Abstract
To evaluate the association between a first-trimester subchorionic hematoma (SCH) and pregnancy loss before 20 weeks of gestation in singleton pregnancies. We conducted a retrospective cohort study of singleton pregnancies from January to December 2021. All patients had routine first-trimester ultrasound scans and were followed up for pregnancy outcomes. We compared pregnancy loss rates before 20 weeks in women with and without SCH and analyzed risk factors using logistic regression. Out of 1,144 singleton pregnancies, 559 (48.9%) had SCH. Women with SCH had higher rates of vaginal bleeding (38.1 vs. 23.2%, P < 0.001). SCH was independently associated with miscarriage before 20 weeks (adjusted OR 1.94, 95% CI 1.19–3.15). Earlier SCH diagnosis increased miscarriage risk (adjusted OR 2.71 for diagnosis before 7 weeks, 95% CI 1.45–5.07). SCH size was not linked to pregnancy loss, but “large” SCH increased placental abruption risk (adjusted OR 5.03, 95% CI 1.20–21.11). Dydrogesterone use appeared protective against miscarriage (adjusted OR 0.28, 95% CI 0.15–0.52). First-trimester SCH is associated with an increased risk of miscarriage before 20 weeks. Large SCHs increase the risk of placental abruption, while dydrogesterone use may reduce miscarriage risk.
Similar content being viewed by others
Introduction
Subchorionic hematoma (SCH) is defined as the accumulation of fluid in the uterine cavity, and it is considered to be result from subchorionic bleeding, which is caused by the separation of the trophoblast from the uterine wall1. It was first described by Mantoni and Pedersen in 19812.The reported incidence varies widely, from as low as 0.46% to as high as 48%3,4. As a result of remarkable advancements in ultrasound resolution, the diagnosis of SCH is becoming more prevalent.
Previous studies have reported conflicting results, the clinical significance of SCH has been questioned. A large systematic review found that subchorionic hematomas were associated with an increased risk of early and late pregnancy loss, abruption, and preterm premature rupture of membranes5, Yet other studies have found no increased rate of pregnancy loss6,7. There are many reports on the relationship between the size of the SCH and pregnancy outcomes8, but different studies have come to different conclusions. Abu-Yousef et al. reported the poor outcomes of pregnancies with a SCH correlated well with both the absolute and relative hematoma size9, while in most recent studies, authors failed to demonstrate this association6,10,11. The discrepancy in these results might be related to different patient populations, and the route and resolution of ultrasonography used, study design, range of gestational ages, and lack of a standard definition.
Furthermore, many studies did not include a general obstetric population, focusing instead on high-risk groups such as patients who underwent in vitro fertilization (IVF)12, experienced recurrent pregnancy losses13, or had threatened miscarriages14. In addition, several studies15,16 have overlooked clinical factors like previous miscarriages, premature births, and IVF use. Consequently, the association between SCH and pregnancy loss remains unclear. Additionally, most similar studies have not examined the effect of medication treatment on pregnancy outcomes.
This study aims to investigate the relationship between first-trimester SCH and pregnancy outcomes, particularly pregnancy loss before 20 weeks, in a general obstetric population, by using detailed clinical data and analyzing the effects of hematoma size and medication treatment.
Methods
Study population
This retrospective study involved women with singleton pregnancies who had first-trimester ultrasounds at Yuyao People’s Hospital from January to December 2021. This study was a retrospective analysis using data from electronic medical records, where obtaining informed consent from each patient was not feasible. According to the Declaration of Helsinki, if obtaining consent is impossible or impractical, research can proceed only after review and approval by a research ethics committee. In this study, informed consent was waived by the Ethics Committee of Yuyao People’s Hospital (YS2023-09-010) because it involves a retrospective review of existing data from standard patient care, and no patient information is disclosed. We reviewed the ultrasound examination performed between 5 0/7 and 13 6/7 weeks of gestation for each patient presented for prenatal care at our hospital. All women included in this study underwent at least two ultrasounds before 14 weeks of gestation, and those who did not have their first ultrasound before 7 weeks being excluded. Gestational age was determined based on the last menstrual period or first-trimester ultrasound scan result according to the standard guideline17. We excluded pregnancies with multiple gestations, a vanishing twin, pregnancies with fetal abnormalities, elective pregnancy termination, or a fetal heart rate less than 100 beats per minute. Exclusion criteria also included uterine anomaly (unicornuate, didelphys, bicornuate and septate uteri, intrauterine adhesions and submucosal myomas), chronic hypertension, pre-pregnancy diabetes, autoimmune diseases, and other identified medical conditions that could contribute to miscarriage or adverse pregnancy outcomes in the second and third trimesters.
Data collection
We reviewed each ultrasound report for the presence of a subchorionic hematoma, and all cases where it was detectable by ultrasound were included in the SCH group. The size of any subchorionic hematomas and the size of gestational sac were all routinely noted on the ultrasound report (measured by averaging the antero-posterior, longitudinal, and height dimensions). According the ratio of average SCH diameter to average gestational sac diameter, SCH was stratified into three sizes: SCH was stratified into three sizes: a small SCH comprising < 5% of the gestational sac, a medium SCH comprising 5–25% of the gestational sac, and a large SCH comprising > 25% of the gestational sac10. We also reviewed electronic medical record for each woman to obtain demographic, baseline clinical information, and medical record data including the gestational age at first detection of SCH and the gestational age at SCH peak (largest diameter recorded during pregnancy), the presence or absence of vaginal bleeding, use of dydrogesterone, as well as pregnancy outcomes.
Outcomes of interest
The specific outcomes examined were miscarriage (loss before 20 weeks), stillbirth (loss after 20 weeks), and live birth. Our primary focus was pregnancy loss before 20 weeks. In the SCH subgroup, we also assessed whether SCH size was linked to pregnancy loss and late outcomes, such as placental abruption, preeclampsia, and fetal growth restricted.
Statistical analysis
Data management and statistical analysis were performed using SPSS 26.0 statistical package (SPSS, Chicago, IL, USA) and R version 4.0.3. A significance level of 5% was selected. We compared baseline characteristics and pregnancy outcome between the women with and without subchorionic hematomas using Student t test, ANOVA, the Wilcoxon rank-sum test, or Chi-square or Fisher’s exact test, as appropriate for the data type.
The associations between SCH and pregnancy loss were estimated using logistic regression analyses. Initially, unadjusted analyses estimated crude odds ratios and 95% confidence intervals (CIs). Multivariable logistic regression analysis was used to adjust for possible confounding factors including vaginal bleeding and use of dydrogesterone.
Results
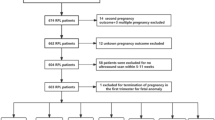
A total of 1,385 women with singleton pregnancies sought prenatal care before 7 weeks of gestation during the study period. Of these, 1,144 were ultimately included in the analysis. Among these women, 559 had a subchorionic hematoma and 585 did not (Fig. 1).
Table 1 presents the baseline characteristics of the patients with and without subchorionic hematoma. There were no significant differences in baseline factors such as maternal age, primiparity, body mass index, use of IVF, presence of intramural leiomyomas, history of miscarriage, cesarean delivery, or preterm delivery. Univariable analysis showed that SCH was associated with a higher rate of miscarriage before 20 weeks of gestation (9.8 vs. 5.8%, p = 0.011). However, there was no significant difference in stillbirth rates between the two groups (Table 2).
Table 3 displays the adjusted risk of miscarriage before 20 weeks of gestation. Clinical characteristics of the miscarriage and live birth groups are shown in Table S1. In the miscarriage group (< 20 weeks), cases of SCH (61.8 vs. 47.9%, p = 0.012) and vaginal bleeding (51.7 vs. 28.6%, p < 0.001) were significantly higher. Although there was no difference in dydrogesterone use between the groups, its potential impact on pregnancy outcomes led to its inclusion as a confounding factor in the multivariate analysis. After adjusting for vaginal bleeding and dydrogesterone use, the association between SCH and miscarriage before 20 weeks remained significant (adjusted odds ratio 1.94, 95% CI 1.19–3.15).
In patients with SCH, there was no significant difference in age or basal BMI between the miscarriage before 20 weeks group and the live birth group. The size of SCH was also not related to pregnancy loss before 20 weeks of gestation. However, compared with the live birth group, the miscarriage group had a higher frequency (54.5 vs 36.5%, p = 0.009) of vaginal bleeding in first-trimester. Compared with the live birth group, the patients who miscarried before 20 gestation weeks were diagnosed with SCH earlier and the gestational week at which SCH reached its peak occurred earlier as well (Table4). Besides, we found that the use of dydrogesterone in the live birth group was significantly more common than that who miscarried before 20 gestation weeks (77.7 vs 56.4%, p < 0.001).
On univariable analysis, vaginal bleeding, gestational age at SCH peak, and gestational age at diagnosis were associated with an increased risk of pregnancy loss, while the use of dydrogesterone is a protective factor for miscarriage before 20 weeks of gestation (Table4). As shown in Table 5, gestational age at diagnosis before 7 weeks (adjusted odds ratio 2.71, 95% CI 1.45–5.07) and vaginal bleeding (adjusted odds ratio 2.57, 95% CI 1.42–4.66) were independently associated with miscarriage before 20 weeks of gestation, the use of dydrogesterone seems to be a protective factor for miscarriage before 20 weeks of gestation (adjusted odds ratio 0.28, 95% CI 0.15–0.52). Furthermore, we found the risk of miscarriage before 20 weeks of gestation is higher when the peak of SCH appears before 7 weeks (adjusted odds ratio 3.39, 95% CI 1.87–6.13).
Although there was no correlation between the size of SCH and pregnancy loss in our data, when we compare the clinical characteristics of patients with different grades of SCH, we find that the size of SCH is related to basal BMI, prior miscarriages/abortions and vaginal bleeding. Patients with large SCH had a lower basal BMI, whereas those with small SCH had a higher incidence of prior miscarriages/abortions and vaginal bleeding. We found the peak in large SCH appeared later, and the proportion that SCH lasted until the second trimester also increased significantly (Table6). Table 7 indicates that there is no significant difference in pregnancy loss across the various grades of SCH groups. Our data showed that the pregnancy outcome after 20 weeks related to the size of SCH was only placental abruption (1.6 vs 0.7 vs 5.4%, p = 0.012), and the other pregnancy outcomes had no significant correlation (Table8). On univariable analysis, the “large” size of SCH was associated with an increased risk of placenta abruption. It is common knowledge that preeclampsia is associated with placental abruption when after adjusting for preeclampsia, this association was still significant. Compared with “small” and “medium”, “large” size of SCH has a higher risk of placental abruption (adjusted odds ratio 5.03, 95% CI 1.20–21.11). The “large” size of SCH was independently associated with an increased risk of placenta abruption.
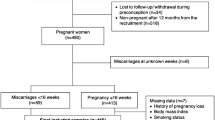
In the correlation between prior miscarriages/abortions and SCH size, additional separate analysis was carried out. The proportion of SCH with an average diameter greater than 10 mm was significantly higher in pregnant women with fewer than 3 prior miscarriages/abortions compared to those with 3 or more prior miscarriages/abortions (19.5 vs 2.4%, p < 0.006). We describe the relationship between the average diameter of SCH and the number of prior miscarriages/abortions by scatter plot (Fig. 2). As can be seen from the scatter plot, the number of prior miscarriages/abortions increases, the frequency of SCH with a larger average diameter decreases gradually.
Discussion
The presence of SCH is common in first-trimester ultrasounds and can be concerning for patients. Prior studies have reported inconsistent results, and we aimed to explore whether SCH could serve as an early marker for adverse pregnancy outcomes. To address uncertainty about the impact of SCH size, we included all detectable hematomas, which led to a higher proportion of SCH cases in our study. We found that SCH in singleton pregnancies is independently associated with miscarriage before 20 weeks. The administration of dydrogesterone appeared to have a protective effect against pregnancy loss, though we found no correlation between SCH size and miscarriage. Most SCH cases resolved by the second trimester in patients who did not miscarry.
Although several studies have identified IVF as a risk factor for SCH18,19, we did not reach the same conclusion in our study. It should be noted that all patients who used IVF were referred from other hospitals, so the earliest ultrasound examination data might not be available, potentially affecting the reliability of our results. Similar to most previous studies8, we found a strong correlation between SCH and vaginal bleeding, which elevated the miscarriage risk. Robert H. et al.10 also found that SCH in patients with vaginal bleeding further increases the risk of miscarriage beyond bleeding alone.
Many existing studies support that earlier onset of SCH is particularly dangerous to maintenance of pregnancy1,16. This is also supported by our data, which showed a significant correlation between earlier diagnosed SCH and miscarriage before 20 weeks of gestation. Cytogenetic evaluations show that over half of early miscarriages are due to chromosomal abnormalities20,21, and while we excluded pregnancies with fetal heart rates below 100 bpm (screening out some chromosomal abnormalities)22. However, it remains unclear whether women with chromosomal abnormalities are more prone to developing SCH.
Although the exact cause of SCH is unclear, it is thought to result from ruptured blood vessels during abnormal placental implantation23. This abnormal development may disrupt trophoblast invasion, a process critical for pregnancy success24. One retrospective cohort study reported that the presence of a SCH in patients undergoing or having undergone chorionic villus sampling or amniocentesis does not appear to be significant with respect to pregnancy outcome10. Therefore, inferring that SCH is a sign of an underlying placental problem is reasonable, which may be associated with an adverse prognosis.
In patients with SCH, the utilization rate of dydrogesterone in patients with miscarriage before 20 weeks of gestation was significantly lower than that in patients with live birth. There are no clear guidelines for the treatment of SCH, and studies have shown that dydrogesterone has an immunomodulatory regulatory effect, which can prevent abortion in pregnancies with subchorionic hematoma25. A significantly increased T-helper (Th)1 cytokine expression may be the underlying immune etiology for reproductive failure26. The mechanism behind SCH may associated with Th1 cells, while the protective mechanism against intravascular coagulation and amputation of decidual vessels is under Th2 control. Progesterone is effective in preventing Th1 embryotoxic cytokinemediated pregnancy loss27. However, the variability in dosage and duration of dydrogesterone use in our retrospective study limits the interpretation of these findings.
The effect of SCH size on rates of pregnancy loss or late pregnancy outcomes also varies by study. Some studies believe that the size of hematoma has no concern with pregnancy outcome6,14,28, while others show increased risks with larger hematomas9,16,29. These various conclusions stem from the differences in the population, the measurement methods of SCH and whether the participants have clinical symptoms or not in different studies. Our data suggest that the size of SCH in singleton pregnancies is not associated with pregnancy loss before 20 weeks of gestation. However, consistent with some previous studies10,30, “larger” SCH is associated with an increased risk of placental abruption. It has been suggested that a hematoma may potentially have the potential to disrupt normal placentation, or that the hematoma itself may result from impaired placentation. There are two factors likely to have an effect on the size of SCH: the rate of drainage of the subchorionic hemorrhage through the cervix and the rate of bleeding (accumulation). Our data shows that vaginal bleeding was more common in the small-sized SCH group compared to the medium and large-sized groups (48.3 vs 34.4 vs 36.3%, p = 0.017), supporting this point to some extent. On the other hand, our research indicates that the likelihood of large SCH significantly decreases with an increase in the number of prior miscarriages or abortions. The average diameter of SCH reflects the absolute value of hematoma size. Therefore, we conjecture that the size of SCH is not only affected by vaginal bleeding, but also may be related to the thin endometrium, which may result from post-abortion/miscarriage curettage leading to defective endometrial healing and vascularization31. The damaged endometrium result from post-abortion/miscarriage curettage then cannot be properly repaired and may lead to thin endometrium. The basic cause is the damage of the basal layer of endometrium, and then endometrial fibrosis causing reduced blood perfusion32,33. When blood vessels rupture during abnormal placenta implantation, patients who experience more abortions may have less bleeding. Thus, we suspect that SCH size may not directly indicate the extent of abnormal trophoblast invasion.
The strengths of our study include a large sample size, comprehensive clinical data, and an analysis of the impact of medication treatment on pregnancy loss in patients with SCH. This represents an improvement from previous studies that focused solely on specific subsets of the obstetric population, such as those undergoing fertility treatments.
Our study has several limitations. Firstly, the data from one hospital, rather than a more heterogeneous population. Secondly, due to the limited ultrasound images available for retrospective data, calculating the size of a hematoma may not be accurate enough. Lastly, limited by retrospective study, we failed to get more detailed information about the dosage and duration of medication treatment. In the future, we aim to conduct multi-center prospective studies to further validate and strengthen the current research findings.
Conclusion
In conclusion, the presence of a first-trimester SCH in singleton pregnancies is independently associated with miscarriage before 20 weeks of gestation. We did not find any correlation between SCH size and pregnancy loss. However, “large” SCH increases the risk of placental abruption. The use of dydrogesterone in patients with SCH may serve as a protective factor against pregnancy loss before 20 weeks. These results will be useful for counseling women with SCH.
Data availability
The dataset supporting the conclusions of this article is available in the Science Data Bank ository, https://www.scidb.cn/en/s/MNVjie.
Abbreviations
- BMI:
-
Body mass index
- FGR:
-
Fetal growth restricted
- GDM:
-
Gestational diabetes mellitus
- CI:
-
Confidence interval
- IVF:
-
In vitro fertilization
- OR:
-
Odds ratio
- PROM:
-
Premature rupture of membranes
- SCH:
-
Subchorionic hematoma
- Th:
-
T-helper
References
Maso, G. et al. First-trimester intrauterine hematoma and outcome of pregnancy. Obstet. Gynecol. 105, 339–344. https://doi.org/10.1097/01.AOG.0000152000.71369.bd (2005).
Mantoni, M. & Pedersen, J. F. Intrauterine haematoma. An ultrasonic study of threatened abortion. Br. J. Obstet. Gynaecol. 88, 47–51. https://doi.org/10.1111/j.1471-0528.1981.tb00936.x (1981).
Khan, R. I. et al. Association of subchorionic hematoma with preterm labour in patients with threatened abortion. J. Ayub. Med. Coll. Abbottabad 33, 451–455 (2021).
Seki, H., Kuromaki, K., Takeda, S. & Kinoshita, K. Persistent subchorionic hematoma with clinical symptoms until delivery. Int. J. Gynaecol. Obstet. 63, 123–128. https://doi.org/10.1016/s0020-7292(98)00153-2 (1998).
Tuuli, M. G., Norman, S. M., Odibo, A. O., Macones, G. A. & Cahill, A. G. Perinatal outcomes in women with subchorionic hematoma: a systematic review and meta-analysis. Obstet. Gynecol. 117, 1205–1212. https://doi.org/10.1097/AOG.0b013e31821568de (2011).
Naert, M. N., Khadraoui, H., Muniz Rodriguez, A., Naqvi, M. & Fox, N. S. Association between first-trimester subchorionic hematomas and pregnancy loss in singleton pregnancies. Obstet. Gynecol. 134, 276–281. https://doi.org/10.1097/aog.0000000000003360 (2019).
Inman, E. R. et al. Outcomes of subchorionic hematoma-affected pregnancies in the infertile population. Int. J. Gynaecol. Obstet. 159, 743–750. https://doi.org/10.1002/ijgo.14162 (2022).
Xiang, L., Wei, Z. & Cao, Y. Symptoms of an intrauterine atoma associated with pregnancy complications: a systematic review. PLoS One 9, e111676. https://doi.org/10.1371/journal.pone.0111676 (2014).
Abu-Yousef, M. M., Bleicher, J. J., Williamson, R. A. & Weiner, C. P. Subchorionic hemorrhage: sonographic diagnosis and clinical significance. AJR Am. J. Roentgenol. 149, 737–740. https://doi.org/10.2214/ajr.149.4.737 (1987).
Ball, R. H., Ade, C. M., Schoenborn, J. A. & Crane, J. P. The clinical significance of ultransonographically detected subchorionic hemorrhages. Am. J. Obstet. Gynecol. 174, 996–1002. https://doi.org/10.1016/s0002-9378(96)70339-3 (1996).
Ben-Haroush, A., Yogev, Y., Mashiach, R. & Meizner, I. Pregnancy outcome of threatened abortion with subchorionic hematoma: possible benefit of bed-rest?. Isr. Med. Assoc. J. 5, 422–424 (2003).
Yue, M., Ma, L., Cao, Y. & Zhai, J. Application of a nomogram for predicting the risk of subchorionic hematoma in early pregnancy with in vitro fertilization-embryo transfer/frozen embryo transfer. Front. Endocrinol. (Lausanne) 12, 631097. https://doi.org/10.3389/fendo.2021.631097 (2021).
Tower, C. L. & Regan, L. Intrauterine haematomas in a recurrent miscarriage population. Hum. Reprod. 16, 2005–2007. https://doi.org/10.1093/humrep/16.9.2005 (2001).
Naz, S., Irfan, S., Naru, T. & Malik, A. Subchorionic hematoma and pregnancy outcomes in patients with threatened miscarriage. Pak. J. Med. Sci. 38, 511–516. https://doi.org/10.12669/pjms.38.3.4283 (2022).
Gu, C. et al. The effects of first-trimester subchorionic hematoma on pregnancy outcomes: a retrospective cohort study. Arch. Gynecol. Obstet. 308, 1159–1164. https://doi.org/10.1007/s00404-022-06776-x (2023).
Heller, H. T. et al. Subchorionic hematoma: Correlation of grading techniques with first-trimester pregnancy outcome. J. Ultrasound Med. 37, 1725–1732. https://doi.org/10.1002/jum.14524 (2018).
Christian, M. P. et al.Committee opinion no 700: Methods for estimating the due date. Obstet. Gynecol. 129, e150-e154. https://doi.org/10.1097/aog.0000000000002046 (2017).
Asato, K. et al. Subchorionic hematoma occurs more frequently in in vitro fertilization pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 181, 41–44. https://doi.org/10.1016/j.ejogrb.2014.07.014 (2014).
Frates, M. C., Benson, C. B. & Doubilet, P. M. Pregnancy outcome after a first trimester sonogram demonstrating fetal cardiac activity. J. Ultrasound Med. 12, 383–386. https://doi.org/10.7863/jum.1993.12.7.383 (1993).
Popescu, F., Jaslow, C. R. & Kutteh, W. H. Recurrent pregnancy loss evaluation combined with 24-chromosome microarray of miscarriage tissue provides a probable or definite cause of pregnancy loss in over 90% of patients. Hum. Reprod. 33, 579–587. https://doi.org/10.1093/humrep/dey021 (2018).
Simpson, J. L. Genes, chromosomes, and reproductive failure. Fertil. Steril. 33, 107–116. https://doi.org/10.1016/s0015-0282(16)44528-0 (1980).
Oztekin, D., Oztekin, O., Aydal, F. I., Tinar, S. & Adibelli, Z. H. Embryonic heart rate as a prognostic factor for chromosomal abnormalities. J. Ultrasound Med. 28, 609–614. https://doi.org/10.7863/jum.2009.28.5.609 (2009).
Kurjak, A. et al. Subchorionic hematomas in early pregnancy: clinical outcome and blood flow patterns. J. Matern Fetal Med. 5, 41–44. https://doi.org/10.1002/(sici)1520-6661(199601/02)5:1%3c41::Aid-mfm10%3e3.0.Co;2-q (1996).
Salafia, C. M. et al. Histologic evidence of old intrauterine bleeding is more frequent in prematurity. Am. J. Obstet. Gynecol. 173, 1065–1070. https://doi.org/10.1016/0002-9378(95)91327-0 (1995).
Pelinescu-Onciul, D. Subchorionic hemorrhage treatment with dydrogesterone. Gynecol. Endocrinol. 23 (1), 77–81. https://doi.org/10.1080/09513590701584741 (2007).
Makhseed, M. et al. Circulating cytokines and CD30 in normal human pregnancy and recurrent spontaneous abortions. Hum. Reprod. 15, 2011–2017. https://doi.org/10.1093/humrep/15.9.2011 (2000).
Choi, B. C., Polgar, K., Xiao, L. & Hill, J. A. Progesterone inhibits in-vitro embryotoxic Th1 cytokine production to trophoblast in women with recurrent pregnancy loss. Hum. Reprod. 15 (1), 46–59. https://doi.org/10.1093/humrep/15.suppl_1.46 (2000).
Naqvi, M. et al. Subchorionic hematomas and adverse pregnancy outcomes among twin pregnancies. Am. J. Perinatol. 38, 779–783. https://doi.org/10.1055/s-0039-3401852 (2021).
Karaçor, T. et al. The effect of vaginal bleeding and non-spesific pelvic pain on pregnancy outcomes in subchorionic hematomas cases. Ginekol. Pol. 90, 656–661. https://doi.org/10.5603/gp.2019.0111 (2019).
Nagy, S., Bush, M., Stone, J., Lapinski, R. H. & Gardó, S. Clinical significance of subchorionic and retroplacental hematomas detected in the first trimester of pregnancy. Obstet. Gynecol. 102, 94–100. https://doi.org/10.1016/s0029-7844(03)00403-4 (2003).
Santamaria, X., Isaacson, K. & Simón, C. Asherman’s syndrome: it may not be all our fault. Hum. Reprod. 33, 1374–1380. https://doi.org/10.1093/humrep/dey232 (2018).
Liu, T., He, B. & Xu, X. Repairing and regenerating injured endometrium methods. Reprod. Sci. 30, 1724–1736. https://doi.org/10.1007/s43032-022-01108-5 (2023).
Lebovitz, O. & Orvieto, R. Treating patients with “thin” endometrium—An ongoing challenge. Gynecol. Endocrinol. 30, 409–414. https://doi.org/10.3109/09513590.2014.906571 (2014).
Funding
This work was supported by Project for Zhejiang Medical Technology and Hygiene Program (2021KY1073).
Author information
Authors and Affiliations
Contributions
Ying Lou conceptualized the study, collected data, wrote the initial paper, analyzed and interpreted the data, revised the paper according to other authors’ comments. Jinting Ma made critical revisions of the manuscript for important intellectual content and contributed to the study concept, design and implementation and acquired funding. GuiliChen assisted in data collection, reviewed and interpreted the data. Lanying Wang and Xiaoqing Zhao assisted in data collection and statistical analysis of data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
Ethical approval of this study was granted by the Ethics Committee of Yuyao People’s Hospital (YS2023-09-010). Informed consent was waived by the Ethics Committee because this is a retrospective review of existing data included in the standard care of patients, and no patient information was published herein.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lou, Y., Chen, G., Wang, L. et al. Association between first-trimester subchorionic hematoma and pregnancy loss before 20 weeks of gestation in singleton pregnancies. Sci Rep 14, 30034 (2024). https://doi.org/10.1038/s41598-024-81759-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-81759-3