Abstract
This study aimed to determine the efficacy of using both the postero-anterior and oblique image intensifier views intra-operatively and late start of post-operative partial weight-bearing (PWB) in reducing the incidence of delayed union in the ischium at one year after curved periacetabular osteotomy. We evaluated computed tomography images to clarify the incidence of delayed union at the osteotomy sites at one year post-operatively for 117 hips in 104 patients. Fifty-eight hips in 54 patients with use of both the postero-anterior and oblique image intensifier views intra-operatively and late start of post-operative PWB were assigned to the oblique view and late PWB group (OL group) and 59 hips in 50 patients with use of only the postero-anterior image intensifier view intra-operatively and early start of post-operative PWB were assigned to the control group (C group). In univariate analyses, the incidence of delayed union in the ischium at one year post-operatively was significantly lower in the OL group (3.5%) than in the C group (22%). Use of both the postero-anterior and oblique image intensifier views during curved periacetabular osteotomy and late start of PWB were effective for reducing delayed union of the ischium at one year post-operatively.
Similar content being viewed by others
Introduction
Several types of periacetabular osteotomy, such as curved periacetabular osteotomy (CPO)1, Bernese periacetabular osteotomy2, transposition osteotomy of the acetabulum3, rotational acetabular osteotomy4, eccentric rotational acetabular osteotomy5, and spherical periacetabular osteotomy6, have been performed to treat symptomatic acetabular hip dysplasia. Our institution has performed CPO, a modified Bernese periacetabular osteotomy, since 1995.
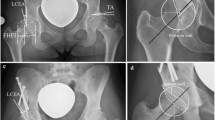
Several complications associated with periacetabular osteotomy have been reported, including delayed union at the osteotomy sites7,8,9,10,11,12,13,14,15,16,17,18,19, stress fractures of the inferior pubic or ischial rami20,21,22, and injuries to the lateral femoral cutaneous or sciatic nerves23,24. Delayed union at the osteotomy sites in the pubis, ischium, and ilium is painful and may require revision surgery9,10,11,14,18. The reported incidence of discontinuity identified on radiographs was 0.4–8.4% for the ischium7,9,18,19, 2.1–16.8% for the pubis7,8,9,10,11,12,14,15,16,17, and 0.4% for the ilium18, while the reported incidence on computed tomography (CT) images was 8.4–10.2% for the ischium, 20.6–28.5% for the pubis, 0% for the ilium7,25, and 0% for the anterior superior iliac spine (ASIS)25. X-ray examinations and image intensifier views have been used to prevent posterior column dissection and intra-articular osteotomy during periacetabular osteotomy5,24. In previous reports, patients who underwent CPO were allowed to undertake partial weight-bearing (PWB) on the second or third post-operative day7,25. Recently, with the aim of reducing delayed union in the ischium at one year post-operatively, we have performed CPO using both the postero-anterior (PA) and oblique image intensifier views to ensure the thickness of the posterior column of the pelvis (Fig. 1) and have allowed patients to start PWB at 2–4 weeks post-operatively to prevent fatigue fractures of the column.
Oblique image intensifier views to prevent dissection of the posterior column and intra-articular osteotomy during curved periacetabular osteotomy. (a) The ischium of the posterior column is osteotomised from the innominate grooves using a curved chisel. (b) The ilium of the posterior column is osteotomised from the arcuate line using a curved chisel. The solid white lines indicate the joint line of the acetabulum, and the dashed white lines indicate the posterior border of the posterior column.
The present study aimed to determine the efficacy of using the oblique image intensifier view in addition to the PA image intensifier view intra-operatively and late start of post-operative PWB in reducing the incidence of delayed union in the ischium at one year post-operatively. We hypothesized that use of both PA and oblique image intensifier views during CPO and late start of post-operative partial weight-bearing reduce the incidence of delayed union in the ischium at one year post-operatively.
Patients and methods
Patients
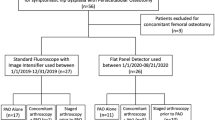
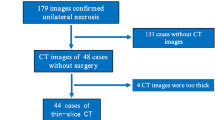
We performed a retrospective review of 153 hips in 136 consecutive patients who underwent CPO surgery performed by either of two experienced senior orthopaedic surgeons between July 2014 and November 2019 at a single institution (Fig. 2). We included patients who underwent CPO between July 2014 and June 2017 and were part of the population described by Kamachi et al.25. Thirty hips in 30 patients were excluded because they did not undergo a CT scan at one year post-operatively. However, the contralateral hips in two of these patients were included (follow-up rate, 80.4%). All six hips in six patients who underwent CPO between February 2017 and June 2017 with use of both the PA and oblique image intensifier views and who undertook PWB on the second or third post-operative day were excluded because of their low number for assignment to a group for statistical analysis. However, the contralateral hips in two of these patients were included. Finally, 117 hips in 104 patients (three men, 101 women) were included in the study. The mean age at surgery was 36.5 ± 14.1 (range, 13–61) years, and the mean body mass index was 22.7 ± 3.7 (range, 16.1–36.8) kg/m2. The pre-operative diagnosis in all patients was developmental dysplasia of the hip.
At our institution, the indications for CPO are age < 65 years at the time of surgery after Y-shaped cartilage closure, pain and limited activities of daily living for > 5 months, lateral centre-edge angle (LCEA) < 25º on an antero-posterior radiograph, and improved joint congruence in the abducted position on an antero-posterior radiograph. Meanwhile, the indications for CPO in the treatment of patients aged > 60 years with developmental dysplasia of the hip are non-end-stage arthropathic changes, good joint compatibility, and strong patient desire for periacetabular osteotomy26.
Surgical technique and post-operative rehabilitation
The surgical procedure was performed via an anterior incision at the distal border of the ASIS. The incision extended distally along the tensor fasciae latae muscle. The ASIS was osteotomised in a wedge-shaped manner, with the inguinal ligament and sartorius muscle remaining attached, to prevent the outer table of the pelvis from dissecting. The osteotomised ASIS was approximately 4 cm in length and retracted medially along with the inguinal ligament and neurovascular bundle. The ischium was osteotomised while preserving the continuity of the posterior column. The pubis was completely osteotomised at the base of the superior pubic ramus. An iliac osteotomy was performed in a C-shape to allow connection with the ischial osteotomy site while preserving the continuity of the posterior column. For patients who underwent CPO between July 2014 and January 2017, only the PA image intensifier view was used. In patients who underwent CPO between February 2017 and November 2019, both the PA and oblique image intensifier views were used. When using the oblique view, the image intensifier was tilted approximately 45 to 70 degrees relative to the PA view, so that the shape of the short-axis tangent of the osteotome was depicted. The function for use of the oblique view was to preserve the continuity of the posterior column during the ischial and iliac osteotomies. The acetabular fragment was rotated laterally and fixed with three poly-L-lactic acid screws. The ASIS was fixed with two 4-mm diameter titanium cannulated cancellous screws. At our institution, we previously simulated the push-off phase of the gait cycle using a servo-hydraulic material testing system on composite model hemipelves after CPO. Biomechanically, we found that the average failure loads did not differ significantly between the group with three titanium screws and the group with three HA/PLLA screws27. Thus, three HA/PLLA screws were used for fixation of the rotated bone fragments. Meanwhile, no studies have been conducted on the stability of titanium screws versus HA/PLLA screws for the anterior superior iliac spine, and therefore we have continued to use titanium screws for fixation of the anterior superior iliac spine. None of the patients in the present study underwent bone grafting at any of the osteotomy sites.
Unlimited range-of-motion (ROM) exercises were initiated on the first post-operative day. The patients who underwent CPO between July 2014 and June 2017 began 10-kg PWB on the second or third post-operative day (early PWB start), while patients who underwent CPO between July 2017 and November 2019 began 20-kg PWB at 2–4 weeks post-operatively (late PWB start), with both sets of patients using two crutches or a walker. In all patients, the weight-bearing was increased by 10 kg every two weeks after beginning PWB.
All patients underwent an initial CT scan at one week post-operatively and a further CT scan at one year post-operatively (mean, 12.3 ± 2.1 months; range, 6–18 months). For the scans, the patients were supine with the hip in a neutral position. All scans were performed using a 64-channel multi-detector CT system (Aquilion TSX-101 A/HA; Toshiba Medical Systems, Tochigi, Japan). The CT scan at one week post-operatively was conducted to measure the narrowest gap at the pubic osteotomy site, in accordance with previous reports8,25, and to measure the minimal post-operative thickness of the ischium (Fig. 3). The CT scan at one year post-operatively was performed to assess bone union at the osteotomy sites in the ischium, pubis, ilium, and ASIS. Bone union at the pubic and ASIS osteotomy sites was assessed on coronal and axial slices, while bone union at the ischial and iliac osteotomy sites was assessed on coronal and sagittal slices (Fig. 4), as previously reported7,25. Delayed union was defined as a lack of bone continuity on both images (Fig. 5).
Measurement of the minimal thickness of the ischium post-operatively. The measurement is shown on an axial computed tomography image of a right hip at one week post-operatively. Line ‘a’ is the line connecting the two ends (white arrows) of the osteotomy site in the ischium. Line ‘b’ is parallel to line ‘a’ and passes through the posterior margin of the ischium (white arrowhead). The post-operative ischial thickness (black double-headed arrow) is measured as the vertical distance between lines ‘a’ and ‘b’. The minimal thickness of the ischium is defined as the thinnest ischial thickness between the proximal and distal ends of the osteotomy.
Images for a 56-year-old woman who underwent curved periacetabular osteotomy for left hip dysplasia. (a–f) The computed tomography images indicated bone union at all osteotomy sites at one year post-operatively. The ischium was assessed for bone union or delayed union on (a) sagittal and (b) coronal slices (white circles). The pubis was assessed for bone union or delayed union on (c) coronal and (d) axial slices (white circles). The ilium was assessed for bone union or delayed union on (a) sagittal and (c) coronal slices (white dashed circles). The anterior superior iliac spine was assessed for bone union or delayed union on (e) sagittal and (f) axial slices (white circles).
Images for a 43-year-old woman who underwent curved periacetabular osteotomy for right hip dysplasia. (a–d) The computed tomography images indicated delayed union at the osteotomy sites in the ischium and pubis at one year post-operatively. The ischium was assessed for bone union or delayed union on (a) sagittal and (b) coronal slices (white circles). The pubis was assessed for bone union or delayed union on (c) coronal and (d) axial slices (white circles).
The LCEA, acetabular roof obliquity (ARO), and head lateralisation index (HLI)28 were measured on antero-posterior radiographs pre-operatively and at one year post-operatively. The severity of osteoarthritis was classified preoperatively and at one year postoperatively according to the Tönnis classification system as grade 0 (no signs of osteoarthritis), grade 1 (slight narrowing of the joint space, slight lipping at the joint margin, and slight sclerosis of the femoral head or acetabulum), grade 2 (small cysts in the femoral head or acetabulum, increased narrowing of the joint space, moderate loss of sphericity of the femoral head), or grade 3 (large cysts, severe narrowing or obliteration of the joint space, severe deformity of the femoral head, avascular necrosis)29.
Patients with use of both the PA and oblique image intensifier views during CPO and late start of post-operative PWB were assigned to the oblique view and late PWB group (OL group), while patients with use of only the PA image intensifier view during CPO and early start of post-operative PWB were assigned to the control group (C group) to determine the incidence of delayed union at the osteotomy sites and conduct statistical analyses for the radiographic and clinical evaluations in the two groups.
The CT images and radiographs were independently assessed by five orthopaedic surgeons. For delayed union of the osteotomy sites, two orthopaedic surgeons evaluated the findings for patients who underwent CPO between July 2014 and January 2017, and another two orthopaedic surgeons evaluated the findings for patients who underwent CPO between July 2017 and November 2019. Regarding the minimal thickness of the ischium at one week postoperatively, two orthopaedic surgeons evaluated the findings for the patients who underwent CPO between July 2017 and November 2019. The observers were blinded to the clinical outcomes and reviewed the CT images and radiographs twice on different days.
The Harris hip score (HHS) was assessed for clinical evaluation pre-operatively and at one year post-operatively. The HHS was investigated on the same day as the CT scan at one year post-operatively. Patient habits such as smoking and drinking as well as comorbidities such as diabetes, liver disease, heart disease, and depression were also examined.
Statistics
The Mann–Whitney U test was used to compare demographic characteristics, duration between surgery and CT scan, radiographic parameters, and HHS between the two groups. Fisher’s exact test was used to compare sex, incidence of delayed union at the osteotomy sites, habits, and comorbidities between the two groups. between the two groups. Use of the oblique view, late start of post-operative PWB, minimal post-operative thickness of the ischium, width of the gap at the pubic osteotomy site, ARO at one year post-operatively, and smoking were included in a binomial logistic regression analysis to identify risk factors for delayed union at the ischial osteotomy site at one year post-operatively. BellCurve for Excel version 3.22 (Social Survey Research Information Co. Ltd., Tokyo, Japan) was used for all statistical analyses. Values of p < 0.05 in all analyses were considered statistically significant.
Ethics
This study was performed in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments. Approval was granted by the Ethics Committee of Fukuoka University Faculty of Medicine (approval number, U23-11-012; approval date, 16 November 2023). Due to the retrospective nature of the study, (the Ethics Committee of Fukuoka University Faculty of Medicine) waived the need of obtaining informed consent. All participants were given the opportunity to refuse to participate in the study (opt-out option).
Results
Fifty-eight hips in 54 patients (54 women) were assigned to the OL group, and 59 hips in 50 patients (three men, 47 women) were assigned to the C group. The demographic characteristics of the patients did not differ significantly between the two groups (Table 1). The incidence of delayed union in the ischium was 3.5% (2/58 hips) in the OL group and 22% (13/59 hips) in the C group, while the incidence of delayed union in the pubis was 24.1% (14/58 hips) in the OL group and 33.9% (20/59 hips) in the C group (Table 2). All of the iliac and ASIS osteotomy sites achieved union at one year post-operatively. In the univariate analyses, the incidence of delayed union in the ischium, mean ARO at one year post-operatively, and width of the gap at the pubic osteotomy site were significantly smaller in the OL group (3.5%, − 2.6º, and 1.5 mm, respectively) than in the C group (22%, 0.4º, and 4.7 mm, respectively), while the LCEA at one year post-operatively, and the amounts of LCEA and ARO correction and the minimal thickness of the ischium at one week post-operatively were significantly larger in the OL group (39.2º, 26.1º, 20.6º, and 18.0 mm, respectively) than in the C group (33.7º, 20.8º, 16.0º, and 13.6 mm, respectively) (Table 3). The mean HLI at one year post-operatively was significantly smaller in the OL group (0.51) than in the C group (0.57), indicating that the OL group obtained more medialisation of the femoral head after CPO than the C group. The mean total, pain, function, and range-of-motion scores in the HHS at one year post-operatively were significantly higher in the OL group (95.3, 41.1, 45.3, and 4.9 points, respectively) than in the C group (89.0, 37.0, 44.2, and 4.8 points, respectively) (Table 3). The multivariate analysis revealed that minimal post-operative thickness of the ischium (odds ratio [OR] 0.79, 95% confidence interval [CI] 0.66–0.94) and width of the gap at the pubic osteotomy site (OR 1.38, 95% CI 1.7–8.5) were significantly associated with delayed union at the ischial osteotomy site as independent risk factors.
The kappa coefficients for delayed union at the osteotomy sites were 0.95–1.00 (intra-observer variance) and 0.96–1.00 (inter-observer variance), and those for the minimal thickness of the ischium at one week post-operatively were 0.99 and 1.00 (intra-observer variance) and 0.91 (inter-observer variance).
Discussion
This study is the first retrospective case–control study to investigate the efficacy of using the oblique image intensifier view during CPO and late start of post-operative PWB. Two major findings were obtained. First, the incidence of delayed union in the ischium at one year postoperatively in patients with use of both the PA and oblique image intensifier views and late start of postoperative PWB was lower than that in patients with use of only the PA image intensifier view and early start of postoperative PWB. Second, the HHS at one year postoperatively was significantly higher in the OL group than in the C group.
Doi et al.30 reported that the mean equivalent stress at the ischial ramus was 1.7 times higher in models for non-union of the pubic osteotomy site than in models for union of the same site in a finite element analysis. The load stress transferred through the ischium to the ischial ramus may increase until union at the pubic osteotomy site is achieved. In the present study, the greater thickness of the ischium after CPO in the OL group compared with the C group may have allowed the ischium to withstand the transmitted load stress until the pubic osteotomy site achieved union, resulting in a smaller incidence of delayed union in the ischium at one year post-operatively in the OL group compared with the C group. Furthermore, minimal post-operative thickness of the ischium was significantly associated with delayed union at the ischial osteotomy site as an independent risk factor. The fact that the ischium was thicker post-operatively in the OL group compared with the control group suggests that the use of the oblique view was beneficial. We believe that the reduced incidence of delayed union in the ischium at one year post-operatively was more closely related to the use of the oblique view than to the late start of post-operative PWB.
Casanova et al.31 described that the cartilage formed in fracture gaps started to become internalised at approximately two weeks post-fracture for conversion into lamellar bone by endochondral ossification. The state of bone union at the ischial osteotomy site at the start of PWB may have been more advanced in the OL group than in the C group. We consider that the late start of PWB may have contributed to the reduced incidence of delayed union in the ischium at one year post-operatively.
Kamachi et al.25 reported that larger width of the gap at the pubic osteotomy site on CT images and amount of ARO correction on radiographs were independent predictors for increased incidence of delayed union in the ischium. Our findings align with their conclusions regarding gap width, but are inconsistent with the findings of earlier studies in relation to ARO correction. In the present study, medialisation of the femoral head was significantly greater in the OL group than in the C group. This raises the possibility for involvement of factors that move the acetabular fragment closer to the pubis, such as medialisation of the fragment. Matsunaga et al.8 reported that patients with a larger width of the gap at the pubic osteotomy site on CT at one week post-periacetabular osteotomy had a higher incidence of delayed union at one year post-periacetabular osteotomy than patients with a smaller width of the gap. Their study showed a trend toward more medialisation of the femoral head in the pubic union group at one year post-operatively compared with the delayed union group (p = 0.057). These findings in the present study and previous studies suggest that medialisation of the femoral head may reduce the width of the gap at the pubic osteotomy site and decrease the incidence of delayed union in the pubis and ischium at one year post-operatively. Currently, we use a bone graft taken from the ilium to fill the gap at the pubic osteotomy site during CPO. In the future, we intend to validate the effectiveness of this surgical technique.
The HHS, LCEA, and ARO at one year post-operatively were significantly better in the OL group compared with the C group. In a previous study, Lerch et al.32 found that the factors associated with poor long-term outcomes after Bernese PAO were THA, radiographic progression of osteoarthritis, and/or Merle d’Aubigné-Postel score < 15. Lesser post-operative LCEA and ARO were not included in the risk factors. Similarly, Tanaka et al.33 found that these parameters were not included in the risk factors for poor long-term outcomes based on a median follow-up period of 10 years after transposition osteotomy of the acetabulum. Therefore, the differences in these parameters may not affected the better HHS in the OL group.
The present study has several limitations. First, the one-year CT scans were conducted at 6 to 18 months postoperatively. Specifically, 12 hips underwent the CT scan at < 10 months postoperatively; among these hips, one hip in the OL group and one hip in the C group showed delayed union in the ischium, and three hips in the OL group and two hips in the C group showed delayed union in the pubis. Meanwhile, 23 hips underwent the CT scan at > 14 months postoperatively; among these hips, five hips in the OL group and 14 hips in the C group showed union in the ischium and three hips in the OL group and 13 hips in the C group showed union in the pubis. Analyses using Fisher’s exact test were performed assuming that the two hips with delayed union in the ischium and five hips with delayed union in the pubis on CT images at < 10 months postoperatively were union, while the 19 hips with union in the ischium and 16 hips with union in the pubis on CT images at > 14 months were delayed union. As a result, the incidence of delayed union in the ischium at one year postoperatively remained lower in the OL group than in the C group. However, the incidence of delayed union in the pubis was significantly lower in the OL group than in the C group. At least, we consider that the effect of the variation in CT scan performance time may have been negligible for the analysis of the incidence of delayed union in the ischium in the present study. Second, the follow-up rate was 80.4%. This slightly low follow-up rate may have affected the results of the study. However, the follow-up rates in other similar studies based on CT scans were approximately 10% lower and ranged from 71.3 to 72.4%7,25. Third, patients with use of both the PA and oblique image intensifier views and early start of post-operative PWB were excluded from the present study because of their low number. If the number of these patients can be increased, it may be possible to determine whether either use of both image intensifier views or late start of post-operative PWB is an independent predictor for decreased incidence of delayed union in the ischium at one year post-operatively. Fourth, only the HHS, a clinician-reported outcome, was investigated in the present study. Further studies should also evaluate patient-reported outcomes.
In conclusion, the incidence of delayed union in the ischium at one year postoperatively was significantly lower in patients who underwent CPO with use of both the PA and oblique image intensifier views intraoperatively and late start of postoperative PWB than in patients who underwent CPO with use of only the PA image intensifier view intraoperatively and early start of postoperative PWB. Use of both PA and oblique image intensifier views during CPO and late start of postoperative PWB were effective for reducing delayed union in the ischium at one year postoperatively.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Naito, M., Shiramizu, K., Akiyoshi, Y., Ezoe, M. & Nakamura, Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin. Orthop. Relat. Res.433, 129–135 (2005).
Ganz, R., Klaue, K., Vinh, T. S. & Mast, J. W. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin. Orthop. Relat. Res.232, 26–36 (1998).
Matsuo, A. et al. Transposition osteotomy of the acetabulum for advanced-stage osteoarthritis of the hips. J. Orthop. Sci.14 (3), 266–273 (2009).
Ninomiya, S. & Tagawa, H. Rotational acetabular osteotomy for the dysplastic hip. J. Bone Joint Surg. Am.66 (3), 430–436 (1984).
Hasegawa, Y. et al. Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years. J. Bone Joint Surg. Am.84 (3), 404–410 (2002).
Hara, T. et al. Spherical periacetabular osteotomy. J. B J. S Essent. Surg. Tech.12(3), e21.00048 (2022).
Akiho, S. et al. Incidence of delayed union one year after peri-acetabular osteotomy based on computed tomography. Int. Orthop.42 (5), 1029–1034 (2018).
Matsunaga, A., Akiho, S., Kinoshita, K., Naito, M. & Yamamoto, T. The prevalence and risk factors for delayed union of the superior pubic ramus at one year after curved periacetabular osteotomy: its risk factor and outcome. Int. Orthop.42 (6), 1253–1258 (2018).
Thawrani, D., Sucato, D. J., Podeszwa, D. A. & DeLaRocha, A. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J. Bone Joint Surg. Am.92 (8), 1707–1714 (2010).
Clohisy, J. C., Nunley, R. M., Curry, M. C. & Schoenecker, P. L. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J. Bone Joint Surg. Am.89 (7), 1417–1723 (2007).
Peters, C. L., Erickson, J. A. & Hines, J. L. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J. Bone Joint Surg. Am.88 (9), 1920–1926 (2006).
Davey, J. P. & Santore, R. F. Complications of periacetabular osteotomy. Clin. Orthop. Relat. Res.363, 33–37 (1999).
Biedermann, R. et al. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int. Orthop.32 (5), 611–617 (2008).
Garras, D. N., Santangelo, J. R., Wang, D. W. & Easley, M. E. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J. Bone Joint Surg. Br.89 (6), 721–724 (2007).
Matta, J. M., Stover, M. D. & Siebenrock, K. Periacetabular osteotomy through the Smith-Petersen approach. Clin. Orthop. Relat. Res.363, 21–32 (1999).
Crockarell, J. Jr., Trousdale, R. T., Cabanela, M. E. & Berry, D. J. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin. Orthop. Relat. Res.363, 45–53 (1999).
Murphy, S. & Deshmukh, R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin. Orthop. Relat. Res.405, 168–174 (2002).
Hussell, J. G., Rodriguez, J. A. & Ganz, R. Technical complications of the Bernese periacetabular osteotomy. Clin. Orthop. Relat. Res.363, 81–92 (1999).
Clohisy, J. C., Barrett, S. E., Gordon, J. E., Delgado, E. D. & Schoenecker, P. L. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J. Bone Joint Surg. Am.88(Suppl (1 Pt), 65–83 (2006).
Espinosa, N., Strassberg, J., Belzile, E. L., Millis, M. B. & Kim, Y. J. Extraarticular fractures after periacetabular osteotomy. Clin. Orthop. Relat. Res.466, 1645–1651 (2008).
Tsuboi, M., Hasegawa, Y., Fujita, K. & Kawabe, K. Pubic/ischial stress fractures after eccentric rotational acetabular osteotomy. J. Orthop. Sci.16 (1), 38–43 (2011).
Malviya, A., Dandachli, W., Beech, Z., Bankes, M. J. & Witt, J. D. The incidence of stress fracture following peri-acetabular osteotomy: an under-reported complication. Bone Joint J.97-B (1), 24–28 (2015).
Doi, N. et al. Incidence and clinical outcome of lateral femoral cutaneous nerve injury after periacetabular osteotomy. Bone Joint J.103-B (4), 659–664 (2021).
Mei-Dan, O. et al. The CU PAO: a minimally invasive, 2-incision, interlocking periacetabular osteotomy: technique and early results. J. Bone Joint Surg. Am.101 (16), 1495–1504 (2019).
Kamachi, Y., Kinoshita, K., Sakamoto, T., Matsunaga, T. & Yamamoto, T. Bone union status of all osteotomy sites one year after curved periacetabular osteotomy based on computed tomography. Orthop. Traumatol. Surg. Res.107 (8), 102955 (2021).
Kinoshita, K. et al. Results of curved periacetabular osteotomy in patients over 60 years. Hip Joint. 34, 215–217 (2008). [in Japanese].
Kashima, N., Shiramizu, K., Nakamura, Y., Shigeaki, M. & Masatoshi, N. Biomechanical comparison of the fixation after curved periacetabular osteotomy using titanium and bioabsorbable screws. Hip Int.25 (2), 164–167 (2015).
Yasunaga, Y. et al. Rotational acetabular osteotomy in patients forty-six years of age or older comparison with younger patients. J. Bone Joint Surg. Am.85 (12), 266–272 (2003).
Tönnis, D. & Heinecke, A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J. Bone Joint Surg. Am.81 (12), 1747–1770 (1999).
Doi, K. et al. Mechanical influence of pubic nonunion on the stress distribution after curved periacetabular osteotomy: patient-specific three-dimensional finite element analysis. J. Arthroplasty. 37 (7), 1390–1395 (2022).
Casanova, M., Schindeler, A., Little, D., Müller, R. & Schneider, P. Quantitative phenotyping of bone fracture repair: a review. Bonekey Rep.3, 550 (2014).
Lerch, T. D., Steppacher, S. D., Liechti, E. F., Tannast, M. & Siebenrock, K. A. Clin. Orthop. Relat. Res.475(4), 1154–1168 doi: https://doi.org/10.1007/s11999-016-5169-5. (2017).
Tanaka, S. et al. Bone Joint J.106–B(8), 783–791 doi: https://doi.org/10.1302/0301-620X.106B8. (2024).
Acknowledgements
The authors thank Alison Sherwin, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript and Yuki Kamachi for data collection in the previous study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Koichi Kinoshita. Data collection was performed by Koichi Kinoshita, Jun Fujita, and Fumihiro Yoshimura. Analysis was performed by Koichi Kinoshita. The first draft of the manuscript was written by Koichi Kinoshita, and all authors commented on versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kinoshita, K., Fujita, J., Matsunaga, T. et al. Use of oblique view in periacetabular osteotomy and delayed postoperative weight bearing reduce delayed union in the ischium after one year. Sci Rep 14, 23720 (2024). https://doi.org/10.1038/s41598-024-75593-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-75593-w
Keywords
This article is cited by
-
Postoperative weight-bearing restrictions and rehabilitation after periacetabular osteotomy: a systematic review
Journal of Orthopaedic Surgery and Research (2025)