Abstract
Several studies have shown that the monocyte count to high-density lipoprotein cholesterol ratio (MHR) serves as a predictive marker for in-stent restenosis (ISR) of bare-metal stents (BMSs). However, the ability of the MHR to predict ISR in patients with drug-eluting stents (DESs) remains uncertain. This study aimed to investigate the predictive value of the MHR for ISR in patients with unstable angina pectoris who have undergone primary DES implantation. A total of 474 consecutive patients with unstable angina pectoris who underwent successful DES-based percutaneous coronary intervention (PCI) from 01-12-2014 to 01-12-2022 were enrolled in the study. Patients were divided into the ISR group and the non-ISR group on the basis of the follow-up results of coronary angiography. The demographic and clinical characteristics of the patients were documented. The MHR was calculated via the following formula: \({{Monocyte \; count[/\mu l]} \mathord{\left/ {\vphantom {{Monocyte \; count[/\mu l]} {HDL}}} \right. \kern-0pt} {HDL}}[mg/dL]\). Multivariate logistic regression models were developed to evaluate the predictive value of the MHR for DES-ISR. The baseline MHR was notably greater in the ISR group than in the non-ISR group (P < 0.001). After adjusting for confounding factors, the MHR emerged as an independent predictor of ISR (OR = 1.244; 95%CI 1.171–1.321). Receiver operating characteristic (ROC) curve analysis revealed that MHR for predicting ISR had an AUC of 0.752 (95% CI 0.708–0.796). For a MHR > 7.32, the sensitivity was estimated to be 59.8% (95% CI 47.2-66.5%) and the specificity was 81.2% (95% CI 71.2-86.4%). Including the MHR in the predictive model for ISR improved the area under the curve (0.698 vs. 0.782, P < 0.001), categorical net reclassification improvement (0.703; 95%CI 0.536–0.871), and integrated discrimination improvement (0.121; 95%CI 0.092–0.151). The MHR can be used to predict DES-ISR in patients with unstable angina pectoris, indicating that the MHR may serve as a valuable marker for risk stratification and prognosis in individuals undergoing DES implantation.
Similar content being viewed by others
Introduction
With the rising number of implanted drug-eluting stents, in-stent restenosis (ISR) has gradually emerged as a challenge in the treatment of coronary artery stenosis, with occurrence rates ranging from 3 to 20% 1,2,3. The risk of adverse clinical outcomes, including recurrent angina, myocardial infarction, and even cardiovascular death, is elevated, necessitating target lesion revascularization through methods such as repeated percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). ISR is a multifaceted phenomenon influenced by a variety of factors, including stent factors, lesion factors and patient factors. Inflammation plays a pivotal role in the pathogenesis of ISR. The implantation of a stent disrupts the endothelial layer, triggering a complex inflammatory response. ISR may occur at any time after stent implantation, therefor at the very moment of stent implantation, therapeutic interventions aimed at preventing ISR need to be initiated. Patient risk stratification serves as the foundation for preventive treatment. To establish a more refined risk stratification, multiple inflammatory biomarkers have been utilized to investigate their correlation with ISR in addition to traditional risk factors, such as the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and C-reactive protein. The MHR, a novel inflammatory biomarkers, was reported for the first time to be associated with cardiovascular events in individuals with chronic kidney disease4. Similarly, previous studies have identified the MHR as a newly emerging prognostic marker for cardiovascular events5,6,7,8. Several investigations have evaluated the prognostic value of the MHR in predicting the BMS-ISR9,10,11. A study explored the relationship between the MHR and DES-ISR in patients with non-ST segment elevation acute coronary syndrome (NSTE-ACS)12. However, for a broader cohort of patients diagnosed with unstable angina, the existence of a correlation between the MHR and ISR remains an open question that warrants further investigation.
Methods
Study population
A total of 2912 patients with unstable angina underwent successful primary DES implantation at Tianjin Chest Hospital from 01-12-2014 to 01-12-2022. Among them, 622 patients underwent follow-up coronary angiography due to chest pain with or without acute elevations in cardiac troponin concentrations, or positive results of coronary computed tomography angiography. Patients with a history of coronary artery bypass graft (CABG), severe liver disease, renal dysfunction (eGFR < 30 mL/min/1.73 m2), active infections, autoimmune or chronic connective tissue diseases, heart failure, thyroid disorders, malignancies, major surgeries, trauma, alcohol abuse, or any hematological conditions were excluded from the study. Figure 1 shows the study flow chart. Our research was approved by the Ethics Committee of Chest Hospital, Tianjin University, and it strictly adhered to the principles outlined in the Declaration of Helsinki. Owing to the retrospective nature of this study, informed consent was not needed.
Intervention and management
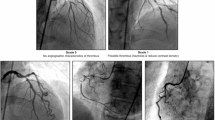
Coronary interventions and periprocedural management were conducted in accordance with the current guidelines established by our medical center13. All patients received dual antiplatelet therapy prior to the intervention, which included the oral administration of aspirin (loading dose: 300 mg; maintenance dose: 100 mg/day) and clopidogrel (loading dose: 300 mg; maintenance dose: 75 mg/day) or ticagrelor (loading dose: 180 mg; maintenance dose: 90 mg twice daily). During the intervention, anticoagulation was administered to maintain an activated clotting time > 250 s via unfractionated heparin (70–100 IU/kg, with an additional bolus if necessary). Judkin’s technique was utilized during coronary angiography, and the images were digitally captured for later quantitative assessment. The operator was allowed to choose the specific type of second-generation drug-eluting stent (DES), the size of the stent, and whether to use glycoprotein IIb/IIIa receptor blockers. Following the intervention, patients were also provided with secondary prevention strategies as recommended by the latest guidelines.
Data collection and definitions
Trained physicians, who were blinded to the study’s objectives, collected clinical data, including sex, age, smoking status, hypertension, diabetes mellitus, left ventricular ejection fraction (LVEF), and medications at discharge, from the patients’ medical records. Peripheral venous blood samples were collected and analysed before the stents implatation. The levels of fasting blood glucose (FBG), total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), serum creatinine, serum uric acid, and high-sensitivity C-reactive protein (hs-CRP) were measured, along with white blood cell (WBC) counts. The MHR was determined via the following formula: \({{Monocyte \; count[/\mu l]} \mathord{\left/ {\vphantom {{Monocyte \; count[/\mu l]} {HDL}}} \right. \kern-0pt} {HDL}}[mg/dL]\). Unstable angina pectoris is defined as myocardial ischaemia at rest or on minimal exertion in the absence of acute cardiomyocyte injury/necrosis. It is characterized by specific clinical findings of prolonged (> 20 min) angina at rest; newonset of severe angina; angina that is increasing in frequency, longer in duration, or lower in threshold; or angina that occurs after a recent episode of myocardial infarction14. Hypertension was defined as having a systolic blood pressure of ≥ 140 mmHg and/or a diastolic blood pressure of ≥ 90 mmHg, on the basis of at least three office blood pressure measurements taken on different days or while receiving antihypertensive therapy. Diabetes mellitus was defined as a fasting blood glucose level of 126 mg/dL or higher or treatment with antidiabetic medications. Smoking status was classified as either current or former smoking. ISR was defined as a diameter stenosis of ≥ 50% at the segment within the stent or involving its 5-mm edges confirmed by quantitative coronary angography. Notably, quantitative coronary angography was conducted by two independent and experienced cardiologists who were blinded to the patients’ information. Any discrepancies encountered in the identification of ISR were resolved through consultation with a senior researcher.
Statistical analysis
The data were tested for a normal distribution via the Kolmogorov‒Smirnov test. Continuous variables are presented as either the mean with standard deviation or the median with interquartile range, depending on the normality of the data. Categorical variables are expressed as percentages (%). Normally distributed data were analysed via an independent t test, whereas nonnormally distributed data were analysed via the Mann‒Whitney U test. The chi-square test was used for categorical variables. Univariate logistic regression was utilized to investigate the correlation between each variable and ISR. Variables were included in the multivariate logistic regression analysis if they presented P values < 0.1 in univariate analysis or were clinically relevant to ISR. The Box–Tidwell test was used to evaluate the assumption of linearity in the logit for the continuous variable. To assess multicollinearity, we employed the Pearson correlation coefficient statistic and checked the variance inflation factor in a multiple regression model with the same dependent and independent variables. The stepwise regression method was employed to determine variables independently related to ISR in the multivariate logistic regression analysis. Subgroup analysis was conducted to investigate the association between the MHR and ISR in different population. A receiver operating characteristic (ROC) curve was used to determine the predictive value of the MHR for DES-ISR, and the area under the curve (AUC) and optimal cut-off values were calculated. We also developed two models to evaluate whether including the MHR in other independently related factors could improve the predictive value for ISR. We used the − 2 log-likelihood ratio test to assess model significance and the Hosmer–Lemeshow goodness-of-fit chi-square test for model fit. DeLong’s test was used to compare the AUCs, and we calculated the categorical net reclassification improvement (NRI) and integrated discrimination improvement (IDI) to assess the predictive value of the MHR. All tests were two-sided at a significance level of 0.05, and all analyses were performed via SPSS version 25.0 and R version 4.2.3.
Results
Baseline characteristics of the patients
A total of 474 patients (283 males; mean age: 60.4 ± 8.6 years) who underwent primary DES implantation were enrolled. Patients were divided into the ISR group (n = 224) and the non-ISR group (n = 250) on the basis of follow-up coronary angiography. Baseline demographic, clinical, and angiographic characteristics are summarized in Table 1.
Age, total stent length, hypertension, smoking status, LVEF, target coronary artery, and the use of ACEIs/ARBs and beta blockers were similar in both the non-ISR and ISR groups. However, the ISR group had a greater percentage of male patients and patients with diabetes. Multivessel disease was more prevalent in the ISR group. The median time between the two coronary angiographies was longer in the ISR group than in the non-ISR group. Additionally, patients with ISR also had a narrower minimal stent diameterand a longer total stent length.
The hematological and biochemical parameters are presented in Table 2. The TC, LDL, and TG levels and lymphocyte counts were comparable between the two groups. However, compared with the non-ISR group, the ISR group presented significantly higher FBG, creatinine, uric acid, and hs-CRP levels; increased WBC, neutrophil, and monocyte counts; and lower HDL levels.
The MHR was significantly greater in the ISR group than in the non-ISR group (12.44 vs. 8.46, P < 0.001; Fig. 2A). Patients were divided into three groups on the basis of MHR tertiles, which revealed a significant increase in the percentage of ISR from tertile 1 (lowest MHR) to tertile 3 (highest MHR) (Fig. 2B).
Multivariate logistic regression analysis identified male, diabetes mellitus, the time between two coronary angiographies, the number of narrowed arteries, and the MHR as independent predictors of ISR. After adjusting for confounding factors, the MHR emerged as an independent predictor of ISR (OR = 1.244; 95%CI 1.171–1.321) (Table 3).
Subgroup analysis was conducted to investigate the association between the MHR and ISR. As illustrated in the forest plot, the correlation between MHR and ISR exhibits consistency across different subgroups (Fig. 3).
ROC analysis showed that the MHR for predicting ISR had an AUC of 0.752 (95% CI 0.708–0.796) (Fig.4A). On the ROC curve, we selected the point where the sum of specificity and sensitivity reached its maximum value. The MHR indicated by this point was 7.32, with a sensitivity of 59.8% (95% CI 47.2-66.5%) and a specificity of 81.2% (95% CI 71.2-86.4%). Additionally, we constructed two predictive models. One incorporated four variables that were independently associated with ISR in our study: male, diabetes, number of narrowed coronary arteries, and time between two coronary angiographies, which we refered to as established risk factors. The other model, in addition to these established risk factors, further includesd the MHR. The ROC curve analysis of the two models suggested that including the MHR improved the AUC from 0.698 to 0.782 (P < 0.001) (Fig. 4B) , and enhanced the predictive performance with a NRI of 0.703 (95%CI 0.536–0.871) and an IDI of 0.121 (95%CI 0.092–0.151) (Table 4).
Discussion
This study explored the relationship between the MHR and DES-ISR in patients with unstable angina pectoris. A higher MHR was linked to a greater likelihood of ISR after DES implantation, and it remained an independent risk factor after adjusting for confounders. The inclusion of the MHR with traditional risk factors may improve early risk stratification for DES-ISR.
Our study design was inspired by the work of Nan and colleagues, who investigated the predictive ability of the the MHR for ISR in patients with NST-ACS12. Utilizing data from our medical center, we aimed to explore the correlation between MHR and ISR in patients with unstable angina pectoris for several reasons: First, our medical center has a higher proportion of patients with unstable angina pectoris compared to those with stable angina pectoris and acute myocardial infarction. The incidence of stent implantation in patients with stable angina pectoris at our center is insufficient. Second, during acute myocardial infarction, there is an enhanced inflammatory response that may temporarily elevate monocyte counts prior to stent implantation, potentially biasing the estimation of the correlation between MHR and ISR. This rationale also underlies our exclusion of other conditions that could elevate inflammation. It is important to note that we selected patients undergoing their first stent implantation, as we were concerned that varying outcomes associated with different stents in patients with prior stenting could complicate interpretation. In our study, the incidence of ISR among patients undergoing first-time stent implantation was 10.1%. Considering those who did not undergo follow-up angiography, the actual incidence may be higher, which aligns with findings reported in other literature.
The development of ISR is significantly influenced by the inflammatory response, which acts as a critical mechanism. In clinical practice, routine assessment of blood cells as inflammatory indicators is feasible for investigating the correlation between the inflammatory response and ISR, such as neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), and C-reactive protein (CRP). Gabbasov et al. performed a research encompassing 126 patients with stable angina pectoris15. All participants underwent DES implantation, followed by angiographic evaluations within a 6- to 12-month timeframe. The results demonstrated that the NLR emerged as a significant, independent predictor of DES-ISR, exhibiting an OR of 2.7 (95% CI 1.3–5.5; P = 0.008). Similarly, Li et al. also identified the NLR as a predictor of DES-ISR in 416 patients with chronic total occlusion coronary artery disease (OR: 3.11; 95% CI 2.10–4.06; P < 0.001)16. They examined the utility of PLR in forecasting DES-ISR among the same cohort of patients, demonstrating that a preoperative increase in PLR correlates with a heightened risk of ISR. For patients with a PLR > 154.9, the sensitivity for restenosis was 54.2%, while the specificity was 88.7%. Despite being a well-studied systemic inflammatory marker closely associated with adverse cardiovascular outcomes, the correlation between CRP and ISR remains unclear. Two studies have reached contrasting conclusions regarding the relationship between ISR and CRP levels in patients with angina pectoris or myocardial infarction following DES implantation17,18. In our study, there were no statistically significant differences in NLR and PLR between the ISR group and the non-ISR group, with P-values of 0.297 and 0.301, respectively. CRP levels demonstrated variability among the various groups; however, upon conducting multivariate analysis, no statistically significant association was found between CRP and ISR. The correlation between inflammatory factors and ISR in various studies appears incnsistent, which may primarily be attributed to relatively small sample sizes and selection bias. Data from several studies revealed that the preprocedural value of the MHR was an independent predictor of BMS-ISR9,10,11. Nan et al. enrolled 214 patients with NSTE-ACS who had undergone DES implantation. The results revealed that the MHR was an independent predictor of DES-ISR (OR: 1.02, 95%CI 1.01–1.03; P = 0.041)12. Across different populations, our study reached the same conclusions as theirs, and in our study for patients with a MHR > 7.32, the sensitivity for restenosis was 59.8%, while the specificity was 81.2%. There are several key differences: we included a larger patient cohort, specifically focusing only on patients with unstable angina and excluding those with acute myocardial infarction, and we only included second-generation stents while excluding first-generation stents. We have endeavored to control confounding factors to the greatest extent possible, inevitably compromising the generalizability of the study conclusions. Similar to the study conducted by Nan et al., we also utilized quantitative coronary angiography analysis as the diagnostic basis for ISR. However, due to the influence of specific lesions (such as calcified lesions) and low-quality angiographic imaging, quantitative coronary angiography may not accurately reflect the degree of ISR within the stent. The introduction of intracoronary imaging examinations may help to reduce such bias. More prospective studies, including those that enroll a broader population and employ more precise intracoronary imaging examinations, are needed in the future to validate the relationship between MHR and ISR.
Excessive neointimal hyperplasia in the stent area is the main cause of ISR19,20. The inflammatory response plays a crucial role in the development of both neointimal hyperplasia and neoatherosclerosis. Monocytes play an indispensable role in inflammatory response. In a rabbit model, Welt et al. reported that neutrophils migrate to the stent area at an early stage and that monocytes sustain recruitment over the course of days or weeks21. Activated monocytes release proinflammatory cytokines that induce vasoconstriction, promote nonspecific cellular recruitment, and facilitate the proliferation and activation of additional cell types within the vessel wall, particularly vascular smooth muscle cells22,23. Fukuda et al. also demonstrated that circulating monocytes are a source of in-stent neointimal hyperplasia24. Furthermore, neoatherosclerosis has been observed earlier and more frequently in patients with DES. It is well known that monocytes serve as initiating cells in the atherosclerotic process and participate in the inflammatory initiation of atherosclerosis. There exists an interaction between HDL and monocytes. HDL has a strong ability to suppress the endothelial expression of adhesion molecules, effectively preventing the recruitment of monocytes to the arterial wall25. HDL closely interacts with monocytes, inhibiting their functional activities and disrupting their differentiation into macrophages, thereby limiting the subsequent inflammatory response26.HDL has several potentially antiatherogenic properties. First, HDL facilitates the removal of cholesterol from cells through the reverse cholesterol transport system, a crucial mechanism for maintaining cholesterol homeostasis27. Second, the antiatherogenic effect of HDL is enhanced by its inherent antioxidant and anti-inflammatory properties, which collectively help mitigate atherogenic processes28. Third, HDL exerts multifaceted protective effects by inhibiting endothelial cell apoptosis, promoting reendothelialization, stimulating endothelial cell-mediated prostacyclin synthesis, reducing platelet aggregability, and modulating endothelial function by increasing the release of endothelial nitric oxide28,29,30. It is noteworthy that a study has indicated that high HDL levels may increase cardiovascular risk in hypertensive patients31. Other studies have also reported similar conclusions32,33. HDL levels appear to exhibit a U-shaped association with cardiovascular events rather than a linear correlation. In our study, significant difference in monocytes and HDL was observed between the ISR group and the non-ISR group, yet neither showed an independent correlation with ISR in multivariate analysis. Possible reasons for this observation lie in the fact that the occurrence of ISR is a consequence of multiple factors acting together, among which monocytes and HDL both play roles. Additionally, there is an interaction between monocytes and HDL. A preoperative high MHR indicates a state of elevated monocytes accompanied by low HDL cholesterol levels in patients. Following stent implantation, inflammation in the coronary artery intima is triggered. With the weakened ability of HDL to inhibit monocyte recruitment, activation, and proliferation, more monocytes interact with the coronary artery intima, promoting excessive intimal hyperplasia. Meanwhile, the combination of high monocytes and low HDL cholesterol predisposes individuals to the formation of atherosclerosis.
Preoperative MHR, as a clinically accessible inflammatory biomarker, demonstrates potential in predicting the occurrence of DES-ISR and can be utilized for risk stratification post-DES implantation. Patients with high MHR values may benefit from intensified treatment strategies to prevent the occurrence of ISR. LDL serves as a determinant factor in coronary artery atherosclerosis. Remnant lipoproteins play an important role of in-stent restenosis in patients with type 2 diabetes34. Lipid-lowering therapy remains the cornerstone of pharmacological treatment following DES procedures. The latest research indicates that long-lasting control of LDL Induces a 40% reductionin the incidence of cardiovascular events35. Accumulating evidence supports the efficacy of PCSK-9 inhibitors in lowering LDL levels. Additionally, several studies have indicated the anti-inflammatory effects of PCSK-9 inhibitors beyond lipid-lowering36,37. PCSK-9 inhibitors exhibit potential as therapeutic agents for the prevention of ISR. In our study, diabetes mellitus is independently associated with ISR. A study has shown that hyperglycemia drives stent restenosis in ST-elevation myocardial infarction patients38. Among antidiabetic drugs, pioglitazone is considered to have cardioprotective effects. The underlying mechanisms may encompass anti-remodeling properties (including endothelium protection, inflammation modulation, anti-proliferation, and anti-fibrosis) as well as modulation of metabolic (such as adipose tissue metabolism and elevated HDL cholesterol levels) and neurohormonal pathways (including the renin-angiotensin-aldosterone system, sympathetic nervous system, and adiponectin) within the cardiovascular system39. Pioglitazone is a another potential drug for the prevention of ISR. Considering the role of HDL in atherosclerosis resistance and inhibition of intimal hyperplasia, HDL-targeted therapies have been reported in vitro and in animal experiments40. The study demonstrates that reconstituted HDL exerts a potent anti-neointimal hyperplasia effect through mechanisms that include reducing leukocyte infiltration and smooth muscle cell proliferation, while simultaneously promoting endothelial cell proliferation. More research is needed to validate its therapeutic effectiveness.
Conclusion
Preoperative MHR, as a clinically accessible inflammatory biomarker, was independently associated with DES-ISR among patients with unstable angina pectoris. It possesses the potential to be utilized in risk stratification for DES-ISR, with the aim of preventing the onset of ISR.
Data availability
The datasets supporting the conclusions of the study are included in the article. Any additional data can be made available from the corresponding author upon reasonable request.
Abbreviations
- ISR:
-
In-stent restenosis
- DES:
-
Drug-eluting stent
- ROC:
-
Receiver operating characteristic
- MHR:
-
Monocyte-to-high-density lipoprotein cholesterol ratio
- PCI:
-
Percutaneous coronary intervention
- BMS:
-
Bare metal sten
- LVEF:
-
Left ventricular ejection fraction
- FBG:
-
Fasting blood glucose
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- LDL-C:
-
Low-density lipoprotein-C
- HDL-C:
-
High-density lipoprotein-C
- hs-CRP:
-
High-sensitivity C-reactive protein
- WBC:
-
White blood cells
- LAD:
-
Left anterior descending artery
- LCX:
-
Left circumflex artery
- RCA:
-
Right coronary arteryara
- ACEI:
-
Angiotensin-converting enzyme inhibitors
- ARB:
-
Angiotensin receptor blockers
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- NSTE-ACS:
-
Non-ST-segment elevation acute coronary syndrome
- STEMI:
-
ST-segment elevation myocardial infarction
References
Alfonso, F., Byrne, R. A., Rivero, F. & Kastrati, A. Current treatment of in-stent restenosis. J. Am. Coll. Cardiol. 63, 2659–2673. https://doi.org/10.1016/j.jacc.2014.02.545 (2014).
Byrne, R. A., Joner, M. & Kastrati, A. Stent thrombosis and restenosis: What have we learned and where are we going? The Andreas Grüntzig lecture ESC 2014. Eur. Heart J. 36, 3320–3331. https://doi.org/10.1093/eurheartj/ehv511 (2015).
Dangas, G. D. et al. In-stent restenosis in the drug-eluting stent era. J. Am. Coll. Cardiol. 56, 1897–1907. https://doi.org/10.1016/j.jacc.2010.07.028 (2010).
Kanbay, M. et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int. Urol. Nephrol. 46, 1619–1625. https://doi.org/10.1007/s11255-014-0730-1 (2014).
Akboga, M. K. et al. Usefulness of monocyte to HDL-cholesterol ratio to predict high SYNTAX score in patients with stable coronary artery disease. Biomark. Med. 10, 375–383. https://doi.org/10.2217/bmm-2015-0050 (2016).
Cetin, M. S. et al. Monocyte to HDL cholesterol ratio predicts coronary artery Disease Severity and Future Major Cardiovascular adverse events in Acute Coronary Syndrome. Heart Lung Circ. 25, 1077–1086. https://doi.org/10.1016/j.hlc.2016.02.023 (2016).
Kundi, H. et al. Association of monocyte/HDL-C ratio with SYNTAX scores in patients with stable coronary artery disease. Herz 41, 523–529. https://doi.org/10.1007/s00059-015-4393-1 (2016).
Zhang, Y. et al. Is monocyte to HDL ratio superior to monocyte count in predicting the cardiovascular outcomes: Evidence from a large cohort of Chinese patients undergoing coronary angiography. Ann. Med. 48, 305–312. https://doi.org/10.3109/07853890.2016.1168935 (2016).
Tok, D. et al. Monocyte to HDL ratio in prediction of BMS restenosis in subjects with stable and unstable angina pectoris. Biomark. Med. 10, 853–860. https://doi.org/10.2217/bmm-2016-0071 (2016).
Ucar, F. M. A potential marker of bare metal stent restenosis: Monocyte count - to- HDL cholesterol ratio. BMC Cardiovasc. Disord. 16 https://doi.org/10.1186/s12872-016-0367-3 (2016).
Yilmaz, S. et al. Usefulness of the monocyte-to-high-density lipoprotein cholesterol ratio to predict bare metal stent restenosis. Biomark. Med. 10, 959–966. https://doi.org/10.2217/bmm-2016-0069 (2016).
Nan, J. et al. The predictive value of Monocyte Count to high-density lipoprotein cholesterol ratio in restenosis after drug-eluting stent implantation. Int. J. Gen. Med. 13, 1255–1263. https://doi.org/10.2147/ijgm.S275202 (2020).
Neumann, F. J. et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur. Heart J. 40, 87–165. https://doi.org/10.1093/eurheartj/ehy394 (2019).
Byrne, R. A. et al. [2023 ESC Guidelines for the management of acute coronary syndromes]. Giornale italiano di cardiologia () 25, e1–e112, (2006). https://doi.org/10.1714/4191.41785 (2024).
Gabbasov, Z. et al. Blood level of CD45 + platelets and development of restenosis after drug-eluting stent implantation in patients with stable coronary artery disease. Wien. Klin. Wochenschr. 128, 898–905. https://doi.org/10.1007/s00508-016-1074-x (2016).
Li, C. et al. Evaluation of Preprocedural Laboratory Parameters as predictors of Drug-Eluting Stent Restenosis in Coronary Chronic total occlusion lesions. Angiology 70, 272–278. https://doi.org/10.1177/0003319717752245 (2019).
Mincu, R. I., Jánosi, R. A., Vinereanu, D., Rassaf, T. & Totzeck, M. Preprocedural C-Reactive protein predicts outcomes after primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction a systematic meta-analysis. Sci. Rep. 7, 41530. https://doi.org/10.1038/srep41530 (2017).
Xu, Y. L. et al. Role of plasma C-reactive protein in predicting in-stent restenosis in patients with stable angina after coronary stenting. Chin. Med. J. 124, 845–850 (2011).
Hoffmann, R. et al. Patterns and mechanisms of in-stent restenosis. A serial intravascular ultrasound study. Circulation 94, 1247–1254. https://doi.org/10.1161/01.cir.94.6.1247 (1996).
Grewe, P. H., Deneke, T., Machraoui, A., Barmeyer, J. & Müller, K. M. Acute and chronic tissue response to coronary stent implantation: Pathologic findings in human specimen. J. Am. Coll. Cardiol. 35, 157–163. https://doi.org/10.1016/s0735-1097(99)00486-6 (2000).
Welt, F. G. et al. Leukocyte recruitment and expression of chemokines following different forms of vascular injury. Vasc. Med. 8, 1–7. https://doi.org/10.1191/1358863x03vm462oa (2003).
Liu, Y. et al. Association between circulating monocyte subsets and in-stent restenosis after coronary stent implantation in patients with ST-elevation myocardial infarction. Circulation Journal: Official J. Japanese Circulation Soc. 74, 2585–2591. https://doi.org/10.1253/circj.cj-10-0544 (2010).
Welt, F. G. & Rogers, C. Inflammation and restenosis in the stent era. Arterioscler. Thromb. Vasc. Biol. 22, 1769–1776. https://doi.org/10.1161/01.atv.0000037100.44766.5b (2002).
Fukuda, D. et al. Circulating monocytes and in-stent neointima after coronary stent implantation. J. Am. Coll. Cardiol. 43, 18–23. https://doi.org/10.1016/j.jacc.2003.08.026 (2004).
Cockerill, G. W., Rye, K. A., Gamble, J. R., Vadas, M. A. & Barter, P. J. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler. Thromb. Vasc. Biol. 15, 1987–1994. https://doi.org/10.1161/01.atv.15.11.1987 (1995).
Murphy, A. J. et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler. Thromb. Vasc. Biol. 28, 2071–2077. https://doi.org/10.1161/atvbaha.108.168690 (2008).
Barter, P., Kastelein, J., Nunn, A. & Hobbs, R. High density lipoproteins (HDLs) and atherosclerosis; The unanswered questions. Atherosclerosis 168, 195–211. https://doi.org/10.1016/s0021-9150(03)00006-6 (2003).
Barter, P. J. et al. Antiinflammatory properties of HDL. Circul. Res. 95, 764–772. https://doi.org/10.1161/01.Res.0000146094.59640.13 (2004).
Seetharam, D. et al. High-density lipoprotein promotes endothelial cell migration and reendothelialization via scavenger receptor-B type I. Circul. Res. 98, 63–72. https://doi.org/10.1161/01.RES.0000199272.59432.5b (2006).
Zeiher, A. M. & Schächinger, V. Coronary endothelial vasodilator dysfunction: Clinical relevance and therapeutic implications. Z. Kardiol. 83 (Suppl 4), 7–14 (1994).
Trimarco, V. et al. High HDL (high-Density lipoprotein) cholesterol increases cardiovascular risk in hypertensive patients. Hypertens. (Dallas Tex. : 1979). 79, 2355–2363. https://doi.org/10.1161/hypertensionaha.122.19912 (2022).
Liu, C. et al. Association between high-density lipoprotein cholesterol levels and adverse cardiovascular outcomes in high-risk populations. JAMA Cardiol. 7, 672–680. https://doi.org/10.1001/jamacardio.2022.0912 (2022).
Hirata, A. et al. Association of extremely high levels of high-density lipoprotein cholesterol with cardiovascular mortality in a pooled analysis of 9 cohort studies including 43,407 individuals: the EPOCH-JAPAN study. J. Clin. Lipidol. 12, 674–684e675. https://doi.org/10.1016/j.jacl.2018.01.014 (2018).
Qin, Z. et al. Remnant lipoproteins play an important role of in-stent restenosis in type 2 diabetes undergoing percutaneous coronary intervention: A single-centre observational cohort study. Cardiovasc. Diabetol. 18, 11. https://doi.org/10.1186/s12933-019-0819-z (2019).
Trimarco, V. et al. Long-lasting control of LDL cholesterol induces a 40% reduction in the incidence of cardiovascular events: New insights from a 7-Year study. J. Pharmacol. Exp. Ther. 388, 742–747. https://doi.org/10.1124/jpet.123.001878 (2024).
Marfella, R. et al. Evidence of an anti-inflammatory effect of PCSK9 inhibitors within the human atherosclerotic plaque. Atherosclerosis 378, 117180. https://doi.org/10.1016/j.atherosclerosis.2023.06.971 (2023).
Cariou, B., Ding, Z. & Mehta, J. L. PCSK9 and atherosclerosis: Beyond LDL-cholesterol lowering. Atherosclerosis 253, 275–277. https://doi.org/10.1016/j.atherosclerosis.2016.08.007 (2016).
Mone, P. et al. Hyperglycemia drives stent restenosis in STEMI patients. Diabetes care. 44, e192–e193. https://doi.org/10.2337/dc21-0939 (2021).
Nesti, L., Tricò, D., Mengozzi, A. & Natali, A. Rethinking pioglitazone as a cardioprotective agent: A new perspective on an overlooked drug. Cardiovasc. Diabetol. 20, 109. https://doi.org/10.1186/s12933-021-01294-7 (2021).
Kim, Y. J. et al. Mechanistic insights into the anti-restenotic effects of HSP27 and HO1 modulated by reconstituted HDL on neointimal hyperplasia. Sci. Rep. 13, 22078. https://doi.org/10.1038/s41598-023-49367-9 (2023).
Acknowledgements
We thank Xu Meng and Lingyan Wang for their support in writing the manuscript.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
HM made substantial contributions to the study design, data analysis, data interpretation and manuscript writing. ZY and XJZ collected and analysed the angiography data. YYL and LSL collected and analysed the clinical, biochemical and hematological data. YZ and YJL designed the study, analysed the data and revised the manuscript. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was submitted to and approved by the Ethics Commission of Chest Hospital, Tianjin University (IRB-SOP-016[F]-001-03), and strictly adhered to the principles of the Declaration of Helsinki. This was a retrospective study, so the content to be included was not applicable.
Consent for publication
This study does not contain data from any individual person, so consent for publication is not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Meng, H., Zhou, X., Li, L. et al. Monocyte to high-density lipoprotein cholesterol ratio predicts restenosis of drug-eluting stents in patients with unstable angina pectoris. Sci Rep 14, 30175 (2024). https://doi.org/10.1038/s41598-024-81818-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81818-9