Abstract
With the continuous spread of the SARS-CoV-2 globally, viral mutations have accumulated. As a result, SARS-CoV-2 became more contagious, and has a higher risk of immune escape and reinfection. To identify variants and have an awareness of the prevalence of these variants, this study selected four segments containing mutations on the S gene of the SARS-CoV-2. Then a rapid and convenient variants detection method was established using high-resolution melting(HRM) analysis combined with nested polymerase chain reaction(PCR). The total detection process takes about 5 h. Through comprehensive analysis of the results from the four reaction systems, the identification of seven important Omicron variants(BA.2, BA.2.75, BA.5.2, BF.7, BQ.1, XBB.1 and XBB.2) can be achieved, with significant differentiation in the melting curves of each variant group. The method established in this study was used to genotype positive specimens in COVID-19 nucleic acid testing, the overall concordance rate compared to whole genome sequencing results was 88.9%, and the positive concordance rate of each sublineage was greater than 80% and the negative concordance rate was greater than 94.4%. The detection of clinical specimens has demonstrated that the HRM analysis established in this study is an effective, rapid and convenient variant identification method, which can be used for monitoring SARS-CoV-2 variants and has important value in addressing public health issues caused by the ongoing mutations of the SARS-CoV-2.
Similar content being viewed by others
Introduction
Since the outbreak of COVID-19 in January 2020, the pandemic has had an unprecedented impact on the global public health system. In the past month (from 8 January to 4 February, 2024), over 503000 new cases of COVID-19 and more than 10000 new fatalities have been reported worldwide1. With the widespread transmission of the disease globally, the genetic mutations of the SARS-CoV-2 have emerged, affecting its transmissibility, pathogenicity, vaccine immune efficacy, and treatment strategies and resulting in thousands of different variants2,3,4. Multiple variants of concern (VOCs) and variants of interest (VOIs) have been designated by World Health Organization (WHO), such as B.1.1.7 (Alpha), B.1.351 (Beta), P.1 (Gamma), B.1.617.2 (Delta), and B.1.1.529 (Omicron) has been designated as variants of concern (VOCs)5, based on their observed change in epidemiology and fitness advantage. The Omicron variant was detected in November 2021 and has shown rapid growth6, and severe immune escape potential7, spreading worldwide during a short period of time. Currently, the Omicron and its sublineages are the main variants globally1. Since its emergence, the Omicron variants has continued to evolve in its genetic and antigenic properties, with an expanding range of sublineages, making it the variant with the most mutations8. The increasing mutations have led to changes in the virus’s transmissibility, resulting in higher infectivity, properties of immune escape, and risk of reinfection9,10. This has led to an increase in healthcare visits and hospitalizations, causing a significant burden on society. The emergence of unpredictable new variants also poses a potential significant risk. Therefore, strengthening the monitoring capacity of variants, timely detection of potential variants, and knowing the prevalence of variants are of great practical value in dealing with the ongoing mutations of the SARS-CoV-2, with important implications for reducing the burden of disease. In China, since the implementation of the new SARS-CoV-2 management policy in 2023, variant monitoring has also become a focus of SARS-CoV-2 infection prevention and control under the new situation.
The SARS-CoV-2 genome encodes four structural proteins, among which the spike protein is the region where the virus binds to host cells. Mutations in this structure can significantly alter the virus’s transmissibility, pathogenicity, and immunogenicity11. WHO and the guidelines from the European Centre for Disease Prevention and Control (ECDC) indicate that SARS-CoV-2 whole genome sequencing, or at least S gene sequencing, should be used to confirm variant infections12, highlighting the importance of S gene mutations in SARS-CoV-2 variants identification. Among the numerous mutations in Omicron, over 30 mutations are located in the S protein13. Different variants have formed stable genetic mutations in this region, which can serve as targets for identifying variants.
Currently, variant monitoring mainly relies on whole genome sequencing, which can obtain the complete genome sequence of the virus. Gene sequencing plays an important role in variant monitoring, epidemiological investigation, risk assessment and basic research. However, gene sequencing is costly, time-consuming and technically challenging, making it difficult to be widely implemented in grassroots laboratories and to quickly identify variants in the early stages. Therefore, there is an urgent need for a fast, simple and low-cost method for variant identification. High-resolution melting (HRM) analysis is a molecular biology technique based on the property that double-stranded DNA melts into single-stranded DNA as the temperature increases. By introducing a saturating fluorescent dye during PCR and collecting the fluorescence signals during nucleotide melting, characteristic melting curves can be obtained to reflect gene changes at single or multiple sites in the DNA chain. Currently, HRM analysis has been widely applied in medical diagnosis, microbiology, animal and plant research, food industry and other fields14,15,16. In disease-related areas, it is mainly used for genetic typing, drug resistance detection and methylation analysis17,18,19,20. This method has advantages of fast detection speed, simplicity in operation, closed-tube processing to prevent laboratory contamination, high throughput and low cost without the need for expensive reagents and consumables.
Therefore, this study aims to establish a faster, simpler and more cost-effective variant detection method using HRM analysis targeting the S gene of the SARS-CoV-2. This method will enable rapid identification and monitoring of variants in the current situation of variants emergence.
Materials and methods
Specimen source
The nucleic acid samples used in this study were obtained from positive nucleic acid detection specimens of the SARS-CoV-2 stored in our laboratory, collected from throat swabs or nasal swabs of COVID-19 patients in Chengdu from 2021 to 2023. Nucleic acid extraction was performed using the SMPE-960 automated nucleic acid extraction system (Suresh, Jiangsu, China). Prior to inclusion in the study, all samples were re-tested using real-time RT-PCR to confirm positive detection of SARS-CoV-2 nucleic acid, that Ct values less than 32.
All experiments were performed in accordance with relevant guidelines and regulations. All experimental protocols in this study were approved by Chengdu Center for Disease Control and Prevention. The informed consent for the detection of SARS-CoV-2 was obtained from all subjects at the time of sample collection.
Mutations selection
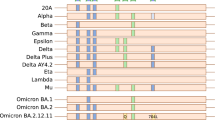
To specifically identify the Omicron variant of the SARS-CoV-2, key mutations relevant to the identification and classification of the Omicron variants were selected based on the specific mutations published by the WHO, and the shared mutations from CoVariants(CoVariants, 2024). A total of 4 gene segments, including 12 mutations, were selected as shown in Fig. 1.
Methods
Primer design
To improve the sensitivity and specificity of the method, nested PCR was used for detection. Four pairs of primers targeting the gene fragments containing the mutations were designed using Oligo7 software. To enhance HRM analysis’s resolution, the first amplification products of approximately 200 bp, while the length of the second amplification product for HRM analysis is controlled within the range of 80–120 bp, with the mutations located in the central region of the amplification product. Primers were synthesized by Sangon Biotech Co., Ltd(Shanghai, China). The design schematic of the primers and mutations are shown in Fig. 2, and the primer sequences are listed in Table 1.
Establishment of detection system
The first PCR amplification using the SuperScript III One-Step RT-PCR System with Platinum Taq DNA Polymerase kit (Invitrogen, USA). The reaction system was prepared with a total volume of 50 µl, including 25 µl 2×Reaction Mix, 2 µl Taq Mix, 1 µl of each primer (10 µM), 16 µl water, and 5 µl RNA. The reaction was performed on a Thermal Cycler PCR instrument (ABI, USA) with the following program: 45 °C for 30 min; 94 °C for 2 min; 94 °C for 15 s, 55 °C for 30 s, 68 °C for 15 s, 40 cycles; 68 °C for 5 min.
The products of the one-step PCR amplification were diluted in a gradient and 1000-fold diluted amplification products were used as templates for HRM analysis. The HRM analysis was performed using the HRM Analysis Kit (EvaGreen) (Tiangen, Beijing, China) with a reaction system volume of 20 µl, contained 10 µl 2×HRM Analysis PreMix, 0.6 µl of each primer (10 µM), 7.8 µl water, and 1 µl of the 1000-fold diluted first PCR products. The detection was carried out on a LightCycler480 II Real-Time PCR system(Roche, Switzerland) with the following program: pre-incubation at 95 °C for 2 min; amplification at 95 °C for 10 s, 60 –55 °C for 20 s (step size 1 °C), 72 °C for 30 s, 40 cycles; melting curve analysis was carried out at 95 °C for 1 min, 40 °C for 1 min, 60 °C for 1s, and melting curve generation from 60 °C to 90 °C with continuous temperature increase (RampRate 0.03 °C/s), and cooling at 40 °C for 30 s.
Analytical performance of the method
Specificity of the method: We used nucleic acids from clinical samples that tested positive for other 10 common pathogens in respiratory tract infections to test for possible cross-reactivity. The viruses include coronavirus OC43, coronavirus NL63, coronavirus HKU1, adenovirus, bocavirus, rhinovirus, influenza A virus H1N1, parainfluenza viruses 1, parainfluenza viruses 4 and respiratory syncytial virus.
Sensitivity of the method: We used the standard substance (Bdsbiotech Co., Ltd. Guangzhou, China) of SARS-CoV-2 reference isolate Wuhan-hu-1 (MN908947.3) to quantify the variant samples by realtime-PCR. The standard substance number is GBW(E)091132. For sensitivity tested, decimal serial dilutions of the quantified variant samples (BA. 2, BA. 2.75, BA. 5.2, BF. 7, BQ. 1, XBB. 1, XBB. 2) were detected by the established method.
Reproducibility of the method: In order to evaluate the reproducibility of the established detection system, two independent runs were performed on two different days.
Detection of clinical samples
The HRM detection system was applied to type 45 clinical samples, and the results were compared with those obtained from Next-generation sequencing(NGS) to evaluate the HRM analysis developed in this study.
Next-generation sequencing was performed using the Illumina sequencing system (Illumina, USA). The ULSEN® SARS-CoV-2 whole-genome capture kit (Beijing Micro-Future Technology Co., Ltd., Beijing, China) was used for reverse transcription and multiplex PCR amplification, and the library was prepared using the Illumina Nextera XT DNA Prep Kit (Illumina, USA). Genome assembly was performed with CLC Genomics Workbench (version 23.0), and the viral clades were determined by Nextclade (https://clades.nextstrain.org/). Briefly, reads with length less than 30 nucleotides were trimmed, then trimmed reads were mapped to reference sequences (accession number MN908947.3). The minimum percentage of the total alignment length and similarity was set as 60% and 80%, respectively. Local realignment were then performed to improve mapping results. Low frequency variant detection was performed to call variants. Consensus sequences were created using the neucleotides with the highest frequency, and the regions with read depth less than 30× were not used for consensus generation.
Results
Establishment of HRM detection system
Fourteen samples (1 BA.2, 1 BA.2.75, 2 BA.5.2, 2 BF.7, 6 XBB.1, 1 XBB.2, 1 BQ.1) were selected for method establishment based on accurate genotype obtained from whole-genome sequencing. The results showed that all four primer pairs can achieve good discrimination.
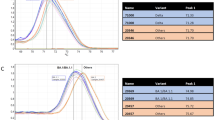
Reaction system 1: primers 210–213
This reaction system covered two mutations on the S gene. As shown in Fig. 3, through HRM analysis, the 7 variants could be differentiated into 3 groups. The groups were designated as A, B, and C, according to the Tm values in ascending order. XBB.1 and XBB.2 belonged to group A with an average Tm value of 76.15 °C. BA.2, BA.5.2, BF.7 and BQ.1 belonged to group B with an average Tm value of 76.68 °C. BA.2.75 was assigned to group C with an average Tm value of 77.38 °C. The variants within each group were significantly distinguished.
Reaction system 2: primers 252–257
This reaction system covered three mutations on the S gene. The HRM analysis results (Fig. 4) showed that the 7 variants were divided into 3 groups based on the Tm values in ascending order. BA.2.75 and XBB.1 belonged to group A with an average Tm value of 76.84 °C. BA.2, BA.5.2, BF.7 and BQ.1 belonged to group B with an average Tm value of 77.25 °C. XBB.2 belonged to group C with an average Tm value of 77.75 °C.
Reaction system 3: primers 440–460
This reaction system covered six mutations on the S gene. The HRM analysis results (Fig. 5) showed that the 7 variants were divided into 5 groups based on the Tm values in ascending order. BA.2.75 belonged to group A with an average Tm value of 72.5 °C. XBB.1 and XBB.2 belonged to group B with an average Tm value of 72.95 °C. BA.2 belonged to group C with an average Tm value of 73.07 °C. BA.5.2 and BF.7 belonged to group D with an average Tm value of 73.44 °C. BQ.1 belonged to group E with an average Tm value of 73.83 °C.
Reaction system 4: primer C1243F
The BF.7 had a specific C1243F(nucleotide mutation: G25290T) mutation in the spike protein. The HRM analysis results (Fig. 6) showed that the BF.7 could be significantly distinguished from other variants, with an average Tm value of 78.62 °C, assigned to group A. Other variants belonged to group B with an average Tm value of 79.02 °C.
HRM analysis for Omicron variants
Based on the comprehensive analysis of the results from the four reaction systems, the seven Omicron variants(BA.2, BA.2.75, BA.5, BF.7, XBB.1, XBB.2 and BQ.1)can be identified and classified. The results of HRM analysis for the seven Omicron variants are shown in Table 2. The samples that match the grouping results can be determined as the corresponding variant.
Analytical performance of the method
Specificity of the method
The established system was used to detect negative samples for SARS-CoV-2 and 10 other viruses (coronavirus OC43, coronavirus NL63, coronavirus HKU1, adenovirus, bocavirus, rhinovirus, influenza A virus H1N1, parainfluenza viruses 1, parainfluenza vi-ruses 4 and respiratory syncytial virus.), there was no effective amplification for expected HRM analysis.
Sensitivity of the method
We used the standard substance of SARS-CoV-2 reference isolate Wuhan-hu-1 (MN908947.3) to quantify the variant samples by realtime-PCR. The standard curves generated with serially diluted standard substance showed an R2 of 0.9908, with an amplification efficiency of 93%, y=-3.1975x + 42.721. The sensitivity test with quantified variant samples shows that there are differences in sensitivity among the four systems for detecting different Omicron variants (Table 3).
Reproducibility of the method
For intra-assay reproducibility test, we selected two or more samples for each variant, except for BQ.1, XBB. 2, and BA. 2.75 which had only one sample, each sample was tested twice, and consistent results were obtained for parallel samples. Two independent runs performed on two different days obtained ideal results, with significant differences in melting curve shape, and variants can be well distinguished. The average Tm value of each group fluctuates between batches, but displayed a remarkable difference between groups, without affecting the typing results.
Clinical samples detection
The above HRM analysis for Omicron variants was used to detect and identify variant strains in 45 samples with positive nucleic acid detection of SARS-CoV-2. The results were compared with the whole-genome sequencing results. The samples used during the establishment of the method were used as a reference (one of each type). Samples with melting curves clustering with the reference were determined to be of the same group.
All 45 samples were found to be Omicron variants with a coverage of ≥ 99% through Next-generation sequencing (NGS). This included 2 samples of BA.2.75, 9 samples of BA.5.2, 10 samples of BF.7, 22 samples of XBB.1, and 2 samples of XBB.2.
Using the HRM system established in this study, 2 samples of BA.2.75, 11 samples of BA.5.2, 8 samples of BF.7, 19 samples of XBB.1, and 2 samples of XBB.2 were detected. Two samples were only classified as XBB and could not be further divided into XBB.1 or XBB.2. The Next-generation sequencing results showed that both of these samples were XBB.1. Another sample only had typing results in the 252–257 system, which could be XBB.1 or BA.2.75, but the Next-generation sequencing results indicated it was an XBB.1.
Comparing the results of the HRM analysis with the Next-generation sequencing results, the overall concordance rate was 88.9%(40/45). The positive concordance rate(true positive/(true positive + false negative))and negative concordance rate(true negative/(true negative + false positive))were calculated for each variant are shown in Table 4. As there were no BA.2 and BQ.1 variants among the 45 test samples, so they could not be evaluated.
The results showed that the HRM analysis established in this study can effectively detect and identify the Omicron variants. The positive concordance rate for detecting BA.2.75, BA.5.2, BF.7, XBB.1, and XBB.2 was greater than 80%, and the negative concordance rate was greater than 94%.
Discussion
In November 2021, multiple countries around the world reported a new variant, B.1.1.529 (Omicron). On November 24th of the same year, WHO designated it as a “variant under monitoring (VUM),” and on November 26th, it was upgraded to a “variant of concern (VOC).” The Omicron lineages are also currently the predominant type in global circulation1. The seven variants included in this study are important sublineages of the Omicron variants, including BF.7 and BQ.1 as sublineages of BA.5, BA.2.75 as a sublineage of BA.2, and XBB* is recombinant of BA.2.10.1 and BA.2.75. All of these variants have been defined as VOCs by WHO5, and some sublineages of XBB.1 are still designated as VOIs at the time of submission. According to the surveillance results in China in 2023, the prevalent variant nationwide are all Omicron, with the main types being BA.5.2 and its sublineages, BF.7 and its sublineages, BA.2.75 and its sublineages, XBB and its sublineages21.
This study targeted the S gene of the SARS-CoV-2 and selected four fragments containing mutations. A rapid, convenient, and low-cost variant detection method was established using HRM analysis. The melting curve were significantly distinguishable, and by analyzing the combination of the results from the four reaction systems, the identification of seven important Omicron variants, including BA.2, BA.2.75, BA.5.2, BF.7, BQ.1, XBB.1 and XBB.2, can be achieved. The overall concordance rate compared with Next-generation sequencing results was 88.9%. For each variant, the positive concordance rate was greater than 80%, with BA.2.75, BA.5.2, and XBB.2 reaching 100%. The negative concordance rate was greater than 94.4%, with BF.7 and XBB.1 reaching 100%. Using the method established in this study, 96-well reactions can be performed at a time, and the overall detection process, takes approximately 5 h. There are fewer manual operations, requiring only two reaction mixture configurations and one product dilution. Compared with Next-generation sequencing, it is faster and more suitable for rapid screening of variants. The operation is simpler, with lower requirements for equipment, making it more suitable for promotion in laboratories with relatively limited conditions, such as laboratories at the grassroots level. This study also combined nested PCR, first using a one-step reverse transcription amplification, and then using the products of the first amplification as the template for HRM analysis. By performing two-step PCR amplification of the target gene fragment, both reverse transcription of SARS-CoV-2 RNA and improved sensitivity and specificity can be achieved. ARMS-PCR is another method for the detection of variants, which one pair of primers that can detect only one mutation, compared with the HRM detection system established in this study, a pair of primers can detect up to six mutations and distinguish five groups of variants. Compared to probe-based qPCR detection, one pair of primers can also distinguish more variants without probe design, and the method is simpler to establish. HRM can also establish multiplex reaction systems that, in one reaction system, can distinguish more variants. Prior to this study, some researchers have established a rapid detection methods for SARS-CoV-2 variants based on HRM analysis22,23,24, and successfully identified Alpha, Beta, Gamma, Delta and Omicron BA.1, BA.2, BA.3, BA.4, BA.5 lineages, etc., all of which have obtained good results, indicating that HRM is an effective method that can be used to distinguish SARS-CoV-2 variants. However, none of the above studies involved the identification of Omicron sublineages. Besides, no literature was consulted on the detection methods of the current major circulating variants XBB*, BF.7, BQ.1 and BA.2.75. Our study was reported for the first and filled the research gap.
RNA viruses may enhance the infectivity, transmissibility, or virulence of the virus due to their high mutation rate during adaptive evolution within the host25, and SARS-CoV-2 also has many key mutations that affect pathogenicity, such as D614G, which can enhance the infectivity of the virus26. Some researchers have developed rapid detection methods for these hot-spot mutations(such as D614G, N501Y), including HRM analysis27,28,29,30. However, these hot-spot mutations often exist in multiple variants and are not specific, making it difficult to identify the types of variants. This study comprehensively analyzed the mutations of the major Omicron variants and selected four gene fragments on the S gene that are meaningful for distinguishing variants. Among them, the C1243F mutation only exists in the BF.7 variant and has no interference from other variants, making it a good specific marker for identifying the BF.7 variant. The region spanning amino acids 210–213 contains two mutations on the S gene, namely the I210V (A22190G) mutation in the BA.2.75 variant and the V213E (T22200A) mutation in the XBB.1 and XBB.2 variants, which are different from the V213G (T22200G) mutation in BA.2, BA.5.2, BA.2.75, BF.7, and BQ.1. Therefore, by detecting this region, BA.2.75 can be effectively distinguished from XBB.1 and XBB.2. The region spanning 252–257 contains three variant sites on the S gene, mainly represented by the G252V (G22317T) mutation in the XBB.1 variant, the D253G (A22320G) mutation in the XBB.2 variant, and the G257S (G22331A) mutation in the BA.2.75 variant. Therefore, by detecting this gene fragment, BA.2.75, XBB.1, and XBB.2 can be well distinguished from other types. The region spanning 440–460 contains six mutations on the S gene, which provides a rich combination of mutations and can present various melting curve morphologies, enabling better distinction of most variants. However, on the other hand, due to the large number of mutations, the results are more susceptible to interference. Therefore, when interpreting the results, the amplification results of the other gene fragments should be considered for comprehensive judgment.
The clinical sample detecting results showed some inconsistencies with expectations. One sample’s genetic sequencing showed it as BF.7, but the detection result in the 210–213 reaction system established in this study was XBB, which did not match the results of several other reaction systems. However, based on the overall judgment of other primer pairs, it was determined to be BF.7. Analysis of its whole-genome sequence revealed two additional mutations, R214S (CGT-AGT) and D215G (GAT-GGT), on the basis of the V213G mutation, which made the melting curve of this specimen inconsistent with other BF.7 specimens. Therefore, the detection result in the 210–213 reaction system for this specimen is not reliable. Two other samples that were interpreted as XBB in the 252–257 system could not be able to distinguish between XBB.1 and XBB.2. Whole-genome sequencing showed that both of these specimens were XBB.1, and analysis of their whole genome sequences revealed the additional S256L (TCA-TTA) mutation, which altered the melting curve morphology and did not match the expected grouping result. Therefore, unexpected mutations in the target region may affect the detection results, but on the other hand, this may also be a way to discover new mutations.
In conclusion, the method established in this study has the advantages of being fast, simple, and cost-effective. It allows for the quick identification of some known variants, and understanding the prevalence of variants. But it does not replace the whole genome sequencing of SARS-CoV-2 to identify the virus variants. Even because the concordance rate of the established HRM technique compared to NGS is less than 95% and its not designed to detect unknown variants. But it seems to be a good methodology to reduce costs with genomic sequencing by using it as an inference method to select the most interesting samples to NGS methods. In addition, this method can only identify relatively rough lineages and cannot further divide into more specific sublineages. At the same time, this study had a small sample size, with some sublineages having no samples or insufficient sample quantities, which limits the evaluation of the method. Further expansion of the detection range is needed to obtain more accurate assessments. The rapid pace of viral mutation and the rapid succession of variants require timely updates of the included mutations in future studies to achieve the identification of new variants. Such as JN.1, which is a descendent lineage of BA.2.86 and is the most prevalent SARS-CoV-2 variant currently. JN.1 in comparison with BA.2.86 carries the additional spike mutation L455S that can be used as a detection target and can also be recognized at high speed and low cost.
Data availability
All data generated or analysed during this study are included in this published article.
References
World Health Organization. COVID-19 epidemiological update-16 https://www.who.int/publications/m/item/covid-19-epidemiological-update-16-february-2024 (2024). Accessed 26 February 2024.
Volz, E. et al. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature. 593(7858), 266–269. https://doi.org/10.1038/s41586-021-03470-x (2021).
Iacobucci, G. Covid-19: New UK variant may be linked to increased death rate, early data indicate. BMJ. https://doi.org/10.1136/bmj.n230 (2021).
Collier, D. A. et al. Sensitivity of SARS-CoV-2 B.1.1.7 to mRNA vaccine-elicited antibodies. Nature. 593(7857), 136–141. https://doi.org/10.1038/s41586-021-03412-7 (2022).
World Health Organization. Historical working definitions and primary actions for SARS-CoV-2 variants. https://www.who.int/publications/m/item/historical-working-definitions-and-primary-actions-for-sars-cov-2-variants. Accessed 23 January 2024.
Viana, R. et al. Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in southern Africa. Nature. 603(7902), 679–686. https://doi.org/10.1038/s41586-022-04411-y (2022).
Ai, J. et al. Omicron variant showed lower neutralizing sensitivity than other SARS-CoV-2 variants to immune sera elicited by vaccines after boost. Emerg. Microbes Infect. 11(1), 337–343. https://doi.org/10.1080/22221751.2021.2022440 (2022).
World Health Organization. Statement on the update of WHO’s working definitions and tracking system for SARS-CoV-2 variants of concern and variants of interest. https://www.who.int/news/item/16-03-2023-statement-on-the-update-of-who-s-working-definitions-and-tracking-system-for-sars-cov-2-variants-of-concern-and-variants-of-interest(accessed. Accessed 23 January 2024.
Sun, L. et al. Rapid Detection of Predominant SARS-CoV-2 variants using Multiplex High-Resolution Melting Analysis. Microbiol. Spectr. 11(3), e0005523. https://doi.org/10.1128/spectrum.00055-23 (2023).
Tian, D., Sun, Y., Xu, H. & Ye, Q. The emergence and epidemic characteristics of the highly mutated SARS-CoV-2 Omicron variant. J. Med. Virol. 94(6), 2376–2383. https://doi.org/10.1002/jmv.27643 (2022).
Shereen, M. A., Khan, S., Kazmi, A., Bashir, N. & Siddique, R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 24, 91–98. https://doi.org/10.1016/j.jare.2020.03.005 (2020).
European Centre for Disease Prevention and Control/World Health Organization Regional Office for Europe. Methods for the detection and identification of SARS-CoV-2 variants: second update. https://www.ecdc.europa.eu/sites/default/files/documents/Methods-for-the-detection-char-SARS-CoV-2-variants_2nd%20update_final.pdf(accessed 26 January 2024).
He, X., Hong, W., Pan, X., Lu, G. & Wei, X. SARS-CoV-2 Omicron variant: Characteristics and prevention. MedComm. 2(4), 838–845. https://doi.org/10.1002/mco2.110 (2021).
Tong, S. Y. & Giffard, P. M. Microbiological applications of high-resolution melting analysis. J. Clin. Microbiol. 50(11), 3418–3421. https://doi.org/10.1128/JCM.01709-12 (2012).
Druml, B. & Cichna-Markl, M. High resolution melting (HRM) analysis of DNA-its role and potential in food analysis. Food Chem. 158, 245–254. https://doi.org/10.1016/j.foodchem.2014.02.111 (2014).
Galuszynski, N. C. & Potts, A. J. Application of High Resolution Melt analysis (HRM) for screening haplotype variation in a non-model plant genus: Cyclopia (Honeybush). PeerJ. 8, e9187. https://doi.org/10.7717/peerj.9187 (2020).
Harrison, L. B. & Hanson, N. D. High-Resolution Melting Analysis for Rapid Detection of sequence type 131 Escherichia coli. Antimicrob. Agents Chemother. 61 (6), e00265–e00217. https://doi.org/10.1128/AAC.00265-17 (2017).
Towler, W. I. et al. Analysis of HIV diversity using a high-resolution melting assay. AIDS Res. Hum. Retroviruses. 26 (8), 913–918. https://doi.org/10.1089/aid.2009.0259 (2010).
Hashemizadeh, Z., Bazargani, A., Kalantar-Neyestanaki, D., Mohebi, S. & Hadi, N. Determining spa-type of methicillin-resistant Staphylococcus aureus (MRSA) via high-resolution melting (HRM) analysis, Shiraz, Iran. BMC Res. Notes. 13(1), 97. https://doi.org/10.1186/s13104-020-04948-z (2020).
Xiao, Z. et al. Validation of methylation-sensitive high-resolution melting (MS-HRM) for the detection of stool DNA methylation in colorectal neoplasms. Clin. Chim. Acta. 431, 154–163. https://doi.org/10.1016/j.cca.2014.01.044 (2014).
Chinese Center for Disease Control and Prevention. Epidemic situation of novel coronavirus infection in China. https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_13141/202401/t20240110_271902.html(accessed 26 January 2024).
Diotallevi, A. et al. Rapid monitoring of SARS-CoV-2 variants of concern through high-resolution melt analysis. Sci. Rep. 13(1), 21598. https://doi.org/10.1038/s41598-023-48929-1 (2023).
Koshikawa, T. & Miyoshi, H. High-resolution melting analysis to discriminate between the SARS-CoV-2 omicron variants BA.1 and BA.2. Biochem. Biophys. Rep. 31, 101306. https://doi.org/10.1016/j.bbrep.2022.101306 (2022).
Kiani, S. J. et al. High resolution melting curve analysis for rapid detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants. Acta Virol. 67(1), 91–98. https://doi.org/10.4149/av_2023_109 (2023).
Duffy, S. Why are RNA virus mutation rates so damn high? PLoS Biol. 16(8), e3000003. https://doi.org/10.1371/journal.pbio.3000003 (2018).
Korber, B. et al. Tracking changes in SARS-CoV-2 spike: Evidence that D614G increases infectivity of the COVID-19 Virus. Cell. 182(4), 812–827e19. https://doi.org/10.1016/j.cell.2020.06.043 (2020).
Miyoshi, H., Ichinohe, R. & Koshikawa, T. High-resolution melting analysis after nested PCR for the detection of SARS-CoV-2 spike protein G339D and D796Y variations. Biochem. Biophys. Res. Commun. 606, 128–134. https://doi.org/10.1016/j.bbrc.2022.03.083 (2022).
Zhong, Z. et al. An encodable multiplex microsphere-phase amplification sensing platform detects SARS-CoV-2 mutations. Biosens. Bioelectron. 203, 114032. https://doi.org/10.1016/j.bios.2022.114032 (2022).
Gazali, F. M. et al. Detection of SARS-CoV-2 spike protein D614G mutation by qPCR-HRM analysis. Heliyon. 7(9), e07936. https://doi.org/10.1016/j.heliyon.2021.e07936 (2021).
Aoki, A. et al. A modified high-resolution melting-based assay (HRM) to identify the SARS-CoV-2 N501Y variant. J. Virol. Methods. 314, 114678. https://doi.org/10.1016/j.jviromet.2023.114678 (2023).
Funding
This research was funded by the ”Key Technology Research and Development Program of the Science and Technology Department of Sichuan Province, grant number 2021YFS0064”, the”Youth Innovation Research Project by the Sichuan Medical Association, grant number Q22017”, and the”Science Foundation of the Health and Family Planning Commission of Chengdu, grant number 22056”.
Author information
Authors and Affiliations
Contributions
Conceptualization: CY, ZYZ and CH; Methodology: CY and ZYZ; Investigation: CY, ZYZ, SDY, HX and XWJ; Writing-Original Draft: CY; Writing-Review&Editing: CYZ and CH; Supervision: MJT; Project administration: CH. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cheng, Y., Zhou, Y., Chen, Y. et al. Rapid detection of the SARS-CoV-2 omicron variants based on high-resolution melting curve analysis. Sci Rep 14, 28227 (2024). https://doi.org/10.1038/s41598-024-79254-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-79254-w