Abstract
We evaluated the impact of adenomyosis and ovarian endometriosis on ovarian reserve function through transvaginal three-dimensional ultrasound and anti-mullerian hormone testing. A total of 150 female patients who were admitted to our hospital from January 2023 to May 2024 were selected; 58 cases had adenomyosis (adenomyosis group), 36 had ovarian endometriosis (ovarian endometriosis group), and 56 were healthy (healthy group). There were no statistically significant differences in clinical baseline data among the three groups (all P > 0.05). However, significant overall differences were found in anti-Mullerian hormone levels, antral follicle count, ovarian volume, vascularization index, flow index, and vascularization flow index among the three groups (F values were 90.34, 146.50, 92.61, 63.87, 59.50, 49.36 respectively; all P < 0.001); compared to the healthy group, these indicators were all decreased in the adenomyosis group and ovarian endometriosis group (all P < 0.05). Pearson correlation analysis revealed that serum anti-mullerian hormone levels were positively correlated with antral follicle count, ovarian volume, vascularization index, flow index, and vascularization flow index (r = 0.80, 0.73, 0.50, 0.48, 0.45, respectively; all P < 0.01). These data suggest that adenomyosis and ovarian endometriosis can lead to a decline in ovarian reserve function in women of reproductive age compared to their peers. Also, antral follicle count and ovarian volume are the optimal indicators for evaluating ovarian reserve function in these patients.
Similar content being viewed by others
Introduction
Adenomyosis (AM) is a form of intrinsic endometriosis characterized by the presence of ectopic endometrial epithelial cells and stromal fibroblasts within the myometrium, which leads to hyperplasia and hypertrophy of the surrounding smooth muscle cells1. Common symptoms of AM include chronic pelvic pain, dysmenorrhea, menorrhagia, and infertility2. AM may also be associated with other complications, such as leiomyomas and extrinsic endometriosis. Additionally, there has been growing evidence linking AM to infertility and reproductive failure3. A recent cross-sectional study suggested a prevalence of AM of approximately 24.4% in infertile women aged ≥40 and a prevalence of 7.5–22% in infertile women aged < 404.
Anti-Müllerian Hormone (AMH), a glycoprotein hormone that negatively regulates folliculogenesis in females, is one of the most studied parameters of fertility. Studies using AMH have found that alterations in this regulatory mechanism can lead to primary ovarian insufficiency and polycystic ovary syndrome5. In addition, existing research suggested that women with AM might have lower levels of AMH6.
The pathological processes involved in AM and ovarian endometriosis (OEM), including inflammation, immune regulation, oxidative stress, extracellular matrix remodeling, abnormal angiogenesis, as well as genetic and epigenetic changes, are associated with alterations in oocyte development, endometrial receptivity, implantation, successful maintenance of pregnancy, and delivery7. Studies have also suggested that altered immunological responses and inflammatory cascades in patients with AM combined with OEM could lead to follicular damage within the ovaries and diminished ovarian reserve (DOR); this was not observed in healthy women8. Therefore, it is speculated that the ovarian reserve function in patients with AM and OEM might be lower than in healthy women.
The assessment of ovarian reserve function primarily relies on basic endocrine hormone measurements and ultrasonography. AMH is considered the gold standard for evaluating ovarian reserve function. However, although AMH can qualitatively assess ovarian function, it cannot provide a comprehensive dynamic evaluation of ovarian function, nor can it determine the total number of antral follicles count(AFC).
Ultrasonography is a widely recognized tool whose major advantages are non-invasiveness, simplicity of operation, and dynamic imaging capabilities9. Studies have suggested that three-dimensional transvaginal ultrasound (3D-TVS), with the help of SonoAVC software, can asses AFC (number, size, and volume of AFC) with good resolution and accuracy; the software automatically shows each follicle in a different color and calculates the three diameters and volume. Compared to two-dimensional ultrasound, 3D-TVS requires less time, yielding better results10. Moreover, a three-dimensional power Doppler ultrasound combined with VOCAL software, which relies on a three-dimensional reconstruction method, can automatically calculate the vascularization index (VI), blood flow index (FI), and vascularization flow index (VFI), providing a three-dimensional visual display of the ovarian vascular tree and an objective quantitative assessment of ovarian blood perfusion11.
However, there are few reports on using 3D-TVS to assess the ovarian reserve function in AM and OEM. This study evaluated the diagnostic value of transvaginal three-dimensional in assessing ovarian function in patients with AM and OEM. We also explored the relationship between AMH and quantitative parameters of 3D-TVS.
Methods
Patients
A total of 150 female patients who visited our hospital between January 2023 and May 2024 and underwent an ultrasound examination were included in this study. Inclusion criteria were: (1) married women of childbearing age, aged 20–42 years with (2) both ovaries and no history of pelvic surgery and (3) no history of anti-estrogen drug therapy. Exclusion criteria were the following: (1) patients who had one or both ovaries removed; (2) those who recently used sex hormone drugs; (3) patients with bilateral fallopian tube obstruction; (4) decreased ovarian function or premature ovarian failure caused by unilateral or bilateral ovarian surgery; (5) those who had one or both fallopian tubes removed; (6) patients with other ovarian pathologies besides endometriosis (such as inflammation, simple cysts, tumors, etc.).
Based on ultrasound examination results, patients were randomly divided into three groups: a healthy group (56 cases), an AM group (58 cases), and an OEM group (36 cases).
All patients were informed about the research details and signed an informed consent form. This research was approved by the hospital’s ethics committee (Ethics number: [2023] Fujian Medical College Second Affiliated Hospital Ethics Approval Number [253]).
Diagnostic and assessment criteria
The diagnosis of AM complies with the diagnostic criteria12 set by the Canadian Society of Obstetricians and Gynaecologists, which includes clinical symptoms such as dysmenorrhea, pelvic pain, menorrhagia, and infertility. At least two or more of the following ultrasound signs must be present for the diagnosis: uniformly enlarged uterus with unclear boundaries of myometrial lesions, asymmetrical thickening of the anterior and posterior walls of the myometrium, multiple small cystic areas within the myometrium, hyperechoic islands, sector-shaped acoustic shadows, subendometrial hyperechoic lines or masses, punctate blood flow, and irregular or interrupted JZ (junctional zone).
The diagnosis of OEM was based on the postoperative pathology data.
Instruments and methods
The American GE Voluson E10 Color Doppler Ultrasound Diagnostic System, equipped with a three-dimensional cavity volume probe with a frequency of 5–9 MHz, was used in this study.
Patients underwent a 3D-TVS examination on the 3rd, 4th, and 5th day of their menstrual cycle. After emptying the bladder, the patients were placed in a lithotomy position. The ultrasound probe, covered with a condom, was inserted into the vagina up to the cervix. The first operator performed a routine examination of the uterus and ovaries, assessing the size, shape, echogenicity, etc.; data were grouped according to the AM ultrasound diagnostic standards. Then, the second operator used a two-dimensional ultrasound to locate the maximum diameter of the ovary and applied a 3D mode using the SonoAVC automatic measurement software to detect AFC within the ovaries. All detected follicles were classified based on their diameter sizes, with each distinct follicle color-coded and manually editable to adjust for any recognition biases in the automatic follicle count and size measurements, as shown in Fig. 1.
With power Doppler superimposition, the 3D mode was initiated for volume scanning. After the scan was completed, the Volume Analysis manual method was selected. In transparency mode, the ovarian contour was manually outlined; each section was rotated at an angle of 15°, and 12 outlines were drawn to obtain two complete contours. This reconstruction yielded the ovarian volume (OV). Continuing with the Volume Histogram, the quantitative parameters of ovarian blood flow were obtained, including VI, FI, and VFI. The results were imported into the workstation for retention and analysis records, as shown in Fig. 2. If combined with OEM, the lesion contour was manually outlined using Volume Analysis to obtain the volume of the lesion.
The AFC was taken as the sum of the total AFC from both ovaries. The average values from both ovaries were used for OV, VI, FI, and VFI. For cases with unilateral OEM, the OV was calculated as [(overall volume of the affected ovary - volume of the lesion) + volume of one healthy ovary] ÷ 2; for cases with bilateral OEM, the OV was calculated as (overall volume of both ovaries - volume of the lesion) ÷ 2.
Body mass index (BMI)
Weight and height were measured in a fasting state on the initial visit. BMI was calculated using the following formula:
Blood biochemical examination
Following the ultrasound examination, 5 ml of fasting venous blood was drawn in the morning at any time during their menstrual cycle. After centrifugation, the upper layer of serum was collected. The levels of AMH were determined using the Enzyme-Linked Immunosorbent Assay method.
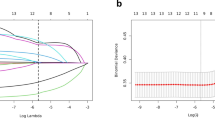
Statistical analysis
Data processing was carried out using SPSS 25.0 software. Measurement data were expressed as mean ± standard deviation \((\overline{x}\pm\text{s})\). Comparisons of parameters among the three groups were performed using analysis of variance (ANOVA). Intergroup comparisons were conducted using the Student’s t-test. A P-value < 0.05 was considered statistically significant. Correlation analysis was performed using Pearson correlation, with a P-value < 0.05 indicating statistical significance. A correlation coefficient (r) between 0.7 and 1.0 indicated a strong correlation, between 0.4 and 0.7 indicated a moderate correlation, and between 0 and 0.4 indicated a weak correlation.
Results
Comparison of clinical baseline data
There were no significant differences in age, menstrual cycle, and BMI among all groups (all P > 0.05), as shown in Table 1.
Comparison of AMH and ultrasonic examination results among different groups
In the AM group, the ultrasound examination showed asymmetric thickening of the anterior and posterior walls of the uterus, the presence of hyperechoic islands, and irregularities in the junctional zone (JZ) (Fig. 3). Compred to healthy group, AM group ovaries had fewer AFC, smaller OV, and lower blood flow parameters (Fig. 4). In the OEM group, the presence of endometriotic cysts in both ovaries, with a reduced number of AFC, smaller OV, and low blood flow parameters, were observed by ultrasound (Fig. 5).
AMH, AFC, OV, VI, FI, and VFI were significantly different in the healthy group, the AM group, and the OEM group (F values were 90.34, 146.50, 92.61, 63.87, 59.50, and 49.36, respectively; all P values < 0.001). The AMH levels in the healthy group were significantly higher than those in the AM and OEM groups (all P < 0.05), indicating better ovarian reserve in healthy patients; the AMH levels in the AM group showed a decline, while the OEM group displayed a significant reduction in AMH, suggesting impairment in ovarian reserve. AFC and OV were maintained at a higher level in the healthy group, while they were reduced in the AM and OEM groups (levels in the OEM group were lower than those seen in the in the AM, all P < 0.05). In addition, VI, FI, and VFI all decreased in the AM and OEM groups compared to the healthy group; levels in the OEM group were lower than those seen in the AM (P < 0.05), as shown in Table 2.
Relationship between AMH and various indicators of 3D-TVS
Pearson correlation analysis revealed that serum AMH levels were positively correlated with AFC, OV, VI, FI, and VFI (r = 0.80, 0.73, 0.50, 0.48, 0.45, respectively; all P < 0.01). Among these, AFC and OV had a strong correlation, while VI, FI, and VFI had a moderate correlation.
Discussion
AM is a common gynecological condition among women of reproductive age, which can lead to infertility. A recent meta-analysis showed that women with potential AM have lower levels of AMH, i.e., reduced ovarian reserve function6. This study found that patients with AM and OEM had lower levels of AMH, AFC, and OV than healthy patients, with the greatest impact observed in the group with OEM. This could be due to the aberrant expression of many inflammatory mediators in the endometrium of patients with AM, creating a pro-inflammatory network1. Inflammation may induce excessive oxidative stress, leading to ovarian cortical fibrosis and DOR during folliculogenesis, causing decreased oocyte DNA damage13,14,15. As inflammation spreads, the extent of ovarian damage increases.
In this study, patients with OEM showed significantly lower AMH, AFC, and OV compared to the healthy group, which is consistent with a meta-analysis16that reported that the presence of OEM is associated with a significant reduction in AFC and AMH, suggesting reduced ovarian reserve in OEM patients. This could be related to the inflammation and transformation of the healthy cortical structure caused by the development of OEM lesions, diminishing the physiological function of the adjacent ovarian cortex as a follicular reservoir17.
Our patients with AM and OEM had reduced ovarian blood perfusion compared to the healthy group, and the group with OEM exhibited the most severe reduction. The formation of OEM cysts is detrimental to the ovaries, possibly through structural tissue changes or direct damage to ovarian follicles by invading the ovarian cortex18. Additionally, OEM cysts might compress ovarian vessels, decreasing ovarian blood flow. Furthermore, our research results show that ovarian blood perfusion in patients with AM is reduced. This could potentially be related to ovarian dysfunction caused by excessive estrogen and progesterone resistance19, where excessive estrogen is negatively fed back to reduce androgens. Subsequently, secondary reductions in AMH occur due to decreased androgen levels, leading to lower expression of vascular endothelial growth factor and insulin-like growth factor, thus reducing ovarian blood perfusion11. It is also possible that retrograde menstruation led to endometrial cells infiltrating the myometrium and the ovaries20, resulting in DOR.
This study showed that serum AMH levels were positively correlated with AFC, OV, VI, FI, and VFI, with AFC having the strongest correlation, which is largely consistent with data reported by Sinha et al.21. Compared to other markers, AMH more accurately reflects the continuous decline of the follicular pool with age, and it seems to be the best indicator of the gradual reduction in AFC and OV22. AMH is considered the most reliable method for assessing ovarian reserve but is more expensive than the relatively cost-effective AFC, making AFC a viable option for ovarian reserve testing23. This is particularly applicable to patients with lower socioeconomic status and family income.
Ovarian reserve function refers to the ability of the ovarian cortex to produce follicles and for those follicles to develop into fertilizable oocytes. DOR accounts for approximately 20% of ovarian diseases in women, with an incidence rate of about 10% in the infertile population. The prevalence of DOR is gradually increasing, with a trend towards affecting younger patients24. Therefore, an early and accurate assessment of a patient’s ovarian reserve function, timely diagnosis, and prompt treatment are of great importance clinically in improving fertility rates and preventing premature ovarian failure25. In the past, the assessment of ovarian reserve function primarily involved biochemical testing to measure hormone levels; however, this approach has certain limitations as it does not provide morphological information on the ovaries9,26. 3D-TVS is the best method for monitoring follicles and is currently the most accurate method available. 3D-TVS compensates for the deficiencies of two-dimensional ultrasound in providing quantitative indicators and ovarian volumetric measurement, allowing for a more intuitive and precise evaluation of OV9. The strength of this study lies in its integration of advanced imaging techniques, specifically the transvaginal three-dimensional SonoAVC technology, with serum AMH levels to provide a comprehensive assessment of ovarian reserve function. This approach enhances the accuracy and reliability of ovarian reserve evaluation and offers valuable insights for clinical decision-making and treatment strategies for patients with AM. Furthermore, identifying ovarian reserve decline early and providing targeted interventions can significantly impact patient outcomes, potentially delaying or reversing the progression to premature ovarian insufficiency.
The study has several limitations, including the relatively small number of patients included. Due to time constraints, long-term follow-up observations were not possible, which limited our ability to gain further insights into the pregnancy outcomes and subsequent changes in ovarian function among the groups. Future studies should expand the sample size and include subsequent observations.
Conclusions
AM and OEM impaired ovarian reserve function; however, OEM had a stronger effect on ovarian reserve function than AM. Our data also suggested that 3D-TVS compensates for the shortcomings of two-dimensional ultrasound, thus being an important examination for assessing ovarian reserve function. By conducting 3D-TVS examinations in all groups, those with OEM and AM had poorer ovarian reserve function than the healthy group. The mechanisms leading to our study results may be related to various factors such as inflammation, structural tissue changes, direct damage to ovarian follicles, vascular compression by OEM cysts, hormonal imbalances, and endometrial cell infiltration into the ovaries due to retrograde menstruation. AFC and OV are the optimal indicators for evaluating ovarian reserve function in patients with AM and OEM.
Data availability
All data generated or analysed during this study are included in this published article.
References
Zhai, J., Vannuccini, S., Petraglia, F. & Giudice, L. C. Adenomyosis: mechanisms and Pathogenesis. Semin Reprod. Med. 38, 129–143 (2020).
Martone, S. et al. Pathophysiologic mechanisms by which adenomyosis predisposes to postpartum haemorrhage and other obstetric complications. Med. Hypotheses. 143, 109833 (2020).
Younes, G. & Tulandi, T. Effects of adenomyosis on in vitro fertilization treatment outcomes: a meta-analysis. Fertil. Steril. 108, 483–490e483 (2017).
Abu Hashim, H., Elaraby, S., Fouda, A. A. & Rakhawy, M. E. The prevalence of adenomyosis in an infertile population: a cross-sectional study. Reprod. Biomed. Online. 40, 842–850 (2020).
Howard, J. A., Hart, K. N. & Thompson, T. B. Molecular mechanisms of AMH Signaling. Front. Endocrinol. (Lausanne). 13, 927824 (2022).
Gulino, F. A. et al., Anti-Mullerian Hormone (AMH) and adenomyosis: Mini-review of literature of the last 5 years. Front. Endocrinol. (Lausanne) 1014519 (2022).
Horton, J. et al. Reproductive, obstetric, and perinatal outcomes of women with adenomyosis and endometriosis: a systematic review and meta-analysis. Hum. Reprod. Update. 25, 592–632 (2019).
The Effect of Surgery for Endometriomas on Fertility. Sci. Impact Paper 55 BJOG 125, e19–e28 (2018).
Chen, Q. et al. Three-dimensional transvaginal ultrasonography in the evaluation of diminished ovarian reserve and premature ovarian failure. Pak J. Med. Sci. 39, 747–751 (2023).
Silva, V. et al. Junctional Zone in Infertile women: a three-dimensional Ultrasound Study. Rev. Bras. Ginecol. Obstet. 42, 152–159 (2020).
Wang, W. Q., Chu, G. H. & Hou, X. X. A comparison of Doppler measures of ovarian blood flow between women with and without ovarian dysfunction and correlations of Doppler indices with ovarian dysfunction markers: a meta-analysis. Ann. Transl Med. 11, 110 (2023).
Dason, E. S. et al. Guideline 437: diagnosis and management of adenomyosis. J. Obstet. Gynaecol. Can. 45, 417–429e411 (2023).
Tan, Z. et al., What We Have Learned from Animal Models to Understand the Etiology and Pathology of Endometrioma-Related Infertility. Biomedicines. 10, (2022).
Hayashi, S. et al. Novel ovarian endometriosis model causes infertility via iron-mediated oxidative stress in mice. Redox Biol. 37, 101726 (2020).
Cacciottola, L., Donnez, J. & Dolmans, M. M. Can endometriosis-related oxidative stress pave the way for New Treatment targets? Int. J. Mol. Sci. 22, (2021).
Tian, Z., Zhang, Y., Zhang, C., Wang, Y. & Zhu, H. L. Antral follicle count is reduced in the presence of endometriosis: a systematic review and meta-analysis. Reprod. Biomed. Online. 42, 237–247 (2021).
Kitajima, M. et al. Association between ovarian endometrioma and ovarian reserve. Front. Biosci. (Elite Ed). 10, 92–102 (2018).
Karadag, C., Yoldemir, T., Demircan Karadag, S. & Turgut, A. The effects of endometrioma size and bilaterality on ovarian reserve. J. Obstet. Gynaecol. 40, 531–536 (2020).
Lamceva, J., Uljanovs, R. & Strumfa, I. The main theories on the pathogenesis of endometriosis. Int. J. Mol. Sci. 24, (2023).
Bulun, S. E. et al. Endometriosis and adenomyosis: shared pathophysiology. Fertil. Steril. 119, 746–750 (2023).
Sinha, S., Sharan, A. & Sinha, S. Anti-mullerian hormone as a marker of Ovarian Reserve and function. Cureus 14, e29214 (2022).
Dayal, M., Sagar, S., Chaurasia, A. & Singh, U. Anti-mullerian hormone: a new marker of ovarian function. J. Obstet. Gynaecol. India. 64, 130–133 (2014).
Anuradha, K., Majumder, P. & Shiffin, R. Correlation of anti mullerian hormone and Antral Follicular Count in Ovarian Reserve Testing. Obstet. Gynecol. Res. 5, 170–174 (2022).
Ata, B., Seyhan, A. & Seli, E. Diminished ovarian reserve versus ovarian aging: overlaps and differences. Curr. Opin. Obstet. Gynecol. 31, 139–147 (2019).
Zhang, Q. L. et al. Treatment Progress in diminished Ovarian Reserve: western and Chinese medicine. Chin. J. Integr. Med. 29, 361–367 (2023).
Karakus, S., Yildiz, C., Aydin, H., Akkar, O. & Cetin, A. Value of in situ ovarian volume measured during cesarean delivery to assess the potential of diminished ovarian reserve. J. Matern Fetal Neonatal Med. 30, 1016–1022 (2017).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Hui Yin, Jiemin Chen and Qiuyue Chen carried out the studies, participated in collecting data, and drafted the manuscript. Guorong Lyu and Qiuyue Chen performed the statistical analysis and participated in its design. Hui Yin and Guorong Lyu participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This research was approved by the hospital’s ethics committee (Ethics number: [2023] Fujian Medical College Second Affiliated Hospital Ethics Approval Number [253]). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yin, H., Chen, J., Chen, Q. et al. Assessment of ovarian reserve function in patients with adenomyosis and ovarian endometriosis by three-dimensional transvaginal ultrasound and Anti-Müllerian hormone. Sci Rep 14, 30799 (2024). https://doi.org/10.1038/s41598-024-81033-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81033-6
Keywords
This article is cited by
-
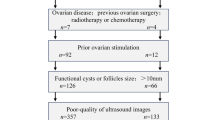
Analysis of cumulative live birth rate outcomes of four ovarian stimulation protocols in Poseidon groups 3/4 patients with adenomyosis
Journal of Assisted Reproduction and Genetics (2025)