Abstract
Hypertension causes aortic wall thickening until the original wall stress is restored. We hypothesized that this regulation involves stress fiber (SF) tension transmission to the nucleus in smooth muscle cells (SMCs) and investigated the strain in the SF direction as a condition required for this transmission. Thoracic aortas from Wistar Kyoto (WKY) and spontaneously hypertensive rats (SHRs) were examined. SFs in aortic SMCs were fluorescently labeled and observed under a confocal microscope while stretched along the circumferential (θ) axis. Three conditions were studied: WKY physiological (WKYphys; blood pressure changes from diastolic to systolic for WKY), high-strain state (WKYhigh; diastolic to hypertensive level for WKY simulating initial hypertension), and SHR physiological (SHRphys; diastolic to systolic for SHR simulating after wall-thickening). SF strain and direction were measured. The SF inclination angle from the θ axis was 18° ± 3° in WKYphys, 13° ± 2° in WKYhigh, and 20° ± 1° in SHRphys. SF strain was 0.01 ± 0.02 in WKYphys, 0.20 ± 0.04 in WKYhigh, and 0.02 ± 0.02 SHRphys. SF strain was minimal in WKYphys, significantly increased in WKYhigh, and reduced to approximately zero in SHRphys. These findings support SFs function as mechanosensors in response to hypertension.
Similar content being viewed by others
Introduction
The aortic wall thickens under hypertension1,2,3 and is accompanied by increased protein production, such as collagen1, and the hypertrophy of smooth muscle cells (SMCs)2. This thickening is believed to maintain constant circumferential tensile stress3, which is proportional to intraluminal pressure and inversely proportional to the wall thickness, according to Laplace’s law. Spontaneously hypertensive rats (SHRs) also exhibit wall thickening4, SMC hypertrophy5, and increased production of proteins such as collagen6. These responses in the aortic media are associated with SMCs, suggesting that SMCs regulate wall thickening under hypertension. However, how SMCs sense the changes in blood pressure, respond to them, and stop the response remains poorly known.
SMCs are aligned circumferentially in the aortas7, are subjected to circumferential tensile stress due to blood pressure, and respond to stretching. Numerous reviews have discussed the response of SMCs to stretching8,9,10. Cyclic stretching of cultured SMCs upregulates collagen synthesis11 and mitogen-activated protein kinase12, a regulator of proliferation and differentiation, leading to SMC hypertrophy12. Thus, hypertension-caused wall thickening is attributed to the SMCs’ stretch response. However, the mechanisms by which SMCs sense the stretch and convert it to chemical signals remain unknown. Several studies have reported that forces applied to cells are transmitted to the cell nucleus via stress fibers (SFs)13,14. Nagayama et al.13 reported that force applied through SFs altered DNA distribution in the nucleus, converting aggregated heterochromatin into euchromatin. Since euchromatin has a higher transcription rate due to its low aggregation15, increased tension in SFs might enhance gene transcription.
The SF direction relative to the stretch direction affects the magnitude of transmitted forces. When a cyclic stretch was applied to human fibroblasts of the patellar tendon, cells that aligned with the stretching direction produced more alpha-smooth muscle actin, indicating differentiation into myofibroblasts16,17. Since SFs in cultured SMCs generally align with the cell’s long axis18, SF tension should be high when cells are stretched parallel to their long axis. Additionally, the deformation of SMC nuclei depends on the stretch direction: circumferential stretching of aortic tissue deforms SMC nuclei, whereas axial stretching hardly does so19.
In aortic tissues at normal blood pressure, the pulse pressure from diastolic to systolic does not induce significant strain in the SF direction. In the thoracic aorta, SFs are oblique to the elastic lamina (EL) plane (longitudinal-circumferential plane)20 with an inclination angle of 17° from the circumferential (θ) to the radial-circumferential (r-θ) plane21. We reported a normal strain of almost zero at 120 mmHg in the SF direction21, indicating that SFs align in the zero strain direction under normal blood pressure, which indicates no stretch or shrinkage.
Based on these studies, we hypothesized that SF tension regulates the wall-thickening response of SMCs under hypertension. In the initial hypertension phase, elevated circumferential tensile stress likely increases SF strain, leading to greater nuclear deformation and altered gene transcription, driving wall thickening. According to this hypothesis, SF strain must return to its original value after wall thickening ceases. In this study, as the necessary condition for this hypothesis, we measured strain in the SF direction under normal pressure, in a high-strain state simulating initial hypertension phase without wall-thickening, and at physiological pressure in wall-thickened hypertensive rats.
Methods
Tested three states
We examined three blood pressure conditions. In the WKYphys group, blood pressure changes from diastolic to systolic were tested as normal physiological pulse pressure. In the WKYhigh group, blood pressure changes from normal diastolic pressure to hypertensive systolic pressure were tested, simulating strain at the initial hypertension phase without wall-thickening. The hypertensive systolic pressure was set at 179 mmHg based on preliminary measurements of SHR systolic pressure. In the SHRphys group, blood pressure was changed from diastolic to systolic at a hypertensive level to reflect the physiological pulse pressure of SHRs, representing the state after wall thickening. The first two conditions were tested using Wistar Kyoto (WKY) rats, which have normal blood pressure, and the last condition was tested using SHRs.
Animals
We used five WKY/Izm and five SHR/Izm rats (male, 10–14 weeks, 250–324 g, Japan SLC, Shizuoka, Japan). All animal experiments were approved by the Institutional Review Board of Animal Care at Nagoya Institute of Technology (approval numbers #2020008, #2021006, and 2022003) and performed according to the relevant guidelines, following recommendations from their Guide for Animal Experimentation and this study is reported under ARRIVE guidelines (https://arriveguidelines.org).
Systolic and diastolic blood pressures were monitored using a noninvasive tail-cuff plethysmography system (BP-98A-L, Softron, Tokyo). Each rat was measured three times, and the average was used as the data point.
Aorta resection
The thoracic aorta was resected as described in previous studies22,23. Briefly, rats were euthanized in a CO2 chamber, and the thoracic aorta was exposed by trimming fat and loose connective tissues. The in vivo longitudinal length was marked with gentian violet dots at 3-mm intervals on the aorta surface. After cauterizing the intercostal arteries, a 2–3 cm-long tubular specimen was obtained. The specimen was preserved in 4 ℃ Krebs–Henseleit solution and used within 24 h.
Pressure–diameter test
The pressure–diameter test was performed on the obtained tubular specimen using an experimental setup (Fig. 1a) reported previously22,23. The specimen was held with longitudinal elongation to its in vivo length using gentian violet markers. Intraluminal pressure was set (Fig. 1b) at diastolic and systolic levels using a pressure-pneumatic regulator (640BA20B, Asahi Enterprise, Asahi Enterprise, Tokyo, Japan), digital-analog/analog–digital (DA/AD) converter (NI USB-6363, National Instruments, Austin, TX, USA), software (NI LabVIEW2010, National Instruments), sensor (ASM1-010B-G-2F-2B-03-A, SETRA), and personal computer (FMV BIBLO, Fujitsu, Tokyo, Japan; PC). For the WKYhigh, the WKY sample was also pressurized at the hypertension level. The specimen was imaged using a camera (XCAM4K8MPB, RelyOn, Tokyo, Japan) and a stereoscopic microscope (SZX16, Olympus, Tokyo, Japan).
Experimental devices. (a) Experimental setup of the pressure-diameter test. (b) Image of the aorta during intraluminal pressurization. (c) Binarized image of (b). Diameter was measured at three positions (yellow lines). (d) Experimental setup for the tensile tester. The sample was fixed on a PET film with adhesive, and a fluorescent image was captured using a microscope. (e) Representative image of the specimen under a tensile test.
Aortic diameter was measured from captured images using ImageJ Fiji (1.53c, National Institutes of Health, Bethesda, MD, USA). Diameters were measured at three positions (Fig. 1c) and averaged for each condition: 0 mmHg (D0), diastolic pressure (Ddia), and systolic pressure (Dsys). For the WKYhigh, the diameter at hypertensive pressure (Dhyp) was also measured. The circumferential stretch ratio λx of the aorta under each pressure condition x (x = dia, sys, hyp) was calculated as
This stretch ratio was used in the tensile test section. The circumferential strain εtissue applied to aortic tissue was also calculated based on the diastolic pressure.
Stress fiber labeling
The tubular specimen was sectioned perpendicularly to its long axis to obtain a ring specimen. After the pressure-diameter test, the specimen was embedded in a 3% agar (01,059–85, Nacalai Tesque, Kyoto, Japan) solution and sliced into 200-μm-thick sections using a micro-slicer (DTK-1000, Dosaka-EM, Kyoto, Japan). The SFs of SMCs in a ring specimen were fluorescently labeled by immersion in 330 nM Alexa fluor 647 phalloidin (A22287, Thermo Fisher Scientific, MA, USA) in phosphate-buffered saline [PBS(-)] containing 0.2% bovine serum albumin (019–23,293, Fuji-film Wako, Osaka, Japan) for 2 h. The specimen was then washed with PBS(-). In a few specimens, nuclei of SMCs are stained with 5 µg/mL Hoechst 33,342 (Life Technologies, Carlsbad, CA, USA).
Tensile test and fluorescent microscopy
The ring specimen with fluorescently labeled SFs was uniaxially stretched in the circumferential direction. The laboratory-made tensile tester24 is presented in Fig. 1d. Parts of the ring specimen were glued on a polyethylene terephthalate (PET) film, which was then attached to a lever arm of the tensile tester. The tester was placed under a confocal laser scanning microscope (FV3000, Olympus, Tokyo, Japan). The ring specimen was immersed in PBS(-) at room temperature.
The specimen was stretched circumferentially at 0.1 mm/s (Fig. 1e). The initial length (L0) was determined when the tester detected a force change of 0.24 mN, which is the force resolution of the tester. The bulk stretch ratio (λ) was calculated as
where L is the length of the specimen in the tensile direction. A five-cycle preconditioning was performed in the range λ= 1–1.5 before the tensile test.
ELs and SFs in the r−θ plane were imaged with a 60 × objective lens (NA = 1.0, LUMPLFLN60XW, Olympus). Laser light was used for ELs (488 nm, 2%–10% power) and SFs (640 nm, 2%–10% power) with 10.0 µs/pixel scanning. EL autofluorescence and SF fluorescence were imaged using 490–590 nm and 650–750 nm bandpass filters, respectively. The captured longitudinal (z-) direction range was 30–60 µm from the ring specimen surface at Δz = 0.41 µm intervals.
ELs were locally photobleached as strain markers using a 488 nm laser at 10% power for 30 s, as described previously23,25. Photobleaching was performed in two 100-µm apart regions in a single EL.
The ring specimen was stretched to reach diastolic λdia and systolic stretch ratio λsys. For WKY rats, the specimen was also stretched to hypertension level λhyp. At each stretch ratio, the r-θ plane of the ring specimen was imaged as described.
Stress fiber direction and thickness measurements
Images were analyzed using ImageJ Fiji. Maximum intensity projection images were taken for SFs and ELs. The “Directionality” function was applied to the EL image to determine the EL orientation as the angle with the maximal probability. The image was then rotated to align the EL direction with the horizontal axis, defining the θ axis. The same rotation was applied to the SF image. SF angles αSF were measured from the circumferential direction, averaging at least three SFs per analyzed area.
Aortic thickness was measured by averaging the distance between internal and external ELs at three positions.
Strain analysis
Marker positions were determined as displayed in Fig. 2. For a photobleached marker in EL (Fig. 2a), a 10-µm line segment was drawn across the EL and along the r-axis (Fig. 2b). The line position was slightly shifted from the marker to the image center, where EL was visible. The intensity I distribution of the line segment was fitted to a Gaussian function:
where a, b, c, and d were fitting parameters (Fig. 2c). Parameter c, indicating the intensity center, was used as the marker position in the r-axis. The EL image was then inverted (Fig. 2d), and a ten-micrometer line segment was drawn along the θ axis, on the EL, and over the marker (Fig. 2e). A similar process was applied along the θ axis to determine the marker position in the θ axis.
Schematic of image analysis. (a) Image of EL autofluorescence captured in the radial-circumferential (r-θ) plane. (b) An analysis line segment was drawn near the marker along the r-axis, toward the center of the image from the marker, to obtain the marker coordinate in the r-axis. (c) A Gaussian function was fitted to the intensity curve along the analysis line in (b). (d) Inverted image of (a). (e) An analysis line segment was drawn on the marker along the θ axis, aligned with the centerline of the EL, to obtain the marker coordinate in the θ axis. (f) A Gaussian function was fitted to the intensity curve along the analysis lines in (e). (g and h) The four makers (i, j, k, l) in (g) real coordinates (r, θ) were converted to (± 1, ± 1) in (h) the imaginary coordinates (ξ, η) before deformation. The same converting function was then applied to the markers after deformation. Strain was first calculated in the imaginary coordinates and then converted to the real coordinates. For details, see Sugita et al.23.
The strain between images was measured using isoparametric mapping with a first-order shape function, calculating 2D infinitesimal strains of four markers and converting them to real axes using Jacobian23. The coordinates of four markers (i, j, k, l) in real axes (θ, r) in the image before deformation were converted to (± 1, ± 1) in the imaginary axes (ξ, η) using a shape function. The coordinates of these markers in the image after deformation were similarly converted to imaginary axes (ξ, η) using the same shape function. In these imaginary coordinates, the 2D infinitesimal strains of the four markers between the two images were calculated and converted back to the real axes strains using Jacobian. Through this process, normal circumferential strain (εθθ), normal radial strain (εrr), and shear strain (εrθ) were calculated. From these three strains, we calculated the first principal strain (ε1), indicating the maximum strain in the smooth muscle-rich layer (SML) in the r-θ plane, the second principal strain (ε2), representing the minimum normal strain, and the first principal strain direction (α1), indicating the direction of ε1. The normal strain in the SF direction (εSF) and the zero normal strain direction (αmin), which indicate no stretch or shrinkage, were also calculated as previously reported21. The εSF was also normalized with the macroscopic circumferential strain εtissue to compare the magnitude of strains.
Statistical method
Data among the WKYphys, WKYhigh, and SHRphys groups were analyzed using the Steel–Dwass test with R software v. 1.53t (R core team). WKY and SHR were compared using the Mann–Whitney U test, using the same software. The results were expressed as plots with mean ± standard deviation (SD). A significance level of P ≤ 0.05 was used.
Results
SHR displayed hypertension and wall thickening
WKY and SHR rats weighed 296 ± 18 g and 273 ± 15 g, respectively. Although the difference was not statistically significant (U value = 3.5, number of WKY nWKY = 5, number of SHR nSHR = 5), WKY rats tended to be heavier.
Figure 3a presents the blood pressure measurements for WKY and SHR rats. Systolic and diastolic pressures in SHRs (systolic, 193 ± 6 mmHg; diastolic, 156 ± 6 mmHg) were significantly higher than in WKYs (systolic, 116 ± 11 mmHg; diastolic, 80 ± 12 mmHg; U value = 0), confirming that SHRs are hypertensive.
Blood pressure and wall thickness of individuals and their mean ± SD. (a) Systolic and diastolic blood pressures of SHR and WKY. Those pressures were significantly higher in SHR than in WKY (U value = 0). (b) SHR and WKY wall thickness. The SHR wall thickness tended to be higher, but the difference was not significant (U value = 3). (c) Wall thickness normalized by rat weight. The normalized SHR wall thickness was significantly higher than that of WKY (U value = 0). These results confirmed that SHRs are hypertensive and have thickened aortic walls. WKY, Wistar Kyoto rat; SHR, spontaneously hypertensive rat; Dia, diastolic blood pressure; Sys, systolic blood pressure; N, number of rats. Analyzed using the Mann–Whitney U test.
SMC nuclei were observed between the ELs and aligned in the circumferential axis (see Supplementary Fig. S1 online). Wall thickness was measured from the autofluorescence of IEL and EEL. Figure 3b presents the wall thickness of WKY and SHR aortas. Although SHR wall thickness tended to be greater than that of WKY, the difference was not statistically significant (U value = 3, nWKY = 5, nSHR = 5). Since larger animals typically have larger organs, we normalized wall thickness by rat weight (Fig. 3c). The normalized SHR wall thickness was significantly greater than that of WKY (U value = 0, nWKY = 5, nSHR = 5). This result indicates that SHRs remodel and thicken the aortic wall to adapt to hypertension.
Aortic walls elongated circumferentially and shrunk radially with shear strain
The circumferential strains applied to aortic sample were εtissue = 0.08 ± 0.04 in WKYphys, εtissue = 0.18 ± 0.07 in WKYhigh, and εtissue = 0.08 ± 0.03 in SHRphys. The WKYhigh aortic tissue was stretched 2.3 times of WKYphys, and SHRphys showed no difference.
Figure 4 displays ELs and SFs during a tensile test. The strain markers on ELs indicate aorta deformation. Figure 4a,b and Movie 1 illustrate the deformation of WKY aortas from diastolic (Fig. 4a) to systolic pressure (Fig. 4b). The distance between two markers on the same EL increased, indicating aorta elongation along the θ axis. Due to the Poisson effect of the circumferential stretch, the aorta shortened radially. The two markers on adjacent ELs moved differently along the θ axis, resulting in a shear strain in the r-θ plane. Several SFs bridged two neighboring ELs obliquely. These observations agreed with previous studies23. Figure 4a,c, and Movie 2 present the deformation of the WKY aorta from diastolic (Fig. 4a) to hypertensive pressure (179 mmHg) (Fig. 4c). The aorta in Fig. 4c got more deformed than the one in Fig. 4b.
Elastic laminas (ELs, red) and stress fibers (SFs, green) in the aorta in the radial-circumferential (r- θ) plane. Images were captured at (a) diastolic pressure from WKY, (b) systolic pressure from WKY, (c) 179 mmHg from WKY, (d) diastolic pressure from SHR, and (e) systolic pressure from SHR. Yellow arrowheads indicate the photobleached marker positions in ELs used to calculate strains. Insets at the bottom right of each panel indicate enlarged areas of the white-boxed regions. WKY, Wistar Kyoto rat; SHR, spontaneously hypertensive rat. Image intensity was adjusted to enhance visibility. Scale bars = 50 μm.
Figure 4d,e, and Movie 3 display the deformation of SHR aortas from diastolic (Fig. 4d) to systolic pressure (Fig. 4e). The strain markers moved similarly to those in Fig. 4a–c, indicating that the aortic tissue elongated along the θ axis, shortened along the r-axis, and neighboring ELs moved oppositely along the θ axis.
From the deformation images, we quantified normal circumferential strain εθθ, normal radial strain εrr, and the absolute value of shear strain |εrθ| (Fig. 5a) of the SML in the WKYphys, WKYhigh, and SHRphys groups. Figure 5b indicates the εθθ values. In WKYphys, εθθ was 0.04 ± 0.03, suggesting that the aorta’s circumference increased by 4% due to pulse pressure changes in normal pressure rats. The normal strain εθθ of WKYhigh was 0.21 ± 0.05, indicating that the aortic tissue elongates along the θ axis when blood pressure suddenly increases. The normal strain εθθ of SHRphys was 0.04 ± 0.01, which was significantly smaller than that of WKYhigh and similar to that of WKYphys. These results suggest that aortic tissues experience increased strain along the θ axis when blood pressure becomes hypertensive, while the strain from diastolic to systolic pressures returns to ~ 4% after wall thickening.
Normal circumferential strain εθθ, normal radial strain εrr, and absolute shear strain |εrθ| in the radial-circumferential (r-θ) plane. (a) Schematic illustration of strains εθθ, εrr, and εrθ. Aortic tissue before deformation (dashed line) changes into the tissue after deformation (solid line). (b–d) Strains of (b) εθθ, (c) εrr, and (d) |εrθ| of WKYphys, WKYhigh, and SHRphys. A significant difference was found for εθθ and εrr only in WKYhigh. WKYphys, state from diastolic to systolic blood pressure in WKY rats; WKYhigh, state from diastolic to hypertensive blood pressure (179 mmHg) in WKY rats; SHRphys, state from diastolic to systolic blood pressure in spontaneously hypertensive rats. Analyzed using the Steel–Dwass test.
Figure 5c presents the normal strain in the radial direction εrr. The εrr of the WKYphys was − 0.05 ± 0.02, suggesting that the aortic wall thins by ~ 5% from diastolic to systolic pressures in normal pressure rats. Because the thickness decreased along the r-axis, the values were negative. The εrr of the WKYhigh was − 0.12 ± 0.03, significantly smaller than that of the WKYphys, indicating that the wall thickness further thins along the r-axis when blood pressure suddenly increases. The radial strain εrr of SHRphys was significantly larger than that of WKYhigh and recovered to − 0.03 ± 0.03, comparable to that in WKYphys. These results suggest that the aortic tissues temporarily thin along the r-axis when blood pressure becomes hypertensive. After wall thickening, hypertensive rats recover − 5% of strain in the r-axis from diastolic to systolic pressures.
Figure 5d presents the absolute value of shear strain |εrθ|. The strain |εrθ| for WKYphys, WKYhigh, and SHRphys were 0.05 ± 0.04, 0.07 ± 0.08, and 0.02 ± 0.02, respectively. No significant differences were observed among them.
Strain in stress fiber direction increases under a high-strain state and returns to normal strain levels in the wall-thickened rats
As strain changes with direction (Fig. 5), we calculated the first principal strain ε1, which indicates the maximum strain, and the strain in SF direction εSF. Figure 6 displays the magnitude and direction of the first principal and SF direction strains in the r-θ plane. In WKYphys, the two strains were distributed around the origin, meaning that ε1 and εSF were small in magnitude. In WKYhigh, ε1 exceeded 0.15, and εSF ranged from 0.14 to 0.25, higher than in WKYphys. In SHRphys, ε1 and εSF were distributed around the origin, suggesting that the strain magnitude returns to a lower level.
The magnitude and direction of the first principal strain ε1 and the strain in the SF direction εSF for WKYphys, WKYhigh, and SHRphys. In this graph, the direction and distance from the origin to the plots indicate the strain direction and magnitude, respectively. Numbers on gray circles indicate strain magnitude. WKYphys, state from diastolic to systolic blood pressure changes in WKY rats; WKYhigh, state from diastolic to hypertensive blood pressure (179 mmHg) changes in WKY rats; SHRphys, state from diastolic to systolic blood pressure changes in spontaneously hypertensive rats; r, radial direction; θ, circumferential direction.
Figure 7a displays the SF direction αSF. In WKYphys, SFs were aligned at αSF = 18° ± 3° from the θ axis in the r-θ plane. This angle significantly decreased to αSF = 13° ± 3° in WKYhigh, indicating that the SFs align more closely to the θ axis with a sudden increase in blood pressure. In SHRphys, SFs aligned at αSF = 20° ± 2°, similar to the angle in WKYphys, indicating that the SF angle returned to normal level after wall thickening.
SF direction αSF and strain in the SF direction εSF in WKYphys, WKYhigh, and SHRphys. (a) The absolute value of SF direction αSF relative to the circumferential direction. (b) Strain in the SF direction εSF. Significant differences in αSF and εSF were found only in WKYhigh. WKYphys, state from diastolic to systolic blood pressure in WKY rats; WKYhigh, state from diastolic to hypertensive blood pressure (179 mmHg) in WKY rats; SHRphys, state from diastolic to systolic blood pressure in spontaneously hypertensive rats. Analyzed using the Steel–Dwass test.
Figure 7b presents the strain εSF in the SF direction. In WKYphys, the strain was εSF = 0.01 ± 0.03 indicating minimal strain. The normalized εSF relative to the circumferential tissue strain εtissue was 0.00 ± 0.45, suggesting that SFs orient themselves toward zero normal strain to avoid strain from diastolic to systolic pressures. In WKYhigh, the strain εSF in the SF direction was εSF = 0.20 ± 0.04, significantly higher than —32.9 times that of WKYphys. The normalized εSF with εtissue was 1.35 ± 0.59, exceeding that of WKYphys. In SHRphys, the strain was εSF = 0.02 ± 0.02, 2.9 times higher than WKYphys, with a normalized εSF of 0.23 ± 0.24, lower than WKYhigh. The εSF in SHRphys was significantly lower than WKYhigh but not significantly different from WKYphys. These results indicate that strain levels returned to those observed in WKYphys.
We compared SF direction αSF with the directions of the first principal (maximum) strain α1 and zero normal strain αmin at the same position to evaluate whether SF direction returned to zero normal strain direction in SHRphys (see Supplementary Fig. S2 online). In WKYphys, αSF (green ○) was closer to the αmin (black ○) in 5 out of 6 data points, indicating that SFs align in the non-stretched direction. In WKYhigh, αSF (green ●) was closer to the α1 (red ●) in 4 out of 6 specimens, indicating that SFs are directed in a well-stretched direction. In SHRphys, αSF (green □) was closer to the α1 (red □) in 4 out of 8 data points, with the other half closer to αmin (black □). This result suggests that, while the SF direction in SHRphys tended to realign to the original direction of WKYphys, it did not fully recover. The average angles of α1 and αmin from αSF are displayed in Supplementary Fig. S3 online. This quantified data indicates that the SF angle αSF is significantly closer to the αmin in WKYphys, while it is significantly closer to α1 in WKYhigh. In SHRphys, αSF tended to be closer to the αmin, though the αSF and αmin angles were not significantly different from the αSF and α1 angles.
Discussion
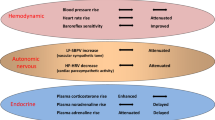
Our previous study21 demonstrated that the aortic tissue strain in the SF direction during physiological pressurization was almost zero, indicating that pulse pressure changes do not induce SF strain and stress. This study confirmed zero strain in the SF direction from diastolic to systolic pressures in WKYphys (Fig. 7b). If SFs act as mechanosensors transmitting forces to SMCs during hypertension-caused wall thickening, the SF strain should increase with a sudden blood pressure rise. Moreover, since circumferential stress returns to the normal physiological level a few weeks after blood pressure elevation2, halting wall thickening, the strain in the SF direction should become nearly zero after thickening. This study demonstrates these SF strain changes, as illustrated in Fig. 8. Under normal blood pressure in WKYphys, the strain in the SF direction was zero. Strain increased in the high-strain state, simulating a sudden rise in blood pressure in WKYhigh and returned to zero in SHRphys. Thus, SFs are mechanosensor candidates triggering wall thickening.
In vitro studies have demonstrated that SFs align in zero strain directions in cells23,26. This alignment trend was confirmed in the aortic tissues21, including in this study, under normal physiological pressure (WKYphys). This alignment was also found at physiological pressure in hypertensive rats (SHRphys). These results strongly suggest that SFs align in the zero-strain direction regardless of the mechanical environment.
Matsumoto and Hayashi3 induced hypertension by clipping the renal artery to reduce blood flow, confirming wall thickening of the aortic media, with circumferential normal stress returning to normal blood pressure levels. SHRs displayed increasing blood pressure until ten weeks old27, and their aortic walls were thicker than those of WKY28. This study also confirmed elevated pressure and wall thickening in SHR compared to WKY, validating SHR as a model for wall thickening under hypertension.
Only large stretches due to significant blood pressure changes would be considered to increase strain in the SF direction in WKYhigh. We agree that significant stretches occurred due to large blood pressure changes in WKYhigh. However, SF aligns in almost zero strain direction at normal pressures, indicating that it cannot transmit strain or force in the angle. The SF direction also changed in WKYhigh, likely enhancing force transmission through SFs (Fig. 7a). If strains εrr, εθθ, and |εrθ| in SHRphys were applied to the SF angle αSF in WKYhigh, the SF direction strain εSF in WKYhigh would still be larger than in WKYphys and SHRphys. Furthermore, the ratio of SF direction strains εSF in WKYhigh to WKYphys was 32.9, significantly exceeding the circumferential tissue strain ratio of 2.3. This result indicates that SF strain increases more than anticipated under elevated blood pressure conditions. In SHRphys, the εSF ratio to WKYphys was 2.9, slightly higher than the circumferential strain ratio of 1.0, suggesting that εSF has returned to baseline levels. Therefore, SF direction changes can sharply sense the increased strain in the SF direction under sudden blood pressure elevation.
In this study, we frequently observed poorly defined SFs, likely due to the use of unfixed specimens. To verify the reliability of our results with unfixed specimens, we conducted additional measurements on fixed specimens with formalin: WKY and SHR under physiological conditions, and WKY under hypertensive of intraluminal pressurization. Four ring specimens were prepared per mouse, and we selected three smooth muscle-rich layers, excluding innermost and outermost layers. In each layer, four clearly visible SFs were measured, yielding a total of 48 SFs per mouse. The results showed SF angles of αSF = 21° ± 1° in WKY at physiological pressure, αSF = 18° ± 1°at hypertensive pressure, and αSF = 20° ± 1° in SHR at physiological pressure (see Supplementary Fig. S4 online), consistent with the findings in Fig. 7a. These results confirm the reliability of SF angle measurements in unfixed specimens.
Intraluminal pressurization is the preferred mechanical stimulus to replicate the in vivo mechanical environment. However, this study stretched the aorta circumferentially, as measuring the SF direction under intraluminal pressurization was challenging based on preliminary studies. In our initial analysis, we captured the image stack of the aorta as a z-θ plane from outside the cylindrical aorta and reconstituted the r-θ plane. The low image resolution in the light axis (r-axis) made SF observation difficult in z-θ plane images. To directly observe the SF in the r-θ plane, we opted for circumferential stretching of a ring specimen instead of intraluminal pressurization. We investigated the effects of circumferential stretch versus intraluminal pressurization on strain and SF direction. In a previous study23, the average circumferential normal strain εθθ, radial normal strain εrr, and absolute shear strain |εrθ| under intraluminal pressurization from 80 to 120 mmHg were 5.3%, –3.0%, and 7.6% respectively. These results are comparable to this study’s data, albeit being reported from mouse models23. Furthermore, fixed aortas with formalin under physiological pressure intraluminal pressurization also showed comparable SF angles to this study’s data (See supplemental Fig. S4 online). Therefore, we concluded that the difference in the mechanical loading between intraluminal pressurization and circumferential stretch had negligible effects on the present results.
Blood pressure of SHRs tends to increase with age, reaching plateau around 15 weeks29. This suggests that older rats, compared to 10–14-week-old rats used in this study, may be a preferred condition. We tested 22–24-week-old SHRs and found that their blood pressure was comparable to that of the younger group (see Supplementary Fig. S5 online). Thus, we conclude that the use of 10–14-week-old rats does not alter the conclusions of our study.
This study found that not all SFs returned to zero strain direction after wall thickening. One reason might be insufficient time for SFs to recover their direction. We used 10–14-week-old rats, while 22–24-week-old SHR tended to have thicker aortic media, suggesting that the wall-thickening process might be ongoing.
We hypothesize that the wall-thickening is driven by force transmission through SFs, and the current findings partially support this. Strain in the SF direction increased under high-strain conditions, simulating initial hypertension in WKY, and returned to approximately zero levels in SHR. However, to fully confirm this hypothesis, further investigation is needed, such as nuclear deformation and changes in gene expression related to collagen production and cell proliferation. While these responses under SMC stretch have been previously confirmed11,12, future studies should elucidate their specific link to SF strain.
Conclusion
We hypothesized that SFs act as mechanosensors, leading to hypertension-caused wall thickening, and measured the SF directional strain in healthy rats at normal blood pressure, in an elevated circumferential stretch state simulating elevated blood pressure conditions, and in spontaneously hypertension rats, representing wall thickening conditions. The strain in the SF direction was approximately zero at normal blood pressure but increased in elevated circumferential stretch state. In hypertensive rats, the SF direction strain was reduced to near zero. These results support the hypothesis that SMCs-derived SFs detect increased stretch under hypertension and return to zero strain after wall-thickening, suggesting their potential role as mechanosensors for hypertension.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Wolinsky, H. Response of the rat aortic media to hypertension morphological and chemical studies. Circ. Res. 26, 507–522. https://doi.org/10.1161/01.res.26.4.507 (1970).
Matsumoto, T. & Hayashi, K. Stress and strain distribution in hypertensive and normotensive rat aorta considering residual strain. J. Biomech. Eng. 118, 62–73. https://doi.org/10.1115/1.2795947 (1996).
Matsumoto, T. & Hayashi, K. Mechanical and dimensional adaptation of rat aorta to hypertension. J. Biomech. Eng. 116, 278–283. https://doi.org/10.1115/1.2895731 (1994).
Marque, V., Kieffer, P., Atkinson, J. & Lartaud-Idjouadiene, I. Elastic properties and composition of the aortic wall in old spontaneously hypertensive rats. Hypertension 34, 415–422. https://doi.org/10.1161/01.HYP.34.3.415 (1999).
Owens, G. K., Rabinovitch, P. S. & Schwartz, S. M. Smooth muscle cell hypertrophy versus hyperplasia in hypertension. Proc. Natl. Acad. Sci. U. S. A. 78, 7759–7763. https://doi.org/10.1073/pnas.78.12.7759 (1981).
Deyl, Z., Jelínek, J., Macek, K., Chaldakov, G. & Vankov, V. N. Collagen and elastin synthesis in the aorta of spontaneously hypertensive rats. Blood Vessel. 24, 313–320. https://doi.org/10.1159/000158708 (1987).
Clark, J. M. & Glagov, S. Structural integration of the arterial wall. I. Relationships and attachments of medial smooth muscle cells in normally distended and hyperdistended aortas. Lab. Invest. 40, 587–602 (1979).
Shaw, A. & Xu, Q. Biomechanical stress-induced signaling in smooth muscle cells: an update. Curr. Vasc. Pharmacol. 1, 41–58. https://doi.org/10.2174/1570161033386745 (2003).
Hellstrand, P. & Albinsson, S. Stretch-dependent growth and differentiation in vascular smooth muscle: role of the actin cytoskeleton. Can. J. Physiol. Pharmacol. 83, 869–875. https://doi.org/10.1139/y05-061 (2005).
Shyu, K. G. Cellular and molecular effects of mechanical stretch on vascular cells and cardiac myocytes. Clin. Sci. (London) 116, 377–389. https://doi.org/10.1042/cs20080163 (2009).
Sumpio, B. E., Banes, A. J., Link, W. G. & Johnson, G. Jr. Enhanced collagen production by smooth muscle cells during repetitive mechanical stretching. Arch. Surg. 123, 1233–1236. https://doi.org/10.1001/archsurg.1988.01400340059010 (1988).
Richard, M. N., Deniset, J. F., Kneesh, A. L., Blackwood, D. & Pierce, G. N. Mechanical stretching stimulates smooth muscle cell growth, nuclear protein import, and nuclear pore expression through mitogen-activated protein kinase activation. J. Biol. Chem. 282, 23081–23088. https://doi.org/10.1074/jbc.M703602200 (2007).
Nagayama, K., Yahiro, Y. & Matsumoto, T. Stress fibers stabilize the position of intranuclear DNA through mechanical connection with the nucleus in vascular smooth muscle cells. FEBS Lett. 585, 3992–3997. https://doi.org/10.1016/j.febslet.2011.11.006 (2011).
Versaevel, M., Grevesse, T. & Gabriele, S. Spatial coordination between cell and nuclear shape within micropatterned endothelial cells. Nat. Commun. 3, 671. https://doi.org/10.1038/ncomms1668 (2012).
Huisinga, K. L., Brower-Toland, B. & Elgin, S. C. The contradictory definitions of heterochromatin: transcription and silencing. Chromosoma 115, 110–122. https://doi.org/10.1007/s00412-006-0052-x (2006).
Wang, J. H., Yang, G., Li, Z. & Shen, W. Fibroblast responses to cyclic mechanical stretching depend on cell orientation to the stretching direction. J. Biomech. 37, 573–576. https://doi.org/10.1016/j.jbiomech.2003.09.011 (2004).
Wang, J. H. C., Yang, G. & Li, Z. Controlling cell responses to cyclic mechanical stretching. Ann. Biomed. Eng. 33, 337–342. https://doi.org/10.1007/s10439-005-1736-8 (2005).
Nagayama, K. & Matsumoto, T. Estimation of single stress fiber stiffness in cultured aortic smooth muscle cells under relaxed and contracted states: Its relation to dynamic rearrangement of stress fibers. J. Biomech. 43, 1443–1449. https://doi.org/10.1016/j.jbiomech.2010.02.007 (2010).
Fan, Y., Wang, J., Kim, J., Maeda, E. & Matsumoto, T. Dependency of deformation of cell nucleus on stretch direction of tissue: Relation to anisotropic response of aortic media to hypertension. J. Mech. Behav. Biomed. Mater. 133, 105326. https://doi.org/10.1016/j.jmbbm.2022.105326 (2022).
Karimi, A. & Milewicz, D. M. Structure of the elastin-contractile units in the thoracic aorta and how genes that cause thoracic aortic aneurysms and dissections disrupt this structure. Can. J. Cardiol. 32, 26–34. https://doi.org/10.1016/j.cjca.2015.11.004 (2016).
Sugita, S., Mizuno, N., Ujihara, Y. & Nakamura, M. Stress fibers of the aortic smooth muscle cells in tissues do not align with the principal strain direction during intraluminal pressurization. Biomech. Model. Mechanobiol. 20, 1003–1011. https://doi.org/10.1007/s10237-021-01427-7 (2021).
Sugita, S. & Matsumoto, T. Multiphoton microscopy observations of 3D elastin and collagen fiber microstructure changes during pressurization in aortic media. Biomech. Model. Mechanobiol. 16, 763–773. https://doi.org/10.1007/s10237-016-0851-9 (2017).
Sugita, S., Kato, M., Wataru, F. & Nakamura, M. Three-dimensional analysis of the thoracic aorta microscopic deformation during intraluminal pressurization. Biomech. Model. Mechanobiol. 19, 147–157. https://doi.org/10.1007/s10237-019-01201-w (2020).
Sugita, S. & Matsumoto, T. Yielding phenomena of aortic wall and intramural collagen fiber alignment: possible link to rupture mechanism of aortic aneurysms. J. Biomech. Sci. Eng. 8, 104–113. https://doi.org/10.1186/1475-925X-12-3 (2013).
Jayyosi, C., Fargier, G., Coret, M. & Bruyère-Garnier, K. Photobleaching as a tool to measure the local strain field in fibrous membranes of connective tissues. Acta Biomater. 10, 2591–2601. https://doi.org/10.1016/j.actbio.2014.02.031 (2014).
Takemasa, T., Yamaguchi, T., Yamamoto, Y., Sugimoto, K. & Yamashita, K. Oblique alignment of stress fibers in cells reduces the mechanical stress in cyclically deforming fields. Eur. J. Cell Biol. 77, 91–99. https://doi.org/10.1016/S0171-9335(98)80076-9 (1998).
Fukuda, S., Tsuchikura, S. & Iida, H. Age-related changes in blood pressure, hematological values, concentrations of serum biochemical constituents and weights of organs in the SHR/Izm SHRSP/Izm and WKY/Izm. Exp. Anim. 53, 67–72. https://doi.org/10.1538/expanim.53.67 (2004).
van Gorp, A. W. et al. In spontaneously hypertensive rats alterations in aortic wall properties precede development of hypertension. Am. J. Physiol. Heart Circ. Physiol. 278, H1241-1247. https://doi.org/10.1152/ajpheart.2000.278.4.H1241 (2000).
Hom, S. et al. Comparative changes in the blood-brain barrier and cerebral infarction of SHR and WKY rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 292, R1881–R1892. https://doi.org/10.1152/ajpregu.00761.2005 (2007).
Acknowledgements
This work was partly supported by AMED Grant Number JP20gm0810005 and JSPS KAKENHI Grant Number 21H04955a.
Funding
Japan Society for the Promotion of Science, 21H04955a, Japan Agency for Medical Research and Development, JP20gm0810005.
Author information
Authors and Affiliations
Contributions
S.S. wrote the original draft of manuscript and designed the study. R.K. mainly performed experiments and analyses. S.S., Y.U., and M.N. contributed interpretation of data and organized paper structure. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Video 1.
Supplementary Video 2.
Supplementary Video 3.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sugita, S., Kawai, R., Ujihara, Y. et al. Stress fiber strain is zero in normal aortic smooth muscle, elevated in hypertensive stretch, and minimal in wall thickening rats. Sci Rep 14, 29731 (2024). https://doi.org/10.1038/s41598-024-81229-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81229-w