Abstract
Endophthalmitis is a serious infectious eye disease that causes permanent vision loss. This study developed a method for rapid identification and drug resistance analysis of pathogens in vitreous humor. After short-term rapid culture, 30 Staphylococcus aureus isolates were enriched and purified from the vitreous humor using Fc-MBL@Fe3O4, and then identified by MALDI-TOF MS. The bacterial solution was adjusted to 106 CFU/mL and mixed with CAMHB containing cefoxitin (4 µg/mL) at the same volume. After culture, it was enriched by Fc-MBL@Fe3O4 and identified by MALDI-TOF MS. MRSA was judged according to whether the bacteria could successfully be identified. The enrichment efficiency of Fc-MBL@Fe3O4 for S. aureus in CAMHB was 88.1%. The detection rate of S. aureus reached 100% after 8 h of vitreous humor culture. The best test performance was achieved with Fc-MBL@Fe3O4 enrichment after a 3 h incubation. At this time point, 96.7% validity, 100% sensitivity, and 100% specificity were achieved. Thus, the identification and drug resistance analysis of S. aureus (51–110 CFU) in vitreous humor was completed within 11 h. This study provides a new method for rapid clinical diagnosis of endophthalmitis and precise treatment with antibiotics.
Similar content being viewed by others
Introduction
Infectious endophthalmitis refers to an intraocular infection caused by pathogens (e.g., bacteria or fungi) in the vitreous and aqueous humor1,2. It is one of the most devastating eye infections and can lead to irreversible blindness in the infected eye within hours or days of symptom onset3. Most infectious endophthalmitis is exogenous and occurs during cataract surgery, intravitreal injection, vitrectomy, and complications of eye trauma. It may also be endogenous, caused by hematogenous dissemination of pathogens during bacteremia or fungemia2. Staphylococcus aureus is a common cause of infectious endophthalmitis and can be found in traumatic infections and endocarditis-related endogenous infections1. As the global population ages, cataract surgery is increasing dramatically. At the same time, the demand for intraocular injection is also increasing with the emergence of new intravitreal drugs for the treatment of various retinal diseases4,5,6. The identification of pathogenic bacteria and drug resistance in infectious endophthalmitis are key to timely and effective clinical treatment.
Microbial culture is the gold standard for diagnosing infectious endophthalmitis. Positive culture results are observed in approximately 90% of vitrectomy specimens, 50 to 70% of vitreous aspirates, and 40% of aqueous aspirates7,8,9. In addition to the low detection rate of traditional culture methods, the time required for bacterial identification and drug sensitivity tests is relatively long, usually 3–5 days, which will delay patient treatment. Molecular diagnostic technology can quickly identify pathogens and detect drug resistance in intraocular fluid. It is still effective in culture-negative samples, and 20–30% of culture-negative intraocular fluid specimens can be detected by molecular diagnostic techniques10. Although molecular diagnostic techniques have reduced detection times, the method is demanding for laboratories and personnel, and the instruments are expensive. To meet the practical needs of clinical practice, it is necessary to develop simpler and more economical detection methods11.
In recent years, the emergence and development of matter-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) has provided a simple, rapid, and low-cost method for accurately identifying pathogenic bacteria in clinical specimens12,13. In addition to pathogen identification, MALDI-TOF MS had also been used to detect drug resistance in bacteria. Some studies have shown that MRSA and MSSA can be distinguished directly by the characteristic mass spectrometry peaks14. Idelevich et al. recently developed a MALDI-TOF MS-based direct targeted microdrop growth assay (DOT-MGA) that enables universal fast antimicrobial susceptibility testing(AST) in 4–5 h. DOT-MGA can be used to analyze drug-resistant bacteria in blood culture bottles and solid media15,16,17. Zhen Liu et al. used DOT-MGA to analyze the drug resistance of Enterobacteriaceae bacteria in urinary tract infections within 4 h18. DOT-MGA uses tissue to remove the iquid medium to purify the bacteria. If the purification steps can be further optimized, the detection time may be reduced.
Immunomagnetic separation (IMS) has become an alternative method for obtaining target microorganisms. Covalently linking mannose-binding lectin (MBL) to the Fc portion of IgG1 in a genetically engineered form (FC-MBL) allows extensive removal of unknown pathogens and endotoxins from the blood19. A novel functionalized magnetic nanoparticle (Fc-MBL@Fe3O4) has been developed to directly enrich bacteria in blood culture bottles, cerebrospinal fluid, bone trauma wounds, urine, and aqueous humor20,21,22,23,24. These studies have shown that Fc-MBL@Fe3O4 can effectively enrich bacteria in clinical samples, providing a new scheme for the pre-treatment of clinical samples.
Based on Fc-MBL@Fe3O4 enrichment combined with MALDI-TOF MS identification, the present study intends to establish a complete MRSA identification and drug resistance rapid detection scheme for trace amounts in vitreous fluid samples.
Results
Specificity of magnetic beads
Our previous study introduced the synthetic process for Fc-MBL@Fe3O4 and its characterization24. We investigated the efficiency of magnetic beads to enrich bacteria in CAMHB and sterile water. As shown in Fig. 1A-B, the enrichment efficiency of magnetic beads was 98.1% in sterile water and 88.1% in CAMHB. Thus, the magnetic beads have high enrichment efficiency in both sterile water and CAMHB. Transmission electron microscopy was performed to image the binding of Fc-MBL@Fe3O4 to S. aureus (Fig. 1C).
Rapid identification of pathogens in vitreous humor by microbroth culture
The workflow of the proposed method is illustrated in Fig. 2. The initial number of bacteria in vitreous humor fluids was 79.8 CFU on average (range, 51 CFU to 110 CFU) through plate colony counting. During the short-term culture of vitreous samples, the LB broth volume influenced the change in the OD600 (Table S1). When the vitreous samples were cultured for 8 h without adding LB broth, the OD600 value did not change significantly. When the vitreous humor samples were cultured for 7 h with 60 µL LB broth, the OD600 was 1.39 ± 0.31. When the vitreous samples were cultured for 7 h with 120 µL LB broth, the OD600 was 0.87 ± 0.40. The change trend of OD value of 30 strains of S. aureus during culture is shown in Fig. S1. For 30 strains of S. aureus, 53.3% cultured to 7 h could be used for MALDI-TOF MS identification, and 100% cultured to 8 h could be used for MALDI-TOF MS identification. The OD600 values are provided in Table S2.
Characterization of bacterial isolates by standard methods
The MIC50, MIC90, and MIC range of cefoxitin for MRSA isolates were 32, > 256, and 8 to > 256 mg/mL, respectively. For MSSA isolates, the MIC50, MIC90, and MIC range of cefoxitin were 2, 4, and 2 to 4 µg/mL. Detailed results are provided in Table S3. The MIC of the S. aureus QC strain (ATCC 25923) was within the recommended range throughout the study. Phenotypic susceptibility results were confirmed by genotypic characterization. The mecA gene was detected in all clinical MRSA isolates.
Bacterial resistance analysis of vitreous humor by Fc-MBL@Fe3O4-binding MALDI-TOF MS.
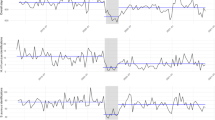
Trace amounts of CAMHB can effectively expand bacteria in a short time. As shown in Fig. 3A, MSSA cannot grow in CAMHB containing cefoxitin (4 µg/mL). There was a significant difference (P < 0.009) in the OD600 between the growth control group and the drug group before incubation to 2 h. MRSA can proliferate in CAMHB with or without cefoxitin (4 µg/mL) but grows slowly in broths containing antibiotics (Fig. 3B). There was no significant difference (P > 0.065) in the OD600 between the growth control group and the drug group before incubation to 7 h. The OD600 values are given in Table S4. Based on the pre-experiment and reported DOT-MGA results15,16,17, 2 h, 3 h, and 4 h were selected as the detection times (Fig. 3C-D). As shown in Table S5, the OD600 of MRSA cultured in CAMHB for 2 h, 3 h, and 4 h was 0.08 ± 0.03, 0.33 ± 0.1, and 0.72 ± 0.11, respectively; the OD600 of MRSA cultured in CAMHB (4 µg/mL cefoxitin) for 2 h, 3 h, and 4 h was 0.07 ± 0.03, 0.26 ± 0.1, and 0.58 ± 0.15, respectively. As shown in Table S6, the OD600 of MSSA cultured in CAMHB for 2 h, 3 h, and 4 h was 0.08 ± 0.03, 0.32 ± 0.07, and 0.72 ± 0.12, respectively; the OD600 of MSSA cultured in CAMHB (4 µg/mL cefoxitin) for 2 h, 3 h, and 4 h was 0.02 ± 0.01, 0.02 ± 0.02, and 0.02 ± 0.01, respectively.
The mass spectra of MRSA and MSSA were shown in Fig. 4A-D. The identification scores for the 30 strains of S. aureus are provided in Table S7 and S8. When S. aureus was incubated for 3 h, the validity of identification of MRSA by Fc-MBL@Fe3O4 enrichment combined with mass spectrometry was 96.7%, and the sensitivity, specificity, positive predictive value, and negative predictive value were all 100%. The validity also reached 100% after incubation for 4 h. The results are provided in Table 1. As no significant difference (P = 1) was found between the effective rates of 3 h and 4 h, 3 h was judged to be the best incubation time for identification of MRSA by Fc-MBL@Fe3O4 enrichment combined with mass spectrometry. When S. aureus was incubated for 3 h, the effective rate of identification of MRSA by centrifuge enrichment combined with mass spectrometry was only 40%.
OD600 values for MSSA and MRSA with culture time. (A)1 strain of MSSA was cultured in CAMHB with or without cefoxitin (4 µg/mL) for 8 h. The experiment was repeated three times. (B) 1 strain of MRSA was cultured in CAMHB with or without cefoxitin (4 µg/mL) for 8 h. The experiment was repeated three times. (C) 15 MSSA strains were cultured (2 h, 3 h, and 4 h) in CAMHB with or without cefoxitin (4 µg/mL). (D) 15 MRSA strains were cultured (2 h, 3 h, and 4 h) in CAMHB with or without cefoxitin (4 µg/mL). *P < 0.05 between the growth control group and drug group.
Coherence analysis
The results of Fc-MBL@Fe3O4 enrichment combined with mass spectrometry and microbroth dilution of 30 strains of S. aureus at the optimal incubation time were analyzed by the kappa test (Table S9). The results of both methods were identical (kappa = 1).
Discussion
Endophthalmitis is a serious eye infection that can lead to irreversible blindness in the infected eye within hours or days of symptom onset, requiring rapid diagnosis and treatment to save the patient’s vision. Staphylococcus, including coagulase-negative staphylococcus and S. aureus, are common causes of bacterial endophthalmitis26. Perioperative prophylaxis with topical antibiotics can effectively reduce the risk of progression to endophthalmitis. However, the effectiveness of this preventive measure may be limited by an increase in bacterial resistance, particularly MRSA27,28. Staphylococcus isolates have high levels of in vitro resistance, up to 46%, to commonly used ophthalmic antibiotics, particularly methicillin29. In patients diagnosed with endophthalmitis, the recommended empirical treatment consists of a combination of Vancomycin and either Ceftazidime or Amikacin. Even if MRSA is detected, vancomycin can still be used to treat endophthalmitis. However, the overuse of vancomycin can result in the emergence of antibiotic-resistant bacteria. A recent 10-year study conducted in India on various types of endophthalmitis reported that Gram-positive bacteria exhibited resistance to vancomycin, with rates ranging from 0–20%30. Rapid identification of MRSA is conducive to the correct selection of antibiotics in the early clinical stages and reduction of the patient blindness rate.
Traditional drug susceptibility tests take a long time and currently require at least 1 day to report results. PCR can quickly detect MRSA, but this method has its own shortcomings14,31. Many studies have shown that MALDI-TOF MS has good application prospects in microbial resistance detection32,33,34. Three methods have been developed for rapid identification of drug-resistant bacteria using MALDI-TOF MS, which detects the hydrolytic products after a period of antibiotic action. The characteristic peak of the strain is detected on the mass spectrum, but this can only determine whether it is drug-resistant bacteria, not the strength of the drug resistance. The MIC values of strains are evaluated by DOT-MGA, a method proposed by Idelevich that can be used to rapidly detect the antibiotic resistance of a variety of bacteria. This method has the advantages of low cost, fast speed, and high throughput15,16,17. There are still two problems with the method of using tissue to remove liquid medium from the process of bacteria purification by DOT-MGA, which are broth remaining on the target plate and contamination of adjacent targets, both of which will affect the identification of bacteria.
Fc-MBL@Fe3O4 has a good enrichment effect on bacteria in complex environments. Therefore, a rapid pathogen identification and antimicrobial susceptibility assay with Fc-MBL@Fe3O4 enrichment combined with MALDI-TOF MS analysis was evaluated in this study. In order to make comparisons with the traditional microbroth dilution method, the selected bacterial concentration was 5 × 105 CFU/mL. As no special material is used in the literature, we selected the traditional enrichment by centrifugation method as the pre-treatment control group. In this study, the enrichment efficiency of Fc-MBL@Fe3O4 in CAMHB was 88.1% by the plate colony count method. When enrichment by Fc-MBL@Fe3O4 was used as pre-treatment, the validity of S. aureus identification reached 96.7% after 3 h of culture. When enrichment by centrifugation was used as pre-treatment, the validity of S. aureus culture after 3 h was only 40%. Thus, enrichment by Fc-MBL@Fe3O4 is superior to conventional centrifugal enrichment.
In this study, we evaluated the validity of Fc-MBL@Fe3O4 enrichment combined with MALDI-TOF MS analysis in distinguishing MRSA and MSSA at three culture times (2 h, 3 h, 4 h). The validity of S. aureus after 2 h of culture was 36.7%, and the sensitivity and negative predictive value were poor, so it is not recommended as the optimum incubation time. The validity of S. aureus after 3 h of culture was 96.7%, and the sensitivity, specificity, positive predictive value, and negative predictive value were all 100%. As the difference in validity between 3 h and 4 h was not significant, 3 h could be used as the best incubation time to identify MRSA. The identification results for MRSA and MSSA in this study were completely consistent with those using the microbroth dilution method, indicating that Fc-MBL@Fe3O4 enrichment combined with MALDI-TOF MS has high accuracy in the identification of MRSA and MSSA. Some studies have used the DOT-MGA method to identify MRSA, and the validity of S. aureus culture for 3 h was 28.6%. The validity of 4 h was 85.7%. The validity of 5 h was 100%17. Compared with the DOT-MGA method, Fc-MBL@Fe3O4 enrichment can shorten the culture time from 5 h to 3 h. The OD600 of the liquid medium was detected by UV–vis absorption spectroscopy. In this study, the OD600 value for “MRSA + CAMHB (4 µg/mL cefoxitin)” began to change at 2 h and significantly changed at 3 h. The OD600 value for “MSSA + CAMHB (4 µg/mL cefoxitin)” did not change significantly after 8 h of culture. As the time for significant changes in the OD600 of the culture medium is consistent with the optimal incubation time for the identification of MRSA and MSSA, monitoring the OD600 of the culture medium is recommended as an auxiliary method to determine whether enrichment of the culture medium and mass spectrometry is necessary.
The combination of Fc-MBL@Fe3O4 enrichment with MALDI-TOF MS analysis has been widely used for rapid identification of pathogenic bacteria. For the first time, we used Fc-MBL@Fe3O4 enrichment combined with MALDI-TOF MS analysis to rapidly identify bacterial drug resistance, which could not only identify resistant and sensitive bacteria, but also detect the accurate MIC values of bacteria against antibiotics. In this study, the identification and drug resistance analysis of S. aureus in vitreous humor was completed within 11 h. This method is expected to guide clinicians in the correct use of antibiotics in time after the subsequent verification of multiple drug-resistant bacteria. This study has certain limitations. Firstly, it only included S. aureus. In the future, we intend to conduct rapid drug sensitivity testing for Pseudomonas aeruginosa, Klebsiella pneumoniae, and Streptococcus. Secondly, we added bacteria to vitreous humor to simulate the context. Our goal is to apply this method to clinical vitreous humor identification. Our results should be validated with larger samples from endophthalmitis patients. Finally, Fc-MBL@Fe3O4 we utilized were non-specific for bacterial enrichment. Subsequently, there is a need to develop targeted magnetic beads for the enrichment of common pathogens associated with endophthalmitis.
Methods
Bacterial strains
Thirty non-duplicate S. aureus isolates were provided by Eye & ENT Hospital of Fudan University. This cohort consisted of 15 MRSA strains and 15 MSSA strains. The presence of the mecA gene, which is specific for MRSA, was analyzed by PCR, and the results were consistent with routine susceptibility testing.
Vitreous humor preparation
Fresh porcine eyeballs were obtained from the butcher. The porcine eyeballs were submerged in a 5% povidone-iodine solution for disinfection and subsequently rinsed with sterile water after 10 s. A puncture was made in the posterior chamber with 1 mL syringe and vitreous humor withdrawn. Usually, 1 mL of vitreous humor was obtained per eyeball. The vitreous humor was filtered through a 0.22 mm filter membrane and transferred to a 1.5 mL centrifuge tube. The vitreous humor was subjected to UV irradiation for a duration of 30 min and subsequently stored at -80 °C in a refrigerator until further use.
Determination of MIC
The MIC for S. aureus was determined by the microbroth dilution reference method according to the CLSI and ISO guidelines25. Bacterial colonies from the TSA plate were carefully selected using a sterile inoculation loop and transferred into a centrifuge tube containing sterile water. Following thorough grinding and mixing, the optical density at 600 nm (OD600) of the bacterial suspension was measured using UV-visible absorption spectrometry. The instrument was zeroed with sterile water, and the OD600 value of the bacterial suspension was adjusted to 0.7 to 0.8, at which point the bacterial concentration was approximately 108 CFU/mL, and the bacterial concentration was diluted 1:100 with CAMHB to achieve a final concentration of 106 CFU/mL. The concentration of bacteria was determined by triplicate plate colony counting. The diluted bacterial suspension (100 µL) was added to a 96-well plate containing cefoxitin. The volume of the solution in the final 96-well plate was 200 µL, and the final concentration of bacteria was approximately 5 × 105 CFU/mL. The final concentration of cefoxitin was 256 µg/mL, 128 µg/mL, 64 µg/mL, 32 µg/mL, 16 µg/mL, 8 µg/mL, 4 µg/mL, 2 µg/mL, 1 µg/mL, or 0.5 µg/mL. The MIC results were interpreted according to the CLSI breakpoint. The MIC50, MIC90, and MIC range of the experimental strains were calculated for analysis.
Enrichment efficiency of Fc-MBL@Fe3O4 in CAMHB
The bacterial suspension was diluted to a concentration of 103 CFU/mL using sterile water, and 10 µL of this suspension was subsequently added to 90 µL of CAMHB with thorough mixing. Fc-MBL@Fe3O4 solution (5 µL, 10 mg/mL) and Tris-HCl solution (100 µL, 0.1 mM, pH 7.4) were added to 100 µL of the CAMHB mixture (100 CFU) and incubated at 37℃ for 20 min with consistent shaking at 1200 rpm. After magnetic separation, the supernatant was removed, and the magnetic beads washed three times with 30 µL of sterile water. The supernatant and washing solution were mixed and inoculated on TSA plates. The above steps were replicated using sterile water in place of CAMHB to evaluate the enrichment efficiency of S. aureus by Fc-MBL@Fe3O4 in sterile water.
Rapid identification of pathogens in the vitreous humor
After bacterial suspension was diluted 105 times with sterile water, 10 µL of the bacterial suspension and 50 µL of vitreous humor were added to different volumes (0 µL, 60 µL, and 120 µL) of LB medium. The mixture was incubated at 37 °C with shaking at 850 rpm, and the OD600 was measured every hour (1 to 8 h). When the OD600 exceeded 0.8, the culture medium was diluted to an OD600 of 0.7–0.8 using sterile water. Once the OD600 reached this range, a volume of 50 µL from the mixture was centrifuged at 8000 rpm for 10 min at room temperature to collect the bacterial cells. The supernatant was carefully discarded without disturbing the pellets. The pellet was washed three times with 100 µL of sterile distilled water, resuspended in 5 µL of 70% formic acid and 5 µL of ACN (vortexed thoroughly), and analyzed by MALDI-TOF MS. The above steps were repeated three times. The optimal volume of LB broth was established by comparing the OD600 readings across three groups with varying volumes. Thirty strains of S. aureus were rapidly identified by the above method.
MALDI-TOF MS-based rapid antimicrobial susceptibility testing directly from vitreous humor
Upon completion of the short-term culture of LB broth in vitreous humor, 50 µL of the culture solution was extracted for rapid bacterial identification, followed by the collection of 10 µL for assessing bacterial resistance. A 10 µL aliquot of the bacterial suspension was diluted 100 times with sterile water and mixed thoroughly. Referring to the previous research results for short-term culture of pathogenic bacteria in aqueous humor, we selected 20 µL of diluted bacterial suspension in CAMHB as the optimal culture volume24. Cefoxitin solution was prepared with CAMHB as the solvent. After adding 20 µL of cefoxitin solution to 20 µL of diluted bacterial suspension in CAMHB, the final inoculum size was expected to be approximately 5 × 105 CFU/mL, as recommended by the CLSI. The final concentration of cefoxitin was 4 µg/mL. A single strain of MRSA and a single strain of MSSA were randomly selected for the preparation of the bacterial suspension. CAMHB serves as a blank control. CAMHB containing cefoxitin was added to the bacterial suspension as the experimental group, and CAMHB was added to the bacterial suspension as a growth control group. Both groups were separately incubated at 37 °C with shaking at 850 rpm, and the OD600 was measured every hour (1 to 8 h). By plotting the bacterial culture time on the x-axis and OD600 on the y-axis, a standard curve was established to illustrate the linear relationship between bacterial culture duration and OD600. For bacterial identification, the culture was terminated when the OD600 value of the mixture changed. At the end of the culture, 100 µL Tris-HCL solution and 5 µL Fc-MBL@Fe3O4 were added to the sample and incubated at 37 °C for 20 min with consistent shaking at 1200 rpm. The supernatant was discarded, and the Fc-MBL@Fe3O4 enrichment was resuspended in 5 µL of 70% formic acid and 5 µL ACN. The bacterial protein solution obtained through extraction was analyzed using MALDI-TOF mass spectrometry. The aforementioned procedures were subsequently repeated for the remaining MRSA and MSSA strains.
MALDI-TOF MS identification
A 1.5 µL aliquot of the bacterial protein solution derived from Fc-MBL@Fe3O4 was deposited onto the MALDI-TOF MS target. MALDI-TOF mass spectrometry was performed in linear positive mode, and the target plates were subjected to mass spectrometry on an M-Discover 100 Excellence mass spectrometer. The mass range of the M-Discover 100 Excellence mass spectrometer is 2,000 to 20,000 Da. The raw mass spectra were processed using MicroCtrl version 1.0 software. The data processing parameters included spectral smoothing, baseline correction, and automatic peak finding. In the absence of cefoxitin, a growth control score of ≥ 1.7 for species identification was deemed valid, while a score < 1.7 indicated an invalid test result. For samples containing cefoxitin, successful species identification (score ≥ 1.7) suggested that the isolate was not susceptible, whereas failed species identification (score < 1.7) was interpreted as indicative of susceptibility. A median result for three spots was calculated and used for analysis. The scoring method of the MicroDiscovery software we used is the same as that used in the Bruker Biotyper software.
Statistical analysis
Statistical analyses were conducted using SPSS version 26.0. Depending on the nature of the data, results are presented as mean ± standard deviation (SD) or percentages. The continuous correction χ² test was employed to assess validity comparisons, while the kappa statistic was utilized to evaluate the agreement between the DOT-MGA and microbroth dilution methods.
Data availability
Data is provided within the manuscript or supplementary information files. The MALDI-TOF MS datasets for the current study are available from the corresponding author on reasonable request.
References
Durand, M. L. Bacterial and fungal endophthalmitis. Clin. Microbiol. Rev. 30 (3), 597–613 (2017).
Monteiro, J. P. et al. Vitreous humor in the pathologic scope: insights from proteomic approaches. Proteom. Clin. Appl. 9 (1–2), 187–202 (2015).
Borroni, D. et al. Shotgun metagenomic sequencing in culture negative microbial keratitis. Eur. J. Ophthalmol. Jul. 33 (4), 1589–1595 (2023).
Gower, E. W. et al. Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst. Rev. 2 (2), CD006364 (2017).
Biswas, S. & Rolain, J. M. Use of MALDI-TOF mass spectrometry for identification of bacteria that are difficult to culture. J. Microbiol. Methods. 92 (1), 14–24 (2013).
Mailhac, A. et al. MALDI-TOF mass spectrometry for rapid diagnosis of postoperative endophthalmitis. J. Proteom. 152, 150–152 (2017).
Das, T. Endophthalmitis management: Stain-Culture, empirical treatment, and Beyond. Asia Pac. J. Ophthalmol. (Phila). 9 (1), 1–3 (2020).
Mishra, D., Satpathy, G., Chawla, R., Paliwal, D. & Panda, S. K. Targeted metagenomics using next generation sequencing in laboratory diagnosis of culture negative endophthalmitis. Heliyon 7 (4), e06780 (2021).
Lee, C. S. et al. Endophthalmitis study group. prognostic utility of whole-genome sequencing and polymerase chain reaction tests of ocular fluids in Postprocedural Endophthalmitis. Am. J. Ophthalmol. 217, 325–334 (2020).
Chiquet, C. et al. French institutional endophthalmitis study group. Eubacterial PCR for bacterial detection and identification in 100 acute postcataract surgery endophthalmitis. Invest. Ophthalmol. Vis. Sci. 49 (5), 1971–1978 (2008).
Borroni, D. et al. Metagenomics in ophthalmology: current findings and future prospectives. BMJ Open. Ophthalmol. Jun. 4 (1), e000248 (2019).
Oros, D. et al. Identification of pathogens from native urine samples by MALDI-TOF/TOF tandem mass spectrometry. Clin. Proteom. 17, 25 (2020).
Croxatto, A., Prod’hom, G. & Greub, G. Applications of MALDI-TOF mass spectrometry in clinical diagnostic microbiology. FEMS Microbiol. Rev. 36 (2), 380–407 (2012).
Gao, W., Li, B., Ling, L., Zhang, L. & Yu, S. MALDI-TOF MS method for differentiation of methicillin-sensitive and methicillin-resistant Staphylococcus aureus using (E)-Propyl α-cyano-4-Hydroxyl cinnamylate. Talanta 244, 123405 (2020).
Idelevich, E. A., Sparbier, K., Kostrzewa, M. & Becker, K. Rapid detection of antibiotic resistance by MALDI-TOF mass spectrometry using a novel direct-on-target microdroplet growth assay. Clin. Microbiol. Infect. 24 (7), 738–743 (2018).
Idelevich, E. A. et al. Rapid direct susceptibility testing from positive blood cultures by the Matrix-assisted laser desorption ionization-time of Flight Mass Spectrometry-based direct-on-target Microdroplet Growth Assay. J. Clin. Microbiol. 56 (10), e00913–e00918 (2018).
Nix, I. D. et al. Detection of methicillin resistance in staphylococcus aureus from agar cultures and directly from positive blood cultures using MALDI-TOF Mass Spectrometry-based direct-on-target Microdroplet Growth Assay. Front. Microbiol. 11, 232 (2020).
Liu, Z. et al. Rapid Identification and Drug Sensitivity Test to urinary tract infection pathogens by DOT-MGA. Infect. Drug Resist. 15, 1391–1397 (2022).
Didar, T. F. et al. Improved treatment of systemic blood infections using antibiotics with extracorporeal opsonin hemoadsorption. Biomaterials 67, 382–392 (2015).
Xue, Y. et al. Rapid identification of bacteria directly from blood cultures by co-magnetic bead enrichment and MALDI-TOF MS profiling. Talanta 233, 122472 (2021).
Yu, M., Zhang, L., Qian, G., Shi, H. & Yu, S. Fc-MBL-modified Fe3O4 magnetic bead enrichment and fixation in Gram stain for rapid detection of low-concentration bacteria. Mikrochim Acta. 189 (4), 169 (2022).
Ying, J. et al. Application of MALDI-TOF MS profiling coupled with functionalized magnetic enrichment for rapid identification of pathogens in a patient with open fracture. Front. Chem. 9, 672744 (2021).
Cheng, W. et al. Rapid identification of bacterial mixtures in urine using MALDI-TOF MS-based algorithm profiling coupled with magnetic enrichment. Analyst 147 (3), 443–449 (2022).
Ren, J. et al. Rapid Pathogen Identification in aqueous humor samples by combining Fc-MBL@Fe3O4 Enrichment and Matrix-assisted laser desorption ionization-time of Flight Mass Spectrometry Profiling. Microbiol. Spectr. 10 (6), e0176722 (2022).
CLSI. Performance standard for antimicrobial susceptibility testing. 30th ed. CLSI Supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; (2020).
Patel, S. N., Gangaputra, S., Sternberg, P. Jr & Kim, S. J. Prophylaxis measures for postinjection endophthalmitis. Surv. Ophthalmol. 65 (4), 408–420 (2020).
Schimel, A. M., Miller, D. & Flynn, H. W. Jr Endophthalmitis isolates and antibiotic susceptibilities: a 10-year review of culture-proven cases. Am. J. Ophthalmol. 156 (1), 50–52 (2013). e1.
Olson, R. J. et al. Cataract in the adult eye preferred practice pattern®. Ophthalmology124 (2), P1–P119 (2017).
Asbell, P. A., Mah, F. S., Sanfilippo, C. M. & DeCory, H. H. Antibiotic susceptibility of bacterial pathogens isolated from the aqueous and vitreous humor in the antibiotic resistance monitoring in Ocular microorganisms (ARMOR) surveillance study. J. Cataract Refract. Surg. 42 (12), 1841–1843 (2016).
Satpathy, G. et al. Clinicomicrobiological profile of endophthalmitis: a 10-year experience in a tertiary care center in North India. Indian J. Pathol. Microbiol. Apr-Jun. 60 (2), 214–220 (2017).
Chun, L. Y. et al. Rapid pathogen identification and antimicrobial susceptibility testing in in vitro endophthalmitis with matrix assisted laser desorption-ionization time-of-flight Mass Spectrometry and VITEK 2 without prior culture. PLoS One. 14 (12), e0227071 (2019).
Wu, X. et al. Prediction of Mycobacterium tuberculosis drug resistance by nucleotide MALDI-TOF-MS. Int. J. Infect. Dis. 121, 47–54 (2022).
Zvezdanova, M. E. et al. Detection of azole resistance in aspergillus fumigatus complex isolates using MALDI-TOF mass spectrometry. Clin. Microbiol. Infect. 28 (2), 260–266 (2022).
Tang, H. et al. Direct-on-target Microdroplet Growth Assay for detection of bacterial resistance in positive blood cultures. Infect. Drug Resist. 14, 4611–4617 (2021).
Author information
Authors and Affiliations
Contributions
Jun Ren performed the experiments and data analysis and wrote the original draft. Wenjing Gao performed the experiments. Menghuan Yu and Chungong Liu helped with the data processing. Shengjie Li revised the original draft of the manuscript. Chuanfan Ding modified the manuscript. Shaoning Yu and Wenjun Cao supervised all aspects of the work. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ren, J., Gao, W., Yu, M. et al. Detection of methicillin resistance of Staphylococcus aureus in vitreous humor using MALDI-TOF MS and Fc-MBL@Fe3O4 enrichment. Sci Rep 14, 30757 (2024). https://doi.org/10.1038/s41598-024-80715-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-80715-5