Abstract
Sarcopenia is a severe complication affecting patients receiving hemodialysis (HD) treatment over an extended period of time. This cross-sectional study assessed knowledge, attitude, and practice (KAP) towards sarcopenia among maintenance HD patients in Northeastern China between 13 December 2023 and 13 January 2024. A total of 752 questionnaires were collected. Multivariate logistic regression showed that completed high school or vocational secondary school, college or bachelor’s degree, and maintenance HD lasting ≥ 11 years were independently associated with proactive practice. The Structural equation modeling (SEM) showed that knowledge directly affected attitude and practice. Moreover, attitude directly affects practice. Maintenance HD patients showed inadequate knowledge, positive attitude, and proactive practice towards sarcopenia. Healthcare providers should focus on educational campaigns to increase patient awareness of sarcopenia, its risk factors, and preventive measures.
Similar content being viewed by others
Background
Sarcopenia poses a significant threat to patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD), particularly those undergoing long-term maintenance hemodialysis (HD)1. In the context of HD, the prevalence of sarcopenia varies considerably, ranging from 4–64%2. Given the substantial impact of sarcopenia on health, including its association with adverse outcomes such as falls, fractures, frailty, physical disability, and hospitalization, addressing this condition is of utmost importance3. Accordingly, ensuring optimal fluid volume and implementing preventive measures to mitigate sarcopenia have pivotal roles in managing HD patients4. Sarcopenia has the potential to compromise the standard quality of life, which underscores the urgency of developing effective interventions designed to either forestall or delay its onset5.
The knowledge, attitude, and practices (KAP) survey functions as a diagnostic research tool, illuminating comprehension, beliefs, and actions of a particular group on a specific subject, particularly within the realm of health literacy, where it is based on the premise that knowledge positively influences attitudes, which in turn mold behaviors6,7,8.
Recent studies have underscored the importance of educational interventions and public health measures in improving health outcomes. For instance, the impact of maternal health education on pediatric oral health in Banda Aceh reveals how targeted educational programs can significantly enhance health behaviors9. Additionally, the COVID-19 public health and social measures in Southeast Nigeria demonstrate the critical role of strategic public health management in mitigating health crises and promoting sustainability10. Furthermore, economic analyses, such as the study on healthcare financing reforms in Nigeria, demonstrate the broader implications of health interventions on macroeconomic outcomes11.
Considering the significant impact of sarcopenia on the health and life quality in maintenance HD patients, gaining insight into patients’ knowledge levels, attitudes, and behavioral practices is instrumental for healthcare professionals to meet patients’ needs more efficiently and provide more effective health education and prevention strategies. Furthermore, the research findings can be used to formulate relevant policies and guidelines to enhance the management and prevention of muscle mass loss. Currently, there is a dearth of research in this particular domain. Most existing studies have focused on healthcare professionals, revealing gaps in knowledge and practice12,13,14. Additionally, a study that included the general population in Malaysia revealed a limited understanding of sarcopenia15. To date, there have been no KAP studies specifically targeting sarcopenia in maintenance HD patients.
This study aimed to investigate the KAP towards sarcopenia among maintenance HD patients. By identifying the gaps in patient awareness, attitude trends, and actual behaviors, it is possible to conduct targeted health education, clinical management, and lifestyle interventions to improve the prevention and treatment of sarcopenia, enhance patient quality of life, and reduce the incidence of complications.
Methods
Study design and participants
This cross-sectional study included patients undergoing maintenance HD in hospitals in Northeastern China between 13 December 2023 and 13 January 2024. Inclusion criteria encompassed CKD patients receiving regular HD who were willing to participate. Specifically, participants had to be diagnosed with CKD stage 5 or ESRD and be currently receiving regular HD treatment. They were required to undergo HD at least three times per week for a minimum of three months. Eligible participants were between 18 and 80 years old, possessed sufficient cognitive capacity to understand the study content and provide informed consent, and had no severe cardiovascular diseases, diabetes, or other serious health conditions that could interfere with the study results. Exclusion criteria encompassed questionnaires completed in < 114 s or > 1800 s, incomplete questionnaires, and patients unable to cooperate in completing the questionnaire. The flow chart is shown in Fig. 1.
The research protocol has been granted ethical approval by our Hospital Institutional Review Board, and all participants provided informed consent.
Procedures
The questionnaire design was developed based on the previous relevant literature16,17,18. The initial design underwent a series of rigorous internal discussions and subsequent modifications that refined its content and structure. A pilot test was carried out, resulting in a high Cronbach’s α reliability coefficient of 0.829, signifying strong internal consistency among the questionnaire items. Additionally, the Kaiser-Meyer-Olkin (KMO) value, a measure of sampling adequacy, was determined to be 0.865, suggesting that the data obtained from the survey was suitable for further statistical analyses.
The final questionnaire was administered in the Standard Chinese language, and it encompassed four distinct dimensions. The first dimension aimed to collect demographic information from participants, and it included 10 questions. The second dimension, “Knowledge”, consisted of 12 questions, where questions 5 and 7 were multiple-choice while the remaining were single-choice. Correct answers were assigned a score of 1 point, with an accumulative total score range of 1–20 points, while incorrect or uncertain responses were scored with 0. The third dimension, “Attitude”, included 6 questions, all evaluated using a five-point Likert scale, with scores ranging from 6 to 30 points, reflecting the varying degrees of attitude. The fourth dimension, “Practice”, included 10 questions, with the first being an open-ended inquiry and the remaining being evaluated on a five-point Likert scale. The score for this dimension ranged from 9 to 45 points, representing different action levels. For each section, scores > 70% of the maximum possible score were defined as adequate knowledge, positive attitudes, and proactive practices, establishing a clear benchmark for evaluating respondents’ comprehension and behavior19.
An online questionnaire was created using the WeChat-based Questionnaire Star app, and a QR code was generated to facilitate data collection through WeChat. Participants accessed and completed the questionnaire by scanning the QR code provided within the WeChat platform. In order to maintain data quality and ensure comprehensive responses, only one submission per IP address was permitted, and all questionnaire items were designated as mandatory. The completeness, internal consistency, and overall reasonableness of all collected questionnaires were carefully scrutinized by team members to verify the reliability and validity of the data. Efforts to address potential sources of bias included recruiting participants from multiple hospitals in eastern China to enhance sample representativeness and reduce regional bias. Clear and consistent inclusion criteria ensured participants met CKD conditions and regular HD, minimizing selection bias. The questionnaire was designed based on relevant literature and was subject to thorough internal discussion and pre-testing to ensure clarity and validity. Additionally, the structured questionnaire and standardized measurement tools focused on current knowledge, attitudes, and practices to reduce recall bias by minimizing reliance on participants’ memories.
Statistical analyses
SPSS 26.0 (IBM Corp., Armonk, N.Y., USA) and AMOS 21.0 (Amos Development Corporation, Chicago, IL) were used for statistical analysis. Continuous variables were described using median, 25th percentile, and 75th percentile, and between-group comparisons were performed using t-tests or analysis of variance (ANOVA). Categorical variables were presented as n (%). Pearson correlation analysis was employed to assess the correlations between knowledge, attitude, and practice scores, aiming to validate the KAP theory, which posits that knowledge influences attitudes, subsequently affecting practice. In multivariate analysis, median scores for each dimension were used as cut-off values to identify significant predictors and potential risk factors. Univariate variables with P < 0.25 were included in the multivariate regression to ensure comprehensive risk factor identification. Structural equation modeling (SEM) was utilized to explore the relationships between knowledge (K), attitude (A), and practice (P), providing a robust framework for understanding these interrelationships and identifying key risk factors. Two-sided p < 0.05 represented statistical significance in this study.
Results
Demographic characteristics and impact on KAP
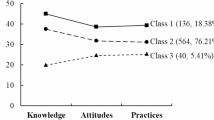
807 questionnaires were returned, 40 did not agree to use the collected data for scientific research, and 15 questionnaires took less than 78 s or more than 1800 s to complete, making a total of 752 valid questionnaires. Among 752 questionnaires that were included in the statistical analysis, 449 (59.7%) were filled out by male patients, 238 (31.6%) by those with undergraduate/junior college education, 288 (38.3%) by those who were retired, 400 (53.2%) by those with a monthly income of < 3,000 yuan, 308 (41.0%) by those under maintenance HD for 5 years, 338 (44.9%) by those who were sure they had no sarcopenia, and 434 (57.7%) by those who were cared for by their spouses. The median (25th percentile, 75th percentile) scores of knowledge (possible range: 1–20), attitude (possible range: 6–30), and practice (possible range: 9–45) were 9 (5, 11), 25 (21, 28) and 33 (28, 37), respectively. The knowledge score varied in patients with different occupation (P = 0.015), residence (P < 0.001), duration of maintenance HD (P = 0.047), and whether they had sarcopenia (P < 0.001). As for the attitude score, there were differences among patients with different levels of education (P < 0.001), occupation type (P = 0.029), and whether they had sarcopenia (P = 0.005). The difference in practice score was found among patients with different education (P < 0.001), monthly income (P = 0.003), and whether they had sarcopenia (P < 0.001) (Table 1). Additionally, 54.1%, 52.7%, and 51.7% had knowledge, attitude, and practice scores greater than or equal to the median, respectively (Table 2).
KAP distribution
The knowledge of patients about sarcopenia was less than optimal, with 68.1% stating that they had never heard of the condition (K1). More than 55% recognized weight loss, inability to lift heavy objects, muscle atrophy, and mobility issues as early symptoms of sarcopenia, while 91.6% incorrectly identified walking faster as one of the symptoms (K5). Concerning the risks posed by sarcopenia, falls and inability to live independently were the most known (71.4% and 64.1%, respectively), while more than half of the patients also misidentified disability and cardiovascular disease (K7). A total of 52.7% knew that proper exercise can prevent sarcopenia (K12). Apart from the above-listed items, the largest proportion of participants opted for “Uncertain” for all other items, exceeding 50%, which indicated that the knowledge of patients needs to be raised urgently (Table 3).
The attitude dimension revealed that 37.9% were very concerned about the development of sarcopenia due to continuous HD (A1), and 56.1% felt that sarcopenia had a significant impact on their daily lives (A2). The importance of three nutritious meals with balanced vegetables and meat (A3) was fully recognized by 63.4% of participants who ultimately agreed with the statement. In addition, 36.6% and 34.2% strongly believed that poor sleep (A4), depression, and negative mood (A5) were positively correlated with the development of sarcopenia. When it comes to the prevention of sarcopenia, 46.7% expressed a strong preference for regular exercise (A6) (Table 4).
Patients had different behaviors towards sarcopenia-related practices, where 47.2% reported a strong need to be educated by professionals on ways to prevent sarcopenia (P2). Moreover, 36.0% (P4) patients generally achieved regular diet and nutrition; however, 34.0% reported that they rarely exercised (P5), and 31.6% were rarely screened for sarcopenia (P7). Relatively optimistically, 50.9% and 57.4% paid regular attention to the changes in their BMI (P9) and actively regulated their mood (P10) (Table 5).
Factors associated with KAP levels
Correlation analyses revealed positive correlations between knowledge and attitude (r = 0.256, P < 0.001) as well as practice (r = 0.189, P < 0.001). There was also a significant positive correlation between attitude and practice (r = 0.391, P < 0.001) (Table 6). However, “Have you noticed a decline in your muscle strength?” (P1) was found to be negatively correlated with attitude (r = -0.232, P < 0.001) and practice (r = -0.124, P < 0.001) (Table 7).
Multivariate logistic regression showed that no factors were independently associated with good knowledge (Table 8). However, college or bachelor’s degree (OR = 1.832, 95% CI: [1.227–2.734], P = 0.003), not suffering from sarcopenia (OR = 0.337, 95% CI: [0.168–0.674], P = 0.002), and uncertainty about their condition (OR = 0.342, 95% CI: [0.171, 0.684], P = 0.002) were independently associated with positive attitude (Table 9). Furthermore, completing high school or vocational secondary school (OR = 1.694, 95% CI: [1.089–2.634], P = 0.019), college or bachelor’s degree (OR = 1.656, 95% CI: [1.069–2.565], P = 0.024), and undergoing maintenance HD for 11 years and above (OR = 0.616, 95% CI: [0.387–0.982], P = 0.042) were independently associated with proactive practice (Table 10).
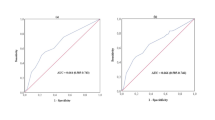
Structural equation model analysis
The residual connection method was adopted to modify the SEM model to achieve a good fit (CMIN/DF value: 3.805, RMSEA value: 0.061, GFI value: 0.853, and AGFI value: 0.826) (Fig. 2). The model results showed that knowledge directly affected attitude (β = 0.475) and practice (β = 0.203). Moreover, attitudes directly affected practice (β = 0.565) (Table 11).
Discussion
The results of the present study showed that maintenance HD patients had a limited understanding of the specific risk factors and preventive measures for sarcopenia, although they were generally aware of the basic concepts. Despite showing concern and worry about sarcopenia, patients often lacked sufficient motivation and resources to take effective action. While some patients attempted to prevent sarcopenia through diet and exercise, the lack of systematic health education and support led to suboptimal practices. These findings suggest that patients with lower educational backgrounds require special attention. Interventions should focus on enhancing knowledge about sarcopenia and its prevention, fostering positive attitudes, and providing the necessary resources and support to encourage proactive practices.
Maintenance HD patients in Northeastern China revealed suboptimal levels of knowledge, attitude, and proactive practice concerning sarcopenia. These deficiencies were evident in the median knowledge, attitude, and practice scores. Various demographic factors such as occupation type, residence, duration of maintenance HD, education, monthly income, and having sarcopenia were found to influence KAP scores. Notably, over half of the participants scored at or below the median in all three domains. The multivariate logistic regression analysis revealed that different factors independently affected knowledge, attitude, and practice. While no specific factors were independently associated with adequate knowledge, a positive attitude was independently associated with having a college or bachelor’s degree, not having sarcopenia, and uncertainty about one’s condition. Furthermore, greater proactive practice was associated with educational background, completing high school or vocational secondary school and a college or bachelor’s degree, and undergoing maintenance HD for 11 years or more. These findings emphasize the importance of tailored educational interventions to address the distinct needs of maintenance HD patients, enhancing their awareness and understanding of sarcopenia, attitudes, and, ultimately, their clinical practices in managing this condition20,21.
The study results highlight the importance of addressing varying levels of awareness and understanding of sarcopenia among respondents, which can significantly impact clinical practice. While the majority acknowledged the role of age and recognized early symptoms and associated risks, there were notable uncertainties and misconceptions, particularly regarding the relationship between maintenance HD, body weight, and malnutrition in the context of sarcopenia. Comprehensive education and training programs should be prioritized for healthcare professionals to advance clinical practice, providing them with accurate, evidence-based information and strategies to promote early detection, prevention, and sarcopenia management22,23. This multifaceted approach should also emphasize the significance of nutrition, exercise, and lifestyle modifications in mitigating the risk of sarcopenia, particularly among populations at risk, such as maintenance HD patients24,25,26.
The present study provides valuable insights into the attitudes of individuals undergoing maintenance HD towards sarcopenia, shedding light on both areas of concern and potential avenues for improvement in clinical practice. Our results revealed a noteworthy proportion of respondents expressing concerns about the link between maintenance HD and sarcopenia, indicating a substantial knowledge gap. In order to address this deficiency, it is essential to develop educational initiatives tailored to these patients, supplying them with comprehensive information and strategies for prevention27,28. Existing studies have shown that resistance exercise can significantly enhance muscle strength, muscle function, and walking ability in HD patients. When combined with proper nutrition, these interventions can further improve outcomes for those with sarcopenia29. However, our research reveals that 44% of patients are in good condition despite not engaging in any form of even mild aerobic exercise. 2023, a Malaysian study showed that public awareness of sarcopenia was generally low, mainly related to age and educational background. The present study found that hemodialysis patients were similarly poorly informed about sarcopenia, and that there was an effect of the patient’s educational level and place of residence on their level of awareness15. By understanding that patients with lower educational backgrounds are less likely to engage in active practice, physicians can focus on simplifying complex medical information and using culturally relevant examples to ensure that these patients are fully aware of the importance of preventing sarcopenia. The referenced study reveals that while Chinese nurses have limited knowledge about sarcopenia, they maintain a positive attitude towards its management, though there is potential for improving their practical behaviors12. Our study found that patient attitudes and practices regarding sarcopenia differed across education levels, emphasizing the need for targeted educational interventions to enhance healthcare professionals’ knowledge and practical management of sarcopenia. Furthermore, Given the findings that some patients recognize a decline in muscle strength but may not respond with appropriate practices, physicians should prioritize regular assessments of muscle health during routine consultations. By doing so, they can provide timely interventions and reinforce the importance of maintaining physical activity and proper nutrition as preventive measures against sarcopenia. Additionally, the present study detected varying beliefs about the impact of sarcopenia on daily life, indicating a need to promote awareness of the potential consequences among this patient population, which could be addressed through structured patient education programs. We also observed a range of beliefs concerning the role of nutrition, sleep quality, and emotional well-being in the development of sarcopenia, calling for evidence-based guidance to clarify these relationships and guide clinical practice. Encouragingly, respondents exhibited a willingness to exercise regularly to prevent sarcopenia, suggesting an opportunity for healthcare providers to emphasize the importance of physical activity as a critical preventive measure. The present study affirms the importance of tailored patient education, evidence-based guidance, and physical activity promotion to improve clinical practice and enhance the prevention and management of sarcopenia among maintenance HD patients30,31,32.
Our findings offer critical insights into the practices and attitudes of maintenance HD patients concerning sarcopenia, with implications for enhancing clinical care and patient outcomes. Notably, a substantial proportion of respondents reported feeling a decline in muscle strength, highlighting the need for healthcare providers to pay closer attention to monitoring muscle health in this patient population33,34. Policymakers should consider developing national or regional health campaigns focused on sarcopenia awareness, particularly in areas with high concentrations of maintenance HD patients. These campaigns could include mass media initiatives, community workshops, and digital platforms to disseminate information on the risks of sarcopenia and the benefits of early prevention. Furthermore, we detected a considerable willingness among respondents to proactively seek education and guidance from professionals on sarcopenia prevention, signifying an opportunity for healthcare institutions to establish educational programs addressing this need. Interestingly, while a significant proportion of patients expressed the importance of dietary and nutritional balance, some reported not adhering to regular and balanced daily meals, underlining the significance of nutritional counseling and support in clinical practice35. Our results also revealed varying levels of engagement in physical activity, with a substantial number of patients expressing family support, highlighting the potential for family involvement in exercise promotion36. Moreover, not all patients regularly underwent sarcopenia-related examinations, indicating the need to improve the accessibility and awareness of such assessments within clinical practice. Finally, the responses concerning seeking prompt medical attention for muscle weakness or pain and paying attention to body weight or BMI changes varied, underlining the importance of encouraging patients to be more vigilant about these health indicators37,38.
Our correlation analyses revealed several key insights that have significant implications for improving clinical practice related to sarcopenia. Firstly, the positive correlations between knowledge and attitude and between knowledge and practice emphasize the importance of increasing patients’ understanding of sarcopenia, which may positively impact their attitudes and behaviors. These findings suggest that educational interventions focusing on enhancing patients’ knowledge can serve as a foundation for improved attitudes and practices related to sarcopenia. Furthermore, the significant positive correlation between attitude and practice emphasizes that shaping positive attitudes among patients is crucial to promoting better clinical practice. Healthcare providers should consider incorporating attitude-building strategies into patient education programs to encourage more proactive and effective preventive actions. Interestingly, the negative correlations of the question “Have you noticed a decline in your muscle strength?” with attitude and practice indicate potential concern. This suggests that patients who perceive muscle strength decline may be less likely to exhibit positive attitudes and engage in recommended practices. Therefore, addressing the fears or concerns related to muscle strength loss is essential in patient education and counseling. The SEM results reaffirm the importance of knowledge as a driver of attitudes and practices and attitudes as influential in shaping patients’ actual practices. These findings underscore the need for comprehensive, knowledge-focused educational interventions in clinical practice to bridge the knowledge gap and cultivate positive attitudes, ultimately leading to better preventive practices against sarcopenia. Our results underscore the pivotal role of knowledge enhancement and attitude-building initiatives in improving clinical practice related to sarcopenia prevention and management among maintenance HD patients24.
The findings of this study have several important managerial implications for healthcare providers and policymakers. Targeted health education strategies should be developed to address the inadequate knowledge among maintenance HD patients, which includes creating detailed and easily understandable educational materials that cover the definition, risk factors, and preventive measures of sarcopenia. Personalized intervention plans should be designed based on patients’ KAP levels, with behavior change support and resources provided to those with higher knowledge but insufficient practice and enhanced knowledge education for those with positive attitudes but limited understanding. Optimizing resource allocation is of crucial importance, ensuring that healthcare and educational resources are prioritized for high-risk patients. Multidisciplinary collaboration within healthcare institutions, integrating the expertise of dietitians, rehabilitation therapists, and psychological counselors, can help formulate and implement comprehensive intervention programs.
The present study has some limitations. As a result of the self-reported nature of the online questionnaire, highly specialized aspects, such as uremic toxins, acidosis, and chronic inflammation, were not included due to concerns about the accuracy of patient responses, which poses a significant limitation as these factors are critical in the context of HD patients. In future studies, clinical practitioners should be included more extensively to ensure that these critical health details are accurately captured and considered, thus enhancing the comprehensiveness and applicability of the research findings.
Conclusions
Maintenance HD patients demonstrated inadequate knowledge, positive attitudes, and proactive practices toward sarcopenia. These results suggest that educational programs targeting patients with lower educational backgrounds could be particularly beneficial, as these individuals were less likely to engage in proactive practices regarding sarcopenia. Additionally, efforts should focus on enhancing the knowledge and attitudes of all patients, as the study demonstrates that knowledge directly influences attitudes and practices, and attitudes directly impact practices. Implementing educational initiatives and providing resources to raise awareness about sarcopenia, its consequences, and the importance of preventive measures could contribute to a more proactive approach among these patients, ultimately improving their overall healthcare outcomes. Future research should explore the causal relationships between KAP levels and health outcomes through longitudinal studies and integrate clinical data and objective measurements alongside self-reported data to enhance the accuracy and reliability of the findings, thus providing more comprehensive evidence for effective interventions and policies.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- KAP:
-
Knowledge, attitude and practice
- CKD:
-
Chronic kidney disease
- ESRD:
-
End-stage renal disease
- HD:
-
Hemodialysis
- KMO:
-
Kaiser-Meyer-Olkin
- ANOVA:
-
Analysis of variance
- SEM:
-
Structural equation modeling
References
Fan, Z., Guo, Y., Zhong, X. Y. & Circulating Cell-Free Mitochondrial, D. N. A. A potential blood-based biomarker for Sarcopenia in patients undergoing maintenance hemodialysis. Med. Sci. Monit. 28, e934679 (2022).
Sánchez-Tocino, M. L. et al., Sarcopenia and Mortality in Older Hemodialysis Patients. Nutrients. 14, 11 (2022).
Chen, Z., Ho, M., & Chau, P. H. Prevalence Incidence, and Associated Factors of Possible Sarcopenia in Community-Dwelling Chinese older adults: A Population-based longitudinal study. Front. Med. (Lausanne). 8, 769708 (2021).
Hwang, S. D. et al. Risk of overhydration and low lean tissue index as measured using a body composition monitor in patients on hemodialysis: A systemic review and meta-analysis. Ren. Fail. 40, 51–59 (2018).
Pegoli, G. et al., Role of Cdkn2a in the Emery-Dreifuss Muscular Dystrophy Cardiac Phenotype. Biomolecules. 11, (2021).
Khalid, A. et al. Promoting health literacy about Cancer Screening among Muslim immigrants in Canada: Perspectives of imams on the Role they can play in Community. J. Prim. Care Community Health. 13, 21501319211063051 (2022).
Koni, A. et al. A cross-sectional evaluation of knowledge, attitudes, practices, and perceived challenges among Palestinian pharmacists regarding COVID-19. SAGE Open. Med. 10, 20503121211069278 (2022).
Shubayr, M. A., Kruger, E. & Tennant, M. Oral health providers’ views of oral health promotion in Jazan, Saudi Arabia: A qualitative study. BMC Health Serv. Res. 23, 214 (2023).
Reca, R. Impact of maternal health education on pediatric oral health in Banda Aceh: A quasi-experimental study. Healthcraft Front. 2, 10–19 (2024).
Okafor, S. COVID-19 public health and social measures in Southeast Nigeria and its implication to public health management and sustainability. Opportunities Challenges Sustain. 1, 61–75 (2022).
Jafar, A. & Quadri, U. Macroeconomic outcomes of healthcare financing reforms in Nigeria: A computable general equilibrium analysis. J. Acc. Fin Audit Stud. 9, 420–448 (2023).
Ji, M. et al. A survey of nurses’ knowledge, attitudes, and practice of Sarcopenia: A cross-sectional study. Nurse Educ. Pract. 74, 103869 (2024).
Lu, F. et al. Knowledge, attitude, and practice regarding Sarcopenia: A survey between orthopedic and geriatric professionals in China. Aging Clin. Exp. Res. 35, 2019–2028 (2023).
Silva, R. F., Figueiredo, M., Darder, J. J. T., Santos, A. & Tyrrell, M. A. R. Sarcopenia screening in elderly in primary health care: Nurse knowledge and practices. Rev. Bras. Enferm. 73, e20200421 (2020).
Keng, S. L. et al. Knowledge of Sarcopenia and associated factors among the Malaysian General Public: A cross-sectional study. J. Prev. Med. Public. Health. 56, 164–171 (2023).
Mori, K. Maintenance of Skeletal Muscle to Counteract Sarcopenia in Patients with Advanced Chronic Kidney Disease and Especially Those Undergoing Hemodialysis. Nutrients. 13, (2021).
Reis, J. M. S., Alves, L. S. & Vogt, B. P. According to revised EWGSOP Sarcopenia Consensus Cut-Off points, low physical function is Associated with Nutritional Status and Quality of life in maintenance hemodialysis patients. J. Ren. Nutr. 32, 469–475 (2022).
Ren, H., Gong, D., Jia, F., Xu, B. & Liu, Z. Sarcopenia in patients undergoing maintenance hemodialysis: Incidence rate, risk factors and its effect on survival risk. Ren. Fail. 38, 364–371 (2016).
Lee, F. & Suryohusodo, A. A. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: A cross-sectional study. Front. Public. Health. 10, 957630 (2022).
Makhinova, T. et al. Improving Asthma Management: Patient-Pharmacist Partnership Program in Enhancing Therapy Adherence. Pharmacy (Basel). 10, (2022).
Nordfalk, J. M., Holmøy, T., Thomas, O., Nylenna, M. & Gulbrandsen, P. Training physicians in providing complex information to patients with multiple sclerosis: A randomised controlled trial. BMJ Open. 12, e049817 (2022).
Keshavarzi, M. H. et al. Exploration the role of a clinical supervisor to improve the professional skills of medical students: A content analysis study. BMC Med. Educ. 22, 399 (2022).
Yilmaz, Y. et al. What Faculty want: Academic and Community Emergency Physicians’ perceptions of Learner Feedback. Cureus. 14, e23546 (2022).
Dang, L. T. et al. The Associations of Suspected COVID-19 Symptoms with Anxiety and Depression as Modified by Hemodialysis Dietary Knowledge: A Multi-Dialysis Center Study. Nutrients. 14, (2022).
Mahjubian, A., Bahraminejad, N. & Kamali, K. The Effects of Group Discussion Based Education on the Promotion of Self-Management behaviors in Hemodialysis patients. J. Caring Sci. 7, 225–232 (2018).
Sabouri, F., Rambod, M. & Khademian, Z. The effect of positive thinking training on hope and adherence to treatment in hemodialysis patients: A randomized controlled trial. BMC Psychol. 11, 6 (2023).
Mahdi, A., Svantesson, M., Wretenberg, P. & Hälleberg-Nyman, M. Patients’ experiences of discontentment one year after total knee arthroplasty- a qualitative study. BMC Musculoskelet. Disord. 21, 29 (2020).
Olczyk, P., Kusztal, M., Gołębiowski, T., Letachowicz, K. & Krajewska, M. Cognitive impairment in End Stage Renal Disease patients undergoing hemodialysis: Markers and risk factors. Int. J. Environ. Res. Public. Health. 19, 4 (2022).
Li, L., Ma, X., Xie, C. & Li, Y. Resistance exercise interventions for Sarcopenia and nutritional status of maintenance hemodialysis patients: A meta-analysis. PeerJ. 12, e16909 (2024).
Ayers, K. L. et al. Analysis of Real-World Data to Investigate the Impact of Race and Ethnicity on Response to Programmed Cell Death-1 and Programmed Cell Death-Ligand 1 Inhibitors in Advanced Non-Small Cell Lung Cancers. Oncologist. 26 , e1226-e1239 (2021).
Pol-Castañeda, S. et al. Moving Evidence into Practice by Advanced Practice Nurses in Hospitalization Wards. Protocol for a Multicentre Quasi-Experimental Study in Three Hospitals in Spain. Int. J. Environ. Res. Public. Health. 17, 10 (2020).
Yamashita, R. et al. Effects of social network incentives and financial incentives on physical activity and social capital among older women: A randomized controlled trial. BMC Public. Health. 21, 188 (2021).
Klein, I., Kalichman, L., Chen, N. & Susmallian, S. Effect of physical activity levels on oncological breast surgery recovery: A prospective cohort study. Sci. Rep. 11, 10432 (2021).
Xie, Z. et al. Mediation of 10-Year cardiovascular disease risk between inflammatory diet and handgrip strength: Base on NHANES 2011–2014. Nutrients. 15, 4 (2023).
Goodrose-Flores, C., Eke, H., Bonn, S. E., Björkhem-Bergman, L. & Trolle Lagerros, Y. Weight loss in Advanced Cancer: Sex differences in Health-Related Quality of Life and Body Image. Life (Basel). 12, (2022).
Pearson, R. C. & Jenkins, N. T. Dietary intake of adults who participate in crossFit(®) exercise regimens. Sports (Basel). 10, 3 (2022).
Bai, C. et al. Sleep duration, vegetable consumption and all-cause mortality among older adults in China: A 6-year prospective study. BMC Geriatr. 21, 373 (2021).
Mengistu, S. et al. Stillbirth and Associated factors among women who gave birth at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia. Front. Pediatr. 10, 820308 (2022).
Funding
The study was supported by the Project of the Education Department of Jilin Province [JJKH20211192KJ].
Author information
Authors and Affiliations
Contributions
Yanbo Li and Tianyang Lv carried out the studies, participated in collecting data, and drafted the manuscript. Yanan Dong and Hongrui Zhang performed the statistical analysis and participated in its design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The research protocol has been granted ethical approval by the First Hospital of Jilin University Institutional Review Board [23K270-001]. All participants were informed about the study protocol and provided written informed consent to participate. All methods were performed in accordance with the relevant guidelines. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lv, T., Dong, Y., Zhang, H. et al. Knowledge, attitude, and practice regarding Sarcopenia in maintenance hemodialysis patients in Northeastern China. Sci Rep 14, 24775 (2024). https://doi.org/10.1038/s41598-024-75395-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-75395-0