Abstract
In this randomized controlled trial, we assessed the effects of three consecutive intra-silicone oil (SO) injections of methotrexate (MTX) on the outcomes of surgery for proliferative vitreoretinopathy grade C (PVR-C). Seventy-four eyes of 74 patients with PVR-C were included. Of these, 37 eyes were assigned to the MTX group and 37 eyes to the control group. Fourteen patients failed to comply with the 6-month follow-up period. All eyes underwent vitrectomy and SO injection. In the MTX group, 250 µg MTX was injected into the SO after surgery and at weeks 3 and 6 postoperatively. The primary outcome was the retinal reattachment rate at 6 months. The secondary outcomes included limited PVR recurrence and adverse events. Retinal reattachment was achieved in 22 eyes (73.3%) in the MTX group and 23 eyes (76.7%) in the control group (difference: -3.4%, 95% CI: -25.2–18.5%). Limited PVR recurrence was observed in one eye (4.5%) in the MTX group versus nine eyes (39.1%) in the control group at 6 months (P = 0.01). No adverse effects were observed. Adjunctive treatment with three consecutive applications of intra-SO MTX did not reveal a significant effect on the retinal re-detachment rate but could statistically significantly reduce limited PVR recurrence.
Trial registration: http//ClinicalTrials.gov NCT04482543, 22/07/2020.
Similar content being viewed by others
Introduction
Proliferative vitreoretinopathy (PVR) is the main cause of rhegmatogenous retinal detachment (RRD) surgery failure and is characterized by the proliferation and migration of retinal pigment epithelial (RPE) and glial cells on the surface of, within, and underneath the retina1,2,3. Despite recent surgical advancements, PVR following RRD repair remains a major challenge4. Previous studies have revealed an association between PVR and increased concentrations of pro-inflammatory cytokines and growth factors in the vitreous3,4,5,6. Cellular proliferation continues for 6–8 weeks after RRD surgery; therefore, an effective treatment must inhibit this process for at least 45–60 days3.
Various anti-inflammatory and anti-metabolic drugs have been used as adjuvants to prevent and treat PVR. Multiple clinical studies have investigated the efficacy of daunorubicin, steroids, colchicine, 5-fluorouracil (5-FU), low-molecular-weight heparin (LMWH) and bevacizumab7,8,9,10,11,12. However, these agents exhibit limited efficacy13. Another drug that has been considered is methotrexate (MTX), an anti-inflammatory and anti-proliferative agent14,15,16. Its anti-inflammatory effect is regulated by adenosine and inhibition of 5-aminoimidazole-4-carboxamide ribonucleotide transformylase16. MTX is a potent anti-inflammatory agent and its mechanism of action differs from that of other drugs used in the management of PVR17. This feature, along with the antiproliferative and antifibrotic effects of MTX, may make it a suitable candidate for the prevention and treatment of PVR. Although a single injection of MTX does not reduce the rate of PVR-induced recurrent RD18, other studies have reported promising effects of multiple intravitreal injections of MTX after RRD surgery19,20. This multicenter randomized controlled trial (RCT) aimed to evaluate the efficacy of multiple MTX intra-silicone oil (intra-SO) injections in the management of PVR grade C (PVR-C).
Results
A total of 74 eyes of 74 patients were included in this study. Basic information on the study participants is presented in Table 1. The two study groups were comparable in terms of demographic, preoperative, and intraoperative factors (Table 1). Seven patients in each group did not comply with the 6-month follow-up and statistical analyses were performed on 60 eyes (Fig. 1).
Retinal reattachment rate
Retinal reattachment was achieved in 45 eyes (75.0%) at 6 months after surgery. Of these, 22 (73.3%) eyes were in the MTX group and 23 (76.7%) were in the control group (risk difference: -3.4%, 95% CI: -25.2–18.5%, RR:0.95, 95% CI: 0.71–1.28, P = 0.766). Retinal re-detachment due to PVR recurrence occurred in 15 (25%) eyes, consisting of 8 (26.7%) eyes in the MTX group and 7 (23.3%) in the control group (risk difference:3.4%, 95% CI: -18.5–25.2%, RR:1.14, 95% CI: 0.47–2.75, P = 0.766). The difference in the final retinal reattachment rates between the two groups was not statistically significant (P = 0.990).
Of the 47 eyes with reattached retina at month 3, the SO was removed in 45 eyes consisting of 21 eyes in the MTX group and 24 eyes in the control group (one patient in each group declined SO removal). In the MTX group, the retina remained attached in all eyes following SO removal. In the control group, retinal re-detachment occurred in two eyes after SO removal; the retina remained attached in the other 22 eyes up to 6 months after SO removal.
The mean survival times in the control and MTX groups were 152.03 ± 10.08 and 137.8 ± 12.86 days, respectively. As shown in the Kaplan–Meier survival curve, there was no statistically significant difference between the two groups in terms of survival rate (log-rank test: 0.164, P = 0.685) (Fig. 2). Table 2 shows the cumulative survival rate of 76.78% and 73.32% in the control and MTX groups, respectively, at month 6.
Limited PVR recurrence and macular pucker formation
A statistically significant difference was observed between the two groups at 3 months in terms of limited PVR recurrence manifesting as retinal shortening due to membrane re-proliferation without retinal re-detachment: one (4.5%) eye in the MTX group versus six (26.1%) eyes in the control group (P = 0.04). This difference increased up to 6 months and membrane re-proliferation was observed in one eye (4.5%) in the MTX group versus nine eyes (39.1%) in the control group at the last follow-up examination (P = 0.01) (Table 3).
Four (18.2%) eyes in the MTX group and nine (39.1%) eyes in the control group presented with macular puckers at 6 months (P = 0.189) (Table 3). Internal limiting membrane (ILM) peeling showed a statistically significant preventive effect on the rate of macular pucker formation in eyes with reattached retinas at 6 months in both groups (P = 0.025). There was no significant difference between the MTX and control groups in terms of the effect of ILM peeling on the macular pucker rate (26.7% vs. 15%, P = 0.391) (Fig. 2). After adjustment for gender, anterior and posterior PVR-C, history of previous vitrectomy, number of laser spots, and retinotomy/retinectomy, patients with ILM peeling had decreased odds of macular pucker compared to those without ILM peeling (OR = 0.12, 95% CI: 0.01–1.00).
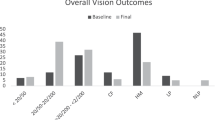
Visual outcome and intraocular pressure
The logarithm of the minimum angle of resolution (logMAR) best-corrected visual acuity (BCVA) improved from 2.18 ± 0.72 and 2.34 ± 0.62 to 1.37 ± 0.64 and 1.37 ± 0.79 in MTX and control groups, respectively, at the final follow-up visit. Although BCVA showed improvement 6 months after surgery in both groups, the difference was not statistically significant between the groups (P = 0.99).
In eyes with a reattached retina at 6 months, BCVA was significantly lower in eyes with macular pucker (1.74 ± 0.67 logMAR) than in eyes without macular epiretinal membrane (1.19 ± 0.67 logMAR) (mean difference: -0.56, 95% CI: 1.00 to -0.11, P = 0.014).
In both groups, the intraocular pressure (IOP) increased after surgery, with no significant difference between the two groups at different time points (mean difference: -2.53, 95% CI: -5.73–0.67, P = 0.118).
Adverse effects
No complications due to repeated MTX injections were observed during the 6-month follow-up period.
Post hoc power analysis
To achieve a study power of 85% and to be able to demonstrate a 30% difference in retinal reattachment rate between the study groups, a sample size of 37 for each group was initially estimated. However, due to the loss of follow-up, the final sample size was reduced to 30 patients in each group, reducing the study power to 71%.
Discussion
This multicenter RCT revealed that intra-SO injection of preservative-free MTX administered at the end of surgery in eyes with RRD complicated by PVR-C and repeated injections at weeks 3 and 6 did not reduce the risk of retinal re-detachment. However, this therapeutic approach could ameliorate the proliferative process, manifesting as a decreased rate of postsurgical membrane re-proliferation, and limited PVR recurrence and macular pucker formation. A reduction in macular pucker had a significant positive effect on postoperative BCVA.
Following the occurrence of RRD, the PVR cascade begins with the breakdown of the blood-ocular barrier, followed by the migration of RPE and glial cells into the vitreous cavity and onto the retinal surface. The influx of cytokines, growth factors, and inflammatory cells leads to increased mitogenic and chemotactic activity in the vitreous cavity, followed by the growth and contraction of cellular membranes. Contraction of these membranes leads to the formation of fixed folds and retinal re-detachment. Owing to the complexity of the PVR process, pharmacological treatment remains a challenging and unsolved issue. Several drugs have been investigated for the prevention and treatment of PVR. Some of these drugs have shown promising results in animal models but are not sufficiently effective in humans. Targeting only part of the PVR cascade could be the main reason for this therapeutic failure. To compensate for this deficiency, a cocktail comprising LMWH and 5-FU infusion during vitrectomy was evaluated for PVR, with initial promising results21. However, this combined modality yielded inconsistent results in further studies, raising concerns about its safety22.
In recent years, hope has arisen regarding the possible role of methotrexate in PVR management, owing to its multi-effect mechanism of action. MTX exerts anti-inflammatory and antiproliferative effects by enhancing the release of extracellular adenosine, which inhibits macrophage activation, leukocyte recruitment, and neutrophil adhesion and can theoretically affect different stages of the PVR process23. In an in vitro study on a patient-derived model of PVR, MTX reduced the proliferation and induced the regulated death of PVR cells. However, it did not affect the cell migration24. Hardwig et al. reported the safety of intravitreal injection of 400 µg MTX in ocular diseases other than primary central nervous system lymphoma25. They also demonstrated that the cumulative dose of up to 1200 µg could be safe in silicone-filled eyes26. Sadaka et al. investigated intravitreal MTX infusion (IMI) during vitrectomy in an interventional case series. They reported that IMI may reduce the risk of retinal re-detachment in eyes at high risk for PVR development, including eyes with recurrent PVR and a history of intraocular inflammation27. Jahangir et al. performed a similar study with no control group on MTX infusion in advanced PVR28. In a comparative non-randomized study, El Baha et al. reported the preventive role of MTX infusion; however, no therapeutic advantage was observed in eyes with established PVR29. In a non-randomized comparative study, Falavarjani et al. reported the results of a single intra-SO injection of 250 µg MTX administered at the end of surgery in eyes with RRD and PVR-C. The MTX group had a higher anatomical success rate than the control group; however, this difference did not reach statistical significance18. In a prospective case series, Nourinia et al. injected 250 µg MTX into the SO-filled vitreous cavity at the end of surgery and again at weeks 3 and 6 to address the PVR cascade more efficiently and extend the possible therapeutic effects of MTX30. Considering the promising results of this pilot study, the present RCT was designed.
Different frequencies and doses of MTX injections have been used to manage PVR; these vary from weekly to every three weeks and 100–400 micrograms. Clearance of MTX may be reduced in SO filled eyes but there is no pharmacokinetic data in this regard. In a small retrospective case series, Benner et al. administered five intraocular injections of MTX at 2-week intervals; a 100 µg dose was used in most cases31. Superficial keratopathy was observed in one eye. In a retrospective study, Roca et al. went further with weekly injections of MTX after surgery for PVR32. There was a statistically significant difference between patients who received four to eight intravitreal injections of MTX and controls with no MTX injections in terms of the retinal reattachment rate (86% vs. 22.2%, P = 0.04). Corneal epitheliopathy was not observed in the MTX group. Elliot and Stryjewski invented and patented intravitreal MTX 0.8%, called ADX-2191, which was applied in the GUARD study, a phase 3, multicenter, randomized trial in the United States33,34. Patients in the treatment group were scheduled to receive ADX-2191 at the conclusion of surgery or on postoperative day 1, followed by weekly injections for 8 weeks and then every other week from weeks 8 to 16, for a total of 13 injections. The primary outcome was the rate of retinal re-detachment due to PVR requiring reoperation within 24 weeks of the study period. Recently, in a small retrospective case series, Ahmed and Stewart showed that MTX administered in multiple series may be a safe and effective adjunct to surgery for preventing recurrent PVR, even in patients with refractory disease35. In their study, patients received nine intravitreal MTX injections. Each series consisted of a single intraoperative MTX injection, followed by eight postoperative MTX injections weekly. None of the patients experienced treatment-limiting side effects35. We decided to administer MTX (250 micrograms) at three-week intervals based on our previous study and balancing its therapeutic versus adverse effects30.
Survival analysis revealed that there was no statistically significant difference between the two groups regarding the time of surgical failure due to retinal re-detachment. The removal of SO 3 months after retinal reattachment did not have a significant effect on the surgical outcome. Retinal shortening following RRD may be induced by epiretinal membrane proliferation and/or intraretinal PVR. This RCT showed that the rate of postoperative limited PVR, presenting as retinal shortening without retinal re-detachment, decreased significantly in the MTX group. The rate of macular epiretinal membrane formation leading to macular puckering was also reduced in the MTX group compared to that in the control group, although this difference was not statistically significant. In addition, ILM peeling had a preventive effect on the occurrence of postoperative macular puckers in both groups. Similar results have been reported in eyes undergoing vitrectomy for RRD and PVR36,37. The reduced rate of macular puckering had a positive effect on the final BCVA.
The total rate of complete retinal reattachment in this study was 75%, which could be due to the inclusion of patients with advanced PVR. The nearly 20% patient dropout rate was a shortcoming for the current study. This could be attributed to the coronavirus disease pandemic, which has affected research activities, specifically RCTs worldwide38. Despite the relatively large extent of loss to follow-up (LTFU), the distributions were equal between the two groups. This minimized the potential biasing effects of LTFU39.
Considering the post hoc power analysis and the fact the observed difference in retinal re-attachment rates was actually not in favor of the treatment group and also regarding the bounds of 95% CI (-25.2 to 18.5%), it seems evident that no statistically or clinically meaningful difference is conceivable based on the original sample size calculation. The study, albeit acknowledging its limitations, suggests that MTX adjunctive therapy did not significantly alter the retinal reattachment rate compared to the control group.
In summary, the results of this multicenter RCT showed that three intra-SO injections of 250 µg MTX had a modest beneficial effect on the anatomical results of surgery for the management of PVR-C, with no alarming adverse effects. Further prospective controlled studies are required to assess the benefits and risks of increasing the number of MTX injections.
Methods
In this multicenter parallel two-arm RCT, patients with RRD and PVR-C were recruited from August 2020 to March 2022. The study protocol adhered to the Declaration of Helsinki and was approved by the Ethics Committee of the Ophthalmic Research Center, Research Institute for Ophthalmology and Vision Science, Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.ORC.REC.1399.007). Informed consent was obtained from all participants. The RCT was registered at http://ClinicalTrials.gov (NCT04482543, 22/07/2020).
Participants
The inclusion criteria were RRD associated with PVR-C with or without a history of previous surgery for retinal detachment. The severity of PVR was graded according to the updated classification of the Retina Society40. Patients were recruited from nine medical centers in Tehran, Mashhad, and Tabriz. Those with diabetic retinopathy, retinal vascular occlusions, giant retinal tears, chronic uveitis, glaucoma, macular diseases, and a history of intraocular injections or penetrating ocular trauma were excluded. Patients aged less than 18 years and pregnant and monocular patients were also excluded from the study.
Randomization and masking
Patients were randomly assigned to either the MTX or control group in a 1:1 ratio. A simple randomization method was used via an online randomization website (Research Randomizer, https://www.randomizer.org). Collaborators from all contributing centers shared a unique electronic randomization table. Surgeons were exposed to the groups immediately before the completion of the surgical procedure and after the injection of SO.
The assessors who performed the postoperative ocular examinations were blinded. No sham injections were administered in the control group.
Outcome measures
The primary outcome measure was the complete retinal reattachment rate at 6 months. Secondary outcome measures included membrane re-proliferation leading to limited PVR and retinal foreshortening without retinal re-detachment, macular pucker secondary to the epimacular membrane, BCVA, IOP, and adverse effects associated with repeated injections of MTX. The effect of a macular pucker on BCVA and the effect of the ILM peeling on macular pucker formation was also investigated.
Sample size
Considering the presumed retinal reattachment rate of 60% in eyes undergoing vitrectomy for the management of PVR-C, an estimated increase in this rate to 90% with adjunctive therapy using MTX, and a probable dropout rate of 10%, a total sample size of 74 (37 eyes in each group) was calculated to detect a significant difference of 5% (2-sided) with a study power of 85%.
Study procedures and interventions
A comprehensive eye examination was performed. The extent and location of the PVR-C, previous scleral buckling or vitrectomy, and the type of previous internal tamponade were recorded. All participants underwent a standard three-port 23- or 25-gauge pars plana vitrectomy. If there was pre-existing SO, it was removed using a viscous fluid extractor. All epiretinal membranes were peeled off the retinal surface using forceps. The subretinal membranes were removed via access retinotomy. In cases of intraretinal PVR and retinal shortening, relaxing retinotomy/retinectomy was performed. The number of laser spots, need for retinotomy/retinectomy, peeling of the ILM, removal of the lens with or without intraocular lens implantation, and placement of a circumferential scleral buckle were recorded as intraoperative data. Intraoperative laser applications were divided into low (less than 1000 spots) versus high (1000 or more spots). At the surgeon’s discretion, 1000–1300 or 5000–5700 centistokes SO were injected for internal tamponade.
In the MTX group, 250 µg/0.1 ml preservative-free MTX (Ebetrex, Ebewe Pharma Ges.m.b.H Nfg.KG, Austria) was injected trans pars plana into the inferior part of the SO-filled vitreous cavity at the end of surgery. Sub-Tenon injection of triamcinolone acetonide was avoided. No systemic steroids were prescribed after surgery. Intra-SO injections of the same dose of MTX were repeated at weeks 3 and 6 postoperatively.
Follow-up
Postoperative follow-up was scheduled for six months. The participants were scheduled to be examined at 1, 3, 6, 12, 16, and 24 weeks after surgery. Examinations included assessment of BCVA, IOP, retinal status, and possible MTX side effects, including corneal epitheliopathy, signs of early SO emulsification, and intraocular inflammation. For patients with a successfully attached retina, SO removal was scheduled at month 3.
Statistical analysis
Statistical analyses were performed using SPSS software version 26.0 (IBM Corp, Armonk, NY). Chi-square and Fisher’s exact tests were used to analyze nominal variables. The t-test was used to compare numeric data. The Kaplan–Meier curve and log-rank test were used to examine the difference in the time of the occurrence of retinal re-detachment between the control and MTX groups. Logistic regression models were used to explore the relationship between ILM peeling and the occurrence of macular pucker, adjusted for sex, anterior and posterior PVR-C grades, history of previous vitrectomy, number of laser spots, and retinotomy/retinectomy. Statistical significance was set at P < 0.05.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Adelman, R. A. et al. Clinical variables associated with failure of retinal detachment repair: The European vitreo-retinal society retinal detachment study report number 4. Ophthalmology. 121, 1715–1719 (2014).
Pastor, J. C. Proliferative vitreoretinopathy: An overview. Surv. Ophthalmol. 43, 3–18 (1998).
Pastor, J. C. et al. Proliferative vitreoretinopathy: A new concept of disease pathogenesis and practical consequences. Prog Retin Eye Res. 51, 125–155 (2016).
Pennock, S. et al. Is neutralizing vitreal growth factors a viable strategy to prevent proliferative vitreoretinopathy? Prog Retin Eye Res. .40, 16–34 (2014).
Ricker, L. J. et al. Interleukin and growth factor levels in subretinal fluid in rhegmatogenous retinal detachment: A case-control study. PloS One. 6, e19141 (2011).
Roldán-Pallarés, M. et al. Retinal detachment: visual acuity and subretinal immunoreactive endothelin-1. J. Fr. Ophthalmol. 31, 36–41 (2008).
Wiedemann, P. et al. Adjunctive daunorubicin in the treatment of proliferative vitreoretinopathy: Results of a multicenter clinical trial. Am. J. Ophthalmol. 126, 550–559 (1998).
Dehghan, M. H. et al. Effect of oral prednisolone on visual outcomes and complications after scleral buckling. Eur. J. Ophthalmol. 20, 419–423 (2010).
Ahmadieh, H. et al. Triamcinolone acetonide in silicone-filled eyes as adjunctive treatment for proliferative vitreoretinopathy: A randomized clinical trial. Ophthalmology. 115, 1938–1943 (2008).
Ahmadieh, H. et al. Oral colchicine for prevention of proliferative vitreoretinopathy : A randomized clinical trial. Acta Ophthalmol. 93, e171–172 (2015).
Garcia, R. A. et al. Combined 5-fluorouracil, low-molecular-weight heparin, and silicone oil in the management of complicated retinal detachment with proliferative vitreoretinopathy grade C. Ophthalmic Surg. Lasers Imaging. 38, 276–282 (2007).
Tousi, A. et al. Intravitreal injection of bevacizumab in primary vitrectomy to decrease the rate of retinal redetachment: A randomized pilot study. J. Ophthalmic Vis. Res. 11, 271–276 (2016).
Sadaka, A. et al. Proliferative vitreoretinopathy: Current and emerging treatments. Clin. Ophthalmol. 6, 1325–1333 (2012).
Gangaputra, S. et al. Methotrexate for ocular inflammatory diseases. Ophthalmology. 116, 2188–2198 (2009).
Frenkel, S. et al. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br. J. Ophthalmol. 92, 383–388 (2008).
Cronstein, B. N. Low-dose methotrexate: a mainstay in the treatment of rheumatoid arthritis. Pharmacol. Rev. 57, 163–172 (2005).
McAllister., M. A. et al. Intraocular methotrexate for the treatment and prevention of proliferative vitreoretinopathy: A review. J. Vitreoretin Dis. 7, 144–153 (2022).
Falavarjani, K. G. et al. Intra-silicone oil injection of methotrexate in retinal reattachment surgery for proliferative vitreoretinopathy. Ocul Immunol. Inflamm. 28, 513–516 (2020).
Balas, M. et al. Intravitreal methotrexate for the prevention and treatment of proliferative vitreoretinopathy in rhegmatogenous retinal detachment: A systematic review. Ophthalmic Surg. Lasers Imaging Retina. 53, 561–568 (2022).
Abdi, F. et al. Intravitreal methotrexate. J. Ophthalmic Vis. Res. 16, 657–669 (2021).
Charteris, D. G. et al. A randomized controlled trial of combined 5-fluorouracil and low-molecular-weight heparin in management of established proliferative vitreoretinopathy. Ophthalmology. 111, 2240–2245 (2004).
Chen, C. et al. Combined 5-fluorouracil and low molecular weight heparin for the prevention of postoperative proliferative vitreoretinopathy in patients with retinal detachment: A meta-analysis. Front. Med. 8, 790460 (2021).
Jolivet, J. et al. The pharmacology and clinical use of methotrexate. N Engl. J. Med. 309, 1094–1104 (1983).
Amarnani, D. et al. Effect of methotrexate on an in vitro patient-derived model of proliferative vitreoretinopathy. Invest. Ophthalmol. Vis. Sci. 58, 3940–3949 (2017).
Hardwig, P. W. et al. Intraocular methotrexate in ocular diseases other than primary central nervous system lymphoma. Am. J. Ophthalmol. 142, 883–885 (2006).
Hardwig, P. W. et al. The safety of intraocular methotrexate in silicone-filled eyes. Retina. 28, 1082–1086 (2008).
Sadaka, A. et al. Intravitreal methotrexate infusion for proliferative vitreoretinopathy. Clin. Ophthalmol. 10, 1811–1817 (2016).
Jahangir, S. et al. Use of intravitreal methotrexate infusion in complicated retinal detachment for prevention of proliferative vitreoretinopathy in a pilot study. Cureus. 13, e17439 (2021).
El Baha, S. et al. Anatomical and functional outcomes of vitrectomy with/without intravitreal methotrexate infusion for management of proliferative vitreoretinopathy secondary to rhegmatogenous retinal detachment. J. Ophthalmol. 3648134 (2021).
Nourinia, R. et al. Repeated injection of methotrexate into silicone oil-filled eyes for grade C proliferative vitreoretinopathy: A pilot study. Ophthalmologica. 242, 113–117 (2019).
Benner, J. D. et al. Intravitreal methotrexate for the treatment of proliferative vitreoretinopathy. BMJ Open. Ophthalmol. 4, e000293 (2019).
Roca, J. A. et al. Adjunctive serial post-operative intravitreal methotrexate injections in the management of advanced proliferative vitreoretinopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 259, 2913–2917 (2021).
Eliott, D. et al. Methotrexate for proliferative vitreoretinopathy. US Patent 2017. Accessed May 4, (2022). https://patents.google.com/patent/US10098884B2/en
The, G. U. A. R. D. Trial part 1: a phase 3 clinical trial for prevention of proliferative vitreoretinopathy. Clinicaltrials.gov identifier NCT04136366. (2022). https://clinicaltrials.gov/ct2/show/NCT04136366. Accessed May 4.
Ahmad, T. R. et al. Tolerability and ffficacy of multiple series of intravitreal methotrexate injections for complex retinal detachment associated with proliferative vitreoretinopathy. Future Pharmacol. 3, 464–472 (2023).
Odrobina, D. et al. Internal limiting membrane peeling as prophylaxis of macular pucker formation in eyes undergoing retinectomy for severe proliferative vitreoretinopathy. Retina. 32, 226–231 (2012).
Fallico, M. et al. Internal limiting membrane peeling versus no peeling during primary vitrectomy for rhegmatogenous retinal detachment: A systematic review and meta-analysis. PLoS One. 13, e0201010 (2018).
Audisio, K. et al. Impact of the COVID-19 pandemic on non-COVID-19 clinical trials. J. Cardiovasc. Dev. Dis. 9, 19 (2022).
Akl, E. A. et al. LOST to follow-up information in trials (LOST-IT): A protocol on the potential impact. Trials. 10, 40 (2009).
Machemer, R. et al. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am. J. Ophthalmol. 112, 159–165 (1991).
Acknowledgements
We would greatly appreciate Dr. Kiana Hassanpour for her valuable help on this project.
Author information
Authors and Affiliations
Contributions
Research design: H.A, R.NData acquisition and/or research execution: R.N, S.S, M.M, H.R, M.R.A.A, K.G.F, A.R, S.K, S.F, N.E, E.K, H.N, N.S, N.H, M.H, M.A, F.A, A.R, S.M, M.H.J.B, H.S, P.A, K.F, Ma.M, N.M, B.K, H.A.Data analysis and/or interpretation: R.N, S.S, M.M, H.R, M.R.A.A, K.G.F, A.R, S.K, S.F, N.E, E.K, H.N, N.S, N.H, M.H, M.A, F.A, A.R, S.M, M.H.J.B, H.S, P.A, K.F, Ma.M, N.M, B.K, H.A, S.K.M, F.H, Z.K, M.YManuscript preparation: R.N, S.S, M.M, H.R, M.R.A.A, K.G.F, A.R, S.K, S.F, N.E, E.K, H.N, N.S, N.H, M.H, M.A, F.A, A.R, S.M, M.H.J.B, H.S, P.A, K.F, Ma.M, N.M, B.K, H.A, S.K.M, F.H, Z.K., M.YSubmitted version approval: R.N, S.S, M.M, H.R, M.R.A.A, K.G.F, A.R, S.K, S.F, N.E, E.K, H.N, N.S, N.H, M.H, M.A, F.A, A.R, S.M, M.H.J.B, H.S, P.A, K.F, Ma.M, N.M, B.K, H.A, S.K.M, F.H, Z.K., M.YR.N, S.S, M.M, H.R, M.R.A.A, K.G.F, A.R, S.K, S.F, N.E, E.K, H.N, N.S, N.H, M.H, M.A, F.A, A.R, S.M, M.H.J.B, H.S, P.A, K.F, Ma.M, N.M, B.K, H.A, S.K.M, F.H, Z.K., M.Y have agreed both to be personally accountable for their contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which they were not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was obtained (IR.SBMU.ORC.REC.1399.007) from the Ethics Committee of the Ophthalmic Research Center at the Research Institute for Ophthalmology and Vision Science, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Informed consent was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nourinia, R., Safi, S., Mohammadpour, M. et al. Effects of repeated intra-silicone oil injections of methotrexate on proliferative vitreoretinopathy grade C: a multicenter randomized controlled trial. Sci Rep 14, 28842 (2024). https://doi.org/10.1038/s41598-024-79708-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-79708-1