Abstract
The health advantages of Ramadan fasting, a time-restricted eating from dawn to dusk, have garnered attention. Nevertheless, prior observational studies have found inconsistent findings because of challenges regulating variables such as sleep patterns, dietary habits, and physical activity. This study sought to investigate the impact of the Ramadan fasting model (RFM) on longevity and metabolic biomarkers in obese and non-obese rats. For 12 weeks, 48 male Wistar albino rats were separated into two groups and fed either a standard or a high-fat diet (HFD). During the final four weeks, rats in each group were separated into four subgroups to investigate the effect of RFM with/without training (on Treadmill) or glucose administration on the biomarkers of interest. The HFD groups subjected to RFM had significantly lower Insulin-like growth factor 1 (IGF-1) and mechanistic target of rapamycin (mTOR) serum, whereas AMPK, anti-inflammatory, and antioxidative stress serum levels were significantly higher. All groups reported decreased serum levels of Interleukin-6 (IL-6) and Tumor Necrosis Factor-alpha (TNF-α) compared to the HFD control group. Furthermore, the Real-Time Quantitative Polymerase Chain Reaction (RT-qPCR) results indicated a significant elevation in the TP53 gene expression in groups subjected to RFM. The data indicate that RFM can improve longevity and metabolic biomarkers and reduce pro-inflammation and oxidative stress. Also, RFM improves anti-inflammatory and antioxidant markers in HFD-induced obese rats.
Similar content being viewed by others
Introduction
Exploring the intricacies of fasting, especially through the lens of Ramadan fasting, unveils a complex interplay between dietary practices and metabolic biomarkers, a subject that has garnered research attention in recent years. Fasting has attracted considerable interest for its purported advantageous effects on health, with experimental fasting being cited as a potential enhancer of lifespan and longevity through several metabolic and cellular processes1,2. Fasting and calorie restriction (CR) have been shown to increase autophagy, which may help to prevent the accumulation of damaged molecules and reduce the risk of age-related illnesses3. Important roles in aging and the pathophysiology of age-related illnesses are played by mitochondrial activity and autophagy. Autophagy is the process by which cells break down and recycle damaged or unnecessary cellular components, and autophagy-related genes are still necessary for many anti-aging strategies4. In addition, studies in animal models have suggested that CR could extend lifespan by fostering cellular repair processes and abating oxidative stress, a substantial aging contributor1. Other proposed mechanisms include enhanced mitochondrial function, lowered inflammation5 and reduction in oxidative stress6.
Current evidence indicates that fasting and refeeding may affect cellular aging and the underlying molecular mechanisms and hence longevity in all organisms ranging from yeast to humans, but we still need much work to understand this topic1,7. In humans, available evidence suggests that alternating fasting and refeeding cycles may reduce the risk factors for aging, autoimmunity, and non-communicable diseases3,8. However, the reported beneficial effects of longevity vary with different fasting models1,4,9. Nevertheless, several types of fasting, time-restricted feeding, and CR have been frequently used in animal and human studies, including alternate-day fasting (ADF)10, a 70% energy limit11, the 5:2 diet, which offers 500–700 calories twice a week12, and time-restricted eating (TRE), which typically limits food consumption to 6–12 h/day13. Furthermore, most experimental fasting models permitted water and non-caloric beverages14.
Ramadan fasting is distinguished by daytime abstention from food and drink (including water) from dawn to dusk, with no restrictions at night15. The current findings about autophagy and longevity biomarkers from CR and other forms of experimental fasting may not apply to Ramadan fasting due to its unique peculiarities, particularly since current evidence suggests that the circadian rhythm could influence autophagy effects on aging and lifespan; therefore, the timing of feeding and fasting (day or night) that is limited to night time in Ramadan could affect the peripheral biologic clocks, could impact metabolic biomarkers and longevity16,17,18.
Inflammation and oxidative stress are vital in developing various illnesses, including atherosclerosis, metabolic syndrome, and cardiovascular diseases. Ramadan fasting may reduce cardiovascular risks and improve metabolic syndrome features by decreasing inflammatory responses19,20. Several recent systematic reviews and meta-analyses of observational studies on humans in the free-living environment during Ramadan revealed a trend toward weight loss and improvements in glucometabolic parameters, metabolic syndrome severity, and a number of inflammatory and oxidative stress biomarkers21,22,23,24,25,26. Nevertheless, Ramadan month is associated with several lifestyle changes that may affect metabolism and different metabolism biomarkers, such as increased nocturnal light exposure, decreased sleep duration, and changing dietary pattern, and physical activity27. As most human studies were observational and performed in a free-living environment, the heterogeneity in the findings likely reflects the lack of control for the above confounders. In this study, an animal model was selected to mitigate the influence of various lifestyle variables that might be present during Ramadan and potentially impact the assessed biomarkers. Ramadan Fasting Model (RFM) described a fasting approach on an animal model during their active phase15.
Based on the aforementioned information, a hypothesis was formulated suggesting that refraining from food and drink during the active phase in rats (specifically, from dusk to dawn) may enhance longevity and exhibit positive effects on biomarkers related to autophagy, inflammation, and oxidative stress. Throughout many decades, Wistar Albino Rats have been extensively employed as a prevalent and reliable animal model in experimental research pertaining to age-related and metabolic human ailments, owing to their striking likeness to humans. Furthermore, their metabolism has been impacted in ways that are comparable to those of humans, and many environmental factors are simple to control28,29. Chronic administration of a high-fat diet (HFD) in Wistar Albino rat models has been extensively studied as a reliable approach to induce obesity, heightened inflammation, and oxidative stress28. Hence, the primary objective of this study was to examine the possible health consequences of RFM on lifespan and indicators of metabolic biomarkers, such as insulin-like growth factor-1 (IGF-1), mechanistic target of rapamycin (mTOR), and adenosine monophosphate kinase (AMPK), as well as biomarkers associated with proinflammatory, anti-inflammatory, and oxidative stress responses in Wistar Albino Rats. In this study, we had two main groups of obese and normal-weight rats, and then each group was divided into four subgroups to assess the effect of fasting, diet, training, and glucose (mimicking the consumption of dates at breakfast during Ramadan) on the aforementioned longevity and metabolic biomarkers.
Material and method
RFM conducted in this study is part of a larger project investigating the effects of RFM on various health outcomes in rats. Previously, we have reported data from the same project on the effects of the Ramadan fasting model on nonalcoholic fatty liver in rats15. In the current study, we focused on the longevity effects of this fasting model by measuring specific biomarkers.
Experimental animal preparation
A total of forty-eight male Wistar albino rats, aged three weeks, were acquired from the experimental surgical animals’ lab at the College of Medicine, King Saud University in Riyadh, Saudi Arabia. The rats had an average weight of 60 ± 10 g (g) and were housed at the same facility for the duration of the experiment. The rats were individually kept in ventilated cage (IVC) racks within a controlled environment, with a temperature of 22 ± 2 °C and humidity of 55 ± 5%. They were given free access to water and a standard diet ad libitum for a one-week acclimatization period. They were given free access to water and a standard diet ad libitum for a one-week acclimatization period. This investigation was carried out in compliance with the ARRIVE criteria for reporting research involving animals, guaranteeing comprehensive documentation of the experimental design, techniques, and results. The Institutional Animal Care and Use Committee (IACUC) of King Saud University granted approval for the experimental protocol. (Ref. No.: KSU-SE-21-66). Notably, all procedures involving animals were conducted in accordance with relevant guidelines and regulations, ensuring compliance with ethical standards for the care and use of laboratory animals.
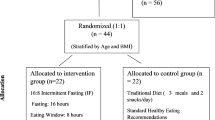
Experimental design
After acclimatization, animals were randomly assigned into two main groups: (1) the standard diet group (n = 24) and (2) the HFD group (n = 24). For eight weeks, the standard diet group had unrestricted access to standard rodent chow (providing 2.9 kcal/g, with fat being 13% of total energy; American Institute of Nutrition AIN-93G purified Rodent diet; catalog number 110700; Dyets Inc, Bethlehem, PA), while the HFD group had free access to a HFD (providing 4.73 kcal/g; Modified Western Diet with 45% fat and AIN-93G vitamin and minerals; catalog number 104293; Dyets Inc, Bethlehem, PA) to induce obesity. To induce obesity, the HFD group was fed a diet providing 4.73 kcal/g (45% fat) for 8 weeks, followed by an additional 4 weeks of HFD feeding combined with the Ramadan fasting model (RFM) intervention. This duration of HFD feeding was chosen based on previous studies demonstrating that feeding male Wistar rats an HFD (providing 45–60% of calories from fat) for 8–12 weeks is sufficient to induce obesity and obesity-related metabolic disorders, such as insulin resistance and dyslipidemia30. In the study, we confirmed that the rats in the HFD group reached a body weight of 320 ± 20 g after 8 weeks of HFD feeding, which was considered obese based on previous literature. However, we acknowledge that providing a more detailed description of the changes in body weight and other obesity-related parameters (e.g., adiposity, glucose tolerance) at multiple time points throughout the 12-week HFD feeding period would provide a clearer picture of the progression of obesity in our model. In future studies, we will consider incorporating additional time points for assessing obesity-related parameters to better characterize the development of obesity and strengthen the interpretation of our findings30. Rats in each main group were then randomly subdivided into four subgroups and underwent further treatment for an additional four weeks. The subgroups were:
-
1.
Control Group standard control (SC): Fed the standard diet and water ad libitum.
-
2.
Standard diet + Ramadan fasting model (S + RFM): Fasting from sunset to dawn, followed by a standard diet and water during the daytime.
-
3.
Standard diet + Ramadan fasting model + Treadmill (S + RFM + T): Observing the same fasting, feeding, and water access as S + RFM, plus morning training on the treadmill for 15 min (3 times/week).
-
4.
Standard diet + RFM + Glucose administration (S + RFM + G): Fasting from sunset to dawn, with glucose administration (1.77 mg/kg) provided orally to break the fast at dawn, followed by the standard diet and water during the daytime.
-
5.
Control Group HFD control (HFDC): Fed the HFD and water ad libitum.
-
6.
HFD + Ramadan fasting model (HFD + RFM): Fasting from sunset to dawn, with a HFD and water provided during the daytime.
-
7.
HFD + Ramadan fasting model + Treadmill (HFD + RFM + T): Observing the same fasting and feeding as HFD + RFM, plus morning training on treadmill for 15 min (3 times/week).
-
8.
HFD + RFM + Glucose administration (HFD + RFM + G): Fasting from sunset to dawn, with glucose administration (1.77 mg/kg) provided orally to break the fast at dawn, followed by the HFD and water during the daytime.
After the total experimental period of 12 weeks, animals in all groups were sacrificed, and blood samples were collected for various analyses.
Ramadan fasting model protocol
The active phase for rats occurs during the nighttime, which corresponds to the daytime in the human cycle15,31. The nocturnal activity period for rats is observed throughout the nighttime, which aligns with the diurnal phase in the human cycle15,31. Consequently, RFM was observed during the period from sunset to dawn, following an 11-hour light and 13-hour dark cycle. The fasting length used for our study, conducted in January 2022, was roughly 13 h from dusk to dawn. This model was sustained for four weeks to mimic the Ramadan fasting period of one month and was implemented between weeks 9 and 12 of the study.
Glucose administration
Glucose powder (Sigma Aldrich, MO, USA) was orally administered to two groups: S + RFM + G and HFD + RFM + G at dawn. The glucose powder was dissolved in distilled water and administered via oral gavage. The selected dose of glucose, 1.77 mg/kg, was determined based on a prior study and is intended to mimic the mean doses derived from three dates, traditionally used to break fasting in humans32.
Training session
Following a familiarization period, the formal training began 5–7 days later. Utilizing a treadmill (MK-680 C No.0807EN03, China), set at a speed of 20–25 m/min, the designated exercise was conducted for 10–15 min in the morning, three times per week33.
Blood sample and tissue collection
At the end of the twelfth week, a fasting period of thirteen hours was observed. In this study, ketamine was administered to ensure rapid onset of anesthesia and effective pain relief for the rats. Dosage was carefully monitored to maintain safety and effectiveness throughout the experiment. Anesthesia was induced with the administration of a single intraperitoneal injection containing a mixture of ketamine and xylazine, with doses of 90 mg/kg and 10 mg/kg, respectively, based on the rat’s weight. The blood samples were collected at 6 a.m. and the blood was extracted directly from the cardiac region and transferred to yellow cap tubes specifically designed for gel separation, devoid of additives. The blood sample was allowed to undergo coagulation at ambient temperature for roughly an hour prior to undergoing centrifugation at a speed of 4000 revolutions per minute for a duration of 10 min to separate the serum. After the completion of the collection process, the euthanized animals were appropriately preserved in zip-lock bags at a temperature of -20 °C until the biohazard business retrieved them.
Measurements variables
Body weight and food consumption
BW was measured at the beginning of the study and, subsequently, every week throughout its duration, utilizing the EK4150 digital scale (Etekcity, Anaheim, CA, USA). Concurrently, food consumption was monitored and documented each week.
For the fasting groups, rats had ad libitum access to food and water from dawn to dusk. From weeks 9 to 12, food intake was assessed weekly by providing rats with precise amounts of food and measuring the remainder after 13 h. A calibrated scale, precise to 0.01 mg, was employed to quantify food consumption. Food consumption (g) was calculated using the formula: [Diet provided (g) - Diet unconsumed (g)], as outlined by Carvalho et al.34.
Longevity and metabolic biomarkers
IGF-1 was assessed utilizing a rat enzyme-linked immunosorbent assay )ELISA( kit (Cat. No. MBS176012, MyBioSource, San Diego, CA, USA). Analysis of mTOR and AMPK were also performed using ELISA kits (Cat. No. MBS266921 and MBS1602983, MyBioSource, San Diego, CA, USA). All analyses were conducted in accordance with the protocols provided with the ELISA kits.
Proinflammatory and anti-inflammatory biomarkers
Interleukin-6 (IL-6), C-Reactive Protein (CRP), Tumor Necrosis Factor-alpha (TNF-α), Interleukin-10 (IL-10), and Adiponectin (ADP) levels were assayed utilizing commercially available sandwich ELISA kits from MyBioSource, San Diego, CA, USA. The specific catalog numbers for the kits used to estimate each biomarker are as follows: IL-6 (Cat. No. MBS355410), CRP (Cat. No. MBS2702539), TNF-α (Cat. No. MBS2507393), IL-10 (Cat. No. MBS2707969), and ADP (Cat. No. MBS2708313). All analyses were conducted strictly following the protocols supplied with the ELISA kits.
Oxidative stress biomarker
Superoxide dismutase (SOD), Glutathione peroxidase (GPx), and Malondialdehyde (MDA) were determined using commercial kits, following the equipment’s instructions (Cat. No. MBS266897; Cat. No. MBS1600242, Cat. No. MBS268427, MyBioSource, San Diego, CA, USA, respectively).
RNA extraction and real-time quantitative polymerase chain reaction (RT-PCR) (RT-qPCR)
Table 1 shows primers used to quantify DNA in real-time qPCR reactions. RNA extraction and subsequent analysis through Real-Time Quantitative Polymerase Chain Reaction (RT-qPCR) were conducted in several detailed steps. Initially, 1 µg of RNA was extracted from 50 mg of liver tissue utilizing TRIzol™ Reagent (Cat. no. 15596026, Thermo Fisher), adhering strictly to the manufacturer’s instructions. This RNA was then converted into cDNA using a GoScript™ Reverse Transcriptase cDNA synthesis kit (Cat no. 5001). The RT-qPCR procedure was subsequently performed, utilizing Applied Biosystems™ to amplify specific cDNA targets. Each reaction was prepared with a total volume of 20 µl, which included SYBR® Green PCR Master Mix (Cat. No. 4309155, Thermo Fisher Scientific), 25 ng of cDNA, and 10 pmol/µl of each forward and reverse primer. In the context of primer design, those used were crafted to target intron-spanning regions, developed via Primer-BLAST, and in the case of oxidative stress (ROS) biomarker analysis, were specified to target the tumor protein (TP53). All samples were run in duplicate on a Fast optical 96-well Reaction plate with Barcode (0.1 ml) (Cat. No. 4346906, MicroAmp® Applied Biosystems). For the expression analysis, non-specific quantitative RT-qPCR expression was calculated using the 2-ΔΔCt method to interrogate gene expression levels, utilizing (RNA) II (DNA directed) polypeptide A (POLR2A) as a housekeeping gene to facilitate data normalization35 .
Statistical analysis
Statistical analyses were performed using Prism 7.1 (GraphPad® software), and all the results are expressed as the mean ± standard deviation unless otherwise stated. Shapiro-Wilk test was used to test data normality. Differences between animal groups were analyzed using a one-way analysis of variance (ANOVA) followed by Tukey’s post-hoc analysis to test when a statistically significant difference was found. For all tests, a p-value < 0.05 was deemed statistically significant.
Results
Body weight and food intake
The BW and food consumption data from the same rats have been published in our previous work15. Figure 1A shows all groups’ BW throughout the experimental period (12 weeks). Table 2 details the BW and food intake of the Standard Diet (S) and HFD groups at the experiment’s conclusion. Within the S groups, no significant differences in BW were observed (Table 2). Contrasting this, amongst the HFD groups, rats within the HFD + RFM group exhibited a notably lower BW compared with the HFDC group (P < 0.004). However, no significant differences were found between the HFD + RFM + T and HFD + RFM + G groups compared with the HFDC group, even though the BW was higher in the general HFD group (Table 2). Noteworthy is that food intake did not show significant differences among the S and HFD groups (Table 2).
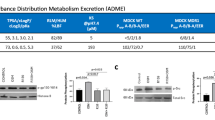
Changes in the longevity and metabolic biomarkers
Figure 2 presents the longitudinal data for longevity and metabolic biomarkers across all groups. For the S groups, a noteworthy decline in serum IGF-1 levels was recorded in the S + RFM + T group relative to the SC group (P = 0.017), as depicted in Fig. 2A. Simultaneously, the S + RFM + G group exhibited a notable decrease in serum mTOR levels compared to the SC group (P = 0.038; Fig. 2C). Moreover, the S + RFM + T group exhibited a pronounced elevation in serum AMPK levels compared to the SC group (P = 0.013). However, both S + RFM (P = 0.006) and S + RFM + G (P = 0.004) groups displayed significantly diminished serum AMPK levels when compared with the S + RFM + T group (Fig. 2E). Addressing the HFD groups, Fig. 2B and D, respectively, illustrate that serum IGF-1 and mTOR levels were distinctly elevated in the HFDC group (P < 0.0001) compared to the HFD + RFM, HFD + RFM + T, and HFD + RFM + G groups. In addition, serum AMPK levels were significantly improved in the HFD + RFM + T (P < 0.0001) and HFD + RFM + G (P = 0.027) groups compared to the HFDC group. Interestingly, it was seen that the HFD + RFM + T group had a notable inclination towards increased AMPK levels in comparison to the HFD + RFM group (P = 0.006; Fig. 2F).
Impact of RFM on longevity and autophagy biomarkers of all groups of rats. Each panel illustrated the effect of RFM on serum levels of : (A) Insulin-like Growth Factor 1(IGF-1) among standard groups, (B) levels of Insulin-like Growth Factor 1(IGF-1) among High fat diet HFD groups, (C) mammalian target of rapamycin (mTOR) among standard groups, (D) mammalian target of rapamycin (mTOR) among HFD groups, (E) AMP-activated protein kinase (AMPK) among standard groups, and (F) AMPK among High Fat diet groups. Data were expressed as (mean ± SD) (n = 6). Data in each group of diet were evaluated by one-way ANOVA followed by Tukey’s t-test as post hoc. The bracket shows statistically significant differences among groups at, *P-value ≤ 0.05; **P-value ≤ 0.005; ***P-value ≤ 0.0005. SC S diet control, S standard diet, HFD high-fat diet, RFM ramadan fasting model, T treadmill, G glucose administration.
Inflammatory and anti-inflammatory biomarkers
Figure 3 delineates the inflammatory and anti-inflammatory biomarkers across all groups. When examining the S groups, the serum levels of IL-6, TNF-α, CRP, IL-10, and ADP did not exhibit significant variances (Fig. 3A,C,E,G & I, respectively). Examining the HFD groups, serum IL-6 levels were notably lower in the HFD + RFM (P = 0.007), HFD + RFM + T (P = 0.012), and HFD + RFM + G (P = 0.007) groups compared to the HFDC group (Fig. 3B). Additionally, serum TNF-α levels were significantly lower in the HFD + RFM (P = 0.002) and HFD + RFM + T (P = 0.016) groups than in the HFDC group (Fig. 3D). Regarding CRP, no significant differences were identified among HFD groups (Fig. 3F). Notably, serum IL-10 levels were significantly elevated in HFD + RFM, HFD + RFM + T, and HFD + RFM + G groups (P < 0.0001) compared to the HFDC group (Fig. 3-H). Furthermore, serum ADP levels were significantly higher in the HFD + RFM (P = 0.006), HFD + RFM + T (P = 0.002), and HFD + RFM + G groups (P = 0.004) when compared with the HFDC group (Fig. 3J).
Impact of RFM on inflammation and anti-inflammation biomarkers of all groups of rats. Each panel illustrated the effect of RFM on serum levels of (A) Interluken-6 (IL-6) in all standard groups, (B) Interluken-6 (IL-6) in all HFD groups, (C) tumor necrosis factor-α (TNF-α) in all standard groups, (D) TNF-α in all HFD groups, (E) C-reactive protein (CRP) in all standard groups, (F) CRP in all HFD groups, (G) interleukin-10 (IL-10) in all standard groups, (H) IL-10 in all HFD groups, (I) adiponectin (ADP) in all standard groups, and (J) ADP in all HFD groups. Data were expressed as (mean ± SD) (n = 6). Data in each group of diet were evaluated by one-way ANOVA followed by Tukey’s t-test as post hoc. The bracket shows statistically significant differences among groups at, *P-value ≤ 0.05; **P-value ≤ 0.005; ***P-value ≤ 0.0005. SC S diet control, S standard diet, HFD high-fat diet, RFM ramadan fasting model, T treadmill, G glucose administration..
Oxidative stress biomarkers
Figure 4 displays the oxidative stress biomarkers of all groups. There were no significant variations between S groups in SOD, GPx, and MDA serum levels (Fig. 4A,C, & E; respectively). In contrast, in the HFD groups, serum SOD levels were significantly higher in the HFD + RFM (P = 0.001), HFD + RFM + T(p = 0.004), and HFD + RFM + G (P = 0.003) groups compared with the HFDC group (Fig. 4B). Serum GPx levels were significantly higher in HFD + RFM (P < 0.0001), HFD + RFM + T (P < 0.0001), and HFD + RFM + G (P = 0.0002) groups compared with the HFDC group (Fig. 4D). In addition, significant differences in ROS responses were noted. The levels of serum MDA were significantly lower in the HFD + RFM (P = 0.0462), HFD + RFM + T (P = 0.0108), and HFD + RFM + G groups (p = 0.0104) compared with the HFDC group (Fig. 4D).
Impact of RFM on oxidative stress biomarkers of all groups of rats. Each panel illustrated the effect of RFM on serum levels of (A) Superoxide Dismutase (SOD) in all standard groups, (B) SOD in all HFD groups, (C) Glutathione peroxidase (GPx) in all standard groups, (D) GPx in all HFD groups, (E) Malondialdehyde (MDA) in all standard groups, and (F) MDA in all HFD groups. Data in each group of diet were evaluated by one-way ANOVA followed by Tukey’s t-test as post hoc. The bracket shows statistically significant differences among groups at, *P-value ≤ 0.05; **P-value ≤ 0.005; ***P-value ≤ 0.0005. . SC S diet control, S standard diet, HFD high-fat diet, RFM ramadan fasting model, T treadmill, G glucose administration.
ROS and inflammation markers at the molecule levels
TP53 mRNA as an indicator for training and metabolic changes
The results obtained from the RT-qPCR analysis demonstrated a statistically significant increase in TP53 gene expression in both the S + RFM and S + RFM + T groups when compared to the SC group, as depicted in Fig. 5A. In a similar vein, it is worth noting that the expression of the TP53 gene was significantly elevated in the HFD + RFM and HFD + RFM + T groups as compared to the HFDC group (Fig. 5B).
Impact of RFM on the molecule levels for TP53 extracted from rat’s liver. Each panel illustrated the effect of RFM on (A) Real-time polymerase chain reaction of tumor protein (TP 53) in all standard groups, (B) Real-time polymerase chain reaction of tumor protein (TP 53) in all HFD groups. Data in each group of diet were evaluated by one-way ANOVA followed by Tukey’s t-test as post hoc. The bracket shows statistically significant differences among groups at, *P-value ≤ 0.05; **P-value ≤ 0.005; ***P-value ≤ 0.0005. SC S diet control, S standard diet, HFD high-fat diet, RFM ramadan fasting model, T treadmill, G glucose administration.
Discussion
This study shed new light on the effects of RFM (13 h of fasting every day for a month) during rats’ active phase on longevity, metabolism, proinflammatory, and oxidative stress biomarkers. Our findings suggest that RFM positively influences longevity and metabolic biomarkers, inflammatory status, and oxidative stress in obese rats.
Many studies have shown that intermittent fasting benefits many chronic diseases, including obesity, diabetes mellitus, cardiovascular disease, nonalcoholic fatty liver disease, cancers, and neurological disorders14,15,38,39. However, data are scarce on whether Ramadan fasting can contribute to healthy longevity, and this is the first study that sheds light on the effect of RFM on the longevity biomarkers under experimentally controlled conditions. Importantly, the hallmarks of aging include altered metabolic control, inflammation, oxidative stress, and reduced immunological function. Interestingly, obese and seniors have remarkably similar immunological profiles in adipose tissues, indicating a substantial overlap in the underlying mechanisms governing both processes discussed in Trim et al.40.
One notable concern that arose from our investigation was the noteworthy decline in IGF-1 levels observed in the S + RFM + T group when compared with the SC group. Additionally, it was observed that IGF-1 levels in the HFD + RFM, HFD + RFM + T, and HFD + RFM + G groups exhibited a significant decrease in comparison to the HFDC group. As reported, IGF-1, blood glucose, and insulin levels are also decreased by intermittent fasting, including ADF and TRF (fasting for 8 weeks, 16 fasting window per day ); meanwhile, insulin sensitivity and adiponectin levels are increased41. Indeed, IGF-1 is a hormone involved in various physiological processes, including growth, development, and metabolism. It has been suggested that IGF-1 may play a role in the aging process and lifespan and that lower levels of IGF-1 are associated with increased lifespan42. In non-human primates, lower levels of IGF-1 have been associated with increased lifespan. For example, Tchkonia et al. found that rhesus monkeys with lower levels of IGF-1 lived longer than those with higher levels43. Holzenberger also reported that mice with lower levels of IGF-1 lived longer and were less likely to develop age-related diseases (i.e., cancer and diabetes) than those with higher levels44. In humans. it has been reported that individuals with lower levels of IGF-1 were more likely to live to exceptionally long ages than those with higher levels42.
A further noteworthy finding in this study related to the lower levels of mTOR in the RFM groups, specifically, the HFD + RFM, HFD + RFM + T, and HFD + RFM + G, compared with the HFDC group. Additionally, we observed an enhancement in AMPK levels among HFD + RFM, HFD + RFM + T, and HFD + RFM + G groups compared with HFDC groups. Concurrent training with RFM significantly increased AMPK, underscoring the benefit of integrating fasting with exercise. Intriguingly, dietary modification (i.e., intermittent fasting ) can activate autophagy and improve longevity through certain molecular actors like mTOR and AMPK1. Our findings are supported by a previous study on an animal model that showed the significant effect of short-term intermittent fasting on the suppression of mTOR45. In studies of laboratory animals on CR, the general finding was that decreased food consumption strongly improves the life span. CR has a beneficial effect on health longevity by suppressing mTOR and inflammations46. Fasting and CR have similar common pathways in animal models. According to Goodrick and colleagues, maintaining rats on an ADF schedule can extend their lifespan by up to 80%47. Consistent with our results, Hatori et al. showed that TRE in mice activated AMPK and suppressed mTOR48. Although not completely clear, proposed mechanisms underlying the effect of IF on longevity and autophagy have been described. Since mTOR is a known autophagy inhibitor, AMPK’s involvement in boosting autophagy largely depends on inhibiting mTOR in low-nutrient environments to reverse mTOR-dependent inhibition1.
Autophagy is crucial in providing healthy longevity pathways intimately connected to AMPK49. Furthermore, TRF or training elevated hepatic AMP levels in mice, which triggered AMPK50. Indeed, AMPK activation brings about a variety of beneficial effects in the body when triggered in the proper tissues. Its activation enhances insulin sensitivity, promotes weight loss, increases muscle strength, and reduces inflammation7,51,52.
In our current work, rats were chronically fed HFD for eight weeks to induce an obese phenotype, which promoted obesity-related characteristics such as increased BW, inflammation, and ROS. This obesity induction was consistent with numerous other findings30,53. The primary mechanism behind HFD-induced obesity and fat accumulation is hyperphagia (overeating)54. In addition, several previous studies have corroborated the current findings, noting a significant increase in BW among the HFD group in this study, and have demonstrated the obesogenic effect of HFD55,56. Accordingly, an important finding in this study is the ability of RFM/RFM + T to reduce BW of the intervention groups compared with the SC and HFDC rats.
Intriguingly, our data could be explained by the ability of RFM itself to utilize fat in fat tissue for decreasing BW57. Several previous meta-analyses supported our findings and showed a significant decrease in BW after Ramadan58,59,60. For instance, a meta-analysis involving 35 studies has shown that Ramadan fasting reduces BW (− 1.24 kg) in both sexes60. Findings from a meta-analysis of 70 studies in overweight and obese individuals reported a significant reduction in body fat percentage58.
Inflammatory cytokines are signaling molecules that play a vital role in the immune response and inflammation61. While inflammation is necessary for the body’s defense against infection and injury, chronic inflammation is associated with a range of age-related diseases, including cancer, cardiovascular disease, and neurodegeneration61. In this context, the relationship between inflammatory cytokines and longevity is complex and remains partially understood. Our study demonstrated a reduction in the proinflammatory cytokines (TNF-α and IL-6) in the RFM groups. We observed that RFM significantly reduced TNF-α and IL-6 levels among HFD rats. Some studies have suggested that higher levels of proinflammatory cytokines may be associated with a shorter lifespan62. IL-6 has long been recognized as being significant in aging and age-related diseases63. Usually, blood levels of IL-6 are low, but they rise as people age and show signs of frailty and chronic disease, and they correlate with mortality62. Additionally, IL-6 has been linked to sarcopenia and a risk factor for cardiovascular disease64. A longevity benefit was observed for carriers of the reduced cytokine-producing IL-6 allele in a large cohort of European nonagenarians and centenarians65. Similarly, supportive findings for this IL-6 allele were also reported in a related case-control study65,66. Research to evaluate the results of IL-6-related inflammation blockade in various age-related disorders with the potential to contribute to more successful aging is either ongoing or planned67,68 Therefore, the impact of RFM practiced intermittently throughout the year on age-related disorders and auto-immune diseases should be assessed in future research.
In our study, TNF- α decreased in the obese model when subjected to the RFM. We noticed that the TNF- α level was significantly lower in HFD + RFM and HFD + RFM + T. TNF- α is a proinflammatory cytokine that plays a critical role in immune system regulation and inflammation and has been linked in some studies with longevity. There was no attrition of the TNF—308 A/G polymorphism in centenarians in research in nonagenarian/centenarian groups from three European nations69,70. Similar to IL-6, research on repurposing anti-inflammatory medications is being developed in light of mounting evidence suggesting a link between rising TNF-α and age-related illnesses. According to research, TNF inhibitors may play preventative or ameliorative functions in several age-related diseases71. The above stresses the importance of conducting long-term studies to assess the effects of RFM on various age-related diseases that may influence lifespan. Moreover, we observed that CRP did not reach a statistical significance reduction among groups. Consistent with our results, previous studies found that TNF-α and IL-6 were the most affected biomarkers after Ramadan fasting among obese participants72,73. Faris et al., (2012)74 and Ünalacak et al., (2011)75 reported that Ramadan fasting reduced circulating levels of inflammatory cytokines (IL-6 and TNF-α) but not CRP among obese individuals. In the same line, this is consistent with Nematy et al., 2012 study76, which demonstrated no significant reduction in CRP after 30 days of fasting compared with the beginning of the study. In contrast, Madlour et al., (2019)77 showed significant improvement in IL-6, CRP, and homocysteine levels among healthy young adults after 30 days of Ramadan fasting. CRP is regularly evaluated to assess inflammation caused by chronic disease, infection, or injury. High sensitivity CRP (hs-CRP) testing is more sensitive than the standard CRP testing and can detect smaller increases in CRP. Thus further studies are needed to asses hs-CRP rather than CRP test78. Indeed, above intervention trials had mixed findings, possibly because of different sample sizes, fasting hours, methodological inconsistencies, or controlling for potential confounders74.
Some potential mechanisms by which fasting promotes healthy longevity include the impairment of activation in the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-B) through intermittent fasting. NF-B is a crucial transcriptional regulator of inflammation that controls the production of proinflammatory cytokines such as IL-6 and TNF-α20. However, in the current study, we did not test this gene; therefore, more investigation is needed to explore the potential mechanisms by which RFM may impact longevity and inflammation, specifically by evaluating the gene expression of NF-B. Another possible mechanism is that RFM helps to reduce hyperplasia and hypertrophy of fat cells, which leads to a decrease in the concentration of inflammatory markers39,60. Hence, RFM could positively improve cardiovascular risks and attenuate metabolic syndrome characteristics by suppressing inflammatory reactions27,79.
There was an increase in the anti-inflammatory cytokine IL-10 in the HFD rats after the RFM. In the current study, the level of IL-10 among rats subjected to RFM was significantly higher in HFD groups. IL-10 is an anti-inflammatory cytokine that plays a crucial role in immune system regulation and inflammation and suppresses the activities of IL-6, TNF-α, and IL-880. Studies on the relationship between IL-10 and longevity have suggested that higher levels of IL-10 may be positively associated with longevity and reduced risk of age-related diseases. The high-producing GG 1,082 variant of the IL-10 promoter polymorphism was associated with a survival benefit in male Sicilian centenarians, indicating that IL-10’s anti-inflammatory properties may serve as a marker for male longevity69. A recent comprehensive study revealed a significant association between IL-10 promoter polymorphisms, specifically rs1800871 and rs1800896, and the syndromic characterization of frailty. This association was observed at both the allelic and haplotypic levels81.
Inflammation and oxidative stress are significant indicators of the aging process. Likewise, these biomarkers are the most important feature associated with obesity82. Chronic feeding of HFD increases adipose tissue mass, which increases the production of inflammatory markers and ROS while decreasing the production of anti-inflammatory30. Our finding showed that HFDC groups had higher levels of proinflammatory biomarkers and low levels of ADP and IL-10. Studies on obese individuals and animal models demonstrated high circulating levels of proinflammatory cytokines and acute-phase proteins like TNF- α, IL-6, or CRP56,83. Moreover, obesity is associated with impaired ADP release from adipocytes84. In the current study, ADP levels were significantly higher in HFD + RFM, HFD + RFM + T, and HFD + RFM + G compared with the HFDC group. It is well established that ADP is an anti-inflammatory hormone that boosts cell antioxidants, downregulates Furthermore, our data indicate that RFM causes an increase in IL-10 levels among HFD + RFM, HFD + RFM + T, and HFD + RFM + G compared with HFDC group. IL-10 is a cytokine that can inhibit the proinflammatory signaling of NF-κB. The proinflammatory cytokine TNF-α is known to have a significant impact on the initiation and sustenance of inflammation78. Conversely, IL-10 is considered a classic anti-inflammatory cytokine due to its ability to suppress the production of inflammatory cytokines and chemokines, including IL-1β, IL-6, and TNF-α. IL-10 functions as an endogenous antagonist of TNF-α by impeding the NF-κB inflammatory pathway85. Hence, RFM can inhibit pro-inflammatory signaling pathways while also stimulate at least one anti-inflammatory pathway. Indeed, IL-10 is pivotal in decreasing weight gain, increasing insulin sensitivity, and reducing inflammation14,20,86,87. Ramadan fasting, as a form of intermittent fasting can reduce systemic inflammation in obese and chronically ill individuals72 and improve the anti-inflammatory agents88 .
Consequently, reduced circulating levels of inflammatory cytokines during RFM could also be attributed to decreased oxidative activity stress8. Importantly, when compared with the HFDC group, we observed an increase in SOD and GPx levels, as well as a decrease in MDA levels, in the HFD + RFM, HFD + RFM + T, and HFD + RFM + G groups during RFM. Similarly, previous studies reported that IF reduces the levels of oxidative stress biomarkers, preventing ROS generation20,89. Oxidative stress arises from an imbalance between the production of ROS and the capacity of antioxidant defenses. A marker indicative of oxidative stress is the level of MDA in the serum. MDA, a byproduct of polyunsaturated fatty acid (PUFA) peroxidation, can serve as a marker for cell or tissue damage due to its association with increased lipid peroxidation. The suggested mechanism is that RFM enhanced gene expression of antioxidant defenses, including mitochondrial transcription factor A (TFAM), SOD2, and nuclear factor erythroid 2 association Factor 2 (Nrf2)76,77. Another possible mechanism is that RFM attenuates the insulin/IGF-1 axis level that predisposes to inflammation and oxidative stress among obese individuals90. Importantly, we found that the overexpression of TP53 in S + RFM and S + RFM + T was greater compared with the SC. Additionally, we observed a significant increase in overexpression of TP53 among HFD + RFM and HFD + RFM + T compared with the HFDC group. Our findings, in line with the reported investigation, were that homozygous knockout (p53−/−) mice significantly demolished the mitochondrial anaerobic capacity in the liver, which promotes TP53’s ability to regulate mitochondrial activity and glycolysis91,92. Moreover, TP53 transcribed mitochondrial glutaminase 2 (GLS2) that enhances glutathione (GSH) synthesis that, in return, reduces ROS in the cell93,94. Notably, the exact mechanism by which p53 regulates aging and longevity is still unknown. Numerous possible Mechanisms have been suggested, including the regulation of the insulin/ IGF-1 and mTOR pathways, stem cells, oxidative stress and ROS95.
Collectively, treatment of HFD-induced obesity with RFM not only reduced BW but also boosted metabolic function. Integrating RFM + T may be an efficient alternative to accelerate weight loss or metabolic changes. Moreover, this study offers some ameliorated changes in cytokines levels in HFD-fed rats subjected to RFM. These findings suggest healthy longevity mediated by decreasing the level of IGF-1 and mTOR, boosting AMPK, controlling inflammation, decreasing the production of ROS, and enhancing the body’s natural antioxidant defense mechanism. This is an independent antioxidant and anti-inflammatory effect, which RFM could also ameliorate in these rats.
The strengths of our paper lie in its innovative approach and rigorous methodology. We present the first application of RFM in an animal model, specifically Wistar Albino Rats. This model is well-established for studying human diseases related to aging and metabolism. The design of our study enabled us to effectively manage confounding factors commonly seen in human investigations, including variations in the dark/light cycle, meal composition, and physical activity. In this controlled experimental design, which included assessments of the effects of fasting, diet, training, and glucose administration, we measure a range of biomarkers related to longevity, autophagy, inflammation, and oxidative stress. Our findings are the first to show that RFM positively affects these indicators in obese rats. However, our study also highlights the need for further research to evaluate the impact of RFM on the microbiota composition and to understand the underlying molecular mechanisms, particularly in relation to the gene expression of the FOXO nuclear factor. Such research could provide deeper insights into the impact of RFM on longevity biomarkers and strengthen the scientific basis for our observed outcomes. Therefore, this study contributes to the existing body of knowledge and opens up new avenues for future research in this area.
The present study has several important limitations that may impact the generalizability and applicability of the findings to humans. Firstly, the study was conducted on rats, which may not always perfectly mimic human physiology and metabolism. Secondly, the study used a HFD to induce obesity in rats, which might not accurately represent the complex etiology of human obesity that involves genetic, environmental, and behavioral factors. While our study demonstrates the positive effects of RFM on some biomarkers of longevity, metabolism, inflammation, and oxidative stress, further research is needed to fully elucidate the underlying mechanisms. Quantifying adipose tissue weight in future studies would provide valuable insights into the role of adipose tissue in mediating the anti-inflammatory and pro-longevity effects of RFM. Additionally, our previously published study has shown a strong correlation between the improvement in lipid profile and the decrease in inflammation levels during RFM. The combination of these findings suggests that the protective effects of RFM may be mediated, in part, by improvements in lipid metabolism and adipose tissue function. However, further research is needed to confirm these mechanisms and explore the specific role of adipose tissue in the context of RFM. Our findings demonstrate significant changes in some plasma biomarkers associated with longevity, metabolism, and inflammation following RFM. However, further research is needed to establish whether these plasma changes are reflective of tissue-specific modulation, particularly in metabolically active organs such as the liver. The liver is central to autophagy regulation and metabolic homeostasis, making it a critical organ for studying the mechanisms underlying the observed systemic effects96. Future investigations should incorporate molecular analyses of autophagy markers, such as Beclin-1 and Autophagy-related 7 (ATG7), as well as phosphorylation studies of mTOR and AMPK, to provide a more comprehensive understanding of how RFM modulates autophagic activity at the tissue level. By doing so, we can better elucidate the pathways through which RFM exerts its protective effects on metabolic health and longevity.
We focused on male rats in this study for several reasons. Firstly, female rats experience regular estrous cycles, which can influence various physiological processes, including metabolism and inflammation97. These hormonal fluctuations could potentially confound the results, making it more challenging to isolate the effects of RFM on the measured biomarkers. Secondly, studies have shown that male rats are more susceptible to diet-induced obesity compared to female rats98. As our study aimed to investigate the impact of RFM on obesity-related biomarkers, using male rats allowed us to more effectively model the obese phenotype. Finally, many studies exploring the effects of intermittent fasting and caloric restriction on longevity and metabolic health have primarily used male animals. By focusing on male rats, our study maintains consistency with the existing literature, facilitating comparisons and interpretations of our findings.
In our study, we measured total AMPK levels using an ELISA kit, but this does not distinguish between inactive and active AMPK forms. Phosphorylation at Thr172 is critical for AMPK activation and its role in energy homeostasis99. Future studies will incorporate techniques like Western blotting or phospho-specific ELISA to measure p-AMPK and explore its activation in tissues such as the liver and skeletal muscle, providing a more comprehensive understanding of RFM’s effects on AMPK signaling100. The study used glucose administration to mimic the consumption of dates at breakfast during Ramadan. However, dates contain other nutrients and bioactive compounds besides glucose, which could have additional effects on health and metabolism. Therefore, using glucose alone might not fully capture the effects of consuming dates.
In conclusion, this study demonstrates the potential of the RFM to improve longevity and metabolic biomarkers, reduce proinflammatory and oxidative stress markers, and enhance anti-inflammatory and antioxidant markers in HFD-induced obese rats. These findings contribute to the growing body of evidence supporting the health benefits of fasting during Ramadan and provide a basis for future research on the underlying mechanisms and potential clinical applications. Further studies are needed to confirm these findings in humans and to explore the long-term effects of RFM on health and longevity.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Longo, V. D., Di Tano, M., Mattson, M. P. & Guidi, N. Intermittent and periodic fasting, longevity and disease. Nat. Aging 1, 47–59 (2021).
Visioli, F., Mucignat-Caretta, C., Anile, F. & Panaite, S. A. Traditional and medical applications of fasting. Nutrients 14, 433 (2022).
Wei, M. et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci. Transl. Med. 9, eaai8700 (2017).
Yin, Z. & Klionsky, D. J. Intermittent time-restricted feeding promotes longevity through circadian autophagy. Autophagy 18, 471–472 (2022).
Brandhorst, S. et al. A periodic Diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and Healthspan. Cell Metab. 22, 86–99 (2015).
Lee, C. et al. Fasting cycles retard growth of tumors and sensitize a range of Cancer Cell types to Chemotherapy. Sci. Transl. Med. 4, (2012).
de Cabo, R. & Mattson, M. P. Effects of Intermittent fasting on health, aging, and disease. N. Engl. J. Med. 381, 2541–2551 (2019).
Lushchak, O., Strilbyska, O., Piskovatska, V., Koliada, A. & Storey, K. B. Intermittent Fasting. In Reference Module in Biomedical Sciences, B9780128012383621335 (Elsevier, 2018). https://doi.org/10.1016/B978-0-12-801238-3.62133-5
López-Otín, C., Galluzzi, L., Freije, J. M. P., Madeo, F. & Kroemer, G. Metabolic Control of Longevity. Cell 166, 802–821 (2016).
Trepanowski, J. F. et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern. Med. 177, 930–938 (2017).
Johnson, J. B. et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic. Biol. Med. 42, 665–674 (2007).
Sundfør, T. M., Svendsen, M. & Tonstad, S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: a randomized 1-year trial. Nutr. Metab. Cardiovasc. Dis. 28, 698–706 (2018).
Chaix, A., Lin, T., Le, H. D., Chang, M. W. & Panda, S. Time-restricted feeding prevents obesity and metabolic syndrome in mice lacking a circadian clock. Cell Metab. 29, 303–319e4 (2019).
Vasim, I., Majeed, C. N. & DeBoer, M. D. Intermittent Fasting Metabolic Health. Nutrients 14, 631 (2022).
Alasmari, A. A. et al. Ramadan fasting model exerts hepatoprotective, anti-obesity, and anti-hyperlipidemic effects in an experimentally-induced nonalcoholic fatty liver in rats. Saudi J. Gastroenterol. https://doi.org/10.4103/sjg.sjg_204_23 (2023).
BaHammam, A. S. & Almeneessier, A. S. Recent evidence on the impact of Ramadan diurnal intermittent fasting, Mealtime, and circadian rhythm on cardiometabolic risk: a review. Front. Nutr. 7, (2020).
Chaudhari, A., Gupta, R., Makwana, K. & Kondratov, R. Circadian clocks, diets and aging. Nutr. Healthy Aging 4, 101–112 (2017).
Ulgherait, M. et al. Circadian autophagy drives iTRF-mediated longevity. Nature 598, 353–358 (2021).
Dote-Montero, M., Sanchez-Delgado, G. & Ravussin, E. Effects of Intermittent Fasting on Cardiometabolic Health: An Energy Metabolism Perspective. Nutrients 14, 489 (2022).
Zouhal, H. et al. Effects of Ramadan intermittent fasting on inflammatory and biochemical biomarkers in males with obesity. Physiol. Behav. 225, 113090 (2020).
Jahrami, H. et al. The impact of Ramadan fasting on the metabolic syndrome severity in relation to ethnicity and sex: results of a systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 32, 2714–2729 (2022).
Jahrami, H. et al. Ramadan Fasting improves body composition without exacerbating Depression in males with diagnosed major depressive disorders. Nutrients 13, 2718 (2021).
Faris, M., Jahrami, H., Abdelrahim, D., Bragazzi, N. & BaHammam, A. The effects of Ramadan intermittent fasting on liver function in healthy adults: a systematic review, meta-analysis, and meta-regression. Diabetes Res. Clin. Pract. 178, 108951 (2021).
Jahrami, H. A. et al. Does four-week consecutive, dawn-to-sunset intermittent fasting during Ramadan affect cardiometabolic risk factors in healthy adults? A systematic review, meta-analysis, and meta-regression. Nutr. Metab. Cardiovasc. Dis. 31, 2273–2301 (2021).
Abdelrahim, D. et al. Impact of Ramadan diurnal intermittent fasting on hypoglycemic events in patients with type 2 diabetes: a systematic review of randomized controlled trials and observational studies. Front. Endocrinol. 12 (2021).
Faris, M. A. I. et al. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res. Clin. Pract. 165, 108226 (2020).
BaHammam, A. S. & Almeneessier, A. S. Recent evidence on the impact of Ramadan diurnal intermittent fasting, Mealtime, and circadian rhythm on cardiometabolic risk: a review. Front. Nutr. 7, 28 (2020).
Marques, C. et al. High-fat diet-induced obesity rat model: a comparison between Wistar and Sprague-Dawley rat. Adipocyte 5, 11–21 (2015).
Sengupta, P. The laboratory rat: relating its age with Human’s. Int. J. Prev. Med. 4, 624–630 (2013).
de Dias, M. Diet-induced obesity in animal models: points to consider and influence on metabolic markers. Diabetol. Metab. Syndr. 13, 32 (2021).
Pickel, L. & Sung, H. K. Feeding rhythms and the circadian regulation of metabolism. Front. Nutr. 7, 39 (2020).
Assirey, E. A. R. Nutritional composition of fruit of 10 date palm (Phoenix dactylifera L.) cultivars grown in Saudi Arabia. J. Taibah Univ. Sci. 9, 75–79 (2015).
Smyers, M. E., Bachir, K. Z., Britton, S. L., Koch, L. G. & Novak, C. M. Physically active rats lose more weight during calorie restriction. Physiol. Behav. 139, 303–313 (2015).
Carvalho, M. R. et al. Influence of high-intensity interval training and intermittent fasting on myocardium apoptosis pathway and cardiac morphology of healthy rats. Life Sci. 264, 118697 (2021).
Rao, X., Huang, X., Zhou, Z. & Lin, X. An improvement of the 2ˆ(–delta delta CT) method for quantitative real-time polymerase chain reaction data analysis. Biostat. Bioinform. Biomath. 3, 71–85 (2013).
Ghatei, N. et al. Evaluation of bax, bcl-2, p21 and p53 genes expression variations on cerebellum of BALB/c mice before and after birth under mobile phone radiation exposure. Iran. J. Basic. Med. Sci. 20, 1037–1043 (2017).
Yokoyama, T. et al. Identification of reference genes for quantitative PCR analyses in developing mouse gonads. J. Vet. Med. Sci. 80, 1534–1539 (2018).
Anic, K. et al. Intermittent fasting—short- and long-term quality of life, fatigue, and safety in healthy volunteers: a prospective, clinical trial. Nutrients 14, 4216 (2022).
Varady, K. A., Cienfuegos, S., Ezpeleta, M. & Gabel, K. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat. Rev. Endocrinol. 18, 309–321 (2022).
Trim, W., Turner, J. E. & Thompson, D. Parallels in immunometabolic adipose tissue dysfunction with ageing and obesity. Front. Immunol. 9 (2018).
Moro, T. et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 14, 290 (2016).
Milman, S. et al. Low insulin-like growth factor-1 level predicts survival in humans with exceptional longevity. Aging Cell 13, 769–771 (2014).
Tchkonia, T. et al. Mechanisms and metabolic implications of Regional differences among Fat Depots. Cell Metab. 17, 644–656 (2013).
Holzenberger, M. et al. IGF-1 receptor regulates lifespan and resistance to oxidative stress in mice. Nature 421, 182–187 (2003).
Bagherniya, M., Butler, A. E., Barreto, G. E. & Sahebkar, A. The effect of fasting or calorie restriction on autophagy induction: a review of the literature. Ageing Res. Rev. 47, 183–197 (2018).
López-Lluch, G. & Navas, P. Calorie restriction as an intervention in ageing: calorie restriction and ageing. J. Physiol. 594, 2043–2060 (2016).
Goodrick, C. L., Ingram, D. K., Reynolds, M. A., Freeman, J. R. & Cider, N. Effects of intermittent feeding upon body weight and lifespan in inbred mice: interaction of genotype and age. Mech. Ageing Dev. 55, 69–87 (1990).
Hatori, M. et al. Time-Restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 15, 848–860 (2012).
Burkewitz, K., Weir, H. J. M. & Mair, W. B. in AMPK as a Pro-longevity Target (eds AMP-activated Protein Kinase, M. D. & Viollet, B.), 227–256 (Springer International Publishing, 2016). https://doi.org/10.1007/978-3-319-43589-3_10.
Chaix, A., Manoogian, E. N. C., Melkani, G. C. & Panda, S. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu. Rev. Nutr. 39, 291–315 (2019).
Canbolat, E. & Cakıroglu, F. P. The importance of AMPK in obesity and chronic diseases and the relationship of AMPK with nutrition: a literature review. Crit. Rev. Food Sci. Nutr. 63, 449–456 (2023).
He, C. et al. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature 481, 511–515 (2012).
Liu, B. et al. Intermittent fasting improves glucose tolerance and promotes adipose tissue remodeling in male mice Fed a High-Fat Diet. Endocrinology 160, 169–180 (2019).
Licholai, J. A. et al. Why do mice Overeat High-Fat diets? How high-Fat Diet alters the regulation of Daily Caloric Intake in mice. Obesity 26, 1026–1033 (2018).
Riat, A. et al. Ramadan Fasting in Germany (17–18 h/Day): effect on cortisol and brain-derived neurotrophic factor in Association with Mood and Body Composition parameters. Front. Nutr. 8, 697920 (2021).
Zhao, L. et al. A combination of quercetin and resveratrol reduces obesity in high-fat diet-fed rats by modulation of gut microbiota. Food Funct. 8, 4644–4656 (2017).
Patterson, R. E. & Sears, D. D. Metabolic effects of Intermittent Fasting. Annu. Rev. Nutr. 37, 371–393 (2017).
Fernando, H., Zibellini, J., Harris, R., Seimon, R. & Sainsbury, A. Effect of Ramadan Fasting on Weight and Body Composition in healthy non-athlete adults: a systematic review and Meta-analysis. Nutrients 11, 478 (2019).
Kul, S., Savaş, E., Öztürk, Z. A. & Karadağ, G. Does Ramadan Fasting Alter Body Weight and blood lipids and fasting blood glucose in a healthy Population? A Meta-analysis. J. Relig. Health 53, 929–942 (2014).
Sadeghirad, B., Motaghipisheh, S., Kolahdooz, F., Zahedi, M. J. & Haghdoost, A. A. Islamic fasting and weight loss: a systematic review and meta-analysis. Public. Health Nutr. 17, 396–406 (2014).
Yu, S. L., Kuan, W. P., Wong, C. K., Li, E. K. & Tam, L. S. Immunopathological Roles of Cytokines, Chemokines, Signaling Molecules, and Pattern-Recognition Receptors in Systemic Lupus Erythematosus. J. Immunol. Res. 2012, e715190 (2012).
Rea, I. M. et al. Age and Age-Related diseases: role of inflammation triggers and cytokines. Front. Immunol. 9 (2018).
Ershler, W. B. & Keller, E. T. Age-Associated increased Interleukin-6 gene expression, late-Life diseases, and Frailty. Annu. Rev. Med. 51, 245–270 (2000).
Alemán, H., Esparza, J., Ramirez, F. A., Astiazaran, H. & Payette, H. Longitudinal evidence on the association between interleukin-6 and C-reactive protein with the loss of total appendicular skeletal muscle in free-living older men and women. Age Ageing 40, 469–475 (2011).
Soerensen, M. et al. Evidence from case–control and longitudinal studies supports associations of genetic variation in APOE, CETP, and IL6 with human longevity. Age 35, 487–500 (2013).
Di Bona, D. et al. Effect of interleukin-6 polymorphisms on human longevity: a systematic review and meta-analysis. Ageing Res. Rev. 8, 36–42 (2009).
Davies, R. & Choy, E. Clinical experience of IL-6 blockade in rheumatic diseases—implications on IL-6 biology and disease pathogenesis. Semin Immunol. 26, 97–104 (2014).
Kao, T. W. & Huang, C. C. Inflammatory Burden and Immunomodulative therapeutics of Cardiovascular diseases. Int. J. Mol. Sci. 23, 804 (2022).
Lio, D. et al. Inflammation, genetics, and longevity: further studies on the protective effects in men of IL-10 – 1082 promoter SNP and its interaction with TNF-α – 308 promoter SNP. J. Med. Genet. 40, 296–299 (2003).
Ross, O. A. et al. Study of age-association with cytokine gene polymorphisms in an aged Irish population. Mech. Ageing Dev. 124, 199–206 (2003).
Ruparelia, N., Chai, J. T., Fisher, E. A. & Choudhury, R. P. Inflammatory processes in cardiovascular disease: a route to targeted therapies. Nat. Rev. Cardiol. 14, 133–144 (2017).
Almeneessier, A. S. et al. The effects of diurnal intermittent fasting on proinflammatory cytokine levels while controlling for sleep/wake pattern, meal composition and energy expenditure. PLoS One 14, e0226034 (2019).
Faris, M. A. I. E., Jahrami, H. A., Obaideen, A. A. & Madkour, M. I. Impact of diurnal intermittent fasting during Ramadan on inflammatory and oxidative stress markers in healthy people: systematic review and meta-analysis. J. Nutr. Intermed. Metab. 15, 18–26 (2019).
Faris, E. et al. Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutr. Res. 32, 947–955 (2012).
Ünalacak, M., Kara, İ. H., Baltaci, D., Erdem, Ö. & Bucaktepe, P. G. E. Effects of Ramadan Fasting on biochemical and hematological parameters and cytokines in healthy and obese individuals. Metab. Syndr. Relat. Disord. 9, 157–161 (2011).
Nematy, M. et al. Effects of Ramadan fasting on cardiovascular risk factors: a prospective observational study. Nutr. J. 11, 69 (2012).
Madkour, M. I. et al. Ramadan diurnal intermittent fasting modulates SOD2, TFAM, Nrf2, and sirtuins (SIRT1, SIRT3) gene expressions in subjects with overweight and obesity. Diabetes Res. Clin. Pract. 155, 107801 (2019).
Mulas, A. et al. Effect of intermittent fasting on circulating inflammatory markers in obesity: a review of human trials. Front. Nutr. 10, 1146924 (2023).
Jahrami, H. A., Alsibai, J., Clark, C. C. T., Faris, M. & A.-I. E. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur. J. Nutr. 59, 2291–2316 (2020).
Ouyang, W., Rutz, S., Crellin, N. K., Valdez, P. A. & Hymowitz, S. G. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu. Rev. Immunol. 29, 71–109 (2011).
Juárez-Cedillo, T. et al. Interleukin 10 gene polymorphisms and frailty syndrome in elderly Mexican people: (Sadem study). Mol. Genet. Genom. Med. 7, (2019).
Santos, A. L. & Sinha, S. Obesity and aging: molecular mechanisms and therapeutic approaches. Ageing Res. Rev. 67, 101268 (2021).
Safaei, M., Sundararajan, E. A., Driss, M. & Boulila, W. Shapi’i, A. A systematic literature review on obesity: understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput. Biol. Med. 136, 104754 (2021).
Martyniak, K. & Masternak, M. M. Changes in adipose tissue cellular composition during obesity and aging as a cause of metabolic dysregulation. Exp. Gerontol. 94, 59–63 (2017).
Schottelius, A. J. G., Mayo, M. W., Sartor, R. B. & Baldwin, A. S. Interleukin-10 signaling blocks inhibitor of κB kinase activity and nuclear factor κB DNA binding *. J. Biol. Chem. 274, 31868–31874 (1999).
Lavallee, C. M., Bruno, A., Ma, C. & Raman, M. The role of intermittent fasting in the management of nonalcoholic fatty liver disease: a narrative review. Nutrients 14, 4655 (2022).
Reyes-Farias, M., Fos-Domenech, J., Serra, D. & Herrero, L. Sánchez-Infantes, D. White adipose tissue dysfunction in obesity and aging. Biochem. Pharmacol. 192, 114723 (2021).
Li, Z., Huang, L., Luo, Y., Yu, B. & Tian, G. Effects and possible mechanisms of intermittent fasting on health and disease: a narrative review. Nutr. Rev. Nuad 026 https://doi.org/10.1093/nutrit/nuad026 (2023).
Faris, E. et al. Effect of Ramadan diurnal fasting on visceral adiposity and serum adipokines in overweight and obese individuals. Diabetes Res. Clin. Pract. 153, 166–175 (2019).
Pellegrini, M. et al. Effects of time-restricted feeding on body weight and metabolism. A systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 21, 17–33 (2020).
Matoba, S. et al. p53 regulates mitochondrial respiration. Science 312, 1650–1653 (2006).
Saleem, A., Adhihetty, P. J. & Hood, D. A. Role of p53 in mitochondrial biogenesis and apoptosis in skeletal muscle. Physiol. Genom. 37, 58–66 (2009).
Hu, W. et al. Glutaminase 2, a novel p53 target gene regulating energy metabolism and antioxidant function. Proc. Natl. Acad. Sci. 107, 7455–7460 (2010).
Suzuki, S. et al. Phosphate-activated glutaminase (GLS2), a p53-inducible regulator of glutamine metabolism and reactive oxygen species. Proc. Natl. Acad. Sci. 107, 7461–7466 (2010).
Feng, Z., Lin, M. & Wu, R. The regulation of aging and longevity: a new and complex role of p53. Genes Cancer 2, 443–452 (2011).
Czaja, M. J., et al. Functions of autophagy in normal and diseased liver. Autophagy 9, 1131-1158 (2013).
Becker, J. B. et al. Strategies and methods for research on sex differences in brain and behavior. Endocrinology 146, 1650-1673 (2005).
Amengual-Cladera, E., Lladó, I., Gianotti, M. & Proenza, A. M. Sex differences in the effect of high-fat diet feeding on rat white adipose tissue mitochondrial function and insulin sensitivity. Metabolism 61, 1108–1117 (2012).
Hardie, D. G. AMP-activated protein kinase: an energy sensor that regulates all aspects of cell function. Genes Dev. 25, 1895–1908. https://doi.org/10.1101/gad.17420111 (2011).
Viollet, B. et al. Targeting AMP-activated protein kinase as a novel therapeutic approach for the treatment of metabolic disorders. Diabetes Metab. 33, 395–402. https://doi.org/10.1016/j.diabet.2007.10.004 (2007).
Acknowledgements
We thank Ahmad Almnaizel for the analysis of blood samples.
Funding
Researchers Supporting Project number (RSP2024R338), King Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
Conceptualization, A.A.A., M.H.A., A.S.A. and A.S.B.; Methodology, A.A.A., M.H.A., N.M.A., R.A., N.M.A.-Y and H.S.A. ; Validation, M.H.A. and A.S.B.; Formal analysis, A.A.A. and B.A.A.; Resources, A.S.A.; Investigation, A.A.A.; Data curation, A.A.A . and M.F.A.; Writing—original draft preparation, A.A.A.; writing—review and editing, M.H.A. and A.S.B. ; Supervision, A.S.A., A.S.B., and M.H.A.; project administration, A.S.A., M.H.A. and A.S.B.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Institutional Animal Care and Use Committee (IACUC) of King Saud University granted approval for the experimental protocol. (Ref. No.: KSU-SE-21-66).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alasmari, A.A., Alhussain, M.H., Al-Khalifah, A.S. et al. Ramadan fasting model modulates biomarkers of longevity and metabolism in male obese and non-obese rats. Sci Rep 14, 28731 (2024). https://doi.org/10.1038/s41598-024-79557-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-79557-y
Keywords
This article is cited by
-
The effects of time-restricted feeding on early vascular, liver, and renal structural changes, oxidative stress, and inflammation in obese rats
Scientific Reports (2025)
-
The combined effects of high-intensity interval training and time-restricted feeding on the AKT/FOXO1/PEPCK pathway in diabetic rats
Scientific Reports (2025)