Abstract
The molecular profile of paracancerous tissue has been reported to be prognostic for recurrence in patients with different cancers. This study investigated the clinical significance of the protein expression of gamma-butyrobetaine hydroxylase 1 (BBOX1) in tumor and paracancerous tissues of hepatocellular carcinoma (HCC) patients. This study assessed the role of BBOX1 mRNA in tumor and paracancerous tissues in HCC via bioinformatics analysis. The protein levels of BBOX1 in paired tumor and paracancerous tissues from 83 HCC patients were determined by immunohistochemistry. The associations among BBOX1 protein levels, clinicopathological characteristics and the survival probability of HCC patients were also analyzed. The results revealed that BBOX1 mRNA expression was significantly lower in HCC tissues than in noncancerous tissues. HCC patients with low BBOX1 mRNA expression had a significantly poorer overall survival than those with high BBOX1 expression did. Immunohistochemical analysis of BBOX1 protein expression further confirmed that its levels were markedly lower in HCC tissues than in paracancerous tissues. High BBOX1 expression in paracancerous tissues correlated with poor overall survival and disease-free survival in HCC patients. These findings suggest that the paracancerous BBOX1 expression might be a credible indicator for overall survival or disease-free survival in HCC patients.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, accounting for a significant burden of cancer-related morbidity and mortality worldwide1. Despite advancements in diagnosis and treatment modalities, the prognosis for HCC patients remains poor, primarily due to high rates of tumor recurrence and metastasis2. Therefore, there is an urgent need to identify reliable prognostic markers that can accurately predict the clinical outcomes of HCC patients.
Most existing HCC studies have focused on tumor tissues, whereas paracancerous tissues are usually used as controls and are rarely studied in depth. Paracancerous tissues, which refer to the non-cancerous tissues adjacent to the tumor, have emerged as critical components in tumor development and progression. It has been increasingly recognized that paracancerous tissues play active roles in facilitating tumor growth and metastasis, creating a favorable microenvironment for tumor cells3. A recent study revealed the molecular features associated with the clinical characteristics of paracancerous tissues in HCC patients and the potential role of proteins in these tissues in the immune microenvironment remodeling of tumors or tumor recurrence4. The molecular alterations that occur in paracancerous tissues have been shown to have prognostic value in various malignancies, highlighting their potential as clinically relevant biomarkers5.
The development and progression of tumors are influenced by a multitude of factors. One significant aspect of tumor biology is the energy metabolism within the organism6. Fat metabolism, in particular, plays a crucial role as a primary source of energy, with fatty acids being oxidized in the mitochondria to generate ATP. Numerous enzymes are involved in the regulation of lipid metabolism, and the proper expression of genes encoding these enzymes may be closely linked to tumorigenesis7. Alterations in the metabolic pathways associated with fat metabolism could therefore have profound implications for the onset and progression of cancer, underscoring the need to delve into the mechanistic relationships between these metabolic processes and tumor biology to identify potential therapeutic targets8. Gamma-butyrobetaine hydroxylase 1 (BBOX1) is a critical enzyme that catalyzes the conversion ofγ- butyl betaine to L-carnitine, which is an essential substance for the transport of active fatty acids across mitochondrial membranes during mitochondrial oxidation9. The levels of betaine and propionyl carnitine in serum could be used as biomarkers along with alpha-fetoprotein to distinguish chronic hepatitis, cirrhosis, and liver cancer10. Several reports have suggested that BBOX1 might be dysregulated in several types of cancer and contribute to tumorigenesis and tumor progression. Previous studies have shown that BBOX1 is a therapeutic target in triple-negative breast cancer11, and that CRIP1 (cysteine-rich protein 1) might promote stemness in HCC by suppressing BBOX1-mediated carnitine metabolism12. These results suggest that BBOX1 is likely to exhibit oncogene-like effects and play different roles in various aspects of malignant tumors, such as metastasis.
Current research highlights the complex interplay between genetics and biochemistry in the pathogenesis of hepatocellular carcinoma (HCC)13. This interaction is not limited to cancerous tissues but is also significantly relevant in adjacent non-cancerous liver tissues. Understanding these interconnections is crucial, as the molecular processes occurring in the surrounding liver tissues can influence tumor development and progression. However, the clinical significance of BBOX1 expression in paracancerous tissues with respect to HCC prognosis remains poorly understood. Investigating the role of BBOX1 in paracancerous tissues could provide insights into the underlying mechanisms involved in tumor progression and metastasis in HCC. Moreover, examining the clinical implications of BBOX1 expression in both tumor and paracancerous tissues may offer valuable prognostic information to guide management and treatment decisions for HCC patients. Therefore, this study aimed to comprehensively evaluate the clinical significance of BBOX1 protein expression in tumor and paracancerous tissues of HCC patients. Exploration of the relationships among BBOX1 expression, clinicopathological features, and its potential as a prognostic marker could contribute to the development of personalized therapeutic strategies for HCC patients. Unraveling the functional role of BBOX1 could identify novel therapeutic targets to improve patient outcomes in HCC. Furthermore, this study would help to understand how molecular processes in surrounding liver tissues can influence tumor initiation and progression. This comprehensive perspective of considering tumor and paracancerous tissues in HCC research might lead to more effective therapeutic strategies and interventions.
Results
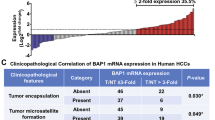
BBOX1 mRNA expression in HCC
According to the TCGA and GTEx databases, the mRNA expression levels of BBOX1 were significantly lower in HCC tissues than in normal liver tissues (Fig. 1a). Additionally, BBOX1 mRNA levels were markedly lower in HCC tissues than in paired paracancerous (PC) tissues (Fig. 1b). To evaluate the prognostic significance of BBOX1 expression in HCC patients, Kaplan-Meier survival analysis was performed. The patients were classified into two distinct groups on basis of the median mRNA expression levels of BBOX1 in tumor tissues. The results demonstrated that HCC patients with low BBOX1 expression had a significantly poorer overall survival (OS) than those with high BBOX1 expression (P < 0.05) (Fig. 1c). However, no significant correlation was detected between the mRNA expression level of BBOX1 in tumor tissues and disease-free survival (DFS) in HCC patients.
Differential expression and survival analysis of BBOX1 gene in HCC. (a) Box-plot showed differences in mRNA levels of BBOX1 between normal liver tissues (n = 160) and HCC tumor tissues (n = 371) in TCGA and GTEx databases. (b) The BBOX1 mRNA level was significantly lower in HCC tissue than in the paired paracancerous (PC) tissue (n = 50). (c) HCC patients with low BBOX1 mRNA levels in HCC, compared to those with high BBOX1 mRNA levels, had a significantly poorer overall survival.
Immunohistochemical analysis of BBOX1 in HCC
In this study, immunohistochemical analysis was performed to evaluate the protein expression level of BBOX1 in HCC tumor and paired paracancerous tissues via a tissue microarray comprising cancer and adjacent noncancerous tissues from 83 patients with hepatocellular carcinoma (Fig. 2a). Figure 2b shows two examples of the expression pattern of BBOX1 in paracancerous tissues, and Fig. 2c shows two examples of the expression pattern of BBOX1 in cancerous tissues. The intensity and distribution of BBOX1 staining were evaluated and the IHC score was calculated. The results indicated that the protein expression levels of BBOX1 were markedly lower in HCC tissues than in paracancerous tissues (Fig. 2d).
Immunohistochemical analysis of BBOX1 in HCC. (a) IHC images of BBOX1 protein expression in tumor and paired paracancerous (PC) tissues from the 83 HCC patients. (b) Two examples of the expression pattern of BBOX1 in the paracancerous tissues. (c) Two examples of the expression pattern of BBOX1 in the cancerous tissues. (d) The BBOX1 protein level was significantly lower in HCC tissue than in the paired PC tissue.
Association of BBOX1 protein expression with clinical characteristics
The associations between the expression levels of the BBOX1 protein and various clinicopathological parameters of HCC patients were explored in this study, utilizing tumor and paracancerous tissue samples from the 83 HCC patients. The 83 patients were divided into two group according to medial BBOX1 protein expression level. The results revealed that there was no correlation between BBOX1 protein levels in HCC tissues and TNM stages. However, high BBOX1 protein levels in paracancerous tissues were related to invasion depth (P = 0.044) and distant metastasis (P = 0.030) in HCC patients. Moreover, the results demonstrated that higher levels of BBOX1 protein expression in paracancerous tissues were significantly associated with advanced tumor stage (P = 0.042) and BCLC (Barcelona Clinic Liver Cancer)-stage B + C + D disease (P = 0.022) (Table 1).
Prognostic value of BBOX1 protein expression in HCC patients
To assess the prognostic value of BBOX1 protein expression in HCC, Kaplan-Meier survival analysis was performed via immunohistochemical analysis of BBOX1 in the 83 HCC patients. HCC patients with high levels of BBOX1 protein in tumor tissues had a favorable overall survival (OS) prognosis (Fig. 3a). These findings suggest a potential protective role of BBOX1 in HCC progression and indicate its potential as a positive prognostic marker. A contrasting pattern was revealed in patients with high levels of BBOX1 protein in paracancerous tissues. These patients had significantly worse OS (HR = 2.16, P = 0.004) and disease-free survival (DFS) (HR = 1.76, P = 0.049) than those with BBOX1 in paracancerous tissues (Fig. 3b and c). These findings suggest that elevated BBOX1 protein levels in paracancerous tissues may indicate a poor prognosis for HCC patients. The identification of BBOX1 as an independent prognostic factor for HCC highlights the complex nature of this disease. The time-dependent ROC (Receiver Operating Characteristic) curve analysis results indicate the following performance over different time horizons: the 1-year AUC (Area Under Curve) is 0.649, the 2-year AUC is 0.655, and the 5-year AUC is 0.638. These values suggest that the model’s ability to discriminate between outcomes is relatively stable (Fig. 3d). The C-index (Concordance Index) analysis results, using age, BBOX1 protein level in paracancerous tissue, and TNM stage as variables, are presented as a line plot showing the C-index values over time. The 1-year C-index is 0.781, the 2-year C-index is 0.793, and the 5-year C-index is 0.798. These results indicate that the model’s discriminatory power improves slightly over time, with a progressive increase in the C-index values from 1 to 5 years, reflecting better prediction accuracy as the follow-up period extends (Fig. 3e). A nomogram was developed for HCC patients based on variables such as age, BBOX1 protein level in paracancerous tissue, TNM stage, and overall survival (OS) data. This nomogram integrates these factors to create a new prognostic model, offering a visual tool for predicting patient outcomes (Fig. 3f). A comprehensive understanding of the molecular mechanisms underlying HCC progression and the potential utility of BBOX1 as a biomarker for patient stratification and personalized treatment approaches are emphasized.
Prognostic value of BBOX1 protein expression in HCC patients. (a) HCC patients with low BBOX1 protein levels in HCC tissues had significantly poorer overall survival. (b) Kaplan-Meier curve showed overall survival of HCC patients between low- and high-protein levels of BBOX1 in PC tissues. (c) Kaplan-Meier curve showed disease-free survival of HCC patients between low- and high-protein levels of BBOX1 in PC tissues. (d) The time-dependent ROC curve analysis results of protein levels of BBOX1 in PC tissues. (e) The C-index (Concordance Index) analysis results of protein levels of BBOX1 in PC tissues. (f) A nomogram predicting is the risk of protein levels of BBOX1 in PC tissues for HCC patients.
Discussion
HCC is a relatively common malignant tumor of the digestive tract, and previous studies have demonstrated that metabolic perturbations are related to the malignant biological behavior and drug resistance of HCC14. This study comprehensively investigated the clinicopathological and prognostic significance of BBOX1 mRNA and protein levels in both tumor and paracancerous tissues. The results revealed that a high protein level of BBOX1 in paracancerous tissue was associated with poor overall and disease-free survival, which was opposite to its impact in HCC tissue on survival probability. These findings suggest that BBOX1 protein levels in tumor and paracancerous tissues demonstrate a rather opposite pattern in terms of prognostic significance.
Immunohistochemical analysis revealed significantly lower protein expression levels of BBOX1 in HCC tumor tissues than in paired paracancerous tissues. Understanding these differences is crucial for identifying potential biomarkers or therapeutic targets that can aid in the early detection and treatment of cancer15. The association analysis demonstrated intriguing correlations observed explicitly in the paracancerous tissues, highlighting the clinical relevance of the observed differential expression of BBOX1. Notably, elevated expression of BBOX1 in the paracancerous tissue was significantly associated with the advanced tumor stage, indicating the potential involvement of BBOX1 in promoting tumor growth and aggressiveness, especially in the paracancerous tissues. These findings suggest that dysregulated BBOX1 expression might disrupt critical cellular processes. The examining of gene profiles in paired tumor and normal tissues could identify molecular differences between cancerous and noncancerous tissues, which can improvee our understanding of the mechanisms underlying cancer development and progression16.
Moreover, we observed a significant correlation between BBOX1 expression and distant metastasis, specifically in the paracancerous tissues. This intriguing association highlights the role of BBOX1 in mediating tumor dissemination from paracancerous regions. Metastasis necessitates intricate molecular events such as epithelial-mesenchymal transition (EMT) and angiogenesis, which enable cancer cells to invade neighboring tissues and establish secondary tumors at distant sites17. BBOX1 is a crucial enzyme of L-carnitine metabolism. L-carnitine may play a key role in the signaling pathways involved in metastasis18, including the MAPK signaling pathway19, PPAR-γ signaling pathway20, and Wnt/β-catenin pathway21. Furthermore, we detected a significant association between high BBOX1 expression and high BCLC stage (B + C + D), specifically in paracancerous tissues. These findings highlight the clinical implications of BBOX1 as a potential biomarker for predicting disease severity and patient outcomes in patients with HCC. The identification of reliable prognostic markers is crucial for tailoring individualized treatment strategies and optimizing patient management.
The observed differential expression of BBOX1 in paracancerous tissues and its correlations with aggressive clinicopathological features raise intriguing questions regarding the functional significance of BBOX1 in HCC progression, especially in the paracancerous regions. Elucidating the underlying molecular mechanisms through which BBOX1 promotes tumor growth, metastasis, and disease progression in paracancerous tissues is critical for advancing our understanding of HCC biology. Further investigations into the specific mechanisms through which BBOX1 influences tumor progression and metastatic spread are warranted, as they could unveil novel targets for therapeutic intervention and provide a deeper understanding of the intricate biology of HCC. Moreover, changes in the abundance of binuclear hepatocytes (ABHs) in paracancerous tissues might be associated with the short-term recurrence of HCC patients after radical resection, and regular ABH expression might be useful for preventing the short-term HCC recurrence22. A comprehensive analysis of these results revealed that a high BBOX1 protein expression in paracancerous tissue was not only a biomarker, but also a contributing factor to metastasis, recurrence, and tumor progression.
In this study, the results also revealed notable differences in the prognostic value of BBOX1 protein expression between tumor and paracancerous tissues. Specifically, HCC patients with high levels of BBOX1 protein within their tumor tissues have a favorable overall survival prognosis. Contrasting results were observed when assessing BBOX1 protein levels in paracancerous tissues. Patients with high levels of BBOX1 protein in their paracancerous tissues presented significantly worse overall and disease-free survival outcomes than those with low BBOX1 expression did. This unexpected observation suggests that elevated BBOX1 levels in paracancerous tissues may serve as an indicator of poor prognosis in HCC patients. The underlying mechanisms driving this differential prognostic significance of BBOX1 in HCC and paracancerous tissues remain unclear and warrant further investigation. BBOX1 may play distinct roles in tumor cells and adjacent paracancerous cells, potentially exerting tumor-suppressive effects within the tumor but contributing to disease progression in the neighboring paracancerous microenvironment. Elucidating the intricate molecular pathways through which BBOX1 exerts its effects in both contexts is essential for unraveling its dualistic prognostic significance and therapeutic potential.
In this study, we found that high BBOX1 levels in paracancerous tissues are associated with worse overall and disease-free survival outcomes. However, there were several limitations in this study. This study was retrospective and was conducted at a single center, possibly introducing selection bias. Future multicenter studies with larger sample sizes are needed for validation. The semiquantitative nature of the immunohistochemical staining used to assess BBOX1 expression may introduce variability and standardized criteria for defining BBOX1 positivity are lacking. The incorporating of more quantitative methods could provide more precise measurements. However, functional experiments are needed to elucidate the underlying mechanisms by which BBOX1 contributes to HCC progression. Additionally, this study focused solely on the prognostic value of BBOX1 expression and its association with clinicopathological characteristics. Other factors such as treatment modalities, comorbidities, and genetic alterations should be considered in future comprehensive prognostic models. Further research is needed to evaluate the efficacy and safety of BBOX1-targeted therapies and identify potential resistance mechanisms. Addressing these limitations through future research will increase our understanding of the role of BBOX1 in HCC.
In summary, this study demonstrates the prognostic value of BBOX1 expression in HCC and highlights its potential as a therapeutic target. These findings underscore the importance of BBOX1 in HCC progression and provide a foundation for future investigations. Prospective multicenter studies, standardized criteria for BBOX1 assessment, quantitative methods, and functional experiments are needed to further validate these findings and elucidate the underlying mechanisms involved. The ability of target BBOX1 may offer a promising avenue for the development of novel therapeutic strategies for HCC, ultimately improving patient outcomes.
Methods
Public data acquisition and gene expression analysis
The RNA expression profile and clinical data for HCC were acquired from the TCGA database (The Cancer Genome Atlas) (HCC tissue: n = 374; paired paracancerous tissues: n = 50) (https://www.cancer.gov/ccg/research/genome-sequencing/tcga)23, and Genotype-Tissue Expression (GTEx) project (normal liver tissues, n = 110) (https://www.genome.gov/Funded-Programs-Projects/Genotype-Tissue-Expression-Project)24. RNAseq data in FPKM (Fragments Per Kilobase of transcript per Million mapped reads) format from the TCGA and GTEx databases were processed uniformly via the Toil process25. The limma package in R software was used to identify differentially expressed genes, including BBOX1, between tumor and normal (or paracancerous) tissues. The criteria for significance were set as a fold change ≥ 2 and an adjusted p-value < 0.05.
Clinical samples and HCC tissue microarray
This study was approved by the Ethics Committee of Bengbu Medical University (No.2020LK078), and was conducted following the ethical guidelines of the Declaration of Helsinki. All participants in this study were over the age of 18 years, and written informed consent was obtained from each participant. We are committed to protecting the privacy and personal information of our participants throughout the research process and ensuring that all procedures performed in the study adhere to the applicable ethical standards. The study included 83 patients who underwent surgical resection for HCC. Data on clinical characteristics and long-term follow-up data from April 2008 to December 2019 were collected. Formalin-fixed, paraffin-embedded tumor and paracancerous tissue samples from the 83 HCC patients were used to construct a tissue microarray (TMA). Core tissue biopsies with a diameter of 1.5 mm and a thickness of 4 μm were obtained from representative areas of each sample and arrayed into recipient TMA blocks.
Immunohistochemical staining and analysis
Immunohistochemical (IHC) analysis was applied on TMA samples according to standard protocols of streptavidin-biotin amplified complex IHC detection reagents followed by BBOX1 antibody (dilution 1:50) (sc-373774, Santa Cruz Biotechnology, US). The IHC staining intensity and distribution of BBOX1 were independently evaluated by two experienced pathologists blinded to the clinical data. The final immunoreactivity score (IHC-score) was calculated via the following formula: IHC-score = PI×I. The staining intensity (I) was scored on a scale of 0 to 3 (negative = 0, weak = 1, moderate = 2, and strong = 3). The PI indicates the percentage of positive cells among all cells.
Analysis of the correlation between BBOX1 protein levels and clinicopathological characteristics
The clinicopathological data of the 83 HCC patients included depth of invasion, lymph node metastasis, distant metastasis, TNM stage, and BCLC (Barcelona Clinic Liver Cancer) stage. According to the median expression of BBOX1, patients with HCC were further divided into two groups (low and high) to analyze the correlation between BBOX1 protein expression levels and clinicopathological features.
Analysis and evaluation of the prognostic value of BBOX1 in HCC patients
The associations between BBOX1 gene expression and overall survival (OS) or disease-free survival (DFS) in HCC patients were evaluated via the Kaplan-Meier method and log-rank test. Patients were divided into two groups on the basis of the median expression levels of BBOX1 mRNA or protein (high vs. low), and survival curves were generated accordingly. The BBOX1 mRNA expression levels and their association with patient survival data were sourced from the TCGA database. In contrast, the BBOX1 protein expression levels and their correlation with patient survival were derived from our study, which includes data from 83 HCC patients. Protein expression levels in the cancerous and paracancerous tissues of these 83 patients were measured using immunohistochemical (IHC) analysis on the tissue microarray (TMA).
Statistical analysis
All statistical analyses were conducted via R software (version 4.0.2). The measurement data between the two groups were compared by via the Wilcoxon rank sum test, or paired Student’s t-test. The “survival” and “survminer” packages were used for survival analysis. The “timeROC” package was used for time-dependent ROC curve analysis. The “pec” package was used for C-index (Concordance Index) analysis. Perform proportional hazards assumption testing and Cox regression analysis using the “survival” package, and construct and visualize nomogram models using the “rms” package. The “ggplot2” package was utilized for data visualization. The associations between BBOX1 expression and clinicopathological parameters were assessed via chi-squared tests. A p-value < 0.05 was considered statistically significant.
Data availability
Publicly available datasets were analyzed in this study, these can be found in database of The Cancer Genome Atlas (https://www.cancer.gov/ccg/research/genome-sequencing/tcga) and Genotype-Tissue Expression (GTEx) project (https://www.genome.gov/Funded-Programs-Projects/Genotype-Tissue-Expression-Project). The authors confirm that the data supporting the findings of this study are available within the article.
References
Singal, A. G., Kanwal, F. & Llovet, J. M. Global trends in hepatocellular carcinoma epidemiology: implications for screening, prevention and therapy. Nat. Rev. Clin. Oncol. https://doi.org/10.1038/s41571-023-00825-3 (2023).
Chen, Y. et al. Effect of infiltrating immune cells in tumor microenvironment on metastasis of hepatocellular carcinoma. Cell. Oncol. (Dordrecht). https://doi.org/10.1007/s13402-023-00841-6 (2023).
Aran, D. et al. Comprehensive analysis of normal adjacent to tumor transcriptomes. Nat. Commun. 8, 1077. https://doi.org/10.1038/s41467-017-01027-z (2017).
Zhu, H. et al. Proteomics of adjacent-to-tumor samples uncovers clinically relevant biological events in hepatocellular carcinoma. Natl. Sci. Rev. 10, nwad167. https://doi.org/10.1093/nsr/nwad167 (2023).
Kim, J. et al. Transcriptomes of the tumor-adjacent normal tissues are more informative than tumors in predicting recurrence in colorectal cancer patients. J. Translational Med. 21, 209. https://doi.org/10.1186/s12967-023-04053-2 (2023).
Hanahan, D. Hallmarks of cancer: new dimensions. Cancer Discov. 12, 31–46. https://doi.org/10.1158/2159-8290.Cd-21-1059 (2022).
Zhang, C. et al. New dawn for cancer cell death: emerging role of lipid metabolism. Mol. Metabolism. 63, 101529. https://doi.org/10.1016/j.molmet.2022.101529 (2022).
Butler, L. M. et al. Lipids and cancer: emerging roles in pathogenesis, diagnosis and therapeutic intervention. Adv. Drug Deliv. Rev. 159, 245–293. https://doi.org/10.1016/j.addr.2020.07.013 (2020).
Rashidi-Nezhad, A., Talebi, S., Saebnouri, H., Akrami, S. M. & Reymond, A. The effect of homozygous deletion of the BBOX1 and fibin genes on carnitine level and acyl carnitine profile. BMC Med. Genet. 15 https://doi.org/10.1186/1471-2350-15-75 (2014).
Huang, Q. et al. Metabolic characterization of hepatocellular carcinoma using nontargeted tissue metabolomics. Cancer Res. 73, 4992–5002. https://doi.org/10.1158/0008-5472.Can-13-0308 (2013).
Liao, C. et al. Identification of BBOX1 as a therapeutic target in triple-negative breast Cancer. Cancer Discov. 10, 1706–1721. https://doi.org/10.1158/2159-8290.Cd-20-0288 (2020).
Wang, J. et al. CRIP1 suppresses BBOX1-mediated carnitine metabolism to promote stemness in hepatocellular carcinoma. EMBO J. 41, e110218. https://doi.org/10.15252/embj.2021110218 (2022).
Ucdal, M., Burus, A. & Celtikci, B. Cross talk between genetics and biochemistry in the pathogenesis of hepatocellular carcinoma. Hepatol. Forum. 5, 150–160. https://doi.org/10.14744/hf.2023.2023.0028 (2024).
Cheng, X. et al. Long-chain acylcarnitines induce senescence of invariant natural killer T cells in hepatocellular carcinoma. Cancer Res. 83, 582–594. https://doi.org/10.1158/0008-5472.Can-22-2273 (2023).
de Assumpção, P. P. et al. Traps and trumps from adjacent-to-tumor samples in gastric cancer research. Chin. J. cancer Res. = Chung-kuo Yen Cheng Yen Chiu. 30, 564–567. https://doi.org/10.21147/j.issn.1000-9604.2018.05.10 (2018).
Hu, S. et al. Transcriptional response profiles of paired tumor-normal samples offer novel perspectives in pan-cancer analysis. Oncotarget. 8, 41334–41347. https://doi.org/10.18632/oncotarget.17295 (2017).
Khan, S. U., Fatima, K., Malik, F., Kalkavan, H. & Wani, A. Cancer metastasis: molecular mechanisms and clinical perspectives. Pharmacol. Ther. 250, 108522. https://doi.org/10.1016/j.pharmthera.2023.108522 (2023).
El-Ashmawy, N. E. & Khalil, R. M. A review on the role of L-carnitine in the management of tamoxifen side effects in treated women with breast cancer. Tumour Biology: J. Int. Soc. Oncodevelopmental Biology Med. 35, 2845–2855. https://doi.org/10.1007/s13277-013-1477-5 (2014).
Mansour, H. H., Kiki, E., Ibrahim, S. M., Omran, M. M. & A. B. & Effect of l-carnitine on cardiotoxicity and apoptosis induced by imatinib through PDGF/ PPARγ /MAPK pathways. Arch. Biochem. Biophys. 704, 108866. https://doi.org/10.1016/j.abb.2021.108866 (2021).
Jiang, F. et al. L-carnitine ameliorates cancer cachexia in mice partly via the carnitine palmitoyltransferase-associated PPAR-γ signaling pathway. Oncol. Res. Treat. 38, 511–516. https://doi.org/10.1159/000439550 (2015).
De Luca, A. et al. Mitochondrial biogenesis is required for the anchorage-independent survival and propagation of stem-like cancer cells. Oncotarget. 6, 14777–14795. https://doi.org/10.18632/oncotarget.4401 (2015).
Zhang, Y. et al. Attenuation of binuclear hepatocytes in the paracancerous liver tissue is associated with short-term recurrence of hepatocellular carcinoma post-radical surgery. FASEB Journal: Official Publication Federation Am. Soc. Experimental Biology. 37, e23271. https://doi.org/10.1096/fj.202301219R (2023).
Weinstein, J. N. et al. The Cancer Genome Atlas Pan-cancer analysis project. Nat. Genet. 45, 1113–1120. https://doi.org/10.1038/ng.2764 (2013).
Ferreira, P. G. et al. The effects of death and post-mortem cold ischemia on human tissue transcriptomes. Nat. Commun. 9, 490. https://doi.org/10.1038/s41467-017-02772-x (2018).
Vivian, J. et al. Toil enables reproducible, open source, big biomedical data analyses. Nat. Biotechnol. 35, 314–316. https://doi.org/10.1038/nbt.3772 (2017).
Funding
This work was supported by Anhui Provincial Natural Science Foundation (2108085MH284), Natural Science Research Project of Anhui Educational Committee (KJ2021ZD0090), and Graduate Innovation Project of Bengbu Medical University (Byycxz23001).
Author information
Authors and Affiliations
Contributions
RF and YG conceived the study and designed the experiments. RF, YZ, XD, and YZ performed bioinformatics analysis and experiments. SL and MY created the figures. RF wrote the manuscript. YG revised the manuscript. YG supervised the study. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fang, R., Zhan, Y., Dong, X. et al. High expression of BBOX1 in paracancerous tissue is associated with poor prognosis in hepatocellular carcinoma patients. Sci Rep 14, 28413 (2024). https://doi.org/10.1038/s41598-024-78127-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78127-6