Abstract
Adverse Childhood Experiences (ACEs) may have an impact on cognitive disability through multiple pathways. Frequent Mental Distress (FMD) could result in cognitive disability through different aspects, but the potential mediating role of FMD in the associations remained unclear. So we aimed to investigate not only the association between self-reported ACEs and cognitive disability, but also the mediating effect of FMD between ACEs and cognitive disability. A cross-sectional analysis of respondents aged 18–25 years old in the 2020 and 2021 Behavioral Risk Factor Surveillance System (BRFSS) was performed. Weighted multivariate logistic regression models were used to assess the association of ACEs with FMD and cognitive disability. Mediation effects were used to investigate FMD as mediation between ACEs and cognitive disability in emerging adults. Among the 10,309 respondents, the prevalence of cognitive disability was 15.8%, and 71.6% of them experienced ACEs. We found experienced ACEs, self-reported FMD were significantly associated with 4.05 and 5.61 times increased risk of cognitive disability, respectively. The more types of ACEs respondents experienced, the higher risks of cognitive disability. And mediating effect analysis found FMD mediated the associations between ACEs and cognitive disability. Our study indicated a strong association between ACEs and cognitive disability in emerging adults. Furthermore, FMD plays a mediating role in the associations.
Similar content being viewed by others
Introduction
Cognitive disability, self-reported difficulty with concentration, memory and/or decision making1is the second most common type of disability in the United States2. Cognitive issues are particularly important to diagnose and treat in emerging adults, with a frequency of 24.1%, according to the 2016 Behavioral Risk Factor Surveillance System (BRFSS)3. Emerging adulthood, the period between 18 and 25 years of age4, has been recognized as a separate developmental stage that is increasingly being examined. It is commonly a time of newly acquired independence from caregivers, further education, or entry into the workforce, as well as an investigation of a variety of potential life courses in terms of belief systems, interpersonal connections, and job pathways. They depend on optimum cognitive functioning to properly perform their duties (such as controlling behavior, adjusting to changes, and handling unfamiliar, complicated, and/or less organized surroundings)5. Many factors can influence cognitive disability status, such as biological, psychological, social factors and so forth6. For example, psychological distress can be defined as a kind of multifactorial and unpleasant experience7. It has been suggested that psychological distress was negatively associated with verbal fluency, which refers to the ability to generate correct words according to a specific criterion and reflects cognitive ability8,9. Specifically, a study based on a large sample from the United Kingdom indicated the moderating role of age on the association between psychological distress and verbal fluency, the association was significant in middle-aged people and older adults10. At the social level, neighborhood social cohesion (NSC) was described as the degree of connectedness, trust, and mutual support for inhabitants belong to the same geographic neighborhood or community, the characteristic of the network relationships include social bonds, shared values and the norms11. So NSC was regarded as a positive predictor of cognitive function, then lower NSC may lead to cognitive disability12. In addition, a study revealed that psychological distress could also mediate the association between NSC and cognitive performance13. Given that preventing cognitive disability is critically important for improving overall population health, there must be sufficient knowledge about the factors that may reduce the risk of cognitive disability in emerging adults or provide protection against its emergence.
A variety of circumstances, including adverse childhood experiences (ACEs), such as growing up in a dysfunctional family or experiencing physical, emotional, or sexual abuse as a young child (under the age of 18)14, may have an impact on cognitive disability. Emerging adulthood in particular may be a potent period for ACE effects, and studies indicate that 73% of emerging adults encounter an ACE at least once15. ACEs may influence cognitive disability through multiple pathways including acquired and traumatic brain injuries16and a decrease in plasma neuropeptide-Y(NPY) levels may be one of the biochemical mechanisms of the memory impairment as well17. Previous research, though not focused on emerging adults, highlights the role of ACEs in cognitive disability18. Participants who had endured emotional and physical neglect performed worse on tests of spatial working memory in healthy adults and the latter was linked to weaknesses in pattern recognition memory19. Cumulative effects from multiple risk factors have been shown to be more predictive of compromised early cognitive development among vulnerable adults in U.S than any one risk factor alone18.
Frequent mental distress (FMD) is one of the potentially modifiable factors that is involved in the hypothesized pathways through which ACEs affect cognitive disability in emerging adults. FMD is defined as 14 or more self-reported mentally unhealthy days in the past 30 days, and becomes a particularly consequence of emerging adulthood20. According to the cumulative inequality (CI) theory21,22, early experiences play a significant role in predicting life course health and well-being. Under the guidance of this hypothesis, a lot of studies highlights how adversity in childhood specifically shapes an adult’s mental health23,24. ACEs are complex early stressors that have the potential to interfere with the development of adaptive emotion control mechanisms by altering psychological interpretations and beliefs25,26. Long-term exposure to dangerous, unfavorable environments causes self-denial in children, which raises their chance of developing mental health issues as emerging adults. Additionally, mental wellness is a critical component of healthy development in emerging adulthood and serves to protect against cognitive disability. The theory of Conservation of Resources (COR) postulates that feelings of mental distress can take up and divert significant amounts of cognitive resources, leading to suboptimal cognitive functioning27. Another position refers that FMD commonly causes people to struggle to maintain homeostasis in their bodies, promotes the loss of neuronal structure and function, amplifies pathological damage, then increases the risk of cognitive dysfunction28. As the psychological symptoms increase, the daily cognitive performance was impaired29. For example, seasonal affective disorder (SAD) is a clinical subtype of mood disorder recurring annually, which has a major impact on cognitive function30, then making those who suffer from it more prone than those who are not depressed to experience daily cognitive failures31. In the current research, ACEs may raise a person’s risk of FMD and subsequently have a harmful effect on that person’s cognitive disability during the emerging adult stage. Since FMD is a consequence of early-life exposure, it may operate as a mediating risk factor in the relationships between ACEs and cognitive disability in emerging adults.
To date, there has been a vast literature on the impact of ACEs on both mental health and cognitive problems. Further, there are numerous theories that depict underlying processes regarding mental feelings and cognitive development. However, no study has investigated the potential association between ACEs, FMD and cognitive disability of emerging adulthood. To our knowledge, this study is the first one to comprehensively test the role of FMD as a mediating mechanism through which ACEs may become biologically embedded and increase the risk of cognitive disability in emerging adults. Understanding the relationships between ACEs, cognitive disability and FMD is important for the design of future interventions to reduce ACEs and prevent cognitive disability across emerging adults. Using cross-sectional data from the 2020 and 2021 BRFSS data, we aimed to investigate: (1) the association between self-reported ACEs and cognitive disability; and (2) the mediating effect of FMD between ACEs and cognitive disability.
Methods
Study design and sample selection
The data were obtained from the BRFSS data in 2020 and 2021. BRFSS is a nationally representative, cross-sectional, random-digit-dialed telephone survey collected at the state/territory level on behalf of the Centers for Disease Control and Prevention (CDC)32. The target population of the BRFSS survey is non-institutionalized adults aged 18 years or older. It also assesses health conditions, health behaviors, and behavioral risk factors among adults in the United States annually33. Standardized questionnaires are designed by CDC and state public health departments, including standard core sections, optional modules and state-added questions34. Furthermore, the data collection process of BRFSS was conducted by a computer-assisted telephone interviewing system, so our study was based on the telephonic interview data35. As BRFSS is a publicly available dataset, the data is being updated now. Detailed information about the survey can be found at https://www.cdc.gov/brfss/.
Adverse childhood experiences
Exposed to ACEs were based on the CDC’s uniform questions in ACEs module, and 11 questions were used to evaluate whether a respondent experienced ACEs. According to the questions, 9 types of ACEs were categorized, Household Mental Illness, Household Alcoholism, Household Drug Abuse, Incarceration History in Home, Parental Separation/Divorce, Parental Intimate Partner Violence, Physical Abuse, Emotional Abuse, Sexual Abuse (Table 1). This measurement has shown good reliability and validity across multiple populations, including among those of different races or sexual orientations36,37. In our study, it also indicated good reliability, with a Cronbachs α score of 0.815. To determine the validity of this scale, Spearman correlation coefficient was also calculated, and the results were shown in Table 2.
We encoded all ACEs answers as binary variables based on the contents of the 11 question. The questions reflected the individuals’ ACEs type, and each measure is coded as “yes” if the respondent agrees with the content of the question. If an individual answered “yes” to one or more of the 11 questions, the individual was considered to have experienced ACEs. As for the ACE score (ranged from 0 to 9, higher scores indicating a higher amount of negative experiences), it was calculated based on the cumulative number of ACEs questions to which participants answered that they have experienced. Then it could be categorized as 0, 1, 2, 3, and ≥ 4.
Mental health
For the condition of mental health, respondents were asked to answer a question in Core Section of BRFSS. “Thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Then the respondents who reported no less than 14 days of poor mental health were classified as experienced Frequent Mental Distress (FMD). This reliable definition is a measure of the respondents’ mental health and has been widely used in previous studies38,39.
Cognitive disability
As one of the six disability types, cognitive disability was classified as respondents who reported affirmative responses to the question in Core Section. “Because of a physical, mental or emotional condition, do you having serious difficulty concentrating, remembering, or making decisions?” Although this measure of cognitive disability is limited by its self-reported nature, which has been used in numerous studies and was considered reliable40,41.
Covariates
In our analysis, we included gender (male/female), age (continuous variable), race/ethnicity (non-Hispanic, White; non-Hispanic, Black; Hispanic and Other race), education level (high school or below, more than high school), marital status (married/unmarried couple, divorced/widowed/separated, never married), income (<$15,000, $15,000-$24,999, $25,000-$34,999, $35,000–$49,999 and ≥$50,000), insurance and urban/rural status. These variables were considered as possible confounders with ACEs, mental health and cognitive disability according to previous literature18,34,39,41.
Statistical analysis
In our study, IBM SPSS 24.0 software was used for statistical analysis. All analyses used survey sampling weights that accounted for the sampling strategy used by the BRFSS study. The survey weights were adjusted to reflect the mean population totals during the period for which these data were collected.
For continuous and normally distributed variables, mean values and standard deviations were calculated, then weighted t tests was used to compare for differences among different mental health groups. For categorical variables, counts and percentages were presented and weighted Chi-square tests was performed. P < 0.05 on both sides was considered statistically significant.
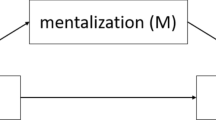
We use standard descriptive statistics to report frequencies for each categorical variable. Then prevalence of ACEs, FMD and cognitive disability were calculated. In addition, logistic regression models were used to evaluate the risk of FMD and cognitive disability with ACEs, ACE score and different types of ACEs, adjusted for covariates and mediation. Logistic regression based on the KHB method proposed by Holm et al42. was used to conduct the mediation analysis, which resulted in the total effect (the effect of treatment variable X on outcome variable Y without mediating variable M) being divided into direct effect (the effect of treatment variable X on outcome variable Y when controlling for mediating variable M) and indirect (mediating) effect (the effect of treatment variable X on outcome variable Y through mediating variable M).
Results
Descriptive analyses and study population
In our present study, 22,194 participants aged 18–25 years that chose the full ACEs module in 2020 and 2021 BRFSS were included. Then we excluded participants with missing values in Cognitive Disability (n = 968), missing values in mental health (n = 325) and missing values or refusals/don’t know/not sure on one or more of the ACEs questions (n = 10,592). Finally, the sample size of 10,309 participants was involved, and the process of sample selection is shown in Fig. 1.
The total sample of the respondents were averaged 21.31 ± 0.08 years old, and nearly all of the covariates were statistically significantly between the respondents with or without cognitive disability, except for race/ethnicity, insurance and urban/rural status (P<0.05). The characteristics of the respondents were summarized in Table 3.
The prevalence of cognitive disability in the overall sample was 15.8%, including 1,567 respondents. As for ACEs, 71.6% of the total respondents experienced at least 1 type of ACEs, especially 25.1% of them experienced no less than 4 types of ACEs. Of those participants classified as cognitive disability, 50.7% also reported having frequent mental distress, compared to 14.2% for those without cognitive disability.
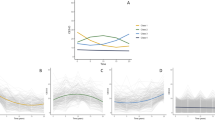
Associations between the ACEs and frequent mental distress
Table 4 shows the associations between ACEs and FMD, we found that ACEs were positively associated with FMD in Model 1, those who experienced ACEs were 3.73 times more likely to have FMD than those who did not. In addition, participants who experienced 2, 3 and ≥ 4 types of ACE were at 3.06, 3.79 and 7.16 times higher risks of reporting FMD compared to those without ACEs, respectively. Each type of ACEs was significantly associated with FMD, and the strongest association with FMD was seen for Household Mental Illness. More specifically, respondents who experienced Household Mental Illness had 4.33 times higher risk of FMD compared to those did not.
However, after controlled for all the covariates in Model 2, ACEs remained positively associated with risks of frequent mental distress, those who experienced ACEs were 3.64 times more likely to FMD than those who did not. And the more types of ACEs respondents experienced, the higher risks of FMD. The associations appeared to follow a dose–response relationship (P for trend < 0.001), especially for those experienced ≥ 4 types of ACEs were 6.62 times the risk of reporting FMD than those did not experienced ACEs. For each type of ACEs, the relationships remained significant after adjusted for covariates, and the strongest association with FMD was seen for Household Mental Illness, too. Those who experienced Household Mental Illness were 3.60 times to report FMD than those who did not.
Associations between ACEs and cognitive disability
Table 5 showed the unadjusted and adjusted associations between ACEs and cognitive disability in models with mediation (Model 1) and without mediation (Model 2). The associations between ACEs and cognitive disability were presented in Model 1, and FMD was added to Model 2. As for the results in Model 1, we found FMD became an important risk factor for cognitive disability in both unadjusted and adjusted models, those who reported FMD were more than five times likely to reporting FMD than those who did not.
In Model 2, we found ACEs were still statistically significantly associated with cognitive disability, those who have experienced ACEs were three times likely to have cognitive disability than those who did not. And we also observed a significant dose-response association between ACE scores and cognitive disability (P for trend < 0.001). Additionally, each type of ACEs was significantly associated with cognitive disability, and the strongest association was found for Emotional Abuse (OR: 3.09, 95CI: 2.46–3.87). However, after adjusted for covariates, all the associations remained statistically significant.
Mediation effects
The results of the mediation analysis are shown in Table 6, and Fig. 2 exhibits the path diagrams for 9 different types of ACEs we retrieved. After adjusting for the confounding factors, the mediation effect of FMD was found in all ACEs types. The total effect, indirect effect of ACEs status on cognitive disability was 1.36 and 0.27, respectively. And FMD was estimated to explain 19.65% of the association between ACEs and cognitive disability. For ACE score, the total effect, indirect effect of ACE score on cognitive disability was 0.47 and 0.11, respectively. So FMD was estimated to explain 22.30% of the association between ACE scores and cognitive disability. Similarly, for each types of ACEs, the effect was considered partial mediation with the mediation proportion varying from 23.72 to 32.98%, while Household Alcoholism had the largest proportion of mediation.
Discussion
Using data from a nationally, representative BRFSS sample, this study promotes our knowledge of the relationships between ACEs and cognitive disability in emerging adults. Our findings confirm the evidence linking ACEs to mental distress and cognitive disability by showing that higher levels of cumulative ACE exposure were linked to increased risk of mental distress and cognitive disability. According to the mediation analysis, FMD plays a mediating role in the associations between ACEs and cognitive disability.
As expected, the cumulative ACE score was associated with cognitive disability in emerging adults, demonstrating that the aggregation of risk factors is linked to impaired cognitive development. This finding is in line with previous research on cognitive disability and cognitive issues18,43. Adversities experienced throughout childhood are significant stressors that contribute to the growth of the stress response and brain function, so the existence of ACEs will significantly impair cognitive function and result in cognitive disability in emerging adults. First of all, because they may constantly feel threatened by their environment, emerging adults who have faced ACEs may have a more active body’s natural stress response. As a result, the normal stress response becomes dysregulated and the allostatic load (i.e., biological adaptive responses that aid in stress recovery) rises over time. Secondly, smaller prefrontal volumes in children have been linked to early life stress, which may hinder their capacity to control their emotions, reflect abstract gain and loss information, then alter stimulus-response linkages44,45. Therefore, in addition to multiple sources of stress, those experienced ACEs may face impairments in a number of socio-emotional and cognitive functions, and they are more prone to experience cognitive handicap as emerging adults. Future study on the relationship between ACEs and cognitive dysfunction can be informed by these findings, and new interventions can be developed to lessen the negative effects of this public health issue.
Numerous studies have investigated the relationship of FMD with ACEs or cognitive disability. According to the Strength Model of Self-Control, the exertion of self-control appears to depend on a limited resource27. Mental distress lowers a person’s cognitive and psychological resources, and it is difficult to make quick, accurate decisions when dealing with external affairs, which ultimately results in cognitive disability. For instance, as a very damaging interpersonal event, childhood maltreatment enhances negative emotion regulation and coping mechanisms including emotional suppression and rumination. Emotional suppression is a cognitively demanding form of self-regulation that may impair incidental recall of information presented during inhibition46, resulting in cognitive disability in emerging adulthood. If pathways can be disrupted through effective treatment of mental distress, the impact of childhood abuse on the development of cognitive disability in emerging adulthood may be reduced.
FMD is also a sign of family dysfunction survivors, because early experiences with parent-child relationships impact mental health and social functioning in many different ways. Early relationship experiences, in accordance with Bowlby (1969/1997), contribute to the development of attachment orientations, which have an impact on how we interpret circumstances, control our emotions, and interact with others. Considering family substance misuse as an example. According to community-based family research47, relatives of drug-dependent people are eight times more likely to develop drug abuse problems than the general population and this high frequency may be inherited. First, brain circuits that have been linked to working memory48,49,50and attentional control51,52,53are major contributors to addiction. Stimulant dependency frequently co-occurs with anxiety and affective disorders and affect-related psychopathologies are also prevalent in families with substance abuse issues54,55. According to the Conservation of Resources (COR) model56,57, people should work to acquire, maintain, and improve their own resources. A person with FMD may lack the necessary psychological resources and find it challenging to interact with their surroundings56,57, which can lead to stress reactions and cognitive disability.
The strengths of this study are as follows. A key strength is the use of a large, nationally representative sample of respondents from the 2020 and 2021 BRFSS39. In addition, we found positive associations between ACEs and cognitive disability, especially for those experienced Emotional Abuse during their childhood. Furthermore, we also observed that the more types of ACEs, the higher the risk of cognitive disability. Also, their associations were also mediated by FMD.
However, our study has a few limitations. First, the BRFSS is a cross-sectional survey, which may impact on causal direction and limit the ability to make any assertions of longitudinal associations58. Second, the information of ACEs, FMD and cognitive disability often relies on memories of past events, which might be subject to recall bias41,59. Third, we lack a determination on the period in which these events actually happened, for example, we couldn’t know at what age respondents experienced ACEs (e.g. separation at age 5 vs. age 17). In addition, the intensity and frequency of such events (e.g. receiving occasionally a slap vs. being regularly slapped and kicked) remained unknown. Fourth, the reliance on self-report information for cognitive disability was used to capture serious difficulty in these basic actions, but it limits the certainty behind the conclusions, and adults with mild or moderate difficulties might not be identified, together with the lack of examples on what people should think of in relation to these serious difficulty18. And it only focus on three domains, including attention, memory and decision-making40. Furthermore, there is no information on possible organic reasons for cognitive difficulties, which might include a wide variety of situations, including substance use, genetic conditions (e.g. Down syndrome), acquired conditions (e.g. head traumas or neurological conditions typical of young age, such as epilepsy or multiple sclerosis). All of this to get to a final statement which suggest caution in the interpretation of results. Last but not least, since perceived cognitive disability and mental illness may have significant overlap, a stronger study would examine objective measures of cognitive disability.
Conclusion
Our study indicated a strong association between ACEs and cognitive disability, the associations appeared to follow a dose–response relationship. Furthermore, FMD plays a mediating role in the associations. The results could provide some support of guide intervention development, including multifaceted approaches to treat FMD. Additionally, other unaccounted factors may be more important than FMD.
Data availability
We have research data to declare. And the data is provided within the supplementary information files.
References
Erickson, W. A guide to disability statistics from the American Community Survey (2008 forward). (2012).
Stevens, A. C. et al. Adults with one or more functional disabilities—United States, 2011–2014. Morbidity Mortal. Wkly. Rep. 65, 1021–1025 (2016).
Okoro, C. A., Courtney-Long, E., Cyrus, A. C., Zhao, G. & Wheaton, A. G. Self-reported short sleep duration among US adults by disability status and functional disability type: results from the 2016 behavioral risk factor Surveillance System. Disabil. Health J. 13, 100887 (2020).
Arnett, J. J. Emerging adulthood: a theory of development from the late teens through the twenties. Am. Psychol. 55, 469 (2000).
Wiebe, D. J. et al. Executive functioning, Daily Self-Regulation, and Diabetes Management while transitioning into emerging Adulthood. Ann. Behav. Med. 57, 676–686. https://doi.org/10.1093/abm/kaad013 (2023).
Landös, A. et al. Childhood socioeconomic circumstances and disability trajectories in older men and women: a European cohort study. Eur. J. Public. Health. 29, 50–58. https://doi.org/10.1093/eurpub/cky166 (2019).
Yu, H. et al. Financial toxicity and psychological distress in adults with cancer: a treatment-based analysis. Asia Pac. J. Oncol. Nurs. 9, 100069. https://doi.org/10.1016/j.apjon.2022.04.008 (2022).
Sharifian, N., Spivey, B. N., Zaheed, A. B. & Zahodne, L. B. Psychological distress links perceived neighborhood characteristics to longitudinal trajectories of cognitive health in older adulthood. Soc. Sci. Med. 258, 113125. https://doi.org/10.1016/j.socscimed.2020.113125 (2020).
Rodríguez-Lorenzana, A. et al. Normative data for test of Verbal Fluency and naming on Ecuadorian Adult Population. Front. Psychol. 11, 830. https://doi.org/10.3389/fpsyg.2020.00830 (2020).
Kang, W. Age moderates the associations between psychological distress and verb Al fluency: N = 33,080. Curr. Psychol. 43, 19639–19642 https://doi.org/10.1007/s12144-024-05785-0
de Vries, S., van Dillen, S. M., Groenewegen, P. P. & Spreeuwenberg, P. Streetscape greenery and health: stress, social cohesion and physical activity as mediators. Soc. Sci. Med. 94, 26–33. https://doi.org/10.1016/j.socscimed.2013.06.030 (2013).
Cagney, K. A. et al. Neighborhood-level cohesion and disorder: measurement and validation in two older adult urban populations. J. Gerontol. B Psychol. Sci. Soc. Sci. 64, 415–424. https://doi.org/10.1093/geronb/gbn041 (2009).
Kang, W. Psychological distress mediates the associations between neighborhood social cohesion (NSC) and cognitive performance in older adults. Curr. Psychol. 43, 7144–7152 https://doi.org/10.1007/s12144-023-04887-5
Felitti, V. J. et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am. J. Prev. Med. 14, 245–258 (1998).
Allem, J. P., Soto, D. W., Baezconde-Garbanati, L. & Unger, J. B. Adverse childhood experiences and substance use among hispanic emerging adults in Southern California. Addict. Behav. 50, 199–204 (2015).
Guinn, A. S., Ports, K. A., Ford, D. C., Breiding, M. & Merrick, M. T. Associations between adverse childhood experiences and acquired brain injury, including traumatic brain injuries, among adults: 2014 BRFSS North Carolina. Inj. Prev. 25, 514–520 (2019).
Bracci-Laudiero, L., Aloe, L., Lundeberg, T., Theodorsson, E. & Stenfors, C. Altered levels of neuropeptides characterize the brain of lupus prone mice. Neurosci. Lett. 275, 57–60 (1999).
Ward, K., Ryan-Ibarra, S., Smith, M. & Sanchez-Vaznaugh, E. V. Adverse childhood experiences and cognitive disability in the 2019 United States behavioral risk factor surveillance system. Prev. Med. Rep. 27, 101826. https://doi.org/10.1016/j.pmedr.2022.101826 (2022).
Majer, M., Nater, U. M., Lin, J. M. S., Capuron, L. & Reeves, W. C. Association of childhood trauma with cognitive function in healthy adults: a pilot study. BMC Neurol. 10, 1–10 (2010).
Arnett, J. J., Žukauskienė, R. & Sugimura, K. The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. Lancet Psychiatry. 1, 569–576 (2014).
Ferraro, K. F., Shippee, T. P. & Schafer, M. H. Cumulative inequality theory for research on aging and the life course. (2009).
Ferraro, K. F. & Shippee, T. P. Aging and cumulative inequality: how does Inequality get under the skin? GERONTOLOGIST. 49, 333–343. https://doi.org/10.1093/geront/gnp034 (2009).
Bracke, P., Delaruelle, K., Dereuddre, R. & Van de Velde, S. Depression in women and men, cumulative disadvantage and gender inequality in 29 European countries. Soc. Sci. Med. 267 https://doi.org/10.1016/j.socscimed.2020.113354 (2020).
Shi, Z. & Wu, C. Early life adversity and health inequality: a dual interaction model. J. Chin. Sociol. 7 https://doi.org/10.1186/s40711-020-00121-y (2020).
Lloyd, A., McKay, R. T. & Furl, N. Individuals with adverse childhood experiences explore less and underweight reward feedback. Proc. Natl. Acad. Sci. U S A. 119 https://doi.org/10.1073/pnas.2109373119 (2022).
Sousa, R., Ribeiro da Silva, D., Petrocchi, N., Gilbert, P. & Rijo, D. At the heart of change: differences in young offenders’ HRV patterns after the delivery of the PSYCHOPATHY.COMP program. Front. Psychiatry. 13, 1032011. https://doi.org/10.3389/fpsyt.2022.1032011 (2022).
Baumeister, R. F., Tice, D. M. & Vohs, K. D. The Strength Model of Self-Regulation: conclusions from the second decade of Willpower Research. Perspect. Psychol. Sci. 13, 141–145. https://doi.org/10.1177/1745691617716946 (2018).
Arnsten, A. F. Stress signalling pathways that impair prefrontal cortex structure and function. Nat. Rev. Neurosci. 10, 410–422. https://doi.org/10.1038/nrn2648 (2009).
Fiorenzato, E., Zabberoni, S., Costa, A. & Cona, G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PloS One. 16, e0246204 (2021).
Shen, J., Kennedy, S. H., Levitan, R. D., Kayumov, L. & Shapiro, C. M. The effects of nefazodone on women with seasonal affective disorder: clinical and polysomnographic analyses. J. Psychiatry Neurosci. 30, 11–16 (2005).
Sullivan, B. & Payne, T. W. Affective disorders and cognitive failures: a comparison of seasonal and nonseasonal depression. Am. J. Psychiatry. 164, 1663–1667 (2007).
Jewett, A., Shults, R. A., Banerjee, T. & Bergen, G. Alcohol-impaired driving among adults - United States, 2012. MMWR Morb Mortal. Wkly. Rep. 64, 814–817. https://doi.org/10.15585/mmwr.mm6430a2 (2015).
Lee, R. D. & Chen, J. Adverse childhood experiences, mental health, and excessive alcohol use: examination of race/ethnicity and sex differences. Child. Abuse Negl. 69, 40–48. https://doi.org/10.1016/j.chiabu.2017.04.004 (2017).
Merrick, M. T., Ford, D. C., Ports, K. A. & Guinn, A. S. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor Surveillance System in 23 States. JAMA Pediatr. 172, 1038–1044. https://doi.org/10.1001/jamapediatrics.2018.2537 (2018).
Gamble, S. et al. Surveillance for certain Health behaviors and conditions among States and selected local areas - behavioral risk factor Surveillance System, United States, 2013 and 2014. MMWR Surveill Summ. 66, 1–144. https://doi.org/10.15585/mmwr.ss6616a1 (2017).
Ford, D. C. et al. Examination of the Factorial structure of adverse childhood experiences and recommendations for three Subscale scores. Psychol. Violence. 4, 432–444. https://doi.org/10.1037/a0037723 (2014).
Dharma, C. et al. Adverse childhood experiences among black sexually minoritized men and black transgender women in Chicago. Int. J. Equity Health. 23, 74. https://doi.org/10.1186/s12939-024-02168-6 (2024).
Slabaugh, S. L. et al. Leveraging Health-Related Quality of Life in Population Health Management: the case for healthy days. Popul. Health Manag. 20, 13–22. https://doi.org/10.1089/pop.2015.0162 (2017).
Grenard, D. L., Valencia, E. J., Brown, J. A., Winer, R. L. & Littman, A. J. Impact of Caregiving during emerging adulthood on frequent Mental Distress, Smoking, and drinking behaviors: United States, 2015–2017. Am. J. Public. Health. 110, 1853–1860. https://doi.org/10.2105/ajph.2020.305894 (2020).
Benn, E. K., Fox, A., Fei, K., Roberts, E. & Boden-Albala, B. Moving towards a more comprehensive investigation of Racial/Ethnic differences in cognitive disability among US adults. J. Immigr. Minor. Health. 17, 1105–1113. https://doi.org/10.1007/s10903-014-0073-0 (2015).
Okoro, C. A., Hollis, N. D., Cyrus, A. C. & Griffin-Blake, S. Prevalence of disabilities and Health Care Access by disability status and type among adults - United States, 2016. MMWR Morb Mortal. Wkly. Rep. 67, 882–887. https://doi.org/10.15585/mmwr.mm6732a3 (2018).
Kohler, U., Karlson, K. B. & Holm, A. Comparing coefficients of nested nonlinear probability models. Stata J. 11, 420–438 (2011).
Oh, D. L. et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 18, 83. https://doi.org/10.1186/s12887-018-1037-7 (2018).
Hanson, J. L. et al. Early stress is associated with alterations in the orbitofrontal cortex: a tensor-based morphometry investigation of brain structure and behavioral risk. J. Neurosci. 30, 7466–7472 (2010).
Hodel, A. S. et al. Duration of early adversity and structural brain development in post-institutionalized adolescents. NeuroImage. 105, 112–119 (2015).
Richards, J. M. & Gross, J. J. Composure at any cost? The cognitive consequences of emotion suppression. Personality Social Psychol. Bull. 25, 1033–1044 (1999).
Merikangas, K. R. et al. Familial transmission of substance use disorders. Arch. Gen. Psychiatry. 55, 973–979 (1998).
Tomasi, D. et al. Widespread disruption in brain activation patterns to a working memory task during cocaine abstinence. Brain Res. 1171, 83–92 (2007).
Fernandez-Serrano, M. J., Pérez-García, M., Schmidt Río-Valle, J. & Verdejo-Garcia, A. Neuropsychological consequences of alcohol and drug abuse on different components of executive functions. J. Psychopharmacol. 24, 1317–1332 (2010).
Ersche, K. D. et al. Peripheral biomarkers of cognitive response to dopamine receptor agonist treatment. Psychopharmacology. 214, 779–789 (2011).
London, E. D. et al. Cerebral metabolic dysfunction and impaired vigilance in recently abstinent methamphetamine abusers. Biol. Psychiatry. 58, 770–778 (2005).
Gooding, D. C., Burroughs, S. & Boutros, N. N. Attentional deficits in cocaine-dependent patients: converging behavioral and electrophysiological evidence. Psychiatry Res. 160, 145–154 (2008).
Ersche, K. D. et al. Abnormal structure of frontostriatal brain systems is associated with aspects of impulsivity and compulsivity in cocaine dependence. Brain Res. 134, 2013–2024 (2011).
Regier, D. A. et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA Pediatr. 264, 2511–2518 (1990).
Merikangas, K. R. et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict. Behav. 23, 893–907 (1998).
Hobfoll, S. E. Conservation of resources: a new attempt at conceptualizing stress. Am. Psychol. 44, 513 (1989).
Lapierre, L. M., Hammer, L. B., Truxillo, D. M. & Murphy, L. A. Family interference with work and workplace cognitive failure: the mitigating role of recovery experiences. J. Vocat. Behav. 81, 227–235 (2012).
Kamen, C. et al. Disparities in Health Risk Behavior and Psychological Distress among Gay Versus Heterosexual Male Cancer survivors. LGBT Health. 1, 86–92. https://doi.org/10.1089/lgbt.2013.0022 (2014).
Kia-Keating, M., Barnett, M. L., Liu, S. R., Sims, G. M. & Ruth, A. B. Trauma‐responsive care in a Pediatric setting: feasibility and acceptability of screening for adverse childhood experiences. Am. J. Community Psychol. 64, 286–297. https://doi.org/10.1002/ajcp.12366 (2019).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors took part in the process of completing the first draft. Y.S. and S.Q. designed, analyzed, and drafted the manuscript. Z.L. designed and drafted the manuscript, too. W.Z. constructed the tables and figures. Y.M. and J.F. reviewed and helped revising the manuscript. S.S. designed and reviewed the manuscript. S.Z., N.L., H.S. and K.T. reviewed the data. X.Z. and Y.Y. supervised and reviewed the manuscript.
Corresponding authors
Ethics declarations
Consent for publication
The corresponding author confirms that the manuscript has been read and approved for submission by all the named authors.
Competing interests
The authors declare no competing interests.
Consent to participate
We confirm the confidentiality of each participant’s answer, and the data will be treated with complete confidentiality, and only for research and statistical purposes only.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, Y., Qu, S., Li, Z. et al. The mediating role of frequent mental distress in the relationship between adverse childhood experiences and cognitive disability in emerging adults. Sci Rep 14, 29717 (2024). https://doi.org/10.1038/s41598-024-79813-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-79813-1