Abstract
To assess the response to monocular occlusion test in basic type intermittent exotropia (IXT) and to evaluate the surgical outcomes of titrated surgery based on the test’s result. Medical records were retrospectively reviewed for patients who underwent bilateral lateral rectus recession for basic type IXT. Patients were categorized into two groups: those who underwent a preoperative diagnostic monocular occlusion test (occlusion group) and those who did not (no occlusion group). In the occlusion group, patients exhibiting a change in deviation angle of ≥ 5 prism diopters (PD), either at distance or near fixation following occlusion therapy, were classified as responders, and augmented surgery was performed for patients with an increased deviation. A total of 215 patients were included in this study, with 79 patients (36.7%) in the no occlusion group and 136 patients (63.3%) in the occlusion group. In the occlusion group, while the mean distance deviation did not significantly change, the mean near deviation significantly increased from 27.2 ± 7.7 PD to 32.5 ± 8.6 PD after diagnostic monocular occlusion (p < 0.001). 58% (58%) of patients showed an increase in near deviation angle of 5 PD or more. Patients with good fusional control at near fixation were more likely to show a change in their deviation after the occlusion (odds ratio = 1.722, p = 0.028). The success rate of the strabismus surgery was significantly higher, and recurrence rate was significantly lower in the occlusion group compared to the no occlusion group (p = 0.025 and p = 0.030), while overcorrection rate was not significantly different between the two groups (p = 1.000). Over half of the patients with basic type IXT demonstrated a significant increase in near deviation angle after diagnostic monocular occlusion. Diagnostic monocular occlusion may be useful for revealing the maximum deviation angle at near fixation and may help determine the optimal surgical dosage in basic type IXT.
Similar content being viewed by others
Introduction
Intermittent exotropia (IXT) is traditionally classified into four types according to Burian’s classification system1, which is based on the difference between distance and near deviation. The choice of surgical treatment may vary considerably depending on its specific type1,2,3,4,5,6,7,8. For example, the surgical dosage for patients with pseudo divergence excess type exotropia is commonly determined based on the full distance deviation, similar to the approach in basic type IXT5. However, a more cautious strategy is recommended for true divergence excess type exotropia, such as operating for a deviation somewhere between the distance and near deviations. This is because full correction of the distance deviation may result in persistent esotropia at near9.
Diagnostic monocular occlusion test plays a critical role in classifying these types, especially in patients with a disparity between distance and near deviation1,10,11Kushner and Morton11reported that all near measurements may be contaminated by tenacious proximal fusion and should be suspended using monocular occlusion. Although previous reports have emphasized the necessity of diagnostic occlusion test for patients with divergence excess type exotropia, there has been limited study that investigated the usefulness of diagnostic monocular occlusion test in basic type IXT. Considering the effect of tenacious proximal fusion, basic type IXT may also exhibit an increased exodeviation, especially at near fixation, following monocular occlusion7.
In this study, we aim to evaluate the response to diagnostic monocular occlusion test in basic type IXT and to compare the surgical outcomes of the titrated bilateral lateral rectus (BLR) recession according to the response to occlusion with those of conventional BLR recession in basic type IXT. To the best of our knowledge, this is the first research focusing on the response to the monocular occlusion test and its impact on surgical outcomes in basic type IXT, the most common type of this disorder.
Results
Demographics
A total of 215 patients were included in this study, with 79 patients (36.7%) in the no occlusion group and 136 patients (63.3%) in the occlusion group. The clinical characteristics were not significantly different between the two groups. There were no differences of the mean angle of deviation at both distance and near between the two groups (Table 1).
Response to diagnostic monocular occlusion
In the occlusion group, the mean deviation at distance was 26.6 ± 7.4 prism diopters (PD) before occlusion and 26.5 ± 7.4 PD after occlusion, which was not significantly different after diagnostic monocular occlusion (p = 0.860). However, the mean deviation at near was 27.2 ± 7.7 PD before occlusion and 32.5 ± 8.6 PD after occlusion, which was significantly larger after diagnostic monocular occlusion (p < 0.001) (Fig. 1).
Changes in angle of deviation at distance and near after the diagnostic monocular occlusion test. The angle of deviation at distance showed no significant change after monocular occlusion test (26.6 ± 7.4 PD vs. 26.5 ± 7.4 PD, p = 0.860), whereas angle of deviation at near significantly increased from 27.2 ± 7.7 PD to 32.5 ± 8.6 PD after monocular occlusion test (p < 0.001).
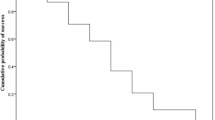
Ninety-nine out of 136 patients (72.8%) showed a change in the angle of deviation of 5 PD or more at distance or near fixation after diagnostic monocular occlusion and were classified as responders. Among these, 25 patients (18.4%) showed an increase of 5 PD or more in their distance deviation, and 79 patients (58.1%) showed an increase of 5 PD or more in their near deviation. In 20 patients (14.7%), both distance and near deviation increased. Twenty-three patients (16.9%) showed a decrease of 5 PD or more in their distance deviation, and 11 patients (8.1%) showed a decrease of 5 PD or more in the near deviation. In 7 patients (5.1%), both distance and near deviation decreased after diagnostic monocular occlusion (Fig. 2).
Response to diagnostic monocular occlusion. The distance deviation angle significantly (5 PD or more) increased in 25 patients (18.4%) and significantly decreased in 23 patients (16.9%). The near deviation angle significantly increased in 79 patients (58.1%) and significantly decreased in 11 patients (8.1%).
Conversion of the type
Of the 99 patients who were classified as responders, 36 patients (36.4%) showed an increase in near deviation by 10 or more PD compared to distance deviation, leading to a conversion to convergence insufficiency type exotropia. Among these patients who were finally diagnosed with convergence insufficiency type exotropia following occlusion test, 34 patients (94.4%) showed significant increase in their near angle of deviation and 2 patients (5.6%) showed significant decrease in their distance angle of deviation, leading to a change of their type of exotropia. There were no patients who changed to divergence excess type exotropia after occlusion.
Surgical outcomes
The occlusion group had a significantly higher success rate and a lower recurrence rate compared to the no occlusion group (p = 0.025 and p = 0.030, respectively). The rate of overcorrection did not differ significantly between the two groups (p = 1.000). Total amount of LR recession was 12.3 ± 2.1 mm in the no occlusion group and 13.0 ± 2.4 mm in the occlusion group with the titrated surgery, which was significantly greater in the latter (p = 0.042). The postoperative deviation at near and distance were not significantly different between the two groups (Table 2).
Subgroup analysis of surgical outcome
Ninety-nine out of 136 patients (72.8%) were classified as responders. At 12 months after surgery, responders demonstrated a significantly higher success rate and a lower recurrence rate compared to the no occlusion group (p = 0.012 and p = 0.014). The overcorrection rate was not higher in the responder group (p = 1.000). There were no significant differences in the success rate, recurrence rate, and overcorrection rate between the non-responder group and the no occlusion group (all p > 0.05). The amount of LR recession was greater in responders compared to no occlusion group (13.3 ± 2.4 mm vs. 12.3 ± 2.1 mm, p = 0.002), while the amount of LR recession in non-responders was not different from no occlusion group (11.9 ± 2.1 vs. 12.3 ± 2.1, p = 0.293) (Table 2).
Factors related to the significant response after diagnostic monocular occlusion
In univariate analyses, age (odds ratio = 1.258, p = 0.031) and good fusional control at near (odds ratio = 1.789, p = 0.016) were significant factors associated with significant change of 5 PD or more after diagnostic monocular occlusion. In multivariate analyses, only good fusional control at near (odds ratio = 1.722, p = 0.028) showed significant association. Gender, refractive error, distance deviation, and near deviation were not significantly associated with significant response after diagnostic monocular occlusion (Table 3).
Discussion
The results of this study provide important insights for clinical practice in treating patients with IXT, particularly those with basic type. First, after diagnostic monocular occlusion, over half of the patients exhibited a change of 5 PD or more in the angle of near deviation, and a considerable number of patients were reclassified to convergence insufficiency type exotropia. Second, augmented BLR recession based on the response to preoperative monocular occlusion resulted in better surgical outcomes without increasing the risk of overcorrection. Third, older patients and those with good fusional control at near fixation are more likely to show a significant change in their angle of deviation following monocular occlusion. Diagnostic monocular occlusion is useful in revealing the maximum angle of deviation and may assist in determining the optimal target angle for surgery.
Diagnostic monocular occlusion is commonly used to classify types of IXT, especially to differentiate between true and pseudo-divergence excess type exotropia by disrupting tonic fusional convergence1,11,12. There have been studies demonstrating that monocular occlusion can increase the deviation angle at distance and near fixation in IXT. However, we were unable to find a report investigating the response to diagnostic monocular occlusion in cases of basic type IXT.
In this study, we found that the mean distance deviation did not change significantly after diagnostic monocular occlusion. However, the mean near deviation showed a significant increase after monocular occlusion in basic type IXT. BLR recession was performed based on the average between distance and near deviation for patients with an increased deviation in the occlusion group whereas BLR recession was conducted based solely on the distance deviation in the no occlusion group. The surgical success rate was significantly higher, and recurrence rate was significantly lower in the occlusion group compared to the no occlusion group, while overcorrection rate was not significantly different between the two groups. According to subgroup analysis, the surgical dosage was greater, success rate was higher, and the recurrence rate was lower in the responder group (≥ 5 change in PD after occlusion). We believe that the higher success rate may be attributed to two factors: firstly, the use of the diagnostic monocular occlusion to reveal the maximum angle of deviation, and secondly, administration of an augmented surgical dosage to responders.
The features and mechanism of distance-near disparity observed in patients with IXT of divergence excess type have been extensively studied. It is believed that superimposed over-convergence on the basic exodeviation is the underlying mechanism11,13,14. However, scant research has conducted on the superimposed convergence mechanism in basic type IXT. We found tonic fusional convergence at near fixation in a considerable proportion of patients with basic type IXT. We believe that apparent ‘basic pattern’ shown in this subset of basic type IXT is attributed to the canceling of insufficient convergence for near fixation by superimposed tonic fusional convergence. Yang et al. used the term “masked CI type exotropia” for this type of IXT in their study analyzing the surgical outcomes of convergence insufficiency type exotropia7. Afterward, the term “masked CI type exotropia” has occasionally been used, especially in cases when the difference between distance and near deviation is less than 10 PD, but the near deviation increases to be 10 PD greater than the distance deviation after monocular occlusion15,16. In our study, among patients with basic type IXT, about a quarter exhibited this type as well, and we think that this term appropriately describes the underlying mechanism of this subtype of IXT.
Several studies have shown that monocular occlusion can increase the deviation angle at distance and near fixation in IXT. Gurlu and Erda10reported that after 1 h of diagnostic occlusion test, the mean distance deviation angle increased from 28.4 PD to 30.0 PD, and the mean near deviation angle increased from 25.7 PD to 31.2 PD. Han et al17. found that 1 day of monocular occlusion increased distant angle in 14%, and near angle in 31% of patients. Jung et al18. reported that 6.5% and 35.5% of patients showed an increase of 5 PD or more in both distance and near fixation after monocular occlusion in IXT encompassing all type of patients. In this study, we found that the mean distance deviation did not change significantly after diagnostic monocular occlusion. The proportion of patients who showed an increase in distance deviation (18.4%) was similar to that of patients who showed a decrease in distance deviation (16.9%). This change in distance deviation, observed in a small portion of patients, is possibly attributed to the normal variability of deviation angle in IXT or potential measurement errors. However, the mean near deviation showed a significant increase, rising from 27.2 ± 7.7 PD to 32.5 ± 8.6 PD after occlusion, and 58.1% of the basic type IXT patients showed an increase of 5 PD or more in their near deviation after monocular occlusion. Our study clearly demonstrates an increase in near deviation angle after monocular occlusion in substantial proportion of basic type IXT, while the tendency of greater response to monocular occlusion at near has been shown in previous studies that included all types of IXT10,18.
Few studies have investigated the factors affecting the response to diagnostic monocular occlusion in patients with IXT. Jung et al18. reported that near deviation increased after occlusion in patients with a small maximum angle of near deviation and fewer visits. In our study, neither distance nor near deviation was a significant factor influencing changes following monocular occlusion. In contrast to Jung’s work that included all types of IXT, our study focused on patients with basic type IXT. The differing patient groups may explain the varying result between the two studies. Shin and Kim19 evaluated the association between the level of control and change in ocular deviation after the monocular occlusion and reported that patients showing good control were more likely to manifest an increase in the ocular deviation. In our study, patients exhibiting good fusional control at near showed significant increase in their exodeviation after occlusion. This aligns with previous findings, suggesting that patients with better control may possess stronger tonic fusional convergence. Age was a significant factor in univariate analysis but not in multivariate analysis, indicating that its impact is less than fusional control when considered with other variables.
This study has several limitations. First, due to its retrospective nature, the treatment options were not randomized. Diagnostic monocular occlusion for basic type IXT commenced in June 2018; thus, patients in the no occlusion group were recruited prior to May 2018, while those in the occlusion group were recruited from June 2018 onward. However, all surgeries were performed by a single experienced surgeon (YHL) using the same surgical table and consistent surgical technique. Second, the minimum required follow-up period after surgery was 12 months, which may be insufficient for fully evaluating the long-term success rates of IXT surgery. Third, patients with mild anisometropia, which could potentially influence the surgical outcomes, were included in this study. However, there was no significant difference in the number of anisometropic patients between the two groups, and we believe this factor did not have a significant impact on the difference in surgical outcomes between the groups. Fourth, the wide 95% CI range for fusional control at near in the logistic regression analysis suggests relatively lower precision and may be the statistical limitation of this study.
In conclusion, after diagnostic monocular occlusion, over half of the patients with basic type IXT demonstrated a significant increase in near deviation angle. This finding indicates the presence of tonic fusional convergence in substantial proportion of these patients. The tonic fusional convergence is more likely to be present in patients with good fusional control. Consequently, diagnostic monocular occlusion is beneficial in revealing the maximum angle of deviation at near even in basic type IXT patients. This approach may help determine the optimal surgical dose, resulting in improved surgical outcomes.
Methods
Patients
A retrospective review of medical records was performed on 215 consecutive patients of age 3 to 16 who underwent BLR recession for basic type exotropia between January 2016 and July 2021 by a single experienced surgeon (Y.H.L). The difference between near and distance angle of exodeviation was within 10 PD in all patients, which was confirmed by repeated examinations before monocular occlusion. Patients were divided into two groups according to whether diagnostic monocular occlusion was performed or not: (1) No occlusion group: patients who underwent surgery without diagnostic monocular occlusion test, (2) Occlusion group: patients who underwent surgery considering the results of diagnostic monocular occlusion test. Since preoperative diagnostic monocular occlusion for basic type IXT was performed from June 2018, patients in the no occlusion group were recruited before the end of May 2018, while patients in the occlusion group were recruited from June 2018. Patients with history of prior strabismus surgery, paralytic or restrictive strabismus, congenital anomaly, or neurologic disorders were excluded. Patients with A or V pattern dissociated vertical deviation, vertical deviation > 5 PD, oblique muscle overaction that required surgery or moderate to severe amblyopia were also excluded. The study protocol was approved by the Institutional Review Board of Chungnam National University Hospital (IRB No. CNUH 2022-11-011) and adhered to the tenets of the Declaration of Helsinki. The obtaining informed patient consent was waived due to the retrospective nature of the study.
Ophthalmic examination
The deviation angle was measured by prism and alternate cover testing with accommodative targets for fixation at near (1/3 m) and distance fixation (6 m). An additional measurement of deviation angle was obtained after 1 h of monocular occlusion of the habitually deviating eye in the occlusion group. In cases of alternating strabismus, the monocular occlusion test was performed on the right eye. The deviation angle was quantified using the prism alternating cover test. Patients exhibiting a change in deviation angle of ≥ 5 PD, either at distance or near fixation following occlusion test, were classified as responders. Fusional control was evaluated through repeated examinations of the cover-uncover test and categorized into three levels: good (manifest deviation only appears after cover test and fusion is quickly reestablished without blinking or refixation), fair (the patient needs to blink or refixate to control the deviation after it is disrupted by covering) and poor (manifest deviation occurs spontaneously in the office without any fusion disruption)20. Refractive errors were analyzed as spherical equivalent obtained using cycloplegic refraction. Anisometropia was defined as a spherical equivalent difference of > 1.50 diopters (D) between two eyes. Mild amblyopia was defined as a difference of ≥ 2 lines between monocular best corrected visual acuities (BCVA), whereas BCVA in the worse eye was > 20/40 (logMAR 0.3). Moderate amblyopia was defined as a BCVA ranging from 20/40 to 20/80 (0.3 to 0.6 in logMAR) and severe amblyopia was defined as a BCVA ranging from 20/100 to 20/400 (0.7 to 1.3 in logMAR) in the worse eye. An A-pattern was defined as an increase of ≥ 10 PD of exodeviation at down gaze compared with up gaze, and V pattern was defined as an increase of ≥ 15 PD of exodeviation at up gaze compared with down gaze.
Surgical procedures
All surgeries were performed under general anesthesia by a single experienced surgeon (YHL). Following a conjunctival incision, the muscle was disinserted, recessed, and sutured directly to the globe. Surgical doses were based on the Parks’ recommendation21. In the no occlusion group, BLR recession was done based on distance deviation. In the occlusion group, BLR recession was performed based on the average deviation between distance and near deviation for patients with an increased deviation. For patients with a decreased deviation, the surgery was performed based on the pre-occlusion distance deviation angle.
Postoperative measurements
Postoperative angle of deviation at near and distance was assessed at 12 months after surgery. A successful surgical outcome was defined as exodeviation of ≤ 10 PD or esodeviation of ≤ 5 PD at distance fixation. Exodeviation of > 10 PD was defined as recurrence, and esodeviation of > 5 PD was defined as overcorrection. Patients with diplopia due to consecutive esotropia managed with alternating full-time patching for 1 to 4 weeks until diplopia resolved. If the significant esotropia persisted beyond 4 weeks, base-out prism glasses were prescribed.
Statistical analysis
Statistical analysis was conducted with SPSS for Window version 22.0 (SPSS Inc, Chicago, Illinois, USA). The student’s t-test, chi-square test, and Fisher’s exact test were employed to compare the patients’ characteristics and surgical outcomes. Logistic regression analysis was employed to identify the factors affecting the significant increase after diagnostic monocular occlusion. A p-values of < 0.05 was deemed statistically significant.
Data availability
Data is provided within the supplementary information files.
References
Burian, H. M. Exodeviations: their classification, diagnosis and treatment. Am. J. Ophthalmol. 62 (6), 1161–1166 (1966).
Burian, H. M. & Spivey, B. E. The surgical management of exodeviations. Am. J. Ophthalmol. 59, 603–620 (1965).
Kushner, B. J. Selective surgery for intermittent exotropia based on distance/near differences. Arch. Ophthalmol. 116 (3), 324–328 (1998).
Mohney, B. G. et al. Three-year observation of children 3 to 5 years of age with untreated intermittent exotropia. Ophthalmology 126(9), 1249–1260 (2019).
Chia, A., Seenyen, L. & Long, Q. B. Surgical experiences with two-muscle surgery for the treatment of intermittent exotropia. J. Aapos. 10 (3), 206–211 (2006).
Choi, M. Y., Hyung, S. M. & Hwang, J. M. Unilateral recession-resection in children with exotropia of the convergence insufficiency type. Eye (Lond.) 21 (3), 344–347 (2007).
Yang, H. K. & Hwang, J. M. Surgical outcomes in convergence insufficiency-type exotropia. Ophthalmology 118 (8), 1512–1517 (2011).
Farid, M. F. & Abdelbaset, E. A. Surgical outcomes of three different surgical techniques for treatment of convergence insufficiency intermittent exotropia. Eye (Lond.) 32 (4), 693–700 (2018).
Wright, K. W. Exotropia. In Handbook of Pediatric Strabismus and Amblyopia. (eds Wright, K. W., Spiegel, P. H. & Thompson, L. S.) (Springer, 2006).
Gürlü, V. P. & Erda, N. Diagnostic occlusion test in intermittent exotropia. J. Aapos. 12 (5), 504–506 (2008).
Kushner, B. J. & Morton, G. V. Distance/near differences in intermittent exotropia. Arch. Ophthalmol. 116 (4), 478–486 (1998).
RG. S. The Oculorotary Muscles. 2nd ed. St Louis: Mosby-Year Book. (1952).
Kenneth, W., Wright, Y. & Ning, J. Strube. Pediatric Ophthalmology and Strabismus 3rd edn (Oxford University Press, 2012).
Kushner, B. J. Exotropic deviations: a functional classification and approach to treatment. Am. Orthopt J. 38, 81–93 (1988).
Chun, B. Y., Oh, J. H. & Choi, H. J. Comparison of surgical outcomes of slanted procedure for exotropia with convergence insufficiency according to their response to preoperative monocular occlusion. Sci. Rep. 10 (1), 7261 (2020).
Farid, M. F. & Abdelbaset, E. A. Surgical outcomes of three different surgical techniques for treatment of convergence insufficiency intermittent exotropia. Eye (Load.) 32 (4), 693–700 (2018).
Han, J. M., Yang, H. K. & Hwang, J. M. Efficacy of diagnostic monocular occlusion in revealing the maximum angle of exodeviation. Br. J. Ophthalmol. 98 (11), 1570–1574 (2014).
Jung, E. H., Kim, S. J. & Yu, Y. S. Comparison of the characteristics of patients with intermittent exotropia according to response to diagnostic monocular occlusion. Jpn J. Ophthalmol. 62 (2), 243–248 (2018).
Shin, J. & Kim, W. J. Changes in Exodeviation after the monocular occlusion test in adult patients with intermittent Exotropia and its Association with the level of control. Korean J. Ophthalmol. 34 (6), 485–490 (2020).
Rosenbaum, A. L. & Stathacopoulos, R. A. Subjective and objective criteria for recommending surgery in intermittent exotropia. Am. Orthoptic J. 42, 46–51 (1992).
Parks, M. M. Duane’s clinical ophthalmology. Vol. 1. In: Tasman W, Jeager EA, editors. Concomitant exodeviations. Philadelphia: Lippincott; p. 12.) (2000).
Author information
Authors and Affiliations
Contributions
Design and conduct of the study (J.Y.S., Y.H.L.); Collection of data (J.Y.S., H.W.L., Y.H.L.); Analysis and interpretation of data (J.Y.S., H.W.L., Y.H.L.); Writing the article (J.Y.S., Y.H.L.); Critical revision of the article (J.Y.S., H.W.L., Y.H.L.); Final approval of the article (J.Y.S., H.W.L., Y.H.L.)
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sung, J.Y., Lee, H.W. & Lee, YH. The role of diagnostic monocular occlusion test in basic type intermittent exotropia. Sci Rep 14, 26013 (2024). https://doi.org/10.1038/s41598-024-77213-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-77213-z