Abstract
This study evaluated the ability of the triglyceride (TG) to high-density lipoprotein cholesterol (TG/HDL-C) ratio to identify individuals at risk of type 2 diabetes mellitus (T2DM) in the non-alcoholic fatty liver disease (NAFLD) population. We retrospectively studied 4,769 patients with NAFLD from the Affiliated Hospital of Hangzhou Normal University (2020–2023). Binary logistic regression models were used to evaluate the association between the TG/HDL-C ratio and lipid parameters with T2DM. TG/HDL-C ratio was positively associated with T2DM in patients with NAFLD, with an odds ratio (OR) of 2.72 (95% confidence interval, 2.23–3.31, p < 0.001) for T2DM in the highest TG/HDL-C ratio quartile compared with the lowest one after adjusting for known confounders. The OR for the TG/HDL-C ratio had a stronger predictive value than those of TG, total cholesterol, HDL-C, and low-density lipoprotein cholesterol, indicating that the TG/HDL-C ratio could be a better discriminator of T2DM. The TG/HDL-C ratio better identifies potential risks of T2DM in individuals with NAFLD than individual lipid parameters. Therefore, clinicians should pay attention to individuals with high TG and low HDL-C levels during T2DM risk assessment in NAFLD cohorts.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) is defined by macrovesicular steatosis in ≥ 5% hepatocytes in the absence of a secondary cause such as alcohol or drugs, and mainly characterized by hepatocellular lipid accumulation especially triglyceride along with inflammation and varying degrees of fibrosis and cirrhosis1. NAFLD is an increasingly common condition believed to affect > 25% of adults worldwide2. The incidence of NAFLD in adults and children is expected to progressively increase in proportion to rising rates of obesity, metabolic syndrome, and type 2 diabetes mellitus (T2DM). The global prevalence of NAFLD is predicted to exceed 35% within the next decade2,3. A growing interest has led to the observation that NAFLD was independently associated with an increased risk of cardiovascular disease, the principal cause of death in patients with NAFLD4,5,6,7,8.
T2DM is another global public health problem with an increasing incidence rate and prevalence that needs to be solved urgently. A large body of evidence suggests a strong association between T2DM and NAFLD9,10. A diagnosis of NAFLD in non-diabetic patients was associated with an increased risk of T2DM11,12, and T2DM was associated with an increased risk of NAFLD13,14. T2DM significantly increases the risk of cardio-metabolic comorbidities and liver-related mortality in patients with NAFLD13,15,16. Considering the independent and overlapped burden associated with these diseases, a clinical evaluation of plasma glucose or glycosylated hemoglobin in patients with NAFLD and early identification of those at risk of developing DM is fundamental to detecting concomitant cardio-metabolic complications.
Although the underlying mechanisms remain incompletely understood, these interactions primarily contribute to visceral adiposity and insulin resistance (IR)17,18. The triglyceride (TG)/high-density lipoprotein cholesterol (HDL-C) ratio, an index based on the individual’s lipoprotein cholesterol concentrations, is closely associated with IR. Most previous studies on the relationship between the TG/HDL-C ratio and the incidence of T2DM reported a positive association19,20,21,22,23.
However, studies on the association between the TG/HDL-C ratio and T2DM in patients with NAFLD are lacking. Furthermore, a comparison of the discriminative abilities of the TG/HDL-C ratio and individual lipid parameters for the risk of T2DM in these patients is also missing. Therefore, the current study aimed to explore the value of the TG/HDL-C ratio in predicting T2DM in patients with NAFLD. We expect the TG/HDL-C ratio to be a practical tool as it is readily available.
Materials and methods
Study population
We retrospectively screened 8,439 patients hospitalized at the Affiliated Hospital of Hangzhou Normal University during 2020–2023 with a clinical diagnosis of NAFLD. Based on the guidelines proposed by the Asia-Pacific Working Party, NAFLD was diagnosed by the presence of fatty liver, while ruling out excessive alcohol intake (> 140 g/week for males; >70 g/week for females), a history of hepatic viral infection, and the utilization of steatogenic or hepatotoxic medicines24. Fatty liver was assessed semi-quantitatively by an experienced ultrasonography operator using standard methods, such as the presence of hepatic steatosis and increased echo in the liver compared to the renal cortex24. T2DM diagnosis followed the American Diabetes Association criteria from 200325. We excluded participants older than 80 or younger than 18 and those with incomplete demographic, biochemical indexes, or hepatic ultrasonographic data. This study is a retrospective research project that has obtained approval from the Ethics Committee of Hangzhou Normal University Affiliated Hospital and informed consent has been waived (protocol code 2024(E2)-KS-083). The study complied with the provisions of the Declaration of Helsinki.
Data collection
Baseline data on demographic characteristics and laboratory results, including metabolic-related parameters such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), fast blood glucose (FBG), creatinine, uric acid, and serum lipids [including TG, total cholesterol (TC), HDL-C, low-density lipoprotein cholesterol (LDL-C)], apolipoprotein A, apolipoprotein B, albumin, white blood cell count, neutrophils, lymphocyte, monocyte, platelets, and C-reactive protein were extracted from the hospital information system and electronic laboratory records, retrospectively. Blood samples were collected after overnight fasting and analyzed by chemiluminescence on an auto-analyzer. Simple, non-invasive indexes used for fibrosis staging, such as the Fibrosis‐4 (FIB‐4) index and NAFLD fibrosis score (NFS), were calculated as follows:
NFS = − 1.675 + 0.037×age (years) + 0.094×body mass index (BMI; kg/m2) + 1.13×impaired fasting plasma glucose (FBG)/diabetes mellitus (yes = 1, no = 0) + 0.99×AST/ALT ratio − 0.013×platelet count (×109/L) − 0.66×albumin (g/dL).
The TG/HDL-C ratio was divided into four quintiles: <25% (Q1), 25–50% (Q2), 50–75% (Q3), and ≥ 75% (Q4).
Statistical analysis
Continuous variables following a skewed distribution are presented as medians and interquartile ranges. Categorical variables are presented as counts and percentages. Qualitative variables were compared using the Chi-squared or Fisher’s exact test as suitable. Quantitative variables were compared using the Mann-Whitney U test. Univariate and multivariate logistic regression analyses were employed to evaluate the relationships between TG/HDL-C ratio, TC, TG, HDL-C, and LDL-C with the risk of T2DM in NAFLD.
To explore the association between TG/HDL-C ratio and T2DM risk, we developed three logistic regression models. Model 0, unadjusted; Model 1, adjusted for age and sex; Model 2, further adjusted for AST and ALT levels; Model 3, further adjusted for LDL-C and creatinine levels. Odds ratios (OR) with 95% confidence intervals (CI) for the risk of T2DM were calculated. All tests were two-sided, and p < 0.05 were considered statistically significant. All data were analyzed using the R software version 4.2.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of the study cohorts
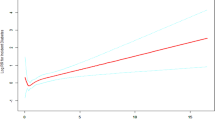
Overall, 4,769 patients with NAFLD were assessed (Figs. 1), 1,164 (24.4%) with T2DM and 3,605 (75.6%) without T2DM. Males constituted 65.4 and 64.9%, respectively. Participants with T2DM were associated with older age and a higher proportion of males. The laboratory results of patients in the two cohorts were markedly different (Table 1). Compared with those without T2DM, participants with T2DM had higher FBG [5.64 (5.06–6.67) vs. 8.25 (6.44–11.7) mmol/L, p < 0.001], TG [1.51 (1.09–2.14) vs. 1.69 (1.18–2.44) mmol/L, p < 0.001], and creatinine [64.4 (49.2–77.6) vs. 67.0 (55.05–80.63) umol/L, p < 0.001], and lower HDL-C [1.05 (0.89–1.24) vs. 0.99 (0.84–1.17) mmol/L, p < 0.001], LDL-C [2.79 (2.28–3.3) vs. 2.61 (1.99–3.25) mmol/L, p < 0.001], and TC [4.63 (3.93–5.37) vs. 4.45 (3.57–5.35) mmol/L, p < 0.001]. Moreover, patients with T2DM had a higher TG/HDL-C ratio than those without [1.69 (1.15–2.68) vs. 1.46 (0.97–2.21), p < 0.001]. Liver fibrosis was more severe in the T2DM than non-T2DM cohort as indicated by higher FIB-4 index [1.17 (0.77–1.71) vs. 1.31 (0.93–1.88), p < 0.001] and NFS [–3.48 (–4.65 to − 2.27) vs. − 2.04 (–3.10 to − 0.68), p < 0.001] values.
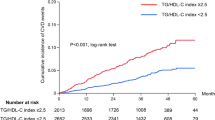
Associations between the TG/HDL-C ratio and lipid parameters and T2DM risk
After univariate logistic regression, Age, WBC, Albumin, TC, TG, FBG, HDL-C, UA, LDL-C, apoA, ALT, AST, NFS, and TG/HDL-C quartile were included in multivariable logistic regression model (Supplementary Table 1). Table 2 shows the OR and 95% CI of T2DM with TG/HDL-C quartile, TC, TG, HDL-C, and LDL-C in the entire population based on binary logistic regression models established separately for each lipid parameter. As shown, TG (OR, 1.12; 95% CI, 1.08–1.16; p < 0.001) was positively associated with T2DM, while TC (OR, 0.93; 95% CI, 0.88–0.98; p = 0.006) and HDL-C (OR, 0.53; 95% CI, 0.42–0.68; p < 0.001) were negatively associated with T2DM. Multivariable analysis indicated that HDL-C, LDL-C were not associated with T2DM.The OR of the TG/HDL - C quartile is higher. The TG/HDL-C ratio Q1, Q2, Q3, and Q4 comprised 18.4%, 25.2%, 23.3%, and 33.2% of the T2DM cohort and 27.2%, 24.8%, 25.5%, and 22.4% of the non-T2DM cohort, respectively (Fig. 2). As presented in Table 3, binary logistic regression models indicated that the T2DM risk was positively associated with the TG/HDL-C ratio. For TG/HDL-C ratio the highest Q4 compared with the lowest one Q1, Model 0 indicated OR of 2.19 (95% CI, 1.81–2.66; p < 0.001), Model 1 indicated OR of 1.60 (95% CI, 1.31–1.96, p < 0.001), Model 2 indicated OR of 2.68 (95% CI, 2.20–3.26; p < 0.001), and Model 3 indicated OR of 2.72 (95% CI, 2.23–3.31; p < 0.001).
Discussion
In this data analysis of 4,769 patients with NAFLD, we found that serum lipid abnormalities in patients with T2DM are highlighted by increased TG and decreased HDL-C. These and the TG/HDL-C ratio were associated with an elevated risk of T2DM. The TG/HDL-C ratio had shown a superior predictive capacity for T2DM with an OR of 2.72 in the highest TG/HDL-C ratio quartile after adjusting for confounders.
T2DM and NAFLD are common chronic diseases in China. The link between them is complex because they share multiple common pro-inflammatory and pro-fibrotic pathways26,27. Increasing evidence from studies with biopsy-diagnosed NAFLD suggests that the coexistence of T2DM represents an independent predictor of histological severity and progression in advanced fibrosis in NAFLD13,14,28. Our analysis found that patients with T2DM tended to have higher FIB-4 index and NFS values. Despite the debate concerning the causality between T2DM and NAFLD, increasing epidemiological evidence suggests that NAFLD might precede T2DM11,12Concomitant T2DM significantly increases the risk of severe cardiovascular events in patients with NAFLD. In 2020, international experts recommended changing the term from NAFLD to Metabolic-Associated Fatty Liver Disease (MAFLD)29.
Changes in its definition further emphasized the strong and bidirectional association between T2DM and NAFLD. Several extensive studies indicated that more than 70% of patients with T2DM develop NAFLD30,31. Our analysis found that patients with T2DM accounted for 24.4% of the NAFLD cohort. This prevalence concurs with previous reports that fluctuated around 29%32,33. Therefore, T2DM screening should be suggested and implemented in patients with NAFLD and/or advanced liver fibrosis.
IR is the primary driver and pathogenic basis of cardiovascular disease and many metabolic diseases, including T2DM and NAFLD34,35. IR leads to increased degradation of HDL-C by increasing the activity of liver esterase; it induces hyperinsulinemia that promotes liver synthesis of TG and VLDL and weakens the clearance of TG, resulting in hypertriglyceridemia35,36. Therefore, high TG and low HDL-C levels are associated with IR, impaired glucose tolerance, T2DM, visceral adiposity, obesity, and metabolic syndrome, all associated with an increased risk of NAFLD. Our NAFLD cohort had comparable results, showing increased TG and decreased HDL-C values, which were associated with an elevated risk of T2DM after adjusting for age, sex, ALT, AST level, TG, LDL-C, and creatinine.
However, TG and HDL-C levels alone were weaker risk factors than the TG/HDL-C ratio because the two parameters are closely interrelated19,37. The TG/HDL-C ratio was first proposed by McLaughlin et al.38, who demonstrated its clinical utility in identifying healthy Caucasians with IR. This ratio has been widely used to assess the associations between IR and various clinical syndromes. Most previous studies on the relationship between the TG/HDL-C ratio and the incidence of T2DM reported a positive association20,23. A cross-sectional study including 687 adults with a 15-year follow-up period reported that increased an TG/HDL ratio increased the risk of type 2 diabetes. And another retrospective cohort study showed the gender differences: a higher TG/HDL-C ratio was the independent predictive factor of incident diabetes in men (hazard ratio 1.30, 95% confidence interval 1.03–1.64), compared with women (hazard ratio 0.85, 95% confidence interval 0.53–1.38)23. Our present study also examined the association between the TG/HDL-C ratio and other lipid parameters with T2DM. In our study, although TC, TG, HDL - C, LDL - C and TG/HDL - C quartile were all associated with T2DM in the univariate analysis, TC, HDL - C and LDL - C lost their significance after multivariate analysis. Moreover, the OR value of the TG/HDL - C quartile was higher than that of TG, both in the univariate and multivariate analyses. The risk of T2DM was positively associated with the TG/HDL-C ratio. In the highest TG/HDL-C quartile, the analysis indicated an OR of 2.19 (95% CI, 1.81–2.66) or 2.72 (95% CI, 2.23–3.31) for developing T2DM, depending on the variables adjusted. A retrospective cohort study in Beijing showed that the TG/HDL-C ratio was positively associated with the incidence of T2DM during a 4-year follow-up (OR, 1.49; 95% CI, 1.26–1.78)39.
We noted that the TC level negatively affected the risk of T2DM in NAFLD while LDL-C showed no significant association, which seems the characteristics of lipid metabolism in patients with T2DM remain controversial. Some studies suggested that lipid metabolism disorder in patients with T2DM is mainly manifested as atherosclerotic dyslipidemia, i.e., increased TG, decreased HDL-C, and increased small dense low-density lipoprotein, with or without an increase in LDL-C40. However, other studies have shown that among patients with T2DM, the incidence of low HDL-C was the highest, followed by high LDL-C41,42. Some studies have shown that IR increases the lipase activity in the liver, which can lead to increased TG degradation throughout the body and the production of a large number of free fatty acids (FFAs). FFAs can be synthesized into very low-density lipoprotein (VLDL) as a substrate in the liver. Under the induction of liver lipase, VLDL is converted into LDL-C43. However, the results of this study suggest that using only LDL-C as a risk assessment indicator might be inappropriate for T2DM risk prediction. This might be because medication-related information, such as the use of statin, was lacking. According to guidelines for risk assessment and management of cardiovascular diseases, it is recommended to start primary prevention drugs early for patients with T2DM who are identified with high cardiovascular risk44. Statin, the cornerstone of treatment, significantly reduces LDLC and cholesterol44.
Our analysis had some limitations. First, because of the characteristics of our hospital’s database, we limited the cohort to inpatients. However, it is generally believed that hospitalized patients have more serious conditions than outpatients, which may have affected our results. Second, some important baseline characteristics affecting the lipid profile of patients with T2DM, including hypoglycemic and hypolipidemic drug use and smoking status, were not acquired.
Data availability
The dataset generated and/or analyzed during the current study are not publicly available but are available from the corresponding author and the first author on reasonable request.
References
Brunt, E. M. et al. Nonalcoholic steatohepatitis: histologic features and clinical correlations with 30 blinded biopsy specimens. Hum. Pathol. 35 (9), 1070–1082. https://doi.org/10.1016/j.humpath.2004.04.017 (2004).
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64 (1), 73–84. https://doi.org/10.1002/hep.28431 (2016).
Duell, P. B. et al. Nonalcoholic fatty liver Disease and Cardiovascular Risk: A Scientific Statement from the American Heart Association. Arterioscler. Thromb. Vasc Biol. 42 (6), e168–e185. https://doi.org/10.1161/ATV.0000000000000153 (2022).
Abosheaishaa, H. et al. Association between non-alcoholic fatty liver disease and coronary artery disease outcomes: a systematic review and meta-analysis. Diabetes Metab. Syndr. 18 (1), 102938. https://doi.org/10.1016/j.dsx.2023.102938 (2024).
Chen, C. C. et al. Association between the severity of nonalcoholic fatty liver Disease and the risk of coronary artery calcification. Med. (Kaunas). 57 (8), 807. https://doi.org/10.3390/medicina57080807 (2021).
Cucoranu, D. C. et al. Correlation between Coronary Artery Disease and Non-Alcoholic Fatty Liver Disease Using Computed Tomography Coronary Calcium Scans. Curr. Health Sci. J. 2023 Apr-Jun 49(2), 244–250. https://doi.org/10.12865/CHSJ.49.02.244.
Pais, R. et al. Relationship among fatty liver, specific and multiple-site atherosclerosis, and 10-Year Framingham score. Hepatology 69 (4), 1453–1463. https://doi.org/10.1002/hep.30223 (2019).
Targher, G., Day, C. P. & Bonora, E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl. J. Med. 363 (14), 1341–1350. https://doi.org/10.1056/NEJMra0912063 (2010).
Tanase, D. M. et al. The intricate relationship between type 2 diabetes Mellitus (T2DM), insulin resistance (IR), and nonalcoholic fatty liver Disease (NAFLD). J. Diabetes Res. 2020, 3920196. https://doi.org/10.1155/2020/3920196 (2020).
Younossi, Z. M. et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J. Hepatol. 71 (4), 793–801. https://doi.org/10.1016/j.jhep.2019.06.021 (2019).
Ballestri, S. et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J. Gastroenterol. Hepatol. 31 (5), 936–944. https://doi.org/10.1111/jgh.13264 (2016).
Yamada, T. et al. Fatty liver predicts impaired fasting glucose and type 2 diabetes mellitus in Japanese undergoing a health checkup. J. Gastroenterol. Hepatol. 25 (2), 352–356. https://doi.org/10.1111/j.1440-1746.2009.05998.x (2010).
McPherson, S. et al. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J. Hepatol. 62 (5), 1148–1155. https://doi.org/10.1016/j.jhep.2014.11.034 (2015).
Goh, G. B. et al. Clinical spectrum of non-alcoholic fatty liver disease in diabetic and non-diabetic patients. BBA Clin. 3, 141–145. https://doi.org/10.1016/j.bbacli.2014.09.001 (2014).
Chan, J. C. N. et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet 396 (10267), 2019–2082. https://doi.org/10.1016/S0140-6736(20)32374-6 (2021).
Emerging Risk Factors Collaboration et al. Association of Cardiometabolic Multimorbidity with Mortality. JAMA 314 (1), 52–60. https://doi.org/10.1001/jama.2015.7008 (2015).
Targher, G. et al. The complex link between NAFLD and type 2 diabetes mellitus - mechanisms and treatments. Nat. Rev. Gastroenterol. Hepatol. 18 (9), 599–612. https://doi.org/10.1038/s41575-021-00448-y (2021).
El Hadi, H. et al. Cardio-metabolic disorders in non-alcoholic fatty liver disease. Int. J. Mol. Sci. 20 (9), 2215. https://doi.org/10.3390/ijms20092215 (2019).
Ren, X. et al. Association between triglyceride to HDL-C ratio (TG/HDL-C) and Insulin Resistance in Chinese patients with newly diagnosed type 2 diabetes Mellitus. PLoS One. 11 (4), e0154345. https://doi.org/10.1371/journal.pone.0154345 (2016).
Young, K. A. et al. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance, β-cell function, and diabetes in hispanics and African americans. J. Diabetes Complications. 33 (2), 118–122. https://doi.org/10.1016/j.jdiacomp.2018.10.018 (2019).
Zhang, Y. et al. Association of TG/HDLC ratio trajectory and risk of type 2 diabetes: a retrospective cohort study in China. J. Diabetes. 19 https://doi.org/10.1111/1753-0407.13123 (2020 Oct).
Chen, Z. et al. Association of Triglyceride to high-density lipoprotein cholesterol ratio and incident of diabetes mellitus: a secondary retrospective analysis based on a Chinese cohort study. Lipids Health Dis. 19 (1), 33. https://doi.org/10.1186/s12944-020-01213-x (2020).
Qin, H. et al. Triglyceride to high-density lipoprotein cholesterol ratio is associated with incident diabetes in men: a retrospective study of Chinese individuals. J. Diabetes Investig. 11 (1), 192–198. https://doi.org/10.1111/jdi.13087 (2020).
Wong, V. W. et al. Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease guidelines 2017-Part 1: definition, risk factors and assessment. J. Gastroenterol. Hepatol. 33 (1), 70–85. https://doi.org/10.1111/jgh.13857 (2018).
Genuth, S. et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 26 (11), 3160–3167. https://doi.org/10.2337/diacare.26.11.3160 (2003).
Adams, L. A. et al. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut 66 (6), 1138–1153. https://doi.org/10.1136/gutjnl-2017-313884 (2017).
Targher, G., Marchesini, G. & Byrne, C. D. Risk of type 2 diabetes in patients with non-alcoholic fatty liver disease: causal association or epiphenomenon? Diabetes Metab. 42 (3), 142–156. https://doi.org/10.1016/j.diabet.2016.04.002 (2016).
Hossain, N. et al. Independent predictors of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 7 (11), 1224–1229. https://doi.org/10.1016/j.cgh.2009.06.007 (2009).
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J. Hepatol. 73 (1), 202–209. https://doi.org/10.1016/j.jhep.2020.03.039 (2020).
Loomba, R. et al. Association between diabetes, family history of diabetes, and risk of nonalcoholic steatohepatitis and fibrosis. Hepatology 56 (3), 943–951. https://doi.org/10.1002/hep.25772 (2012). Epub 2012 Jul 26.
Williams, C. D. et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 140 (1), 124–131. https://doi.org/10.1053/j.gastro.2010.09.038 (2011).
Cao, Y. et al. The association between NAFLD and risk of chronic kidney disease: a cross-sectional study. Ther. Adv. Chronic Dis. 12, 20406223211048649. https://doi.org/10.1177/20406223211048649 (2021).
Montemayor, S. et al. Adherence to Mediterranean Diet and NAFLD in patients with metabolic syndrome: the FLIPAN Study. Nutrients 14 (15), 3186. https://doi.org/10.3390/nu14153186 (2022).
Kiwata, J. L. et al. A pilot randomised controlled trial of a periodised resistance training and protein supplementation intervention in prostate cancer survivors on androgen deprivation therapy. BMJ Open. 7 (7), e016910. https://doi.org/10.1136/bmjopen-2017-016910 (2017).
Bjornstad, P. & Eckel, R. H. Pathogenesis of lipid disorders in insulin resistance: a brief review. Curr. Diab Rep. 18 (12), 127. https://doi.org/10.1007/s11892-018-1101-6 (2018).
Sonmez, A. et al. Low- and high-density lipoprotein subclasses in subjects with nonalcoholic fatty liver disease. J. Clin. Lipidol. 9 (4), 576–582. https://doi.org/10.1016/j.jacl.2015.03.010 (2015 Jul-Aug).
Krawczyk, M. et al. Usefulness of the triglycerides to High-Density Lipoprotein Cholesterol ratio (TG/HDL-C) in prediction of metabolic syndrome in Polish obese children and adolescents. Acta Biochim. Pol. 65 (4), 605–611. https://doi.org/10.18388/abp.2018_2649 (2018).
McLaughlin, T. et al. Use of metabolic markers to identify overweight individuals who are insulin resistant. Ann. Intern. Med. 139 (10), 802–809. https://doi.org/10.7326/0003-4819-139-10-200311180-00007 (2003).
Liu, H. et al. Association of the Ratio of Triglycerides to High-Density Lipoprotein Cholesterol Levels with the risk of type 2 diabetes: a retrospective cohort study in Beijing. J. Diabetes Res. 2021, 5524728. https://doi.org/10.1155/2021/5524728 (2021).
Matsuzaka, T. & Shimano, H. New perspective on type 2 diabetes, dyslipidemia and non-alcoholic fatty liver disease. J. Diabetes Investig. 11 (3), 532–534. https://doi.org/10.1111/jdi.13258 (2020).
Kandula, R. & Shegokar, V. E. A study of lipid profile in patients with type-2 diabetes mellitus. MRIMS J. Health Sci. 1, 23. https://doi.org/10.4103/2321-7006.301931 (2013).
Hyassat, D. et al. Dyslipidemia among patients with type 2 diabetes in Jordan: prevalence, pattern, and associated factors. Front. Public. Health. 10, 1002466. https://doi.org/10.3389/fpubh.2022.1002466 (2022).
Mooradian, A. D. Dyslipidemia in type 2 diabetes mellitus. Nat. Clin. Pract. Endocrinol. Metab. 5 (3), 150–159. https://doi.org/10.1038/ncpendmet1066 (2009).
Marx, N. et al. 2023 ESC guidelines for the management of cardiovascular disease in patients with diabetes. Eur. Heart J. 44 (39), 4043–4140. https://doi.org/10.1093/eurheartj/ehad192 (2023).
Acknowledgements
This study was supported by Medical and Technology Project of Zhejiang Province (No. 2021KY890); Zhejiang Traditional Chinese Medicine Scientific Research Fund Project(No. 2022ZB280); Interdisciplinary Research Project of Hangzhou Normal University(No. 2024JCXK05); The funders have no role in the data collection, data analysis, preparation of manuscript and decision to submission. The work was supported by the Key medical disciplines of Hangzhou.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Conceptualization, L.B., P.Z. and M.W; methodology, T.T. and Q.Y.; validation, X.Y.; data curation, S.H., Y.Y., S.Z.and H.W.; writing original draft preparation, L.B.; writing—review and editing, L.B., X.F., J.C., and X.Z.; resources, X.Z. and M.W.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bian, L., Tang, T., Yu, Q. et al. Association between the triglyceride to high-density lipoprotein cholesterol ratio and type 2 diabetes mellitus in non-alcoholic fatty liver disease. Sci Rep 14, 31048 (2024). https://doi.org/10.1038/s41598-024-82116-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-82116-0