Abstract
Patients with aortic root abscesses experience increased morbidity and mortality compared to those without abscess in aortic valve infective endocarditis. The superior intervention for patients with aortic root abscess is not determined. This research investigates the degree to which increased morbidity and mortality of aortic root abscess, and to describe perioperative characteristics and outcomes of root operations versus root-sparing repairs of aortic root abscess. All patients who underwent surgical treatment of active aortic valve endocarditis between 2011 and 2022 at a single institution were reviewed, yielding 218 patients, of whom 64 had perivalvular abscess. Patients were treated with either simple (root-sparing) or complex (root replacement) techniques. Patients with abscess demonstrated significantly higher rates of previous cardiac surgery, redo endocarditis surgery, aortocavitary fistula, heart block, and prosthetic valve endocarditis. One quarter of abscesses were not detected on preoperative imaging. Presence of abscess was a significant predictor of operative mortality. Prosthetic valve endocarditis was a significant predictor of complex repair in patients with abscess. Five-year survival was similar between simple and complex repair groups in patients with abscess. Aortic root abscess confers significant morbidity and mortality, and measures should be taken to ensure early detection and treatment of this condition.
Similar content being viewed by others
Introduction
Infective endocarditis is a devastating disease process with considerable impact on short- and long-term mortality in affected patients, often necessitating surgical intervention to achieve a cure. In the aortic position, the endocarditis can be limited to the valve, requiring its replacement, or in more aggressive cases, the infection may spread and necrosis can create an abscess within the aortic root. This type of infection begets more extensive debridement to clear the infection, and either reconstruction with a patch and valve replacement or total replacement of the root. Typically, patients with aortic root abscesses experience increased morbidity and mortality compared to those without abscess1. A depiction of root abscess extending beyond the aortic annulus to surrounding structures is shown in Fig. 1.
Although aortic root replacement can be done safely at specialized centers with experienced surgeons, the surgery becomes more complex and requires longer cardiopulmonary bypass times compared to a simpler repair2,3. If the infection involves enough tissue a root replacement will be required, but there still remains a certain amount of equipoise regarding the superior intervention for patients with aortic root abscess. Limited research exists to compare conservative and extensive operations in cases of aortic valve endocarditis with resulting abscess, and the perioperative factors that would drive a surgeon to select one approach over the other4. This research seeks to explore the extent of increased morbidity and mortality of aortic root abscess in cases of aortic valve infective endocarditis, and to describe perioperative characteristics and outcomes of root operations versus root-sparing repairs of aortic root abscess.
Methods
The Joint Data Analytics Team (JDAT) at our institution, a tertiary care hospital, developed a retrospective cohort database of all patients who underwent operative treatment for aortic valve endocarditis between June 2011 and April 2022 based upon diagnostic codes for infective endocarditis and CPT codes for aortic valve surgery, yielding 282 patients. Data collection was started at the introduction of electronic medical records in our health system to collect maximal data for the study. 64 patients with non-active endocarditis were excluded, which entailed patients who did not have acute infective endocarditis and those with fully treated infective endocarditis prior to surgery. We defined the fully-treated population as having all of the following criteria: clear blood cultures prior to surgery, no abscess, native valve endocarditis, greater than six weeks of antibiotics prior to surgical treatment, and no continued sequelae of infection such as fevers or emboli. If a patient did not meet the full list of criteria above, they were noted to have active endocarditis. The final cohort included 218 patients who were surgically treated for active aortic valve endocarditis. Of these patients, 64 were found to have a perivalvular abscess on preoperative imaging or intraoperatively. The power size calculation for the study suggested that 163 patients each in the abscess and non-abscess group would be necessary to detect a significant difference in mortality.
A consort diagram of the study population is shown in Fig. 2.
Demographic information, perioperative and postoperative characteristics, and follow-up information of the cohort were retrieved through manual chart review. With regards to operative technique, all surgeons thoroughly debrided the infected tissue, and thereafter a simple repair of aortic abscess was defined as aortic valve replacement (AVR), AVR + patch, and any other root-sparing technique such as aortic valve repair or vegectomy. Complex repairs were defined as those with a root procedure involved, such as Bentall, Commando, and homograft procedures.
Data from this study are not publicly available to preserve patient confidentiality. All methods were carried out in accordance with relevant guidelines and regulations. Comparison of means, logistic regression, survival analysis, and figure generation were performed in R version 4.2.3 (R Foundation for Statistical Computing). The Institutional Review Board at Yale University approved this study (IRB 2000020356), and informed consent was obtained from all subjects and/or their legal guardians. The study adhered to the Declaration of Helsinki research guidelines.
Results
Demographic characteristics and perioperative characteristics of the overall study population, categorized as abscess (n = 64) versus no abscess (n = 154), are shown in Table 1. Mean age of the entire cohort was 56.9 years, and the cohort was 81.2% male. Patients with abscess demonstrated significantly higher rates of previous cardiac surgery (59.4% vs. 30.5%, P < 0.001), redo endocarditis surgery (31.3% vs. 7.14%, P < 0.001), aortocavitary fistula (25.0% vs. 3.25%, P < 0.001), heart block (21.9% vs. 7.79%, P < 0.001), and prosthetic valve endocarditis (46.9% vs. 18.2%, P < 0.001). 23.4% of abscesses (15) were not detected on preoperative imaging with echocardiogram or CTA, and were only found intraoperatively; 10 abscesses adjacent to native valves and 5 in prosthetic valves.
Available microbiology data are noted in Table 2. Overall, the predominant organism in both the abscess and non-abscess group was alpha-hemolytic streptococci. There were no significant differences in microorganism distribution between groups. For all patients, the average duration of antibiotic treatment was 19.5 days.
Regarding surgical treatment for the cohort of 218 patients, 136 patients received aortic valve replacement (AVR), 26 received Commando or hemi-Commando, 23 received AVR + patch, 19 received Bentall, 10 received homograft, and 4 received another type of treatment such as aortic valve repair or vegectomy (Fig. 3). AVR was performed significantly more in patients with simple aortic valve endocarditis (P < 0.001), while AVR + patch and Commando were performed significantly more in patients with aortic valve abscess (both P < 0.001).
(A) Surgical treatment of patients with aortic valve endocarditis who underwent aortic valve replacement. Pink are patients with abscess, and blue are without. (B) Surgical treatment of patients with aortic valve endocarditis who underwent aortic valve replacement with patch, Bentall, Commando, homograft, or “other” root-sparing techniques (including valve repair and vegectomy). Red borders indicate statistically significant differences between abscess and non-abscess groups.
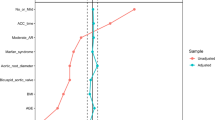
Short-term postoperative outcomes are demonstrated in Table 3. In the immediate postoperative period, prolonged ventilation occurred in 43 patients (19.7%), deep sternal infection occurred in three patients (1.38%), reoperation for bleeding in 12 patients (5.50%), reoperation for other reasons in 13 patients (5.96%), postoperative stroke in 8 patients (2 in the abscess group and 6 in the no abscess group) (3.67%), new renal failure occurred in 7 patients (3.21%), and 17 patients experienced operative mortality (7.80%). In a bivariate logistic regression analysis of postoperative outcomes, the presence of abscess was a significant predictor of operative mortality (OR 5.12, 95% CI [1.8, 14.53], P = 0.002), and when adjusted for previous cardiac surgery, redo endocarditis surgery, prosthetic valve endocarditis, presence of fistula, and presence of heart block, abscess remained a significant predictor of operative mortality (aOR 3.51, 95% CI [1.1, 11.22], P = 0.032).
With regards to long-term outcomes, 11 patients in the non-abscess group (7.1%) experienced recurrent endocarditis, with 10 undergoing redo endocarditis surgery. In the abscess group, 8 patients experienced recurrent endocarditis (12.5%) with 6 necessitating redo surgery.
Of the 64 patients with abscess, 32 underwent simple repair (AVR, AVR + patch, other), and 32 received a complex repair (Bentall, Commando, and homograft) (Table 4). In a bivariate logistic regression analysis, prosthetic valve endocarditis was found to be a significant predictor of complex repair (OR 5.62, 95% CI [1.92, 16.45], P < 0.001). 26 patients in the abscess cohort had their abscess size measured either on imaging (CT or echocardiography) or intraoperatively, with an average maximal diameter of 19.8 mm (SD ± 12.4) (Fig. 4). Of these patients, 12 had simple repairs (mean diameter 17.5 mm, SD ± 12.4) and 14 went on to have complex repairs (mean diameter 21.9 mm, SD ± 12.9). An unpaired t-test did not show a significant difference in abscess size between simple and complex repair groups (P = 0.391).
Boxplot of size of abscess in simple (root-sparing) and complex repair groups, as measured either on preoperative imaging or intraoperatively. Mean maximal diameter: 19.8 mm (SD ± 12.4) (Fig. 3). Simple repairs group: mean diameter 17.5 mm (SD ± 12.4), complex repairs group: mean diameter 21.9 mm (SD ± 12.9), p = 0.391.
A Kaplan-Meier analysis was performed to compare survival with simple or complex repairs in patients with abscess (Fig. 5). At six months, the simple repairs group exhibited 90.6% survival, while complex showed 75.0% survival. At five years, survival in the simple repair group was 74.7% compared to 71.9% in the complex repairs group. This survival difference was not statistically significant by log rank test (P = 0.4). Redo surgery for endocarditis occurred in 7/64 patients, with 4/7 in the simple repairs group and 3/7 in the complex repairs group.
Discussion
This study aimed to confirm the increased morbidity and mortality of aortic root abscess in cases of aortic valve endocarditis, and to describe perioperative characteristics and outcomes of simple compared to complex repairs of aortic root abscess to assist in operative decision making.
In our cohort, we noted that patients with abscess were significantly more likely to have extensive disease, as demonstrated by higher rates of aortocavitary fistula and heart block. Patients with prosthetic valves also exhibited higher rates of abscess, likely correlating with the difficulty of treating infected graft material with antibiotics as compared to native tissue5. Furthermore, abscess was also seen at higher rates in patients who had undergone previous cardiac surgery and redo endocarditis surgery. Notably, a quarter of patients with aortic root abscess were not diagnosed preoperatively and the discovery of abscess was only made intraoperatively. Given the increased morbidity and mortality associated with aortic root abscess, thorough preoperative imaging is warranted in patients with some of the qualities listed above to ensure expeditious surgical treatment if abscess is noted.
As expected, many more operations involving the aortic root were performed for patients with root abscess compared to those without. In the situations where patients without abscess underwent root replacement, the operation was necessitated by a dilated or aneurysmal aortic root. Our study confirmed findings of increased short-term mortality among patients with abscess3, although other short-term outcomes were not significantly different between groups.
We also attempted to characterize the population of patients who require a root replacement procedure for aortic valve endocarditis with abscess compared to a less aggressive approach. Among patients with abscess, patients who ended up with a complex repair were significantly more likely to have prosthetic valve endocarditis. Since microorganisms tend to seed prosthetic material and form a biofilm to inhibit the native immune response, their lingering presence at the annular level can cause tissue necrosis and more extensive abscess despite antibiotic treatment6. Prosthetic valve endocarditis has been known to lead to complete root destruction7. In order to eradicate the abscess and any signs of infections in these cases, root replacement may be warranted. For the subset of patients who had their abscess measured on preoperative imaging or intraoperatively, those who went on to receive a complex repair demonstrated an abscess size more than 4 mm larger than those with a simple repair. Although not significant in our analysis, this trend indicates that smaller abscesses may be successfully treated without an extensive operation.
In survival analysis, we noted an initial survival advantage in those who underwent simple repair, although survival between the groups began to approximate one another over time. It is likely that some of the patients requiring complex repair had a more extensive infection necessitating the complex repair in the first place, and may have commensurately been more ill preoperatively. It has been established that patients who are critically ill preoperatively may have worse postoperative outcomes8, and this may explain the initially poorer short-term mortality of patients with abscess. Besides early mortality in the complex repair group, mid-term survival in both groups was similar to or better than reports in other studies1,9.
Limitations
This study was limited by its single-center, retrospective nature. Some of the analyses may have been better served with a larger sample size to prevent against Type II error. Nevertheless, the odds ratios noted in logistic regression analyses were large and were representative of stark differences between groups in the data, and the study still provides meaningful information regarding disease patterns of aortic endocarditis, the significant morbidity and mortality seen in aortic valve abscess, and the options for surgical management.
Conclusion
In this study, we sought to confirm the increased morbidity and mortality associated with aortic root abscesses in patients with aortic valve infective endocarditis and investigate some of the properties that contribute to a patient receiving a root replacement versus a root-sparing procedure. We noticed greater odds of mortality in patients with aortic root abscesses, and remarked that prosthetic valve endocarditis and abscess size could contribute to selection of a complex repair in patients with aortic root abscesses. Further research should focus on improved detection of abscesses on preoperative imaging and exploring other factors that could contribute to poor outcomes in patients with abscess, such as time from diagnosis to surgery.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to restriction from the Institutional Review Board in order to protect patient privacy. Data are available from the corresponding author for researchers who meet the criteria for access to confidential data.
Change history
26 January 2025
The original online version of this Article was revised: In the original version of this Article, the Acknowledgements were inadvertently added as Supplementary Information file. The Acknowledgements now appear in the main article and the Supplementary Information file has been removed.
References
Yang, B. et al. Root abscess in the setting of infectious endocarditis: short- and long-term outcomes. J. Thorac. Cardiovasc. Surg. 162 (4), 1049–1059e1. https://doi.org/10.1016/j.jtcvs.2019.12.140 (2021).
Malaisrie, S. C. et al. Valve-sparing versus valve-replacing aortic root replacement in patients with aortic root aneurysm. J. Card Surg. 37 (7), 1947–1956. https://doi.org/10.1111/jocs.16473 (2022).
Leontyev, S. et al. Early and late outcomes of complex aortic root surgery in patients with aortic root abscesses†. Eur. J. Cardiothorac. Surg. 49 (2), 447–455. https://doi.org/10.1093/ejcts/ezv138 (2016).
Yoshioka, D. et al. Recent Surgical results for active endocarditis complicated with Perivalvular Abscess. Circ. J. 81 (11), 1721–1729. https://doi.org/10.1253/circj.CJ-17-0355 (2017).
Habib, G. et al. 2015 ESC guidelines for the management of infective endocarditis: the Task Force for the management of infective endocarditis of the European Society of Cardiology (ESC)endorsed by: European Association for Cardio-thoracic surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 36 (44), 3075–3128. https://doi.org/10.1093/eurheartj/ehv319 (2015).
Nataloni, M. et al. Prosthetic valve endocarditis. J. Cardiovasc. Med. 11 (12), 869. https://doi.org/10.2459/JCM.0b013e328336ec9a (2010).
Musci, M. et al. Homograft aortic root replacement in native or prosthetic active infective endocarditis: twenty-year single-center experience. J. Thorac. Cardiovasc. Surg. 139 (3), 665–673. https://doi.org/10.1016/j.jtcvs.2009.07.026 (2010).
Barge-Caballero, E. et al. Preoperative INTERMACS profiles determine postoperative outcomes in critically ill patients undergoing Emergency Heart Transplantation. Circ. Heart Fail. 6 (4), 763–772. https://doi.org/10.1161/CIRCHEARTFAILURE.112.000237 (2013).
Sultan, I. et al. Aortic root replacement with cryopreserved homograft for infective endocarditis in the modern North American opioid epidemic. J. Thorac. Cardiovasc. Surg. 157 (1), 45–50. https://doi.org/10.1016/j.jtcvs.2018.05.050 (2019).
Acknowledgements
Thank you to Sophia Xiao for drawing the graphical abstract of the manuscript.
Author information
Authors and Affiliations
Contributions
ED: conception/design, acquisition/analysis/interpretation of data, drafting, AM: conception/design, acquisition of data, revision. SUBM: conception/design, acquisition of data, revision. SR: conception/design, revision. AA: conception/design, revision. RA: conception/design, revision. PV: conception/design, revision, AG: conception/design, revision.
Corresponding author
Ethics declarations
Competing interests
PV is a consultant for Medtronic Aortic Inc and Terumo Aortic Inc. AG is a consultant for Medtronic Strategic Surgical Advisory Board and Edwards Lifesciences. AA is a consultant for JOMDD. All other authors have no competing financial interests to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Degife, E., Morrison, A., Mahmood, S.B.U. et al. Surgical treatment and outcomes in aortic valve endocarditis and perivalvular abscesses. Sci Rep 14, 29373 (2024). https://doi.org/10.1038/s41598-024-79256-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-79256-8