 reported that 1806 Japanese women with invasive hormone receptor-positive BC received complete resection at the National Cancer Center Hospital East between July 1992 and December 2010, and showed a significant improvement in 5-year OS (92.6% vs. 97.6%, P < 0.001) with a significant difference in the 5-year recurrence-free survival (82.1% vs. 94.5%, P < 0.001) among patients diagnosed between 2007 and 2010 compared to those diagnosed between 1992 and 1996.
During the past several decades, the US FDA has approved many endocrine therapeutics and strategies, which have significantly contributed to improved survival rates for patients with hormone receptor-positive BC35,48,49,50. In a meta-analysis comprising approximately 18,000 women across 55 trials, the proportion of recurrences for women with HR-positive tumors reduced 21%, 28%, and 50% after 1, 2, or 5 years of tamoxifen therapy, respectively27. Similarly, 1, 2, or 5 years of tamoxifen resulted in a decrease in mortality by 14%, 18%, and 28%, respectively, indicating a significant trend towards greater benefits with a longer duration of treatment27. Adjuvant ET with aromatase inhibitors (AIs) for 5 years or as extended therapy after 5 years of tamoxifen significantly reduced the recurrence risk compared to tamoxifen alone for postmenopausal women with hormone receptor-positive BC51. The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) reported that patients who received AIs for 5 years as adjuvant ET had a significantly lower recurrence risk during the treatment period (risk ratio for years 0–1: 0.64, 95% CI 0.52–0.78; risk ratio for years 2–4: 0.80, 95% CI 0.68–0.93) and a 10-year BC mortality rate (12.1% vs. 14.2%, P = 0.009) compared to 5 years of tamoxifen52. Di Leo et al.53,54 reported that a higher fulvestrant dose (500 mg) was associated with a longer PFS (6.5 months vs. 5.5 months, HR = 0.80, P = 0.006), and a 19% decreased risk of mortality compared to a lower fulvestrant dose (250 mg). Moreover, numerous agents targeting mTOR, PI3K, and CDK 4/6 have been added to the regimens for the hormone receptor-positive BC, especially for ET-resistant patients22. Most recently, a favorable OS with palbociclib plus fulvestrant compared to placebo plus fulvestrant was observed in most subgroups, especially in patients with ET-sensitive disease55. Together, refinements in ET may have significantly contributed to a stepwise improvement in survival outcomes among hormone receptor-positive BC patients over the past several decades.
In addition, more widespread participation in BC screening and adjuvant systemic therapy among women in the US throughout the 1990s56,57 has led to a decline in mortality58,59. During this period, BC screening with mammography has become well-accepted in the US, with an increasing prevalence of patients being diagnosed with in situ and early-stage BC31,59. The use of more effective therapeutic agents, including taxanes, anthracyclines, and trastuzumab and extended ET (5–10 years of tamoxifen and/or an AI) may also have had a positive impact on survival in this cohort60,61. Undeniably, the development of surgical treatment, advance in management and chemotherapy may also contribute to the decline in mortality among hormone receptor-positive BC patients62. In order to further comprehensively improve survival rate for all subtypes of BC, it is extremely important to increase the allocation of resources in the future to narrow the rural-urban disparities in terms of access to mammograms and treatment. Moreover, survival analysis for triple negative and HER2 + BCs are also extremely meaningful when comparing prognosis, future study should further explore.
The present study had several limitations. First, the enrolled patients were exclusively US residents. Thus, these findings may not be generalized to patients from other countries or regions. Second, we simply divide breast cancer into hormone receptor-positive and hormone receptor-negative, which may cause a bias. Third, because the SEER database did not provide data related to ET, we could not directly analyze the relationship between ET and survival outcomes of patients with hormone receptor-positive BC. Therefore, a real-world study with a large sample size may be needed to disclose the actual contribution of ET to survival benefits for hormone receptor-positive BC patients. Fourth, transition of the method for detecting hormone receptors and the issue of HER-2 were not mentioned. Fifth, women with hormone receptor-positive BC who were diagnosed later in this study only had a short duration of follow-up. As a result, the estimate for 2-year survival rate for those diagnosed in 2018–2019, as well as the 5-year survival rate for those diagnosed in 2015–2019 could not be calculated. In addition, it is impossible to explore the differences of hormone receptors between metastatic and primary tumors in patients with advanced hormone receptor -positive BCs (stage III-IV) in SEER database. The survival benefits may not be sufficient because drugs, such as mTOR, PI3K, and CDK4/6 inhibitors, were only approved for the treatment of hormone receptor-positive BC in recent years. There is still a need for continuous updates on the survival benefits associated with drug treatments and drug resistance should also be assessed.
Conclusion
In summary, our study showed a stepwise improvement in OS and BCSS over the last three decades among women with hormone receptor-positive BC, although the incidence of hormone receptor-positive BC gradually increased from 1990 to 2019.
Data availability
The data underlying this article were available in NCI SEER 8 database: Incidence-SEER Research Plus Data, 8 Registries, Nov 2021 Sub [1975–2019] at https://seer.cancer.gov/data/access.html, and could be accessed with Surveillance Research Program, NCI SEER*Stat software.
References
Siegel, R. L., Miller, K. D., Wagle, N. S. & Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 73, 17–48. https://doi.org/10.3322/caac.21763 (2023).
National Institutes of Health;National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer stat facts: female breast cancer, https://seer.cancer.gov/statfacts/html/breast.html.
Giaquinto, A. N. et al. Breast Cancer Stat. 2022 CA Cancer J. Clin. 72, 524–541, https://doi.org/10.3322/caac.21754 (2022).
Smolarz, B., Nowak, A. Z. & Romanowicz, H. Breast Cancer-epidemiology, classification, Pathogenesis and treatment (review of literature). Cancers (Basel). 14. https://doi.org/10.3390/cancers14102569 (2022).
Łukasiewicz, S. et al. Breast Cancer-epidemiology, risk factors, classification, prognostic markers, and current treatment Strategies-An updated review. Cancers (Basel). 13 https://doi.org/10.3390/cancers13174287 (2021).
Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70, https://doi.org/10.1038/nature11412 (2012).
Acheampong, T., Kehm, R. D., Terry, M. B., Argov, E. L. & Tehranifar, P. Incidence trends of breast Cancer Molecular subtypes by Age and Race/Ethnicity in the US from 2010 to 2016. JAMA Netw. Open. 3, e2013226. https://doi.org/10.1001/jamanetworkopen.2020.13226 (2020).
Rugo, H. S. The breast cancer continuum in hormone-receptor-positive breast cancer in postmenopausal women: evolving management options focusing on aromatase inhibitors. Ann. Oncol. 19, 16–27. https://doi.org/10.1093/annonc/mdm282 (2008).
Setiawan, V. W. et al. Breast cancer risk factors defined by estrogen and progesterone receptor status: the multiethnic cohort study. Am. J. Epidemiol. 169, 1251–1259. https://doi.org/10.1093/aje/kwp036 (2009).
Bardou, V. J., Arpino, G., Elledge, R. M., Osborne, C. K. & Clark, G. M. Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J. Clin. Oncol. 21, 1973–1979. https://doi.org/10.1200/jco.2003.09.099 (2003).
Horwitz, K. B. & McGuire, W. L. Predicting response to endocrine therapy in human breast cancer: a hypothesis. Science. 189, 726–727. https://doi.org/10.1126/science.168640 (1975).
Osborne, C. K., Schiff, R., Arpino, G., Lee, A. S. & Hilsenbeck, V. G. Endocrine responsiveness: understanding how progesterone receptor can be used to select endocrine therapy. Breast. 14, 458–465. https://doi.org/10.1016/j.breast.2005.08.024 (2005).
Waks, A. G. & Winer, E. P. Breast Cancer Treatment: a review. Jama. 321, 288–300. https://doi.org/10.1001/jama.2018.19323 (2019).
Regan, M. M. et al. Absolute Benefit of Adjuvant Endocrine therapies for Premenopausal Women with hormone Receptor-Positive, human epidermal growth factor receptor 2-Negative early breast Cancer: TEXT and SOFT trials. J. Clin. Oncol. 34, 2221–2231. https://doi.org/10.1200/jco.2015.64.3171 (2016).
Yu, K. D. et al. Cyclophosphamide-Free Adjuvant Chemotherapy for Ovarian Protection in Young Women with breast Cancer: a randomized phase 3 trial. J. Natl. Cancer Inst. 113, 1352–1359. https://doi.org/10.1093/jnci/djab065 (2021).
Davies, C. et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 378, 771–784. https://doi.org/10.1016/s0140-6736(11)60993-8 (2011).
Thürlimann, B. et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl. J. Med. 353, 2747–2757. https://doi.org/10.1056/NEJMoa052258 (2005).
Mehta, R. S. et al. Overall survival with fulvestrant plus anastrozole in metastatic breast Cancer. N Engl. J. Med. 380, 1226–1234. https://doi.org/10.1056/NEJMoa1811714 (2019).
Finn, R. S. et al. Palbociclib and Letrozole in Advanced breast Cancer. N Engl. J. Med. 375, 1925–1936. https://doi.org/10.1056/NEJMoa1607303 (2016).
Nunnery, S. E. & Mayer, I. A. Targeting the PI3K/AKT/mTOR pathway in hormone-positive breast Cancer. Drugs. 80, 1685–1697. https://doi.org/10.1007/s40265-020-01394-w (2020).
Schrodi, S. et al. Outcome of breast cancer patients with low hormone receptor positivity: analysis of a 15-year population-based cohort. Ann. Oncol. 32, 1410–1424. https://doi.org/10.1016/j.annonc.2021.08.1988 (2021).
Jacobs, A. T., Castaneda-Cruz, M., Rose, D., Connelly, L. & M. M. & Targeted therapy for breast cancer: an overview of drug classes and outcomes. Biochem. Pharmacol. 204, 115209. https://doi.org/10.1016/j.bcp.2022.115209 (2022).
National Institutes of Health;National Cancer Institute. Surveillance, Epidemiology, and End Results Program. SEER*Stat Databases: November 2021 Submissions, https://seer.cancer.gov/data-software/documentation/seerstat/nov2021/ (.
Hammond, M. E. et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J. Clin. Oncol. 28, 2784–2795. https://doi.org/10.1200/jco.2009.25.6529 (2010).
Surveillance, Epidemiology, and End Results Program, National Cancer Institute. Use Tiwari et al., 2006 modification for CIs, https://seer.cancer.gov/seerstat/WebHelp/seerstat.htm#Use_Tiwari_et_al.%2c_2006_modification_for_CIs.htm (.
Yoon, K. H. et al. Effect of Estrogen Receptor Expression Level and hormonal therapy on prognosis of early breast Cancer. Cancer Res. Treat. 54, 1081–1090. https://doi.org/10.4143/crt.2021.890 (2022).
Tamoxifen for early. Breast cancer: an overview of the randomised trials. Early breast Cancer trialists’ Collaborative Group. Lancet. 351, 1451–1467 (1998).
Li, C. I., Daling, J. R. & Malone, K. E. Incidence of invasive breast cancer by hormone receptor status from 1992 to 1998. J. Clin. Oncol. 21, 28–34. https://doi.org/10.1200/jco.2003.03.088 (2003).
Anderson, K. N., Schwab, R. B. & Martinez, M. E. Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res. Treat. 144, 1–10. https://doi.org/10.1007/s10549-014-2852-7 (2014).
Li, Y. et al. Clinicopathological characteristics and breast Cancer-specific survival of patients with single hormone receptor-positive breast Cancer. JAMA Netw. Open. 3, e1918160. https://doi.org/10.1001/jamanetworkopen.2019.18160 (2020).
Rosenberg, P. S., Barker, K. A. & Anderson, W. F. Estrogen receptor status and the Future Burden of Invasive and in situ breast cancers in the United States. J. Natl. Cancer Inst. 107https://doi.org/10.1093/jnci/djv159 (2015).
Criscitiello, C. et al. Biopsy confirmation of metastatic sites in breast cancer patients: clinical impact and future perspectives. Breast Cancer Res. 16, 205. https://doi.org/10.1186/bcr3630 (2014).
Pusztai, L., Viale, G., Kelly, C. M. & Hudis, C. A. Estrogen and HER-2 receptor discordance between primary breast cancer and metastasis. Oncologist. 15, 1164–1168. https://doi.org/10.1634/theoncologist.2010-0059 (2010).
Gaudet, M. M. et al. Pooled analysis of nine cohorts reveals breast Cancer risk factors by Tumor Molecular Subtype. Cancer Res. 78, 6011–6021. https://doi.org/10.1158/0008-5472.Can-18-0502 (2018).
Newman, L. A. & Kaljee, L. M. Health disparities and Triple-negative breast Cancer in African American women: a review. JAMA Surg. 152, 485–493. https://doi.org/10.1001/jamasurg.2017.0005 (2017).
Ritte, R. et al. Adiposity, hormone replacement therapy use and breast cancer risk by age and hormone receptor status: a large prospective cohort study. Breast Cancer Res. 14, R76. https://doi.org/10.1186/bcr3186 (2012).
Lowe, G. D. Hormone replacement therapy and cardiovascular disease: increased risks of venous thromboembolism and stroke, and no protection from coronary heart disease. J. Intern. Med. 256, 361–374. https://doi.org/10.1111/j.1365-2796.2004.01400.x (2004).
Brett, K. M. & Madans, J. H. Use of postmenopausal hormone replacement therapy: estimates from a nationally representative cohort study. Am. J. Epidemiol. 145, 536–545. https://doi.org/10.1093/oxfordjournals.aje.a009142 (1997).
White, A. J., Nichols, H. B., Bradshaw, P. T. & Sandler, D. P. Overall and central adiposity and breast cancer risk in the Sister Study. Cancer. 121, 3700–3708. https://doi.org/10.1002/cncr.29552 (2015).
Neuhouser, M. L. et al. Overweight, obesity, and postmenopausal invasive breast Cancer risk: a secondary analysis of the women’s Health Initiative Randomized clinical trials. JAMA Oncol. 1, 611–621. https://doi.org/10.1001/jamaoncol.2015.1546 (2015).
Suzuki, R., Rylander-Rudqvist, T., Ye, W., Saji, S. & Wolk, A. Body weight and postmenopausal breast cancer risk defined by estrogen and progesterone receptor status among Swedish women: a prospective cohort study. Int. J. Cancer. 119, 1683–1689. https://doi.org/10.1002/ijc.22034 (2006).
Picon-Ruiz, M., Morata-Tarifa, C., Valle-Goffin, J. J., Friedman, E. R. & Slingerland, J. M. Obesity and adverse breast cancer risk and outcome: mechanistic insights and strategies for intervention. CA Cancer J. Clin. 67, 378–397. https://doi.org/10.3322/caac.21405 (2017).
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 378, 815–825. https://doi.org/10.1016/s0140-6736(11)60814-3 (2011).
Blüher, M. Obesity: global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 15, 288–298. https://doi.org/10.1038/s41574-019-0176-8 (2019).
Jatoi, I., Chen, B. E., Anderson, W. F. & Rosenberg, P. S. Breast cancer mortality trends in the United States according to estrogen receptor status and age at diagnosis. J. Clin. Oncol. 25, 1683–1690. https://doi.org/10.1200/jco.2006.09.2106 (2007).
Chen, L., Linden, H. M., Anderson, B. O. & Li, C. I. Trends in 5-year survival rates among breast cancer patients by hormone receptor status and stage. Breast Cancer Res. Treat. 147, 609–616. https://doi.org/10.1007/s10549-014-3112-6 (2014).
Yamada, Y. et al. Improved overall survival over recent decades in patients with hormone-receptor-positive, HER2-negative breast cancer: a single-center retrospective analysis of prognostic factors. Jpn J. Clin. Oncol. 48, 248–254. https://doi.org/10.1093/jjco/hyy001 (2018).
Forbes, J. F. et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol. 9, 45–53. https://doi.org/10.1016/s1470-2045(07)70385-6 (2008).
Akli, S. et al. Low-molecular-weight cyclin E can bypass letrozole-induced G1 arrest in human breast cancer cells and tumors. Clin. Cancer Res. 16, 1179–1190. https://doi.org/10.1158/1078-0432.Ccr-09-1787 (2010).
Araki, K. & Miyoshi, Y. Mechanism of resistance to endocrine therapy in breast cancer: the important role of PI3K/Akt/mTOR in estrogen receptor-positive, HER2-negative breast cancer. Breast Cancer. 25, 392–401. https://doi.org/10.1007/s12282-017-0812-x (2018).
Winer, E. P. et al. American Society of Clinical Oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. J. Clin. Oncol. 23, 619–629. https://doi.org/10.1200/jco.2005.09.121 (2005).
Aromatase inhibitors versus. Tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 386, 1341–1352. https://doi.org/10.1016/s0140-6736(15)61074-1 (2015).
Di Leo, A. et al. Final overall survival: fulvestrant 500 mg vs 250 mg in the randomized CONFIRM trial. J. Natl. Cancer Inst. 106, djt337. https://doi.org/10.1093/jnci/djt337 (2014).
Di Leo, A. et al. Results of the CONFIRM phase III trial comparing fulvestrant 250 mg with fulvestrant 500 mg in postmenopausal women with estrogen receptor-positive advanced breast cancer. J. Clin. Oncol. 28, 4594–4600. https://doi.org/10.1200/jco.2010.28.8415 (2010).
Cristofanilli, M. et al. Overall survival with Palbociclib and Fulvestrant in Women with HR+/HER2- ABC: updated exploratory analyses of PALOMA-3, a Double-blind, phase III randomized study. Clin. Cancer Res. 28, 3433–3442. https://doi.org/10.1158/1078-0432.Ccr-22-0305 (2022).
Ghafoor, A. et al. Trends in breast cancer by race and ethnicity. CA Cancer J. Clin. 53, 342–355. https://doi.org/10.3322/canjclin.53.6.342 (2003).
Mariotto, A. et al. Trends in use of adjuvant multi-agent chemotherapy and tamoxifen for breast cancer in the United States: 1975–1999. J. Natl. Cancer Inst. 94, 1626–1634. https://doi.org/10.1093/jnci/94.21.1626 (2002).
Berry, D. A. et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl. J. Med. 353, 1784–1792. https://doi.org/10.1056/NEJMoa050518 (2005).
Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence. 15-year survival: an overview of the randomised trials. Lancet. 365, 1687–1717. https://doi.org/10.1016/s0140-6736(05)66544-0 (2005).
Burstein, H. J. et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update on ovarian suppression. J. Clin. Oncol. 34, 1689–1701. https://doi.org/10.1200/jco.2015.65.9573 (2016).
Denduluri, N. et al. Selection of optimal adjuvant chemotherapy and targeted therapy for early breast Cancer: ASCO Clinical Practice Guideline focused Update. J. Clin. Oncol. 36, 2433–2443. https://doi.org/10.1200/jco.2018.78.8604 (2018).
Roberts, K. E., Rickett, K., Feng, S., Vagenas, D. & Woodward, N. E. Exercise therapies for preventing or treating aromatase inhibitor-induced musculoskeletal symptoms in early breast cancer. Cochrane Database Syst. Rev. 1 (Cd012988). https://doi.org/10.1002/14651858.CD012988.pub2 (2020).
Acknowledgements
The authors would like to thank the SEER database and the reviewers for their professional suggestions.
Funding
This study was supported by grant 82202913 from the National Natural Science Foundation of China (Dr Yunhai Li).
Author information
Authors and Affiliations
Contributions
Conceptualization, Y.L. and F.L.; methodology, H.H., T.W., Y.L. and F.L.; software, H.H., Y.L. and F.L.; validation, Y.L. and F.L.; formal analysis, H.H., T.W., A.Z., H.Z., Y.L. and F.L.; investigation, H.H., Y.L. and F.L.; resources, Y.L. and F.L.; data curation, H.H., Y.L. and F.L.; writing—original draft preparation, H.H., T.W., A.Z., H.Z., L.K., Y.L. and F.L.; writing—review and editing, H.H., T.W., A.Z., H.Z., L.K., Y.L. and F.L.; visualization, H.H., T.W., Y.L. and F.L.; supervision, Y.L. and F.L.; project administration, F.L.; funding acquisition, Y.L. All authors have read and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, H., Wei, T., Zhang, A. et al. Trends in the incidence and survival of women with hormone receptor-positive breast cancer from 1990 to 2019: a large population-based analysis. Sci Rep 14, 23690 (2024). https://doi.org/10.1038/s41598-024-74746-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74746-1
This article is cited by
-
The pleiotropic roles of non-hormonal receptor basigin and regulatory microRNAs in breast cancer
npj Breast Cancer (2025)
-
Identification of factors associated with non-adherence to oral endocrine therapy in breast cancer patients of low socioeconomic status: a single centre retrospective study
International Journal of Clinical Pharmacy (2025)