Abstract
Surgical site infections (SSIs) pose significant challenges in surgical care, impacting patient recovery and healthcare costs. The increasing prevalence of antibiotic-resistant bacteria necessitates effective antimicrobial strategies. This study assesses the therapeutic efficacy and safety of Cefoperazone Sodium and Sulbactam Sodium in managing SSIs and compares its effectiveness against a standard treatment. A retrospective analysis was conducted on 110 patients with clinically and microbiologically confirmed SSIs from December 2020 to December 2023. Patients were divided into two groups: 55 received Cefoperazone Sodium and Sulbactam Sodium, while 55 were treated with Cefuroxime. The efficacy was evaluated based on microbiological eradication and clinical improvement, assessed after 3 days of treatment. Statistical analyses were performed using SPSS version 27.0, with significance set at p < 0.05. Demographic and clinical characteristics showed no significant differences between groups, ensuring comparability. The observation group demonstrated a cure rate of 58.18% and an overall efficacy rate of 94.55%. In contrast, the control group showed a cure rate of 32.73% and an overall efficacy rate of 70.91%. Statistical analysis revealed a significant difference in therapeutic success between the groups (Chi-square value of 9.16, p-value < 0.05). The combination of Cefoperazone Sodium and Sulbactam Sodium could provide a more effective option for managing SSIs, potentially improving cure rates and overall treatment outcomes compared to Cefuroxime.
Similar content being viewed by others
Introduction
In the complex landscape of surgical medicine, the occurrence of surgical site infections (SSIs) presents a significant obstacle to patient recuperation, contributing to elevated healthcare expenditures and influencing the overall success of surgical interventions. These infections, predominantly instigated by a heterogeneous group of pathogenic microorganisms, are capable of extending hospitalization durations, necessitating further surgical procedures, and in extreme instances, escalating the risk of morbidity and mortality1,2. Consequently, the management of SSIs is an essential facet of postoperative care, demanding the adoption of efficacious antimicrobial measures to counteract their detrimental impacts.
The administration of antibiotic therapy is pivotal in the treatment of SSIs, with the selection of the appropriate antibiotic being paramount in achieving therapeutic success3. Within this framework, the amalgamation of Cefoperazone Sodium and Sulbactam Sodium has emerged as a noteworthy option due to its extensive antibacterial properties, especially against microbes that exhibit resistance to traditional antibiotics4,5. Cefoperazone, classified as a third-generation cephalosporin, is distinguished by its robust effectiveness against an expansive spectrum of Gram-positive and Gram-negative bacteria6. Nonetheless, the predicament of bacterial resistance, particularly the synthesis of beta-lactamases capable of deactivating cephalosporins, necessitates the incorporation of beta-lactamase inhibitors such as Sulbactam7,8. Although Sulbactam lacks significant antimicrobial prowess on its own, its conjunction with beta-lactam antibiotics like Cefoperazone amplifies their antibacterial range by obstructing beta-lactamase, thereby bolstering their action against beta-lactamase producing strains9.
The synergistic alliance between Cefoperazone Sodium and Sulbactam Sodium presents a potent therapeutic avenue for addressing SSIs, potentially encompassing a vast array of pathogens, inclusive of those resistant to alternative antibiotics10. This combined methodology not only targets a diverse collection of bacterial pathogens but also confronts the escalating dilemma of antibiotic resistance, a matter of increasing concern within the medical fraternity11. In light of the formidable challenge posed by antibiotic resistance in surgical environments, the findings of this investigation could markedly affect the protocols for managing postoperative infections. We hypothesize that the combination of Cefoperazone Sodium and Sulbactam Sodium is more effective in managing SSIs compared to Cefuroxime, resulting in higher cure rates and improved overall treatment efficacy. This study aims to evaluate the therapeutic efficacy of Cefoperazone Sodium and Sulbactam Sodium in treating patients with SSIs, compared to a standard treatment with Cefuroxime. By providing empirical data on treatment outcomes, this research aims to determine whether this combination offers a more effective therapeutic option for enhancing infection management and improving post-surgical patient outcomes.
Methods
Study design
A comprehensive retrospective analysis was undertaken at our institution to evaluate the therapeutic effectiveness of Cefoperazone Sodium and Sulbactam Sodium in the treatment of SSIs. This study spanned from December 2020 through December 2023, encompassing a cohort of 146 patients assessed for eligibility. The following exclusions were made: Not meeting inclusion criteria (n = 18), Severe comorbidities (n = 10), and Declined to participate (n = 8). The final cohort included 110 patients, who developed SSIs following surgical interventions and were subsequently included in the analysis. Of these, 55 patients who received a combined regimen of Cefoperazone Sodium and Sulbactam Sodium for their SSIs were categorized into the case group for the purpose of this investigation (Fig. 1). To facilitate a robust comparative analysis and assess the therapeutic efficacy of Cefoperazone Sodium and Sulbactam Sodium, it was essential to use a consistent treatment protocol for the control group. The control group comprised 55 patients from the same study period who were administered Cefuroxime to ensure baseline comparability between the two cohorts. This antibiotic was selected based on the collective judgment of our surgical team. This decision took into account individual patient characteristics, such as surgical history, type of wound, and potential allergies. Cefuroxime was chosen as a standardized treatment to ensure consistency across the control group and to minimize variability.
Informed consent
was obtained from all subjects and/or their legal guardian(s) via telephone. The study design, objectives, and methodologies were thoroughly examined and approved by the Institutional Ethics Committee of Zhumadian Central Hospital (2023-K147). Every procedure was executed in adherence to the pertinent protocols and laws. This study’s design, execution, and reporting adhered precisely to the ethical principles delineated in the Declaration of Helsinki, which govern medical research involving human subjects. To safeguard the privacy of participants, all personal identifiers were eliminated prior to analysis and replaced with unique numeric IDs, and the data was treated with strict confidentiality.
Inclusion and exclusion criteria
Inclusion criteria:
-
1.
Diagnosis: All participants were required to have a clinically and microbiologically confirmed diagnosis of SSI, which inherently excluded patients receiving only empirical antibiotic treatment. This ensures that only patients with definitive evidence of infection are included, eliminating ambiguity related to diagnosis.
-
2.
Surgical History: Only patients who underwent surgical procedures within the study hospital between December 2020 and December 2023 and subsequently developed SSIs were considered. This criterion ensures consistency in surgical procedures, postoperative care, and hospital environment.
-
3.
Consent: Participants must have provided written informed consent, indicating their willingness to participate in the study.
Exclusion criteria:
-
1.
Pre-existing Infections: Patients with evidence of wound infection prior to the surgical intervention were excluded to ensure that only postoperative infections were studied, thus focusing on the therapeutic impact on SSIs.
-
2.
Allergy History: Individuals with a documented history of hypersensitivity or allergic reactions to Cefoperazone, Sulbactam, Cefotaxime, or any beta-lactam antibiotics were not eligible.
-
3.
Concurrent Antibiotic Therapy: Patients receiving other systemic antibiotic treatments at the time of infection diagnosis were excluded to prevent confounding effects on therapeutic efficacy assessment. This criterion was set to avoid adverse reactions that could interfere with the assessment of treatment efficacy and patient safety.
-
4.
Severe Comorbidities: Patients with severe comorbid conditions such as end-stage renal disease, hepatic failure, uncontrolled diabetes, chronic obstructive pulmonary disease, congestive heart failure, and immunosuppressive conditions which could independently affect wound healing and infection resolution, were excluded. This criterion was intended to minimize confounding variables that might obscure the efficacy of the antibiotic treatment by impacting wound healing outcomes independently.
Diagnostic criteria for surgical site infections
The diagnosis of SSIs requires an integrated evaluation that combines clinical signs, laboratory data, and microbiological evidence. Key clinical indicators include fever with a body temperature exceeding 38 °C (100.4 °F), along with localized symptoms at the wound site such as tenderness, redness, swelling, and warmth, all of which suggest an inflammatory response. Additionally, the observation of wound dehiscence or purulent exudate during clinical examinations or surgical interventions points towards infection. A critical diagnostic step involves the extraction of purulent material from the wound’s deeper layers, typically via percutaneous aspiration, which directly signifies the presence of an infection. Confirmatory evidence comes from microbiological cultures, where the isolation of pathogenic organisms from wound secretions or aspirated fluids not only confirms the infection but also aids in tailoring the antimicrobial treatment, ensuring that therapy is directed against the specific pathogens identified12. Prior to obtaining microbiological reports, patients in the case group were treated with Cefoperazone Sodium and Sulbactam Sodium, while patients in the control group received Cefuroxime. This approach ensured that initial management was standardized across groups.
Evaluation criteria for therapeutic outcomes
In the assessment of therapeutic outcomes, the criteria for evaluating efficacy were categorized as follows: Non-Responsive: If, after 3 days of treatment, microbiological assessments reveal the persistence of pathogens, coupled with no significant alteration in clinical symptoms, the treatment is deemed ineffective. Effective: A treatment is considered effective if, subsequent to 3 days of therapy, microbiological evaluations demonstrate the eradication of pathogens, with the patient exhibiting no adverse reactions at the incision site and a mitigation of complicating symptoms. Cured: The designation of ‘cured’ is applied when, after 3 days post-treatment, the patient experiences no notable pain at the wound site, no complications arise, and microbiological tests confirm the absence of pathogenic organisms.
Statistical analysis
Statistical analyses were performed using SPSS version 27.0. Descriptive statistics were used to summarize demographic and clinical characteristics. Quantitative variables, such as age, were expressed as mean ± standard deviation (SD) and compared between groups using an independent samples t-test, with variance homogeneity assessed by Levene’s test. Within-group comparisons were conducted using paired samples t-tests to evaluate changes before and after treatment. Categorical variables, such as surgery type and treatment outcomes, were expressed as frequencies and percentages, and compared using Chi-square tests. The overall efficacy rates between the control and observation groups were also compared using Chi-square analysis. All hypothesis testing was two-tailed, and a p-value of less than 0.05 was considered indicative of statistical significance.
Results
Demographic and clinical characteristics of study participants
In the study, 110 participants were divided into control and observation groups, each comprising 55 individuals with a balanced gender distribution and a similar age range. The control group, with ages ranging from 42 to 65 years (mean age 51.37 ± 6.08), included 28 gastrointestinal surgeries, 10 orthopedic surgeries, 6 urological surgeries, 6 neurosurgical procedures, and 5 thoracic-cardiovascular surgeries. The observation group, with participants aged 43 to 67 years (mean age 52.53 ± 8.82), underwent 29 gastrointestinal surgeries, 9 orthopedic surgeries, 7 urological surgeries, 5 neurosurgical procedures, and 5 thoracic-cardiovascular surgeries. Statistical comparison of demographic and surgical details between the groups showed no significant differences (P > 0.05), indicating that the groups were comparable and suitable for further analysis of treatment outcomes (Table 1).
3.2 Efficacy of Cefoperazone Sodium and Sulbactam Sodium in treatment outcomes
The study’s analysis, focusing on the efficacy of treatment regimens, demonstrated a significant disparity in outcomes between the observation group, treated with Cefoperazone Sodium and Sulbactam Sodium, and the control group. Within the observation group of 55 patients, the regimen resulted in a cure rate of 58.18%, with an additional 36.36% of cases deemed effectively treated, leading to a marginal non-responsiveness rate of 5.45%. Consequently, the comprehensive efficacy rate for this cohort reached 94.55%. In contrast, the control group, which did not receive this specific treatment combination, exhibited a cure rate of only 32.73%, with 38.18% of cases effectively treated and a significantly higher non-responsiveness rate of 29.09%, culminating in an overall efficacy rate of 70.91% (Table 2). Statistical evaluation through the Chi-square test underscored the significant difference in therapeutic success, with a calculated value of 9.16 and a p-value below 0.05. This statistically significant difference highlights the enhanced effectiveness of the Cefoperazone Sodium and Sulbactam Sodium combination in managing the studied conditions.
Discussion
The management of SSIs remains a critical challenge in surgical care, significantly impacting patient recovery, healthcare costs, and overall clinical outcomes. The emergence of antibiotic-resistant bacteria further complicates this issue, necessitating the exploration of effective antimicrobial strategies13,14. In this context, the combination of Cefoperazone Sodium and Sulbactam Sodium presents a promising therapeutic approach, leveraging the broad-spectrum antibacterial properties of Cefoperazone, a third-generation cephalosporin, in conjunction with the beta-lactamase inhibitory function of Sulbactam. This study’s focus on assessing the therapeutic efficacy of the Cefoperazone-Sulbactam regimen in managing SSIs is timely and relevant, given the increasing prevalence of resistant pathogens in surgical settings15,16. The rationale behind combining Cefoperazone with Sulbactam stems from the need to extend the antibiotic’s spectrum of activity against beta-lactamase producing bacteria, a common resistance mechanism that undermines the effectiveness of many cephalosporins. The findings of this study highlight a significant disparity in treatment outcomes between the observation group, treated with a combination of Cefoperazone Sodium and Sulbactam Sodium, and the control group. The observation group demonstrated markedly higher cure and overall efficacy rates, a result that underscores the effectiveness of this antibiotic regimen.
Cefoperazone Sodium, a third-generation cephalosporin, is renowned for its broad-spectrum antibacterial activity, which encompasses a wide array of Gram-positive and Gram-negative bacteria. Its mechanism of action involves inhibiting bacterial cell wall synthesis, a critical component in bacterial proliferation and infection sustainability. On the other hand, Sulbactam Sodium is a beta-lactamase inhibitor that, although not possessing significant antimicrobial activity on its own, significantly extends the spectrum of beta-lactam antibiotics like Cefoperazone by inhibiting the beta-lactamase enzymes produced by resistant bacteria17,18. This synergistic combination effectively counters the defense mechanisms of resistant bacterial strains, thereby enhancing the antibacterial efficacy of the treatment. The improved treatment outcomes observed in the observation group can be attributed to several pharmacodynamic and pharmacokinetic properties of the Cefoperazone-Sulbactam combination. Firstly, the broad-spectrum activity of Cefoperazone ensures coverage against a diverse array of pathogens commonly implicated in SSIs, including those resistant to standard antibiotics. The addition of Sulbactam enhances this effect by neutralizing the beta-lactamase enzymes, thus preventing the inactivation of Cefoperazone and allowing it to exert its bactericidal effects more effectively. Furthermore, the pharmacokinetic profile of this combination, characterized by optimal absorption and penetration into tissues, ensures adequate drug concentrations at the site of infection, which is crucial for the successful eradication of pathogens19,20. The prolonged half-life of Cefoperazone also facilitates sustained antibacterial activity, reducing the likelihood of bacterial survival and subsequent infection persistence.
The demographic and clinical characteristics of the study participants, including age range, gender distribution, and types of surgery, showed no statistically significant differences between the control and observation groups (p > 0.05), supporting the validity of the comparative analysis. The balanced characteristics between the groups, as shown in Table 1, reduce the likelihood of confounding factors influencing the treatment outcomes. This statistical evidence ensures that the observed differences in efficacy rates can be primarily attributed to the intervention itself, rather than inherent disparities between the groups. The balanced distribution of surgical types and the similar age and gender profiles ensure that the observed differences in treatment outcomes can be attributed with confidence to the therapeutic regimens rather than confounding variables. It is also essential to consider the role of patient adherence to the treatment regimen and the potential impact of hospital-acquired infections, which could influence the outcomes. The controlled setting of this study and the standardized postoperative care protocols likely mitigated these factors, thus highlighting the intrinsic efficacy of the antibiotic regimen. The marked difference in cure rates and overall efficacy between the observation and control groups suggests the potential of the Cefoperazone-Sulbactam combination as a more effective treatment option for SSIs.
A small sample size can limit the generalizability of study results, as it may not fully represent the target population’s diversity, potentially introducing bias. Additionally, small sample sizes increase the risk of Type II errors, meaning significant differences may go undetected. Despite these limitations, our study achieved sufficient statistical power to detect significant differences between treatment groups. The observed difference in treatment efficacy (χ² = 9.16, p < 0.05) between Cefoperazone Sodium/Sulbactam Sodium and Cefuroxime demonstrates that the sample size, though limited, was adequate to reveal clinically meaningful effects. The significant effect size indicates the robustness of our findings, supporting the validity of our conclusions even with a smaller cohort. The study aimed to assess the efficacy of Cefoperazone Sodium and Sulbactam Sodium in managing SSIs, regardless of surgical type. While the incidence of wound infections differs significantly among various surgeries (e.g., higher rates in digestive surgeries vs. neurosurgical procedures), the underlying management principles for SSIs remain consistent. Including diverse surgical interventions allows for a broader evaluation of the antibiotic regimen’s effectiveness, thus enhancing the external validity of our findings. Although this approach introduces heterogeneity, it provides insights into the real-world applicability of the treatment across different surgical contexts.
One limitation of this study is its retrospective design, which inherently restricts the control over variables and potential biases in patient selection and data collection. The confined setting and sample size may not fully represent the broader patient population, limiting the generalizability of the findings. Additionally, the study’s focus on a specific antibiotic regimen may overlook the potential efficacy of alternative treatments or combination therapies. The absence of long-term follow-up also constrains the assessment of sustained efficacy and the emergence of resistance. These factors collectively underscore the need for prospective, randomized controlled trials to validate the findings and enhance the understanding of the therapeutic efficacy of Cefoperazone Sodium and Sulbactam Sodium in managing SSIs.
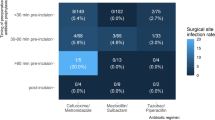
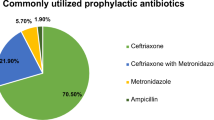
Moving forward, we plan to address the heterogeneity of surgical interventions by conducting more detailed subgroup analyses, which will provide insights into the specific effects of the treatment regimen across different surgical contexts. Furthermore, future studies will involve larger sample sizes and a more standardized approach to comorbidity categorization, thereby refining our methodology. The prospective work by Sheikh et al.21,22,23,24 on intraoperative antibiotic monitoring and optimized prophylactic regimens offers valuable insights for enhancing postoperative infection management. Incorporating these approaches, along with prospective, randomized controlled trials, will be essential to validate our findings and optimize the use of Cefoperazone Sodium and Sulbactam Sodium in managing SSIs.
Conclusion
The utilization of Cefoperazone Sodium and Sulbactam Sodium in treating patients with SSIs has been demonstrated to effectively control infections and enhance cure rates. This therapeutic approach offers a promising avenue for improving patient outcomes in post-surgical care, underscoring its potential as a valuable addition to infection management strategies.
Data availability
The datasets generated and/or analyzed during this study are available from the corresponding author upon reasonable request.
References
Seidel, D. & Bunse, J. <ArticleTitle Language=“En”>[Postoperative wound infections: diagnosis, classification and treatment]. Chirurg. 88 (5), 385–394 (2017).
Kolasiński, W. Surgical site infections - review of current knowledge, methods of prevention. Pol. Przegl Chir. 91 (4), 41–47 (2018).
Dhole, S., Mahakalkar, C., Kshirsagar, S. & Bhargava, A. Antibiotic Prophylaxis in Surgery: Current Insights and Future Directions for Surgical Site Infection Prevention. Cureus. 15 (10), e47858 (2023).
Martinez-Sobalvarro, J. V. et al. Antimicrobial stewardship for surgical antibiotic prophylaxis and surgical site infections: a systematic review. Int. J. Clin. Pharm. 44 (2), 301–319 (2022).
Bashaw, M. A. & Keister, K. J. Perioperative Strategies for Surgical Site Infection Prevention. Aorn j. 109 (1), 68–78 (2019).
Arumugham, V. B., Gujarathi, R. & Cascella, M. Third-Generation Cephalosporins. In: StatPearls. edn. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; (2024).
Ku, Y. H. & Yu, W. L. Cefoperazone/sulbactam: New composites against multiresistant gram negative bacteria? Infect. Genet. Evol. 88, 104707 (2021).
Shah, M. Q. et al. Surgical Site Infection In Orthopaedic Implants And Its Common Bacteria With Their Sensitivities To Antibiotics, In Open Reduction Internal Fixation. J. Ayub Med. Coll. Abbottabad. 29 (1), 50–53 (2017).
Geroulanos, S., Marathias, K., Kriaras, J. & Kadas, B. Cephalosporins in surgical prophylaxis. J. Chemother. 13 (Spec 1(1)), 23–26 (2001).
Huang, C., Lin, L. & Kuo, S. Comparing the Outcomes of Cefoperazone/Sulbactam-Based and Non-Cefoperazone/Sulbactam-Based Therapeutic Regimens in Patients with Multiresistant Acinetobacter baumannii Infections—A Meta-Analysis. Antibiotics. 13 (9), 907 (2024).
Basu, S. & Garg, S. Antibiotic prescribing behavior among physicians: ethical challenges in resource-poor settings. J. Med. Ethics Hist. Med. 11, 5 (2018).
Ban, K. A. et al. American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, 2016 Update. J. Am. Coll. Surg. 224 (1), 59–74 (2017).
Chen, A. F. & Brown, G. A. Management of Surgical Site Infections. J. Am. Acad. Orthop. Surg. 28 (6), e238–e241 (2020).
Bath, M. F., Davies, J., Suresh, R. & Machesney, M. R. Surgical site infections: a scoping review on current intraoperative prevention measures. Ann. R Coll. Surg. Engl. 104 (8), 571–576 (2022).
Jones, R. N. & Wojeski, W. V. Single-dose cephalosporin prophylaxis of 929 surgical procedures in a prepaid group practice: a prospective, randomized comparison of cefoperazone and cefotaxime. Diagn. Microbiol. Infect. Dis. 6 (4), 323–334 (1987).
Rowe-Jones, D. C. et al. Single dose cefotaxime plus metronidazole versus three dose cefuroxime plus metronidazole as prophylaxis against wound infection in colorectal surgery: multicentre prospective randomised study. Bmj. 300 (6716), 18–22 (1990).
Lai, C. C., Chen, C. C., Lu, Y. C., Chuang, Y. C. & Tang, H. J. In vitro activity of cefoperazone and cefoperazone-sulbactam against carbapenem-resistant Acinetobacter baumannii and Pseudomonas aeruginosa. Infect. Drug Resist. 12, 25–29 (2019).
Yang, F. et al. Diminished Susceptibility to Cefoperazone/Sulbactam and Piperacillin/Tazobactam in Enterobacteriaceae Due to Narrow-Spectrum β-Lactamases as Well as Omp Mutation. Pol. J. Microbiol. 71 (2), 251–256 (2022).
Toewiwat, N., Whangsuk, W., Ploypradith, P., Mongkolsuk, S. & Loprasert, S. Cefoperazone induces esterase B expression by EstR and esterase B enhances cefoperazone activity at the periplasm. Int. J. Med. Microbiol. 310 (2), 151396 (2020).
Brogden, R. N. et al. Cefoperazone: A review of its in vitro antimicrobial activity, pharmacological properties and therapeutic efficacy. Drugs. 22 (6), 423–460 (1981).
Sheikh, S., Swapnil, K., Tripathi, C. D., Meshram, G. G. & Karim, B. A. Intra-operative drug level monitoring of pre-operative antibiotic for surgical prophylaxis in the patients of elective spinal surgery. J. Basic. Clin. Physiol. Pharmacol. 34 (6), 797–804 (2023).
Sheikh, S. et al. Antibiotic point prevalence survey at a tertiary healthcare hospital in India: Identifying strategies to improve the antibiotic stewardship program immediately after a COVID-19 wave. Infect. Prev. Pract. 4 (4), 100253 (2022).
Salim, S. et al. Pharmacological evaluation of prophylactic anti-microbial use in laparoscopic cholecystectomy; an open labelled study evaluating the concentrations of single dose intravenous ceftriaxone at serum and tissue level. Eur. J. Clin. Pharmacol. 77 (7), 1011–1016 (2021).
Sheikh, S., Malik, N. K. & Karim, B. A. Antibiotic prophylaxis and surgical site infections; a prospective open label study to clinically evaluate the serum and tissue concentration of single dose prophylactic ceftriaxone in laparoscopic cholecystectomy. Eur. J. Clin. Pharmacol. (2020). https://doi.org/10.1007/s00228-020-02940-x
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ling Zhai.Data curation: Ling Zhai.Formal analysis: Ling Zhai and Peipei Wang.Methodology: Ling Zhai and Peipei Wang.Resources: Ling Zhai.Software: Ling Zhai and Peipei Wang.Writing – original draft: Ling Zhai.Writing – review & editing: Ling Zhai.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was conducted in accordance with the guidelines of the Zhumadian Central Hospital’s Ethics Committee (approval number: 2023-K147). For studies involving human participants, all procedures adhered to the ethical standards of the relevant national and institutional research committees, as well as the 1964 Helsinki Declaration and its subsequent amendments, or equivalent ethical standards. Informed consent was obtained from all individual participants or their legal guardians prior to their involvement in the study.
Consent for publication
Informed consent was obtained from all participants and/or their legal guardians. Consent for the publication of data was also provided by the patients and/or their families involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhai, L., Wang, P. Assessing the therapeutic efficacy of Cefoperazone Sodium and Sulbactam Sodium in managing surgical site infections: a retrospective analysis. Sci Rep 14, 27164 (2024). https://doi.org/10.1038/s41598-024-77906-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-77906-5