Abstract
This prospective cohort study included 80 healthy candidates for Implantable Collamer Lens (ICL) implantation who underwent biometric assessments with Scheimpflug imaging (the Pentacam-AXL) and swept-source optical coherence tomography (SS-OCT; the IOLMaster-700), both before and 3 months after surgery. The main outcome measures were mean keratometry, anterior chamber depth, axial length, and various intraocular lens (IOL) calculation formulas (Haigis, SRK/T, Hoffer Q, Holladay 1, Barrett Universal 2, and Olsen). The interchangeability of the devices was assessed by generating 95% limits of agreement (95% LoA) and associated Bland-Altman plots. The average age of the participants was 31.5 ± 5.4 years (22–43), with 58 (72.5%) being female. Among the cases analyzed, 11 (13.4%) had incorrect anterior lens surface segmentation using the IOLMaster-700, and 1 case (1.2%) had inappropriate segmentation using the Pentacam-AXL. Postoperative IOL power calculation resulted in readings that were, on average, 0.15 to 0.30 D higher compared to preoperative measurements. The 95% LoAs could differ by up to 0.85 D higher after surgery, indicating weak agreement between pre- and postoperative measurements. There was poor agreement between the IOLMaster-700 and Pentacam-AXL in IOL power calculation for eyes with post-ICL implantation, with a difference of more than 1 D in the 95% LoAs. In conclusion, Scheimpflug imaging was found to be less susceptible than the SS-OCT technique to segmentation errors of the anterior lens surface after ICL implantation. Neither device showed interchangeable results for pre- versus postoperative IOL power calculation. The determination of IOL power by the IOLMaster-700 versus Pentacam-AXL was not interchangeable in eyes with ICL implantation.
Similar content being viewed by others
Introduction
Refractive error is a common cause of vision loss worldwide. According to studies conducted between 1991 and 2010, cataracts were found to be the primary cause of blindness (defined as vision less than 3/60), accounting for 33% of cases, followed by uncorrected refractive errors at 21%. However, when it came to moderate to severe vision loss (ranging from 3/60 to 20/60 in the better eye), refractive errors were identified as the leading cause, responsible for 51% of vision impairment cases1. It is estimated that 1,406 million people worldwide suffer from myopia (22.9%), with 163 million having high myopia defined as myopia greater than − 5 Diopters (D), constituting 2.7% of the world’s population. The prevalence of myopia appears to be increasing and is expected to reach 50% of the world’s population by 20502.
There are various approaches for correcting refractive errors, with refractive surgeries having a positive impact on people’s quality of life and reducing their dependence on glasses. Refractive surgeries can generally be categorized into two groups. The first category involves keratorefractive surgeries, which alter the curvature (keratometry) and shape of the cornea. The second category includes surgeries where an intraocular lens (IOL) is inserted3. Phakic Intraocular lenses (pIOLs) are used to correct moderate to high myopia and are a suitable option when keratorefractive surgery is contraindicated. These lenses are divided into two groups: anterior chamber IOLs and posterior chamber IOLs, with the latter, such as Implantable Collamer Lens (ICL), Implantable Phakic Contact Lens, and Eyecrylphakic Lens, being among the most commonly used types4.
Implantable Collamer Lenses, which fall under the category of STAAR surgical lenses (Nidua, Switzerland), are available in different types. One of the newest models, the EvoVisian ICL, has a center aperture of 360 microns. This allows for the movement of aqueous humor and eliminates the need for peripheral iridectomy. These lenses can correct a wide range of myopia, from − 0.5 diopters (D) to -18.0 D, as well as astigmatism, from 0.5 D to 6.0 D, thus their usage is increasing4.
As a result, we anticipate encountering many patients with cataracts in eyes with implanted ICLs in the coming years. While the current methods for determining IOL power are generally precise, they are primarily optimized for eyes that have not undergone any prior surgeries. In theory, the implantation of ICLs can cause changes in ocular biometric measurements, which may potentially affect IOL power calculation. To investigate these changes and their impact on IOL power calculation using various methods, this study was conducted to evaluate preoperative and postoperative ocular biometric parameters in patients undergoing ICL implantation. One of the main aims of the study was to determine the best technique (Scheimpflug vs. swept-source optical coherence tomography [SS-OCT]) and formula for determining IOL power in eyes with ICL implants. Since these patients did not undergo cataract surgery and we do not have post-cataract surgery refraction data, we used the preoperative readings as the reference measurement for this purpose. The second aim of the study was to assess the interchangeability of Scheimpflug and SS-OCT methods in determining IOL power in ICL implanted eyes. This information can guide clinicians who have experience with one instrument and are now new users of the second one.
Materials and methods
Participants
This prospective cohort study involved 82 myopic patients who underwent ICL implantation. The study included patients aged 21–45 years who met the standard indications for ICL implantation, had an anterior chamber depth of more than 3.0 mm, and had a preoperative endothelial cell count of at least 2000 per square millimeter. The exclusion criteria consisted of patients with dry eye, any ocular surface pathology, cataract, glaucoma, poor fixation, and a history of previous ocular surgery or trauma. All patients were informed about the study protocol and provided informed consent upon enrollment. The study was conducted in accordance with the principles of the Helsinki Declaration and received approval from the ethics committee at Shiraz University of Medical Sciences (approval number: IR.SUMS.MED.REC.1400.309).
Surgical technique
All surgical procedures were performed by a single qualified surgeon (RS). After administering either general or local anesthesia, a clear corneal incision measuring 3.2 mm in size was made along the temporal meridian. Afterwards, a viscoelastic agent was used to fill the anterior chamber. The ICL was then implanted into the anterior chamber through the incision using the manufacturer’s injector cartridge. The specific ICL used for the procedure was the EvoVisian model from STAAR Surgical, Switzerland. It was carefully positioned in the sulcus with precise alignment to the axis.
After the ICL placement, any remaining viscoelastic agent was irrigated out of the anterior chamber, and a miotic agent was injected. To prevent postoperative leakage, the corneal incision was hydrated. Postoperatively, betamethasone and levofloxacin eye drops were administered six times a day for one week, gradually tapering over the next three weeks.
Measurements
For each patient, a comprehensive ocular examination and imaging was performed at baseline (prior to the surgery) and three months after ICL implantation. The evaluation process included measuring visual acuity, performing refraction, and conducting a slit-lamp biomicroscopy. Biometric measurements were then randomly taken using the Scheimpflug technique (the Pentacam-AXL; software 1.244r22, Oculus, Wetzlar, Germany) and SS-OCT (the IOLMaster 700; version 1.50, Carl Zeiss Meditec AG). Two expert examiners, who were unaware of the results from the other device, carried out the measurements. Next, intraocular pressure was measured using a Goldmann applanation tonometer, and a dilated fundus examination was conducted. All examinations took place in the morning (between 9 and 11 AM) in the same dimly lit room to minimize the influence of diurnal variation and pupil size on biometric measurements5. For each device, the first image meeting the quality requirements, as recommended by the manufacturer, was selected for analysis.
Statistical analysis
With an alpha level of 0.05 and 90% power, we determined that 68 cases were required to detect a difference of 0.2 D (standard deviation [SD], 0.5) in IOL power measurements on different occasions or using different devices. To account for potential nonadherence and improve the reliability of Bland-Altman plots, we included an additional 20% of patients, resulting in a total sample size of 82.
We conducted statistical analyses using IBM SPSS Statistics (version 26; SPSS Inc., Chicago, Illinois, USA) and MedCalc (version 19.7.2; MedCalc Software, Mariakerke, Belgium). The paired t-test or Wilcoxon signed-rank test, as appropriate, was used to compare measurements obtained before and after surgery. For each variable, we calculated the 95% limits of agreement (LoA) and generated Bland-Altman plots to assess the interchangeability of pre- and post-operative measurements.
To eliminate potential bias caused by the correlation of biometric data from fellow eyes, we performed the statistical analysis exclusively on the results of the right eyes. A p-value less than 0.05 was considered statistically significant.
Results
Finally, this study analyzed data from 80 cases that underwent ICL implantation. The participants had a mean age of 31.5 ± 5.4 years (range, 22 to 43), and 58 (72.5%) were female. The spherical equivalent (SE) refraction was 8.96 ± 3.53 D (-22.25 to -4.40), and corneal astigmatism was 1.95 ± 0.99 D (0.3 to 5.10). The central corneal thickness (CCT) and sulcus length were 504 ± 43 μm (410–594) and 11.86 ± 0.35 mm (11.04 to 12.63), respectively. Mild keratoconus was present in thirteen patients (15.9%).
Eleven cases (13.4%) had incorrect segmentation of the anterior lens surface with IOLMaster 700 (Fig. 1), and one case (1.2%) had inappropriate segmentation with Pentacam AXL. Due to the significant bias caused by these cases, they were excluded from further t-test and agreement analyses.
In a logistic regression model, the only parameter that showed an independent association with the development of IOLMaster segmentation error of the anterior lens surface in ICL-implanted eyes was the ICL size (Odds ratio, 0.276 for each size increase [95% confidence interval, 0.098 to 0.774]; P = 0.014). No significant association was found between age, sex, SE refraction, mean keratometry, astigmatic keratometry, axial length (AL), anterior chamber depth (ACD), CCT, sulcus-sulcus distance, lens thickness, or having mild keratoconus, and the IOLMaster segmentation error.
Out of the 80 implanted ICLs, 9 (11.3%) had a size of 12.1 mm, 38 (47.5%) had a size of 12.6 mm, and 33 (41.3%) had a size of 13.2 mm. The frequency of IOLMaster segmentation error for the anterior lens surface was 33.3%, 18.4%, and 3.0% for each respective size (P = 0.033, Chi-squared test).
Pre- vs. post-operative comparisons
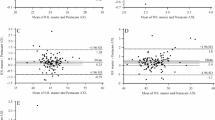
Table 1; Figs. 2 and 3 illustrate the effect of ICL implantation on the agreement of biometric parameters and formulas obtained by each device. Figure 3 shows that postoperative IOL power calculation using any formula and either device can yield average readings that are 0.15 to 0.30 D higher than preoperative measurements. According to the reported 95% LoAs, individual measurements may differ by up to 0.85 to 1.0 D higher, indicating a weak agreement between pre- and postoperative measurements.
Inter-device agreement analysis
The analysis of postoperative agreement between the IOLMaster 700 and Pentacam AXL is shown in Table 2. The IOL power calculation in the eyes with post-ICL implantation showed poor agreement between the IOLMaster 700 and Pentacam AXL when using the 4 studied formulas.
Discussion
Limited studies, all with a retrospective design, have been conducted to assess the accuracy of IOL calculation after the implantation of an ICL6,7,8,9. In the largest study, Vargas et al.6 analyzed 87 eyes and reported that 73% of the patients were within ± 1 D of the target refraction. Other smaller studies reported that 58–69% of the patients were within ± 0.5 D of the target refraction7,8. These results are significantly inferior compared to the accuracy reported in studies on patients with no history of eye surgery, where the range is usually reported as ± 0.25 D10. Since conducting prospective trials to directly assess IOL power determination accuracy in ICL-implanted eyes is challenging due to the rarity of cataract surgery in these eyes, we adopted a surrogate method. This method involved comparing the measured IOL powers in ICL-implanted eyes with the reference preoperative measurements of the same patient. As newer methods tend to have low inaccuracies in eyes without prior surgery, closer values to the reference measurements indicate better accuracy of the method for ICL-implanted eyes.
Both the Pentacam-AXL and IOLMaster-700 are widely used in clinical practice. Previous studies have confirmed good repeatability and reproducibility for biometric variables measured by both devices11. In addition, a few studies have assessed the interchangeability of measurements between these devices in virgin eyes11,12,13,14,15. However, our study is the first of its kind to compare the data obtained from the Pentacam-AXL and IOLMaster-700 before and after ICL EvoVisian implantation.
Segmentation error
According to the printout image of the IOLMaster device, 11 patients (13.4%) had incorrect ACD readings in the postoperative data. The IOL Master measured the distance from the cornea to the anterior surface of the ICL as ACD, resulting in an error of more than 0.5 mm and calculating a shallower ACD than the actual value (Fig. 4). Ouchi et al. noted that 75% of patients experienced this segmentation error problem16. In contrast, when we used the Pentacam AXL, only 1 patient (1.2%) showed an ACD difference of more than 0.5 mm between preoperative and postoperative readings, indicating a segmentation error. Pentacam AXL uses Scheimpflug images to measure ACD and captures more than 20 images to precisely identify the anterior surface of the crystalline lens. As a result, the chances of encountering this segmentation error are significantly reduced compared to the IOLMaster 700, although it is not entirely eliminated.
In the logistic regression model, we identified that a smaller ICL size was the only parameter that independently associated with the observed segmentation error in the IOL Master. The ICL size is primarily determined by the sulcus-to-sulcus distance and the depth of the anterior chamber17. Consequently, smaller eyes with implanted ICLs may be more susceptible to segmentation errors by the IOLMaster 700. In addition, the possibility of a low vault position is higher with smaller ICLs, which probably makes accurate segmentation more difficult for the device.
Biometric parameters
Comparing pre- vs. postoperative measurements
Axial length and corneal keratometry are the two main determining factors in IOL power calculation. Studies have indicated that a change of 0.1 mm in AL can result in a 0.27 diopter change in the measured IOL power18. In our study, the mean differences between the preoperative and postoperative AL was − 0.03 ± 0.14 mm in the IOLMaster 700 and − 0.05 ± 0.06 mm in the Pentacam AXL, which are not clinically relevant. However, the 95% LoAs were − 0.31 mm to 0.25 mm for the IOLMaster 700 and − 0.18 mm to 0.07 mm for the Pentacam AXL, implying that the Pentacam AXL was less affected by ICL implantation. However, both limits of agreement can lead to a difference of > 0.5 D in IOL power calculation, which is beyond clinical acceptance.
Several previous studies have reported no significant change in the mean AL readings after the implantation of an ICL16,19,20. Ouchi et al. demonstrated a mere 0.01 mm change in AL after ICL implantation, which was not expected to impact IOL power calculation16. Chen et al. also reported an insignificant change in AL after ICL implantation using the IOLMaster 700 device20. However, compared to changes in the mean AL, the 95% LoA is a more realistic measure of the interchangeability of pre- vs. postoperative AL measurements, which was not reported in the mentioned studies.
On the other hand, some studies such as Yasa et al. found an increase in the mean AL after Eyecrylphakic IOL implantation, using a Nidek AL scan21. They attributed this increase to the higher refractive index of the phakic IOL compared to the aqueous and vitreous humor. This finding was in line with our results, which showed a slight but statistically significant increase in the mean AL measurements after ICL implantation.
Keratometry is the second crucial factor in determining IOL power18. Each 0.5 D change in mean keratometry approximately corresponds to an equal change in IOL power. In our study, the average difference between preoperative and postoperative mean keratometry was − 0.12 ± 0.56 D in the IOLMaster 700 and − 0.09 ± 0.30 D for the Pentacam AXL. This difference was not statistically significant in either device. Previous studies have also reported similar results consistent with our findings16,19,21. In ICL implantation, the corneal incision is made at the periphery of the cornea, causing minimal impact on corneal curvature. Therefore, a significant change in mean keratometry is not expected. However, the 95% LoAs between preoperative and postoperative mean keratometry for both devices exceeded 0.5 D, especially in the case of the IOLMaster (which was larger than 1 D). Consequently, we do not recommend interchangeable use of mean keratometry from pre and postoperative measurements by either device.
Anterior chamber depth is the third important biometric parameter in IOL power calculation, and IOL power can vary by 0.1 D for a 0.2 mm change in ACD measurement22. After excluding eyes with segmentation errors, our study revealed a mean difference in pre- vs. post-operative ACD of 0.03 ± 0.11 for the IOLMaster 700 and 0.09 ± 0.10 for the Pentacam AXL. Other studies also reported a small decrease in mean ACD in postoperative data16,20. The 95% LoA for the IOLMaster 700 were − 0.20 to 0.25, and for the Pentacam AXL were − 0.10 to 0.28. This level of agreement corresponds to a change of less than 0.25 D in IOL power, and thus the pre- vs. postoperative ACD measurements could be considered interchangeable for determining IOL power. However, especially for the IOLMaster 700, the biometric image should be checked to ensure proper measurement of ACD up to the anterior surface of the crystalline lens (Fig. 4).
Comparing IOLMaster 700 with Pentacam AXL
According to postoperative measurements, the Pentacam showed lower mean keratometry values (mean difference, 0.13 D) and a shorter AL (0.04 mm) compared to the IOLMaster 700. Slightly lower values were also observed for ACD (0.03 mm), which were statistically significant. The two devices were not interchangeable for calculating IOL power when measuring mean keratometry (95% LoA, -0.47 to 0.74 D), but they were interchangeable in ACD measurement (-0.09 to 0.16 mm). The interchangeability of the devices in AL measurement depends on our threshold for acceptable error in IOL power determination. The 95% LoA for AL was 0.11 to 0.18 mm, which can result in a difference of up to 0.49 D in IOL power. If we set the threshold at 0.5 D, the two devices will be interchangeable. However, if we set the threshold at 0.25 D, as is increasingly demanded, then the two devices could not be used interchangeably.
IOL power calculation
Comparing pre- vs. postoperative measurements
The mean difference in the IOL calculation formulas between pre- and post-operative measurements was less than 0.2 D for the IOLMaster 700 after excluding segmentation errors. However, for Pentacam AXL, this difference was higher, ranging from approximately 0.25 to 0.40 D. In all cases, the postoperative calculated IOL power was lower than the preoperative measurements. Other studies also showed a similar decrease of 0.25 D to 0.5 D in the calculated IOL power for all formulas16,18. We hypothesize that the observed mean postoperative difference is due to a slight increase in the measured AL and a decrease in ACD after ICL implantation.
In contrast to our study, Ouchi et al. found that if the segmentation error in the IOLMaster 700 is corrected, then the IOL power calculation in pre- and post-ICL implantation can be used interchangeably for Haigis, SRK-T, and Barrett formulas16. Chen et al. also found that IOL power calculations do not change after an ICL implant when using the Barrett formula20.
According to the 95% LoAs in the present study, all the formulas studied with both devices tend to have an error of more than 0.5 D after ICL implantation. As a result, the pre- and post-operative measurements cannot be considered interchangeable. Notably, the Olsen formula with Pentacam AXL showed the poorest agreement.
Comparing IOLMaster 700 with Pentacam AXL
After ICL implantation, the mean IOL power measured by the Pentacam AXL was approximately 0.3 to 0.45 D higher than with the IOLMaster 700. This difference can be attributed to variations in AL and mean keratometry measurements (Table 2), as the Pentacam AXL measures a shorter AL and lower mean keratometry values compared to the IOLMaster 700. Reyes et al. compared the IOL power formulas between the IOLMaster 700 and Pentacam AXL in virgin eyes and found that the Pentacam AXL tends to yield higher IOL power measurements than the IOLMaster using all formulas, but they concluded that this difference is negligible23. In our study, the 95% LoAs of all studied formulas were greater than 1 D, indicating that the two devices could not be used interchangeably using those formulas after ICL implantation (Table 2).
Powers and limitations
This study is the first of its kind to assess the impact of ICL implantation on the agreement of IOL power calculation using two advanced optical biometric devices and the most commonly used formulas (Haigis, SRK/T, Hoffer Q, Holladay 1, Barrett Universal 2, and Olsen). We could not able to assess all widely used methods, and the role of other new generation formulas such as Kane, Hill RBF, Panacea, Pearl-DGS, and Naeser in this context could be the subject of future studies.
Since ICL implantation has been performed for several years and some patients may develop cataracts, it is crucial to determine how closely or differently the measured IOL power would be after ICL implantation compared to the measured power in virgin eyes, which serves as the gold standard. This method could be cautiously used as a surrogate for appropriate prospective accuracy studies, which are currently hard to perform due to the rarity of cases. Yet, it should be noted that this method cannot directly assess the “accuracy” of IOL power formulas, and the terms agreement and interchangeability are more fitting in this context.
Our sample size was sufficient for evaluating the primary outcome of the study and also acceptable for producing reliable Bland-Altman plots. However, it is important to note that the results of this study are limited by the characteristics of the included patients (young, myopic Iranian patients with a White race and Middle-Eastern ethnicity) and cannot be generalized to individuals with different ethnic, demographic, or clinical profiles.
Conclusions
This study found that optical biometry after ICL implantation can lead to a segmentation error in determining the anterior surface of the crystalline lens in a significant number of eyes, especially when using the IOLMaster 700 device. Therefore, it is crucial to carefully review the printed image to ensure accurate segmentation for ACD measurements and to avoid unexpected IOL power calculations. Moreover, the implanted ICL resulted in an average increase of 0.25 to 0.40 D in IOL power calculations compared to preoperative values, likely due to interference with AL and ACD measurements. None of the tested devices or formulas were found to be interchangeable for determining IOL power before and after ICL implantation. Additionally, the Pentacam AXL and IOLMaster 700 were not interchangeable for measuring IOL power after ICL implantation. This information is valuable for making clinical decisions in cataract patients who have previously undergone ICL implantation.
Data availability
The data that support the findings of this study are not openly available to avoid compromising individual privacy. However, anonymized data are available from the corresponding author upon reasonable request.
References
Bourne, R. R. et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health 1, e339-349 (2013).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042 (2016).
Tsang, J. A., Al-Kire, R. L. & Ratchford, J. L. Prosociality and religion. Curr. Opin. Psychol. 40, 67–72 (2021).
Martínez-Plaza, E. et al. Phakic intraocular lenses: recent advances and innovations. Arch. de la. Sociedad Española De Oftalmología (English Edition) 95, 178–187 (2020).
Momeni-Moghaddam, H. et al. The Effect of Cycloplegia on the ocular biometric and anterior segment parameters: a cross-sectional study. Ophthalmol. Ther. 8, 387–395 (2019).
Vargas, V. et al. Safety and visual outcomes following posterior chamber phakic intraocular lens bilensectomy. Eye Vis. (Lond) 7, 34 (2020).
Del Risco, N. E. et al. Visual outcomes of cataract surgery in patients with previous history of Implantable Collamer Lens. J. Clin. Med. 13, 4292 (2024).
Meier, P. G., Majo, F., Othenin-Girard, P., Bergin, C. & Guber, I. Refractive outcomes and complications after combined copolymer phakic intraocular lens explantation and phacoemulsification with intraocular lens implantation. J. Cataract Refract. Surg. 43, 748–753 (2017).
Kamiya, K., Shimizu, K., Igarashi, A., Aizawa, D. & Ikeda, T. Clinical outcomes and patient satisfaction after Visian Implantable Collamer Lens removal and phacoemulsification with intraocular lens implantation in eyes with induced cataract. Eye (Lond) 24, 304–309 (2010).
Ma, Y. et al. Network Meta-analysis of intraocular lens power calculation formula accuracy in 1016 eyes with long axial length. Am. J. Ophthalmol. 257, 178–186 (2024).
Sel, S., Stange, J., Kaiser, D. & Kiraly, L. Repeatability and agreement of Scheimpflug-based and swept-source optical biometry measurements. Cont. Lens Anterior Eye 40, 318–322 (2017).
Salouti, R. et al. Effect of photorefractive keratectomy on agreement of anterior segment variables obtained by a swept-source biometer vs a Scheimpflug-based tomographer. J. Cataract Refract. Surg. 46, 1229–1235 (2020).
Sayed, K. M. & Alsamman, A. H. Interchangeability between Pentacam and IOLMaster in phakic intraocular lens calculation. Eur. J. Ophthalmol. 25, 202–207 (2015).
Shajari, M. et al. Comparison of axial length, corneal curvature, and anterior chamber depth measurements of 2 recently introduced devices to a known biometer. Am. J. Ophthalmol. 178, 58–64 (2017).
Tañá-Rivero, P., Aguilar-Córcoles, S., Tello-Elordi, C., Pastor-Pascual, F. & Montés-Micó, R. Agreement between 2 swept-source OCT biometers and a Scheimpflug partial coherence interferometer. J. Cataract Refract. Surg. 47, 488–495 (2021).
Ouchi, M. Evaluation of impact of posterior phakic IOL implantation on biometry and effectiveness of concomitant use of anterior segment OCT on IOL power calculation for cataract surgery. J. Cataract Refract. Surg. 48, 657–662 (2022).
Xue, Y., Guo, Y. & Zhao, R. Preoperative anatomy parameters in implantable collamer lenses. Available at Research Square, https://doi.org/10.21203/rs.3.rs-968382/v1 (2021).
Khoramnia, R., Auffarth, G., Łabuz, G., Pettit, G. & Suryakumar, R. Refractive outcomes after cataract surgery. Diagnostics (Basel) 12, 243–257. https://doi.org/10.3390/diagnostics12020243 (2022).
Amro, M., Chanbour, W., Arej, N. & Jarade, E. Third- and fourth-generation formulas for intraocular lens power calculation before and after phakic intraocular lens insertion in high myopia. J. Cataract Refract. Surg. 44, 1321–1325 (2018).
Chen, X. et al. Effect of Implantable Collamer Lens on anterior segment measurement and intraocular lens power calculation based on IOLMaster 700 and Sirius. J. Ophthalmol. 2021, 8988479 (2021).
Yaşa, D., Köse, B., Sucu, M. E. & Ağca, A. Intraocular lens power calculation in a posterior chamber phakic intraocular lens implanted eye. Int. Ophthalmol. 40, 2017–2022 (2020).
Salouti, R. et al. Agreement of corneal diameter measurements obtained by a swept-source biometer and a Scheimpflug-based topographer. Cornea 36, 1373–1376 (2017).
Reyes Reyes, H. A., Zuñiga, K., Ventura, F., Carranza, M. & Espino Icazbalceta, R. Comparative study of the ocular biometric measurements of the anterior segment and the intraocularlens power calculation based on a scheimpflug device and a reference optical biometer in a sample of the Mexican population in an ophthalmological reference center. Investig. Ophthalmol. Vis. Sci. 61, 1861–1861 (2020).
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study concept and design (RS, MHN, MN); data collection (KS, MG, MN); analysis and interpretation of data (MHN); writing the manuscript (RS, MHN, MN, KS, MG); critical revision of the manuscript (RS, MHN); Final approval (All authors); Agreement to be accountable for all aspects of the work (All authors).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Salouti, R., Nazarpour-Servak, M., Salouti, K. et al. Comparison of ocular biometric measurements and intraocular lens power calculation using different methods in eyes with implantable collamer lenses. Sci Rep 14, 24006 (2024). https://doi.org/10.1038/s41598-024-74880-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74880-w
Keywords
This article is cited by
-
Factors affecting the refractive error after cataract surgery
International Ophthalmology (2025)