Abstract
Backgrounds
This investigation seeks to explore the correlation between nonalcoholic fatty liver disease (NAFLD) and cardiovascular diseases (CVDs), and to to provide evidence for the prevention and treatment of CVDs.
Methods
This study utilized data from the Jinchang cohort platform, including 19,399 participants without pre-existing major CVDs. Based on the general population and gender stratification, Cox models were used to analyze the risk of NAFLD for CVDs. The combined effect of NAFLD and different obesity indicators on CVDs was analyzed by additive and multiplicative interaction models and subgroups.
Results
There were 3129 NAFLD patients out of 19399 subjects, and 723 (23.11%) of them had the CVD. After adjusting for multiple confounding factors, the Cox model revealed a 1.17-fold increase in the risk of CVDs among patients with NAFLD compared to those without NAFLD. Moreover, there was no notable disparity in CVDs risk among most NAFLD patients at the same level of obesity. The results indicated no additive interaction between NAFLD and obesity concerning CVDs risk, but rather a positive multiplicative interaction. Using the normal population as a reference, it was found that people with both obesity and NAFLD significantly increased the risk of developing CVDs, with HRs and 95% CIs of 1.790 (1.508, 2.126), 1.356 (1.213, 1.517), and 1.807 (1.503, 2.174), respectively, for BMI, WC, and the combination of BMI and WC.
Conclusions
NAFLD and obesity are independent risk factors for CVDs. The synergy of obesity and NAFLD implies that NAFLD patients should control weight gain. Larger BMI and WC values may increase the CVDs risk for NAFLD patients, especially women.
Similar content being viewed by others
Introduction
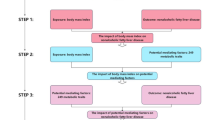
Non-alcoholic fatty liver disease (NAFLD), as a metabolic stress-induced liver injury, is closely associated with insulin resistance (IR) and genetic susceptibility. Patients usually have manifestations related to overnutrition, obesity, and metabolic syndrome, and without intervention, they can progress to liver cirrhosis and even hepatocellular carcinoma (HCC)1. Moreover, NAFLD is a multi-system disease, which not only causes liver-related complications, but also has metabolic comorbidities to a large extent, which increases the risk of extrahepatic diseases such as cardiovascular diseases (CVDs), chronic kidney disease, type 2 diabetes mellitus (T2DM), and malignant tumors2. In recent years, NAFLD has been proposed as an emerging risk factor for CVDs3. Younossi et al. conducted a global epidemiological meta-analysis focusing on NAFLD, revealing a striking incidence of 4.79 CVDs deaths and 0.77 liver disease-related deaths per 1000 person-years within the NAFLD population4. Moreover, increasing clinical and epidemiological evidence has shown that after adjusting for common cardiovascular risk factors, NAFLD is still independently associated with increased prevalence and incidence of CVDs5,6. However, current studies on the association between NAFLD and CVDs are mostly concentrated in economically developed countries and regions, while domestic studies, especially those in northwest China, are very lacking7,8,9. Therefore, it is necessary to carry out relevant studies in this region to provide a new basis for the prevention and control of CVDs.
Studies have shown that obesity is another key and modifiable risk factor for CVDs. NAFLD increases CVD risk through IR, low-grade systemic inflammation, adhesion molecules, and prothrombotic mechanisms10. And Obesity triggers adipocyte proliferation, leading to a low-grade systemic pro-inflammatory state and pro-inflammatory cytokine secretion, which exacerbates IR and thus promotes the development of NAFLD and CVD11. A meta-analysis12 in China showed that the risk of late-life stroke in early adulthood was 1.36 and 1.81 times higher in overweight and obese individuals than in normal-weight individuals, respectively, and the association was stronger in the obese group than in the overweight group, suggesting a dose-response relationship. And results from the China Health and Retirement Longitudinal Study (CHARLS)13 showed that the prevalence of obesity-associated hypertension in people aged 45 years and older in China was 22.7%, or about 120 million people. The meta-analysis evidence of Li et al.14 suggested a clear dose-response relationship between body mass index (BMI) and the risk of NAFLD. At present, the prevalence of NAFLD in non-obese people has been widely reported worldwide, ranging from 3–30%15. Obesity, as a common risk factor for NAFLD and CVDs, may play an important role in the development of CVDs in NAFLD. Contemporary investigations mostly focus on the effect of obesity or NAFLD alone on the prevalence of CVDs. Moreover, it is not clear whether non-obese individuals afflicted with NAFLD face a comparable risk of developing CVDs as their obese counterparts with NAFLD. Therefore, further research is urgently needed, which is of great significance for the prevention and treatment of the outcome of NAFLD population and the reduction of the risk of CVDs.
BMI and waist circumference (WC) are the main indicators of obesity. BMI is a widely used obesity measure in clinical and epidemiological studies to classify general obesity. However, BMI doesn’t distinguish between muscle mass and fat mass, nor does it reflect fat distribution, and it is affected by differences in age, sex, and race. At present, the conclusions on the relationship between BMI and CVDs are inconsistent, and some studies have reported that higher BMI is associated with a higher risk of CVD death16. A Korean cohort showed that lower BMI was associated with a reduced risk of coronary heart disease (CHD)17. Simultaneously, certain scholars have postulated that BMI exerts a safeguarding influence on CVDs among afflicted patients18. WC is an indicator to evaluate central obesity, which can reflect fat distribution and visceral fat accumulation to a certain extent, and is considered to be a good indicator to predict CVDs19. It has been reported that a 1 cm increase in WC increases the risk of future cardiovascular events by 5%20. However, the advantages and disadvantages of BMI versus WC measurement are still under debate21,22. Therefore, it is of great significance to carry out studies on CVDs risk assessment by combining BMI and WC indicators to clarify the evaluation indicators of obesity in the population. In this study, we utilized data from the Jinchang Cohort Study Platform23, located in the western region of China, employing the methodological framework of prospective cohort studies to elucidate the pathogenetic correlation between NAFLD and CVDs. Our inquiry delved into unraveling the potential interplay between obesity and NAFLD concerning CVDs, along with assessing the varying risk of NAFLD on CVDs across different obesity strata. Furthermore, we meticulously stratified our analysis by gender, endeavoring to furnish a scientific underpinning for the prevention and treatment of CVDs within local populations.
Materials and methods
Study population
Our study was based on a cohort of occupational populations that was established in a large, state-owned enterprise in China (Jinchang cohort)23. The cohort completed a baseline survey of 48,001 individuals from June 2011-December 2013, a first follow-up of 33,355 individuals before December 2015, and a second follow-up of 30,291 individuals before December 201724. A total of 30,291 individuals were then matched to baseline and follow-up information based on unique individual numbers for this study. Here, general characteristics, physical examination and biological indicators of the subjects of this study were collected in the baseline, and diagnostic outcomes of CVDs were determined in the follow-up. 8,248 patients with hypertension, 592 patients with coronary artery disease and 205 patients with stroke were excluded from the baseline according to the purpose of the study, followed by the exclusion of 1,847 patients with missing ultrasound results at baseline, resulting in the inclusion of 19,399 patients (Fig. 1).
Data collection
This study used a self-designed questionnaire, and with the informed consent of the respondents, the survey was conducted face-to-face by uniformly trained professional investigators. The content of the survey mainly included general demographic and sociological characteristics, personal behavioral habits, past history of diseases, family history of diseases, and occupational history. Physical examinations were performed by professional clinicians and included measurements of body weight, height, WC, blood pressure (BP), and abdominal liver ultrasound. For clinical biochemical testing, all participants were required to obtain fasting venous blood in the morning. Fasting plasma glucose (FPG), triglyceride (TG), total cholesterol (TC), high density lipoprotein cholesterol (HDL-C), alanine aminotransferase (ALT), aspartate aminotransferase (AST), platelet (PLT) and albumin (ALB) were detected by automatic biochemical analyzer. Inpatient medical records of all employees from January 2011 to December 2017 were collected in the employee hospital affiliated with the cohort employee’s enterprise. The main information included the employee’s ID number, age, gender, visit number, visit time, discharge diagnosis, and International Classification of Diseases, 10th edition (ICD-10).
Assessment of NAFLD and obesity
NAFLD: Excessive accumulation of fat in the liver as demonstrated by ultrasound; no history of alcohol consumption or no excessive alcohol consumption (< 30 g/d in men and < 20 g/d in women), and exclusion of secondary diseases that may cause hepatic steatosis (Hepatitis B Virus, Hepatitis C Virus, Liver Cirrhosis, Autoimmune Liver Disease, etc.) are used as the criteria1.
Obesity: BMI was used to determine overweight/obesity. The formula was BMI = weight(kg)/height2(m2), where BMI < 24 kg/m2 was normal weight, 24 kg/m2 ≤ BMI < 28 kg/m2 was overweight, and ≥ 28 kg/m2 was obese25. WC is used to measure central obesity, men’s WC ≥ 90 cm and women’s WC ≥ 80 cm can be judged as central obesity26.
Definitions of outcomes
The emergence of the study’s findings was defined as the first event of nonfatal CVDs and was coded according to the ICD-10, including hypertension (ICD-10: I10-I15), coronary heart disease (ICD-10: I20-I25), and stroke (ICD-10: I60-I65).
Hypertension: hypertension was defined as systolic blood pressure (SBP) ≥ 140 and/or diastolic blood pressure (DBP) ≥ 90 mmHg27, and/or those who self-reported in epidemiological surveys and were diagnosed as hypertensive by hospitals of the second level or above; and/or those who were diagnosed as hypertensive in their previous hospitalized medical records. Satisfaction of one of the three criteria was sufficient. Of these, if there was duplication with self-reporting and testing for hypertension, the record of the earliest time of diagnosis was retained.
CHD/Stroke: patients who self-report CHD/stroke in epidemiological surveys and can provide proof of clinical diagnosis in hospitals of the second level or above, and/or patients diagnosed with CHD/stroke in previous hospitalized medical records.
Assessment of lifestyle factors and covariates
High-salt and high-fat diets were defined as > 6 g/d of salt and > 30 g/d of cooking oil use, respectively. Physical activity status was categorized as never, occasional and regular. Never means no or very little exercise; occasionally means more than 30 min of exercise 1–2 times per week; and regularly means more than 30 min of exercise 3 or more times per week. Tobacco use includes smoking, quitting and non-smoking. A person who has smoked at least one cigarette a day for more than six months is defined as a smoker, a person who has ever met the criteria for smoking but has stopped smoking for more than six months is defined as a cessation smoker, and non-smoking is defined as a non-smoker who has never smoked or who has smoked occasionally but has not met the criteria for smoking. Alcohol use included alcohol use, abstinence, and no alcohol use. People who drink alcohol on average at least once a week for at least the past 6 months are called “drinkers”; People who met the drinking criteria in the past but have stopped drinking for more than 6 months are considered “abstaining”; Nondrinkers are those who never drink or who drink occasionally but do not meet drinking criteria. In addition, according to the type, frequency and amount of alcohol consumed by the study participants, drinking index (g/week) = number of drinks per week * amount of alcohol per drink (mL) * alcohol coefficient * 0.8. The alcohol coefficient for white wine was 0.50, for red wine 0.12, and for beer 0.04. Drinking ≥ 210 g/week for males, and ≥ 140 g/week for females, was defined as excessive alcohol consumption. Family history of CVD: at least one of the first-degree relatives of the study participant had a cardiovascular type (hypertension, stroke, or CHD) of disease. T2DM was determined by FPG values, and study participants with FPG between 5.6 and 6.9 mmol/L on physical examination were determined to be pre-diabetic28, those with FPG ≥ 7.0 mmol/L on physical examination or those who self-reported T2DM in the epidemiological survey and were able to provide a certificate of diagnosis from a hospital of the second level or higher were defined as having diabetes mellitus. In this study, we chose three basic items for blood lipid testing: TC, TG, and HDL-C, and dyslipidemia was diagnosed when one of them was met, i.e., when TC ≥ 6.2 mmol/L, TG ≥ 1.7 mmol/L29, and HDL-C < 1.0 mmol/L in men or < 1.3 mmol/L in women1. The diagnostic criteria for metabolic syndrome30 encompass WC abnormalities, along with two or more of the following conditions: abnormal blood glucose levels, altered HDL-C levels, abnormal triglyceride levels, and blood pressure exceeding 130/85 millimeters of mercury. The degree of hepatic fibrosis was assessed using the NAFLD Fibrosis Score (NFS).The NFS was calculated as NFS = -1.675 + 0.037* Age (years) + 0.094 * BMI (kg/m2) + 1.13* Pre-diabetes/Diabetes (yes = 1, no = 0) + 0.99*AST/ALT − 0.013 * PLT (109/L) -0.66 * ALB (g/dl)31,32. When NFS < -1.455, advanced liver fibrosis could be excluded, when − 1.455 ≤ NFS < 0.676, the degree of liver fibrosis was uncertain, and when NFS ≥ 0.676, advanced liver fibrosis could be indicated.
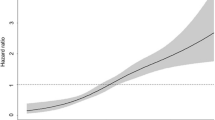
Statistical analysis
In this study, the number of cases and constituent ratio (n, %) were used to describe the categorical data, and the mean ± standard deviation (\(\:\stackrel{-}{x}\pm\:s\)) was used to describe the continuous variables. Continuous variables were compared between groups using t-test or analysis of variance, and categorical data were compared between groups using chi-square test. Multifactorial Cox proportional risk models were used to estimate hazard ratios (HR) and 95% confidence interval (CI) for major CVDs. Additive and multiplicative models were used to assess the interaction of NAFLD with different indicators of obesity on CVDs risk. Differences in the risk of developing CVDs in obese patients with NAFLD were observed by stratified analyses when a population of normal weight and without NAFLD was used as a reference.
Data analysis was completed by SPSS 26.0 and R 4.2.1 statistical software. All analyses were performed by two-sided test, and P < 0.05 was considered statistically significant.
Ethics approval and consent to participate
All study participants provided written informed consent, and the study protocol was approved by the Ethics Committees of the Public Health School of Lanzhou University (2015–01). Moreover, all the methods of the study were carried out in accordance with the relevant guidelines and regulations, in line with the Declaration of Helsinki.
Result
General characteristics of the study participants
A total of 19,399 study participants were ultimately enrolled in this investigation, with a mean age of 42.28 ± 10.80 years. There were 11,341 males, with a male to female ratio of 1.41:1. The prevalence of pre-diabetes and diabetes is 12.46% and 3.69% respectively. 37.19% had a family history of CVDs. 32.06% of them were overweight or obese and 27.46% had abdominal obesity. The mean values of SBP and DBP were 114.52 ± 12.93mmHg and 73.48 ± 7.99mmHg, respectively. Abnormalities in TC, TG and HDL-C were 4.39%, 39.51% and 19.34% respectively. 11.9% had metabolic syndrome and 1.52% had advanced liver fibrosis. Men had more high salt diets, high fat diets, never exercised, smoked, drank alcohol, suffered from diabetes mellitus, overweight/obesity, abdominal obesity, and triglyceride abnormalities than women; men’s mean blood pressure was also higher than women’s; and metabolic syndrome affects more men than women; as well as men’s advanced fibrosis of the liver was more severe than women’s; in addition, women’s mean HDL-C and TC were slightly higher than men’s, and the above differences were all statistically significant P < 0.05). The mean values of HDL-C in men and women and TG in men were higher than the diagnostic criteria for their abnormal values. See Table 1 for details.
As shown in Table 2, there were 3129 patients with NAFLD, with a mean age of 43.35 ± 11.07 years, and 723 major cardiovascular events. The NAFLD population with and without CVD was predominantly male. The prevalence of diabetes or pre-diabetes in patients with NAFLD was 27.78%, and 30.49% met the diagnostic criteria for metabolic syndrome. Compared to NAFLD patients without CVD, the NAFLD population with CVD was older, had more pre-diabetes and diabetes, higher levels of several metabolic markers (BMI, WC, SBP, DBP, TG, TC) (p < 0.05), more people with metabolic syndrome and more advanced liver fibrosis.
Association between NAFLD and CVDs
Table 3 delineates the cumulative incidence rate of these severe CVDs among NAFLD sufferers tallied at 23.11%, markedly surpassing that observed within the general populace (P < 0.001). Table S1 showed that 529 men and 194 women with NAFLD developed major CVDs, and the cumulative incidence rates of major CVDs were 21.87% and 27.32%, respectively, figures markedly eclipsing those observed in counterparts devoid of NAFLD (P < 0.001). Notably, the cumulative incidence of CVDs among women with NAFLD surpassed that among men (P = 0.002). Multivariate Cox proportional hazards regression model was used to analyze the influence of NAFLD on the risk of major CVDs, and the results are shown in Table 3. After adjusting for some confounding factors, the risk of major CVDs in patients with NAFLD was 1.17 times higher than that in people without NAFLD. Among them, the HR and 95% CI for major CVDs in male and female NAFLD patients were 1.165 (1.050,1.292) and 1.220 (1.028,1.447), respectively, as shown in Table S1.
Association between obesity and CVDs
The results in Table S2 show that all three indicators, BMI, WC, and the combination of BMI and WC, were independently associated with the risk of developing CVDs. In particular, BMI obesity was 1.77 times higher than the risk of CVDs in the total population than in the normal population; BMI obesity increased the risk of developing CVDs by 70.1% and 89.2% in the male and female populations, respectively. The risk of developing CVDs in the centrally obese population was smaller than in the overweight/obese population with BMI, increasing the risk of developing CVDs by 25.7%, 24.2%, and 30.8% in the overall, male, and female populations, respectively. In the combined of BMI and WC, the risk of CVDs in patients with both BMI obesity and central obesity was 1.81 times higher than that in the normal population. Among the male and female populations, the risk of CVDs in subjects with both BMI obesity and central obesity was 1.76 times and 1.91 times higher than that in the normal population, respectively. Data under the gender subgroups are detailed in Table S3.
Risk analysis of NAFLD and CVDs under the same obesity level
Table 4, S4, and S5 show that after adjusting for confounding factors, the risk of CVDs in NAFLD group was 1.244 times higher than that in non-NAFLD group in men with overweight and central obesity (95%CI: 1.031, 1.500). In addition, the risk values of CVDs in NAFLD patients in other groups were not statistically significant.
Additive and multiplicative interaction effects of NAFLD and obesity on the risk of CVD
The findings elucidate a significant individual association between NAFLD and obesity with the risk of CVDs in this investigation. Therefore, further interaction analyses were conducted, revealing no additive interaction between NAFLD and any obesity indicators. Consequently, no further subgroup analyses by sex were deemed necessary. The “obesity*NAFLD” under different obesity indicators was included in the Cox proportional risk model, and a multifactorial model was constructed. After adjusting for some variables, it was found that there was a multiplicative effect of BMI, WC, and the combination of BMI and WC with NAFLD on the risk of the development of major CVDs in the total population, men and women, respectively. The interaction effect, in which the combination of both risk factors increased the risk of developing major CVDs above the risk of developing CVDs in the presence of only one risk factor, was statistically significant (Pinteraction<0.05). Detailed results are provided in Table 5 and S6.
Stratified analysis of the relationship between NAFLD, different obesity indicators and CVDs
Utilizing subjects with normal body weight and non-NAFLD as the reference cohort, Table 6, S7, and S8 delineate the adjusted risk of CVDs across various combinations of obesity and NAFLD. The results found that when compared to the cohort devoid of NAFLD and with a normal BMI, individuals harboring both NAFLD and obesity exhibited a significantly heightened risk of major CVDs. The corresponding incidence risks and 95%CI were as follows: 1.724 (1.404, 2.118) for males, 1.980 (1.438, 2.727) for females, and 1.790 (1.508, 2.126) for the total population. The risk of NAFLD and obesity in women was higher than that in men and the total population. Increased BMI affects the increased risk of developing CVDs, both within the non-NAFLD and NAFLD groups. The risk of CVDs in overweight/obese non-NAFLD subjects was similar to that in NAFLD patients, and even in the total study population, the risk of CVDs in obese non-NAFLD patients was slightly higher than that in obese NAFLD subjects (1.796 VS 1.790). And in female population, overweight patients without NAFLD had a higher risk of CVDs than overweight patients with NAFLD (1.403 VS 1.307). In addition, the risk of CVDs in NAFLD patients with normal weight was not significant in each group.
The factor-adjusted risks of developing CVDs for different combinations of WC and NAFLD are shown in Table 6, respectively, using those with normal baseline waist circumference indices without NAFLD as the reference. In the total population and different gender groups, the risk of NAFLD and central obesity was higher than other groups, and the HR (95%CI) were 1.356(1.213,1.517), 1.356 (1.188, 1.548) and 1.405 (1.132, 1.744), respectively. Similarly, Tables S7 and S8 show that the risk of developing NAFLD in the female population with abdominal obesity group was higher than that of both the male and total population. Also there was no meaningful risk of developing CVDs in NAFLD patients with normal waist circumference in all groups.
The association of BMI and WC with NAFLD on CVDs was further analyzed. In the female population, a concurrent diagnosis of BMI obesity and abdominal obesity had the greatest impact on the occurrence of CVDs in patients with NAFLD, with an HR(95% CI) of 2.112 (1.498, 2.977) (Table S7). However, in the overall and male populations BMI obese with normal WC instead had a greater impact on the risk of developing CVDs in the NAFLD population than the other groups, with the risk of developing CVDs being 2.161 and 2.365 times greater than that of those without NAFLD and with normal weight, respectively. See Table 6 and Table S8.
Discussion
A prospective investigation, conducted within the framework of the esteemed Jinchang cohort, has corroborated that NAFLD and obesity stand as independent precursors to CVDs. Moreover, this study has illuminated the potential synergistic interplay between NAFLD and obesity in precipitating the onset of CVDs. Notably, in comparison to the singular assessment of obesity, the amalgamated assessment incorporating both BMI and WC demonstrates superior efficacy in gauging the nexus between obesity, NAFLD, and CVDs. Gender-stratified analysis reveals consistently heightened risks among females relative to their male counterparts. In light of these discernments, prudent counsel advocates for the vigilant management of excess adiposity and waist girth within the Jinchang cohort, with a view to mitigating the cardiovascular risk burden among NAFLD-afflicted individuals. Particular emphasis is warranted for female NAFLD patients exhibiting elevated BMI and WC metrics.
The current investigation has discerned that individuals afflicted with NAFLD face an elevated susceptibility to CVDs compared to the broader populace, mirroring the findings of numerous antecedent inquiries33,34. Not only is NALFD associated with established cardiovascular risk factors such as abdominal obesity, atherogenic dyslipidemia, and IR35,36,37, patients with NAFLD also exhibit a range of non-traditional cardiovascular risk factors. These include hyperuricemia38, vitamin D deficiency39, etc. Our study found that the cumulative incidence and risk of developing major CVDs were higher in women than in the male population. This is similar to the findings of Allen et al.40. Another study also indicated that the female advantage in protection from CVDs was lost in NAFLD subjects, with the occurrence of CVDs and deaths being twice as common in women as in men among approximately 108,711 NAFLD patients41. NAFLD has been reported to be diagnosed predominantly in middle-aged men and estrogen-deficient menopausal women42. Estrogen is a protective factor in the development of NAFLD43, and deficiency leads to the development of postmenopausal metabolic syndrome thus leading to the development of severe steatosis and fibrosis in women closely related. Additional evidence from epidemiologic studies suggests that menopause puts women at increased risk for CVDs, influenced by visceral obesity, atherogenic dyslipidemia, dysregulated glucose homeostasis, NAFLD, and hypertension44. The average age of women in the population included in this study was relatively older, leading to a greater likelihood of female NAFLD patients being in a menopausal state, and therefore a greater risk of increased development of CVDs compared to men. However, there are also different research results. A retrospective observational cohort study45in the United States and the Du et al.46 study both indicated that women with NAFLD generally have a more favorable CVDs risk profile than men. The difference of results was significantly related to factors such as gender and age.
Although obesity has been shown to be a traditional risk factor for CVDs47,48, we still explored the relationship between obesity and CVDs, confirming that obesity also has an independent effect on the risk of developing CVDs in the Jinchang cohort population. Upon further adjustment for covariates, it emerged that the risk of developing CVDs manifested a higher magnitude when influenced by the presence of obesity as opposed to the independent impact of NAFLD. It is posited that this discrepancy may be correlated with the diminished degree of hepatic fibrosis observed within the confines of the present study cohort. In the same obesity group, there was no significant difference in the risk of major CVDs between people exposed to NAFLD and those not, indicating that regardless of NAFLD, obesity significantly affected the occurrence of CVDs, and the impact of obesity on CVDs was more significant than that of NAFLD. Such findings lay the groundwork for postulating the existence of a plausible synergistic interplay between NAFLD and obesity in the pathogenesis of CVDs. A study derived from the Kailuan cohort49 corroborates the findings of the present investigation, indicating a lack of statistically significant variance between non-NAFLD and NAFLD cohorts within the normal-weight populace. There are fewer and controversial studies on the incidence and risk of CVD in NAFLD at the same level of obesity, and studies comparing NAFLD to non-NAFLD in normal weight populations lack high-quality evidence50. A study conducted by Feng et al.51 based on a population in northern China showed that NAFLD increased the risk of hypertension within the normal weight group, but within the obese group, the difference in the risk of hypertension with and without NAFLD was not statistically significant.
The interaction effect analysis of obesity and NAFLD in this study found that obesity and NAFLD had a positive multiplicative interaction, but not an additive interaction, on CVDs. The risk of developing major CVDs was found to increase with increasing BMI class in both non-NAFLD and NAFLD populations. And the risk of major CVDs in the obese female NAFLD population was higher than that in males, which was associated with a higher cumulative prevalence of both NAFLD and obesity in females than in males in this study. In addition, the risk of NAFLD was not statistically significant in people with normal body weight. This is consistent with the results of a cross-sectional study that reported a lower incidence of CVDs in Americans with NAFLD but not obesity than in obese NAFLD subjects52. Lin et al.53found a synergistic effect of fatty liver and overweight on the development of ischemic heart disease based on a cross-sectional study of middle-aged male workers in Taiwan. This may be due to the fact that high levels of adiposity worsen most CVD risk factors, including lipids, blood pressure, insulin resistance, and inflammation54. Thus the normal weight NAFLD group was healthier than obese NAFLD subjects in terms of blood pressure and lipids49. The WC metrics selected for grouping found that, unlike the BMI results, patients with NAFLD who were centrally obese also had a slightly higher risk of developing CVDs compared with those with non-NAFLD who were centrally obese. This is similar to the results of a previous study. Matina et al.55 found a multiplicative interaction between NAFLD and WC in a 10-year follow-up of 3042 participants with CVDs in Greece. There are fewer studies on the association of NAFLD and WC on major CVDs, and the critical value of WC varies in studies from different countries56,57,58, and more prospective clinical studies are needed to make a possible interpretation. Previous studies have shown that the combination of BMI and WC not only better identifies high-risk obesity phenotypes, but also has better predictive power for CVDs risk factors than either metric alone59,60. The results of the present study also support the conclusion that the combination of BMI and central obesity metrics identified a higher risk of CVDs in both the total population and in both sexes than did BMI and central obesity metrics alone. The same results were obtained in a study that observed that the relationship between NAFLD and obesity status and CVDs was altered by central obesity (Pinteraction = 0.062), with central obesity being associated with a higher risk of CVDs in the obese NAFLD group and in the obese non-NAFLD group49.
This study possesses certain limitations warranting acknowledgment. Given the chronic nature of CVDs and their propensity to manifest in middle-aged and elderly cohorts, there exists the potential for underestimation of study outcomes. While the study spanned a commendable 7-year follow-up period, an extended duration would afford a more nuanced understanding of risk dynamics. Furthermore, the reliance on baseline obesity metrics neglects potential fluctuations in adiposity over time, which may influence long-term CVDs susceptibility. Moreover, considering that there is no definitive treatment for NAFLD medication, pharmacological treatment for T2DM may be effective for NAFLD, and we will consider the effect of this factor on the occurrence of CVD in obese NAFLD in future follow-up. Second, the data in this study came from the Chinese metal-exposed workers cohort61, and the Jinchang cohort had higher levels of urinary metals compared with the general occupational population. There is evidence that heavy metals have a lipotropic effect, resulting in obesity and increasing the risk of NAFLD and CVD62,63, e.g., serum copper bioavailability can help predict the risk of CVD in obese NAFLD patients64. However, the effect of heavy metals on the results of the study was not considered in this study for the time being. In the future, this study will delve deeper to assess the effect of heavy metal exposure in the context of the relationship between obesity, NAFLD, and CVDs.
Conclusion
In conclusion, we found that NAFLD was independently associated with CVDs. Moreover, we found a significant synergistic effect of NAFLD and obesity on CVDs risk. According to our findings, the prevention and intervention of NAFLD and the control of body weight within the normal range are the key to healthy intervention of CVDs, and we should pay more attention to obese patients with NAFLD.
Data availability
The data from this study will not be shared publicly. All data included in this study are available upon request by contact with the corresponding author.
Abbreviations
- NAFLD:
-
Non-alcoholic fatty liver disease
- IR:
-
Insulin resistance
- HCC:
-
Hepatocellular carcinoma
- CVDs:
-
Cardiovascular diseases
- T2DM:
-
Type 2 diabetes mellitus
- CHD:
-
Coronary heart disease
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TG:
-
Triglyceride
- HDL-C:
-
High-density lipoprotein cholesterol
- NFS:
-
Non-alcoholic fatty liver disease fibrosis score
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention. and treatment for nonalcoholic fatty liver disease: a 2018 update. Zhonghua gan zang bing za zhi = Zhonghua ganzangbing zazhi = Chin J Hepatol. 26, 195–203. https://doi.org/10.3760/cma.j.issn.1007-3418.2018.03.008 (2018).
Diehl, A. M., Day, C. & Cause,. Pathogenesis, and treatment of Nonalcoholic Steatohepatitis. N. Engl. J. Med.377, 2063–2072. https://doi.org/10.1056/NEJMra1503519 (2017).
Hassen, G. et al. Nonalcoholic fatty liver disease: an emerging modern-day risk factor for Cardiovascular Disease. Cureus14, e25495. https://doi.org/10.7759/cureus.25495 (2022).
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology (Baltimore Md)64, 73–84. https://doi.org/10.1002/hep.28431 (2016).
Targher, G., Day, C. P. & Bonora, E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N. Engl. J. Med.363, 1341–1350. https://doi.org/10.1056/NEJMra0912063 (2010).
Adams, L. A., Anstee, Q. M., Tilg, H. & Targher, G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut66, 1138–1153. https://doi.org/10.1136/gutjnl-2017-313884 (2017).
Alexander, M. et al. Non-alcoholic fatty liver disease and risk of incident acute myocardial infarction and stroke: findings from matched cohort study of 18 million European adults. BMJ (Clinical Res. ed.)367, l5367. https://doi.org/10.1136/bmj.l5367 (2019).
Wu, S. et al. Association of non-alcoholic fatty liver disease with major adverse cardiovascular events: A systematic review and meta-analysis. Sci. Rep.6, https://doi.org/10.1038/srep33386 (2016).
Zhou, J. et al. Epidemiological features of NAFLD from 1999 to 2018 in China. Hepatology (Baltimore Md)71, 1851–1864. https://doi.org/10.1002/hep.31150 (2020).
Ballestri, S. et al. Risk of cardiovascular, cardiac and arrhythmic complications in patients with non-alcoholic fatty liver disease. World J. Gastroenterol.20, 1724–1745. https://doi.org/10.3748/wjg.v20.i7.1724 (2014).
Gutiérrez-Cuevas, J., Santos, A. & Armendariz-Borunda, J. Pathophysiological Molecular Mechanisms of Obesity: A Link between MAFLD and NASH with Cardiovascular Diseases. Int. J. Mol. Sci.22, https://doi.org/10.3390/ijms222111629 (2021).
Guo, Y. et al. Overweight and obesity in Young Adulthood and the risk of stroke: a Meta-analysis. J. Stroke Cerebrovasc. Diseases: Official J. Natl. Stroke Association25, 2995–3004. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.018 (2016).
Zhang, Y. et al. The prevalence of obesity-related hypertension among middle-aged and older adults in China. Front. Publ. Health10, https://doi.org/10.3389/fpubh.2022.865870 (2022).
Li, L. et al. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes. Reviews: Official J. Int. Association Study Obes.17, 510–519. https://doi.org/10.1111/obr.12407 (2016).
Kim, D. & Kim, W. R. Nonobese fatty liver disease. Clin. Gastroenterol. Hepatology: Official Clin. Pract. J. Am. Gastroenterological Association15, 474–485. https://doi.org/10.1016/j.cgh.2016.08.028 (2017).
Kee, C. C. et al. Association of BMI with risk of CVD mortality and all-cause mortality. Public Health. Nutr.20, 1226–1234. https://doi.org/10.1017/s136898001600344x (2017).
Choi, S. et al. Association of Obesity or Weight Change with Coronary Heart Disease among Young adults in South Korea. JAMA Intern. Med.178, 1060–1068. https://doi.org/10.1001/jamainternmed.2018.2310 (2018).
Romero-Corral, A. et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet (London England)368, 666–678. https://doi.org/10.1016/s0140-6736(06)69251-9 (2006).
Xue, R. et al. Abdominal obesity and risk of CVD: a dose-response meta-analysis of thirty-one prospective studies. Br. J. Nutr.126, 1420–1430. https://doi.org/10.1017/s0007114521000064 (2021).
de Koning, L., Merchant, A. T., Pogue, J. & Anand, S. S. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur. Heart J.28, 850–856. https://doi.org/10.1093/eurheartj/ehm026 (2007).
Camhi, S. M. et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obes. (Silver Spring Md)19, 402–408. https://doi.org/10.1038/oby.2010.248 (2011).
Mongraw-Chaffin, M. et al. The sex and race specific relationship between Anthropometry and Body Fat Composition determined from computed tomography: evidence from the multi-ethnic study of atherosclerosis. PLoS ONE10, e0139559. https://doi.org/10.1371/journal.pone.0139559 (2015).
Bai, Y. et al. Cohort Profile Update: the China Metal-exposed workers Cohort Study (Jinchang Cohort). Eur. J. Epidemiol.37, 641–649. https://doi.org/10.1007/s10654-022-00875-4 (2022).
Bai, Y. et al. Cohort Profile: the China Metal-exposed workers Cohort Study (Jinchang Cohort). Int. J. Epidemiol.46, 1095–1096e. https://doi.org/10.1093/ije/dyw223 (2017).
Chinese Nutrition Society Obesity Prevention and Control Section; Chinese Nutrition Society Clinical Nutrition Section; Chinese Preventive Medicine Association Behavioral Health Section; Chinese Preventive Medicine Association Sports and Health Section. Expert Consensus on Obesity Prevention and Treatment in China. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 43, 609–626. https://doi.org/10.3760/cma.j.cn112338-20220402-00253 (2022).
World Health Organization. Regional Office for the Western, P. The Asia-Pacific perspective: redefining obesity and its treatment. 55p. Coordinated by the International Diabetes Institute; co-sponsored jointly by the Regional Office for the Western Pacific (WPRO), World Health Organization, the International Association for the Study of Obesity and the International Obesity Task Force. Sydney: Health Communications Australia. (2000).
Joint Committee for Guideline Revision. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-a report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol: JGC 16, 182–241. https://doi.org/10.11909/j.issn.1671-5411.2019.03.014 (2019).
Jia, W. et al. Standards of medical care for type 2 diabetes in China 2019. Diab/Metab Res Rev35, e3518. https://doi.org/10.1002/dmrr.3158 (2019).
Joint committee issued Chinese guideline for the management of dyslipidemia in adults. 2016 Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin xue guan bing za zhi 44, 833–853. https://doi.org/10.3760/cma.j.issn.0253-3758.2016.10.005 (2016).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation120, 1640–1645. https://doi.org/10.1161/circulationaha.109.192644 (2009).
Vilar-Gomez, E. & Chalasani, N. Non-invasive assessment of non-alcoholic fatty liver disease: clinical prediction rules and blood-based biomarkers. J. Hepatol.68, 305–315. https://doi.org/10.1016/j.jhep.2017.11.013 (2018).
Buzzetti, E., Lombardi, R., De Luca, L. & Tsochatzis, E. A. Noninvasive assessment of fibrosis in patients with nonalcoholic fatty liver disease. Int. J. Endocrinol. 2015, 343828. https://doi.org/10.1155/2015/343828 (2015).
Liang, Y. et al. Association of MAFLD with Diabetes, chronic kidney Disease, and Cardiovascular Disease: A 4.6-Year Cohort Study in China. J. Clin. Endocrinol. Metab.107, 88–97. https://doi.org/10.1210/clinem/dgab641 (2022).
Simon, T. G., Roelstraete, B., Hagström, H., Sundström, J. & Ludvigsson, J. F. Non-alcoholic fatty liver disease and incident major adverse cardiovascular events: results from a nationwide histology cohort. Gut71, 1867–1875. https://doi.org/10.1136/gutjnl-2021-325724 (2022).
Angulo, P. Nonalcoholic fatty liver disease. N. Engl. J. Med.346, 1221–1231. https://doi.org/10.1056/NEJMra011775 (2002).
Marchesini, G. et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatol. (Baltimore Md)37, 917–923. https://doi.org/10.1053/jhep.2003.50161 (2003).
Ratziu, V., Bellentani, S., Cortez-Pinto, H., Day, C. & Marchesini, G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J. Hepatol.53, 372–384. https://doi.org/10.1016/j.jhep.2010.04.008 (2010).
Li, Y., Xu, C., Yu, C., Xu, L. & Miao, M. Association of serum uric acid level with non-alcoholic fatty liver disease: a cross-sectional study. J. Hepatol.50, 1029–1034. https://doi.org/10.1016/j.jhep.2008.11.021 (2009).
Targher, G. et al. Associations between serum 25-hydroxyvitamin D3 concentrations and liver histology in patients with non-alcoholic fatty liver disease. Nutr. Metab. Cardiovasc. Diseases: NMCD17, 517–524. https://doi.org/10.1016/j.numecd.2006.04.002 (2007).
Allen, A. M. et al. Women with nonalcoholic fatty liver Disease Lose Protection against Cardiovascular Disease: a longitudinal cohort study. Am. J. Gastroenterol.114, 1764–1771. https://doi.org/10.14309/ajg.0000000000000401 (2019).
Khalid, Y. S. et al. Increased cardiovascular events and mortality in females with NAFLD: a meta-analysis. Am. J. Cardiovasc. Dis.10, 258–271 (2020).
Hashimoto, E. & Tokushige, K. Prevalence, gender, ethnic variations, and prognosis of NASH. J. Gastroenterol.46(Suppl 1), 63–69. https://doi.org/10.1007/s00535-010-0311-8 (2011).
Bruno, S. et al. Incidence and risk factors for non-alcoholic steatohepatitis: prospective study of 5408 women enrolled in Italian tamoxifen chemoprevention trial. BMJ (Clinical Res. ed.)330, 932. https://doi.org/10.1136/bmj.38391.663287.E0 (2005).
Anagnostis, P., Lambrinoudaki, I., Stevenson, J. C. & Goulis, D. G. Menopause-associated risk of cardiovascular disease. Endocr. Connections11, https://doi.org/10.1530/ec-21-0537 (2022).
Pemmasani, G., Yandrapalli, S. & Aronow, W. Sex differences in cardiovascular diseases and associated risk factors in non-alcoholic steatohepatitis. Am. J. Cardiovasc. Dis.10, 362–366 (2020).
Du, T. et al. Sex differences in the impact of nonalcoholic fatty liver disease on cardiovascular risk factors. Nutr. Metabolism Cardiovasc. Diseases: NMCD27, 63–69. https://doi.org/10.1016/j.numecd.2016.10.004 (2017).
Garvey, W. T. et al. Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes. Metab. Clin. Exp.85, 32–37. https://doi.org/10.1016/j.metabol.2018.02.002 (2018).
Battineni, G. et al. Impact of Obesity-Induced Inflammation on Cardiovascular Diseases (CVD). Int. J. Mol. Sci.22, https://doi.org/10.3390/ijms22094798 (2021).
Lan, Y. et al. Outcomes of subjects who are lean, overweight or obese with nonalcoholic fatty liver disease: a cohort study in China. Hepatol. Commun.6, 3393–3405. https://doi.org/10.1002/hep4.2081 (2022).
Semmler, G. et al. Nonalcoholic fatty liver disease in lean subjects: associations with Metabolic Dysregulation and Cardiovascular Risk-A single-center cross-sectional study. Clin. Translational Gastroenterol.12, e00326. https://doi.org/10.14309/ctg.0000000000000326 (2021).
Feng, R. N. et al. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. World J. Gastroenterol.20, 17932–17940. https://doi.org/10.3748/wjg.v20.i47.17932 (2014).
Weinberg, E. M. et al. Lean americans with nonalcoholic fatty liver Disease have lower rates of cirrhosis and Comorbid diseases. Clin. Gastroenterol. Hepatology: Official Clin. Pract. J. Am. Gastroenterological Association19, 996-1008e1006. https://doi.org/10.1016/j.cgh.2020.06.066 (2021).
Lin, Y. C., Lo, H. M. & Chen, J. D. Sonographic fatty liver, overweight and ischemic heart disease. World J. Gastroenterol.11, 4838–4842. https://doi.org/10.3748/wjg.v11.i31.4838 (2005).
Ortega, F. B., Lavie, C. J. & Blair, S. N. Obesity and Cardiovascular Disease. Circul. Res.118, 1752–1770. https://doi.org/10.1161/circresaha.115.306883 (2016).
Kouvari, M. et al. Skeletal muscle mass and abdominal obesity are independent predictors of hepatic steatosis and interact to predict ten-year cardiovascular disease incidence: data from the ATTICA cohort study. Clin. Nutr.41, 1281–1289. https://doi.org/10.1016/j.clnu.2022.03.022 (2022).
Zhou, B. F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci.: BES15, 83–96 (2002).
Seo, J. A. et al. The cutoff values of visceral fat area and waist circumference for identifying subjects at risk for metabolic syndrome in elderly Korean: Ansan Geriatric (AGE) cohort study. BMC public. health9, https://doi.org/10.1186/1471-2458-9-443 (2009).
Arnaiz-Villena, A. et al. Amerindians normalized waist circumference and obesity diagnosis standarized by biochemical and HLA data. Mol. Biol. Rep.39, 4875–4878. https://doi.org/10.1007/s11033-011-1282-4 (2012).
Du, S. M. et al. Relationship of body mass index, waist circumference and cardiovascular risk factors in Chinese adult. Biomed. Environ. Sci.: BES23, 92–101. https://doi.org/10.1016/s0895-3988(10)60037-2 (2010).
Zhu, S. et al. Combination of BMI and Waist circumference for identifying Cardiovascular Risk factors in whites. Obes. Res.12, 633–645. https://doi.org/10.1038/oby.2004.73 (2004).
Yang, A. M. et al. Heavy metal assessment among Chinese nonferrous metal-exposed workers from the Jinchang cohort study. Biomed. Environ. Sci.: BES30, 530–534. https://doi.org/10.3967/bes2017.070 (2017).
Tinkov, A. A. et al. Adipotropic effects of heavy metals and their potential role in obesity. Fac. Reviews. 10https://doi.org/10.12703/r/10-32 (2021).
Yang, A. M. et al. Environmental heavy metals and cardiovascular diseases: Status and future direction. Chronic Dis. Translational Med.6, 251–259. https://doi.org/10.1016/j.cdtm.2020.02.005 (2020).
Tarantino, G., Porcu, C., Arciello, M., Andreozzi, P. & Balsano, C. Prediction of carotid intima-media thickness in obese patients with low prevalence of comorbidities by serum copper bioavailability. J. Gastroenterol. Hepatol.33, 1511–1517. https://doi.org/10.1111/jgh.14104 (2018).
Acknowledgements
We express our sincere gratitude to all participants and researchers of the Jinchang cohort study.
Author information
Authors and Affiliations
Contributions
Conceptualization, X.W., M.W., and S.Z.; Data curation, X.W., J.Y., J.T., and X.L.; Methodology, X.W., and J.Y.; Software, X.W., J.Y., and J.T.; Validation, X.W., and X.L.; Visualization, X.W.; Writing - original draft, X.W.; Writing - review & editing, R.W., Y.L., Y.B., M.W., and S.Z.; Resources, Y.B., M.W., and S.Z.; Supervision, M.W. and S.Z.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., You, J., Tang, J. et al. Interaction between non-alcoholic fatty liver disease and obesity on the risk of developing cardiovascular diseases. Sci Rep 14, 24024 (2024). https://doi.org/10.1038/s41598-024-74841-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-74841-3