Abstract
After developing job-exposure matrices (JEMs) for screen and sedentary time, we aimed to assess the associations between the JEM-derived exposures and various ocular diseases. We collected data from patients hospitalized from 2005 to 2021. JEMs were developed from 41,718 patients with occupational information and screen and sedentary times. The adjusted means of screen and sedentary time were calculated for 143 occupational groups and categorized into three classes based on the tertiles. The associations between ocular diseases and these JEM-derived exposures were examined using multivariable conditional logistic regression for 727,589 patients. The odds ratios of the class with highest screen time were 1.05 (95% confidence interval, 1.01–1.09) for cataract, 1.24 (1.06–1.45) for primary open-angle glaucoma (POAG), 1.26 (1.06–1.49) for rhegmatogenous retinal detachment (RRD), 1.49 (1.26–1.76) for ptosis, and 0.39 (0.27–0.57) for pterygium. The odds ratios of the class with highest sedentary time were 1.05 (1.01–1.09) for cataract, 1.24 (1.05–1.46) for RRD, 1.68 (1.42–1.99) for ptosis, and 0.60 (0.42–0.84) for pterygium. Both screen and sedentary time were positively associated with cataract, RRD and ptosis. Interestingly, POAG had a positive association with only screen time. Please check and confirm that the authors and their respective affiliations have been correctly identified and amend if necessary."I have confirmed that the content is correct. No amendments are necessary.Please check article title if captured correctly."?>"I have confirmed that the content is correct. No amendments are necessary.
Similar content being viewed by others
Introduction
Visual display terminal (VDT)-related work refers to prolonged work using a monitor, such as a computer, and has multiple effects of accommodative demand in near work and blue light from the screen and physical effects of sitting for long hours. VDT work is associated with musculoskeletal pain in the neck and shoulders1. and ocular manifestations, including dry eyes, eye strain, and visual field abnormalities2,3,4,5. Sedentary work, an element of VDT-related work, is reportedly associated with obesity, diabetes, cardiovascular diseases (CVDs), and some cancers6. However, there is limited information about the association with other diseases. Additionally, the dose–response effect of these exposures remains unclear.
In contrast to the limited studies on screen and sedentary times at work, occupational or industrial history information is commonly collected7,8,9,10,11. Assuming that different occupations involve different exposures, job-exposure matrices (JEMs) have been used as tools to evaluate various exposure factors (e.g., chemical agents, radiation, and workplace physical exposures) from occupational information12,13,14. By leveraging JEMs, researchers could assess various exposures without direct measurements. In this study, we developed JEMs by evaluating the quantity of screen time or sedentary time according to occupation and industry groups. Therefore, occupational history could serve as surrogate indicators of screen and sedentary times by using JEMs.
Applying JEMs to a large occupational history dataset al.lows us to reveal the risks of various diseases associated with exposure to screen and sedentary times or either of them. Previously, we reported that screen time was possibly associated with glaucomatous visual field abnormality3,4; therefore, we aimed to verify whether robust results could be shown using the present data. Furthermore, as there are limited findings regarding the harmful effects of VDT-related work on the eyes2,3,4,5, we investigated the association between other ocular diseases and exposures to screen and sedentary times.
Subjects and methods
We conducted this study using the Inpatient Clinico-Occupational Database of Rosai Hospital Group (ICOD-R), a large-scale survey by the Japan Organization of Occupational Health and Safety (JOHAS), which includes approximately 250,000 cases per year from 34 regional core hospitals, as described in previous reports8,9,10. The ICOD-R is a detailed investigation of diseases, lifestyles, and working conditions, including medical chart information confirmed by physicians. Patients admitted to a JOHAS Group hospital between 1 April 2005 and 31 March 2021 were included in this study, and screen and sedentary times were obtained through interviews at each hospital based on a formatted questionnaire. All information in the ICOD-R was registered with the health information manager at each hospital. Informed written consent was obtained from all participants. From 2016 onwards, the consent acquisition method was changed to broad consent (opt-out). This study adhered to the tenets of the Declaration of Helsinki and conformed to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist15. Access to the dataset was granted by a research agreement between the JOHAS and the researchers. This study was approved by the JOHAS (approval no. R1–006) and the Research Ethics Committee of Tokai University School of Medicine (approval no. 18R–309). Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
All occupations and industries in this study were classified based on the Japan Standard Occupational Classification (JSOC) and the Japan Standard Industrial Classification (JSIC). All occupations were classified into 11 JSOC groups (A–K) as follows: A: Administrative and managerial workers, B: Professional and engineering, C: Clerical workers, D: Sales workers, E: Service workers, F: Security workers, G: Agriculture, forestry and fishery workers, H: Manufacturing process workers, I: Transport workers and machinery operators, J: Construction and mine workers, and K: Carrying and cleaning workers. All industries were classified into 19 JSIC groups (A–S) as follows: A: Agriculture and forestry, B: Fisheries, C: Mining and quarrying of stone, D: Construction, E: Manufacturing, F: Electricity, gas, heat supply, and water, G: Information and communications, H: Transport and postal services, I: Wholesale and retail trade, J: Finance and insurance, K: Real estate and goods rental and leasing, L: Scientific research, professional and technical services, M: Accommodations, eating and drinking services, N: Living-related and personal services and amusement services, O: Education, learning support, P: Medical, health care and welfare, Q: Postal services and industrial cooperatives, R: Other services, and S: Government, except elsewhere classified. Regarding these occupational data, we obtained the current and three past statuses, which reflect the lifetime occupational history to a reasonable degree.
We evaluated screen and sedentary times among 41,718 patients admitted from 2019 to 2021 without missing values and with occupational information (the current occupations), as shown in Supplemental Fig. 1 (DATA 1). The JEMs were developed in three steps. First, questionnaire responses (1: 0–1 h, 2: 1–4 h, 3: 4–8 h, 4: 8–12 h, 5: >12 h) were converted to continuous quantities (0.5, 2.5, 6, 10, and 14 h) for screen and sedentary times. Second, we calculated the adjusted mean values of screen and sedentary times using analysis of co-variance adjusted for age and sex according to 143 occupational groups (limited to groups with at least 5 people) classified using JSOC and JSIC. Finally, the 143 groups were classified into three classes (V1–V3 and S1–S3) based on tertiles of the adjusted mean values, in line with a widely used epidemiological approach.
Applying JEMs-derived screen and sedentary times to the longest-held occupations, we conducted a case-control study including 727,589 patients admitted from 2005 to 2021 with occupational information, as presented in Supplemental Fig. 1 (DATA 2). Clinical diagnoses were coded according to the World Health Organization’s International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD–10). Multiple analyses were performed independently for each ocular disease.
Cases were selected from the following ocular diseases with sufficient sample sizes (N > 100 before case-control matching) excluding symptoms: cataract (ICD–10 = H25.0, H25.1, H25.2, H25.8, H25.9, H26.9), primary open-angle glaucoma (POAG) (H40.1, H40.9), primary angle-closure glaucoma (H40.2), rhegmatogenous retinal detachment (RRD) (H33.0), ptosis (H02.4), eyelid entropion (H02.0), optic neuritis or neuropathy (ON) (H46.X), Vogt–Koyanagi–Harada disease (H30.8), pterygium (H11.0), diabetic retinopathy (DR) (H36.0), retinal vein occlusion (H34.8), and retinal artery occlusion (RAO) (H34.0, H34.1, H34.2).
Controls were selected based on the methodology described in previous studies10,16. We considered potential controls from several combinations of patients. They included patients admitted for the treatment of diseases of the skin and subcutaneous tissue (L00–L99), musculoskeletal system and connective tissue (M00–M99), or genitourinary system (N00–N99). Among them, we excluded those with a history of ophthalmic conditions (H00–H59). We randomly selected one control participant for each case, matched by sex (male or female), age (same strata in 5 years), admission date (same year), and admitting hospital (34 hospitals). None of the controls were matched more than once.
Applying conditional logistic regression for cases and matched controls, we calculated odds ratios (ORs) and 95% confidence intervals (CIs) of the prevalence of ocular diseases. We considered various confounding factors such as drinking (Never, Before, or Now), smoking (Never, Before, or Now), and lifestyle-related comorbidities (Yes or No; hypertension, diabetes, dyslipidemia, CVDs, and obesity). All analyses were performed using SAS version 9.4 for Windows (SAS Institute, Cary, NC, USA).
Results
To develop the JEMs, we enrolled 307,462 patients admitted between 1 April 2019 and 31 March 2021, as shown in Supplemental Fig. 1 (DATA 1). We assessed screen and sedentary times among 41,718 patients with adequate occupational and industrial information. The mean values of screen and sedentary times in this population were 3.4 ± 1.3 and 4.8 ± 1.2 h, respectively. Adjusted mean values of screen/sedentary time for 143 occupational groups are shown in Supplemental Table 1.
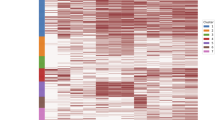
In Fig. 1A, the adjusted mean values of screen time are classified into three classes (V1–V3) based on tertiles and illustrated with different colours. The adjusted mean values of screen time for the V1, V2, and V3 classes were 2.3 ± 0.2, 3.2 ± 0.3, and 5.3 ± 0.8 h, respectively.
Job-exposure matrices for screen and sedentary times. (A) is a job-exposure matrix (JEM) for screen time and (B) is a JEM for sedentary time. To develop JEMs, we evaluated the screen time and sedentary time of 41,718 patients without missing values and with occupational information. We calculated the adjusted means of screen time and sedentary time using an analysis of co-variance adjusted for age and sex according to 143 occupational groups (limited to groups with at least 10 people) classified based on the Japan Standard Occupational Classification and the Japan Standard Industrial Classification. All occupational groups were classified into three exposure levels (V1 [low]–V3 [high] or S1[low]–S3 [high]) based on the tertiles of the adjusted means
Furthermore, in Fig. 1B, the adjusted mean values of sedentary time are classified into three classes (S1–S3) based on tertiles and illustrated similarly. The adjusted mean values of sedentary time for the S1, S2, and S3 classes were 3.8 ± 0.3, 4.7 ± 0.4, and 6.5 ± 0.5 h, respectively.
For the case-control study, we enrolled 727,589 patients admitted between 1 April 2005 and 31 March 2021, as presented in Supplemental Fig. 1 (DATA 2). Patient characteristics are shown in Table 1. Differences in the backgrounds among groups based on the JEMs suggested the need to adjust for several confounding variables; however we addressed this through matching and a multivariate analysis. The associations between exposures (screen time and sedentary time) derived from the JEMs and the prevalence of ocular diseases are presented in Tables 2 and 3, respectively. Moreover, the ORs adjusted for drinking, smoking, and lifestyle-related comorbidities are shown in Model 2 of both tables.
Table 2 presents the association between screen time and some ocular diseases. Compared with the V1 class, the V3 class with the highest screen time exposure was more significantly associated with cataract (OR 1.05, 95% CI 1.01–1.09), POAG (1.24, 1.06–1.45), RRD (1.26, 1.06–1.49), ptosis (1.49, 1.26–1.76), pterygium (0.39, 0.27–0.57), DR (0.76, 0.66–0.87), and RVO (0.72, 0.55–0.95).
Table 3 presents the association between sedentary time and some ocular diseases. Compared with the S1 class, the S3 class with the highest sedentary time exposure was significantly associated with cataract (1.05, 1.01–1.09), RRD (1.24, 1.05–1.46), ptosis (1.68, 1.42–1.99), ON (2.41, 1.28–4.54), and pterygium (0.60, 0.42–0.84).
Table 4 summarises the differences in the prevalence of each ocular disease among the purely sedentary groups (JSOC–JSIC; F–E, F–K, F–M, I–D, I–H, I–N, and I–O) in which sedentary time was high (S3 class); however, screen time exposure was low (V1 class). These groups had a significant association with DR (1.61, 1.27–2.03) and RVO (1.74, 1.06–2.84).
The results of the sensitivity analysis are presented for the population from 2013 to 2021 in Supplemental Tables 2, 3, and 4. Our intention is to consider the differences in investigation periods between JEM development and the case-control studies. These results are nearly consistent with those from the main analysis.
Discussion
We developed JEMs for screen and sedentary times, and subsequently investigated the associations between screen and sedentary times (derived from JEMs) and ocular diseases by applying JEMs to existing occupational history databases spanning several years. Consequently, the results for screen and sedentary times were mostly similar, although interestingly, only screen time was associated with POAG and only sedentary time was associated with ON and RAO.
Differences in screen and sedentary times according to occupations
Identifying occupations with excessively long screen time or sedentary time would be of great interest from an occupational health perspective, allowing focused study of these occupations and providing remedial guidance. Our results showed that different occupations had dissimilar screen times or sedentary times, and the exposure trends for both indicators were consistent for most occupations. However, an interesting point of our results was that despite their similar exposures, there were some occupations where the trends of both exposures diverged (Supplemental Fig. 2). For example, in certain groups (JSOC–JSIC; F–E, F–K, F–M, I–D, I–H, I–N, and I–O), sedentary time was high (S3 class); however, screen time exposure was low (V1 class). Specifically, the occupations with a lower ratio of screen time than that of sedentary time were as follows: office security guards, fishermen, professional drivers, producers of agricultural products and metal materials, and printing and bookbinding suppliers.
Relationship of ocular diseases with screen and sedentary times assessed using JEMs
The study results revealed associations between several ocular diseases and screen/sedentary time derived from JEMs.
Cataract was positively associated with both screen and sedentary times, which might be explained by social factors. For instance, the causal relationship may be that office workers (with a higher screen time or sedentary time) are sensitive to changes in vision quality. Owing to work-related inconvenience, these workers might undergo cataract surgery as early as possible.
POAG had a significant positive association with screen time and no association with sedentary time. The difference between the two results may have involved the effects of blue light from the screen or accommodative demand in near work. As for screen time, prolonged computer work is reportedly a risk factor for visual field disorders and possibly associated with a risk of glaucoma3,4. Recent studies including an adult population revealed an association between screen time and axial elongation or myopia17,18. Generally, myopia is associated with glaucoma19,20. During near work, both eye positions are more adducted than in viewing at a distance, and higher straining of the optic nerve due to adduction may cause structural damage to lamina cribrosa, possibly leading to glaucoma incidence21. Additionally, temporary intraocular pressure changes after near tasks have been reported22,23. Intraocular pressure fluctuations due to frequent near tasks may affect the incidence of glaucoma24,25. Although the influence of blue light on the retina or optic nerve is controversial26, light stimulation may be harmful to retinal ganglion cells27.
RRD had a significant positive association with screen and sedentary times. The first concern about this result may be the association with exercise. Although occupations involving heavy lifting are risk factors for RRD28, there have been no definite findings on whether exercise supports or undermines RRD. During near work, contraction of the ciliary smooth muscle by accommodative demand applies an inward pull force to the choroid and sclera, leading to transient axial elongation and choroidal thinning29,30,31. This structural change may trigger posterior vitreous detachment and RRD. Additionally, screen time may be associated with myopia17,18, and myopia is generally a risk factor for RRD19,32.
Ptosis had a significant positive association with screen and sedentary time. One possibility is that diabetes may serve as a mediator of this association, given the high prevalence of diabetes among classes with the highest screen time or sedentary time (Table 1). Diabetes is a well-known cause of oculomotor nerve palsy and is positively associated with ptosis33. However, we compared both models 1 and 2 to confirm that the association trends remained consistent. Additionally, VDT work may be associated with myopia17,18. Many patients with myopia use contact lenses, which are a risk factor for ptosis34.
Pterygium was negatively associated with screen and sedentary times. The influence of sunlight could reasonably explain both results. In general, sunlight is a positively associated factor for pterygium35. Thus, indoor workers (with higher screen and sedentary times) may have less exposure to sunlight than outdoor workers, leading to a lower risk of pterygium. The same logic could be considered for cataract; however, in this study, cataract was more common among indoor workers, indicating that the result was largely due to social factors, such as inconvenience of visual function and access to surgery, as has been mentioned.
ON was positively associated with sedentary time, and DR and RVO were positively associated with purely sedentary groups. In assessing these associations regarding arteriosclerotic diseases, diabetes and dyslipidemia may serve as mediators, considering the higher prevalence of diabetes and dyslipidemia in the class with the highest sedentary time or purely sedentary groups (Table 1). It is curious that DR and RVO were less likely to develop in the class with the highest screen time, despite the higher prevalence of diabetes and dyslipidemia; however, we compared both models 1 and 2 to ensure the robustness of the association trends. To understand this phenomenon, further research is warranted on the potential mechanisms linking screen time and retinal blood flow.
Study strengths and limitations
Our study had several strengths. First, to the best of our knowledge, this is the first report to clarify the differences in screen and sedentary times according to occupations. Therefore, identifying occupations with excessive exposure would allow us to focus on these occupations and provide remedial guidance. Second, this large-scale multicenter study included large samples of various ocular diseases, by leveraging JEM and extensive occupational information datasets. Despite the small effect sizes in certain diseases, this study was positioned as exploratory research investigating various ocular diseases comprehensively; our results emphasize the need for further empirical studies on specific diseases. Third, this study adjusted for some confounding factors such as lifestyle-related comorbidities (hypertension, diabetes, dyslipidemia, and CVDs), smoking, and drinking. Finally, the quantitative evaluation of screen and sedentary times revealed a dose–response association with ocular diseases.
Our study also had certain limitations. First, non-differential misclassification of ocular diseases for both cases and controls may have introduced selection bias in either direction (toward or away from the null hypothesis). Moreover, certain ocular diseases’ codes such as cataract (H26.9), POAG (H40.9), ptosis (H02.4), ON (H46) may be subject to potential misclassification of subcategories; however, we confirmed that the specific pathological conditions (e.g., infantile cataract, secondary glaucoma, congenital ptosis and multiple sclerosis) accounted for less than a few percent of the total cases. Second, we used JEM-derived variables to assess VDT work and sedentary work exposure indirectly because of the insufficient sample size of raw variables. This might have confounded the characteristics of the occupations. Third, exposures obtained through a questionnaire survey may be subject to recall bias. Moreover, JEM-derived exposures could not evaluate the frequency of personal smartphone and computer use. However, this survey was conducted by trained investigators, which enhances its validity. Fourth, our study was hospital-based, including only inpatient data, which is subject to selection bias regarding the controls (e.g., Berkson’s bias)36. To mitigate this, we selected controls by matching cases with patients admitted to the same hospital in the same period. Moreover, our dataset includes core hospitals in regions throughout Japan; therefore, the cases and controls were likely drawn from the same large community population. Finally, we did not obtain data regarding family history, myopic status, intraocular pressure, although these are potential confounders or mediators for certain results.
In conclusion, the JEMs devised in the study provided a practical methodology for elucidating the risk of various ocular diseases based on occupational information. The JEMs showed the exposure risks for screen and sedentary times according to occupational group. The degrees of screen time and sedentary time exposures were consistent for most occupations; however, some occupations differed in their exposures to both. This study revealed that high screen and sedentary times were positively associated with cataract, RRD, and ptosis and negatively associated with pterygium. Interestingly, POAG had a positive association only with screen time. Further studies on background mechanisms are warranted.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Ong, C. N., Chia, S. E., Jeyaratnam, J. & Tan, K. C. Musculoskeletal disorders among operators of visual display terminals. Scand. J. Work Environ. Health. 21, 60–64 (1995).
Uchino, M. et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am. J. Ophthalmol. 156, 759–766. https://doi.org/10.1016/j.ajo.2013.05.040 (2013).
Nakano, T. et al. Increased incidence of Visual Field abnormalities as determined by frequency Doubling Technology Perimetry in High Computer users among Japanese workers: a retrospective cohort study. J. Epidemiol. 28, 214–219. https://doi.org/10.2188/jea.JE20170004 (2018).
Tatemichi, M. et al. Possible association between heavy computer users and glaucomatous visual field abnormalities: a cross sectional study in Japanese workers. J. Epidemiol. Community Health. 58, 1021–1027. https://doi.org/10.1136/jech.2003.018127 (2004).
Fujita, H., Sano, K., Baba, T., Tanaka, T. & Ohno-Matsui, K. Blind working time in visual display terminal users. J. Occup. Health. 61, 175–181. https://doi.org/10.1002/1348-9585.12027 (2019).
van Uffelen, J. G. et al. Occupational sitting and health risks: a systematic review. Am. J. Prev. Med. 39, 379–388. https://doi.org/10.1016/j.amepre.2010.05.024 (2010).
Sano, K. et al. Association between Alcohol Consumption Patterns and Glaucoma in Japan. J. Glaucoma. 32, 968–975. https://doi.org/10.1097/IJG.0000000000002308 (2023).
Furuya, Y. et al. Occupational physical activity differentially affects the risk for developing later-onset Crohn’s disease and ulcerative colitis among middle-aged and older populations. Scand. J. Gastroenterol. 57, 206–213. https://doi.org/10.1080/00365521.2021.1999495 (2022).
Fukai, K. et al. Alcohol use patterns and risk of incident cataract surgery: a large scale case-control study in Japan. Sci. Rep. 12, 20142. https://doi.org/10.1038/s41598-022-24465-2 (2022).
Zaitsu, M., Takeuchi, T., Kobayashi, Y. & Kawachi, I. Light to moderate amount of lifetime alcohol consumption and risk of cancer in Japan. Cancer. 126, 1031–1040. https://doi.org/10.1002/cncr.32590 (2020).
Hwang, W. J. & Hong, O. Work-related cardiovascular disease risk factors using a socioecological approach: implications for practice and research. Eur. J. Cardiovasc. Nurs. 11, 114–126. https://doi.org/10.1177/1474515111430890 (2012).
El-Zaemey, S. et al. Case-control study to assess the association between colorectal cancer and selected occupational agents using INTEROCC job exposure matrix. Occup. Environ. Med. 75, 290–295. https://doi.org/10.1136/oemed-2017-104795 (2018).
Eheman, C. R., Tolbert, P. E., Coates, R. J., Devine, O. & Eley, J. W. Case-control assessment of the association between non-hodgkin’s lymphoma and occupational radiation with doses assessed using a job exposure matrix. Am. J. Ind. Med. 38, 19–27. https://doi.org/10.1002/1097-0274(200007)38:1<19::aid-ajim3>3.0.co;2-l (2000)."Reference [13] contains a local link (https://doi.org/10.1002/1097-0274(200007)38:1<19::aid-ajim3>3.0.co;2-l); however, this must be replaced with a working internet link. Please provide an alternative URL link. Otherwise, kindly advise if the local link can be deleted."I have confirmed that the currently listed DOI is valid and accessible. However, feel free to delete the link if necessary.
Evanoff, B. A. et al. The CONSTANCES job exposure matrix based on self-reported exposure to physical risk factors: development and evaluation. Occup. Environ. Med. 76, 398–406. https://doi.org/10.1136/oemed-2018-105287 (2019).
von Elm, E. et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int. J. Surg. 12, 1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013 (2014).
Fukai, K., Kojimahara, N., Hoshi, K., Toyota, A. & Tatemichi, M. Combined effects of occupational exposure to hazardous operations and lifestyle-related factors on cancer incidence. Cancer Sci. 111, 4581–4593. https://doi.org/10.1111/cas.14663 (2020).
Honda, T. et al. Association between Information and Communication Technology use and ocular axial length elongation among middle-aged male workers. Sci. Rep. 9, 17489. https://doi.org/10.1038/s41598-019-53423-8 (2019).
Foreman, J. et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit. Health. 3, e806–e818. https://doi.org/10.1016/S2589-7500(21)00135-7 (2021).
Haarman, A. E. G. et al. The complications of myopia: a review and Meta-analysis. Invest. Ophthalmol. Vis. Sci. 61, 49. https://doi.org/10.1167/iovs.61.4.49 (2020).
Shen, L. et al. The Association of Refractive Error with Glaucoma in a Multiethnic Population. Ophthalmology. 123, 92–101. https://doi.org/10.1016/j.ophtha.2015.07.002 (2016).
Chuangsuwanich, T. et al. Adduction induces large optic nerve head deformations in subjects with normal-tension glaucoma. Br. J. Ophthalmol.https://doi.org/10.1136/bjo-2022-322461 (2023).
Yan, L., Huibin, L. & Xuemin, L. Accommodation-induced intraocular pressure changes in progressing myopes and emmetropes. Eye (Lond). 28, 1334–1340. https://doi.org/10.1038/eye.2014.208 (2014).
Read, S. A. et al. Changes in intraocular pressure and ocular pulse amplitude with accommodation. Br. J. Ophthalmol. 94, 332–335. https://doi.org/10.1136/bjo.2009.166355 (2010).
Caprioli, J. & Coleman, A. L. Intraocular pressure fluctuation a risk factor for visual field progression at low intraocular pressures in the advanced glaucoma intervention study. Ophthalmology. 115 (e1123), 1123–1129. https://doi.org/10.1016/j.ophtha.2007.10.031 (2008).
Terauchi, R. et al. Seasonal fluctuation in intraocular pressure and its associated factors in primary open-angle glaucoma. Eye (Lond). 35, 3325–3332. https://doi.org/10.1038/s41433-021-01403-6 (2021).
O’Hagan, J. B., Khazova, M. & Price, L. L. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye (Lond). 30, 230–233. https://doi.org/10.1038/eye.2015.261 (2016).
Osborne, N. N., Lascaratos, G., Bron, A. J., Chidlow, G. & Wood, J. P. A hypothesis to suggest that light is a risk factor in glaucoma and the mitochondrial optic neuropathies. Br. J. Ophthalmol. 90, 237–241. https://doi.org/10.1136/bjo.2005.082230 (2006).
Mattioli, S. et al. Physical exertion (lifting) and retinal detachment among people with myopia. Epidemiology. 19, 868–871. https://doi.org/10.1097/EDE.0b013e318187a7da (2008).
Woodman, E. C. et al. Axial elongation following prolonged near work in myopes and emmetropes. Br. J. Ophthalmol. 95, 652–656. https://doi.org/10.1136/bjo.2010.180323 (2011).
Woodman-Pieterse, E. C., Read, S. A., Collins, M. J. & Alonso-Caneiro, D. Regional changes in Choroidal Thickness Associated with accommodation. Invest. Ophthalmol. Vis. Sci. 56, 6414–6422. https://doi.org/10.1167/iovs.15-17102 (2015).
Croft, M. A. et al. Accommodative movements of the vitreous membrane, choroid, and sclera in young and presbyopic human and nonhuman primate eyes. Invest. Ophthalmol. Vis. Sci. 54, 5049–5058. https://doi.org/10.1167/iovs.12-10847 (2013).
van Leeuwen, R. et al. Association of Rhegmatogenous Retinal detachment incidence with myopia prevalence in the Netherlands. JAMA Ophthalmol. 139, 85–92. https://doi.org/10.1001/jamaophthalmol.2020.5114 (2021).
Bacharach, J., Lee, W. W., Harrison, A. R. & Freddo, T. F. A review of acquired blepharoptosis: prevalence, diagnosis, and current treatment options. Eye (Lond). 35, 2468–2481. https://doi.org/10.1038/s41433-021-01547-5 (2021).
Tossounis, C. M., Saleh, G. M. & McLean, C. J. The long and winding road: contact lens-induced ptosis. Ophthalmic Plast. Reconstr. Surg. 23, 324–325. https://doi.org/10.1097/IOP.0b013e318073c648 (2007).
Threlfall, T. J. & English, D. R. Sun exposure and pterygium of the eye: a dose-response curve. Am. J. Ophthalmol. 128, 280–287. https://doi.org/10.1016/s0002-9394(99)00161-0 (1999).
Berkson, J. Limitations of the application of fourfold table analysis to hospital data. Int. J. Epidemiol. 43, 511–515. https://doi.org/10.1093/ije/dyu022 (2014).
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by the Ministry of Health, Labour and Welfare, Japan (Grant number: 240801-01) and JSPS KAKENHI Grant Number 24K02713. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or /and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
KS, KF, RT, and MT designed the study. KS, KF, RT, YF, SN, TN, and MT analysed and interpreted the data. KS, KF, RT, and MT wrote the manuscript. KF, NK, KH, TN, AT, and MT supervised the study and provided critical comments. NK, KH, AT, and MT received funding and collected the data. All authors have reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sano, K., Fukai, K., Terauchi, R. et al. Association between ocular diseases and screen time and sedentary time derived from job-exposure matrices. Sci Rep 14, 27042 (2024). https://doi.org/10.1038/s41598-024-74854-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74854-y