Abstract
Pseudomonas aeruginosa is a Gram-negative bacterium that is notorious for airway infections in cystic fibrosis (CF) subjects. Bacterial quorum sensing (QS) coordinates virulence factor expression and biofilm formation at population level. Better understanding of QS in the bacterium-host interaction is required. Here, we set up a new P. aeruginosa infection model, using 2D upper airway nasal organoids that were derived from 3D organoids. Using dual RNA-sequencing, we dissected the interaction between organoid epithelial cells and WT or QS-mutant P. aeruginosa strains. Since only a single healthy individual and a single CF subject were used as donors for the organoids, conclusions about CF-specific effects could not be deduced. However, P. aeruginosa induced epithelial inflammation, whereas QS signaling did not affect the epithelial airway cells. Conversely, the epithelium influenced infection-related processes of P. aeruginosa, including QS-mediated regulation. Comparison of our model with samples from the airways of CF subjects indicated that our model recapitulates important aspects of infection in vivo. Hence, the 2D airway organoid infection model is relevant and may help to reduce the future burden of P. aeruginosa infections in CF.
Similar content being viewed by others
Introduction
Pseudomonas aeruginosa is a Gram-negative opportunistic bacterium, which is known to chronically infect the airways of people with cystic fibrosis (CF). CF is a genetic disorder caused by mutations in the gene coding for the cystic fibrosis transmembrane conductance regulator (CFTR) protein. Mutated CFTR leads to an osmotic misbalance of the epithelial surface in multiple organs1,2,3. However, the airways are most affected due to their obstruction by desiccated mucus, which can lead to pulmonary failure4,5. This CF mucus presents a perfect condition for P. aeruginosa growth6. Because P. aeruginosa has a high intrinsic resistance to antibiotics, infections often become chronic7,8,9,10,11, contributing to the high morbidity and mortality observed in people with CF10.
A growing field of research focuses on quorum sensing (QS) as an alternative target to treat P. aeruginosa infections. Via QS, bacteria regulate a broad range of cellular processes based on their local cell density. QS in Gram-negative bacteria is highly conserved: a LuxI-type synthase produces a signal molecule (an acyl-homoserine lactone (AHL)) that can diffuse across membranes and bind to its cognate LuxR-type receptor, altering the expression of target genes12,13. Thus, when bacterial density is high, the concentration of AHLs increases, inducing downstream processes like biofilm formation and the production of virulence factors12.
P. aeruginosa presents a relatively complex QS network, involving three different systems: two typical LuxI/R systems (las-encoded and rhl-encoded system) and a unique Pseudomonas Quinolone Signal (PQS)-based system. These systems are hierarchical and highly interconnected. The Las system is the QS master regulator that induces the expression of the Rhl and PQS systems14. Importantly, inhibition of QS reduces the toxicity of P. aeruginosa in animal models and leads to faster clearing and prolonged survival of the infected animal15,16,17. However, the exact role of QS in human infection and CF is still underexplored18.
To date, P. aeruginosa CF infection models vary from the study of P. aeruginosa isolates from CF subjects19,20,21 to growing P. aeruginosa in vitro in artificial CF sputum and other bacterial media22,23,24,25,26, using various CF animal models27,28,29, working with ex vivo CF lungs30,31, or co-culture systems using cancer cell lines and primary cells32,33,34,35,36,37. Each of these models present distinct advantages and disadvantages38.
Human airway organoids derived from adult stem cells faithfully resemble the cellular composition and physiology of the airway39. Upper airway nasal epithelial cells are accessible, can be acquired relatively easily and may be expanded indefinitely in 3D under defined culture conditions. Additionally, airway organoids derived from CF subjects capture the molecular characteristics of the disorder and therefore are a useful tool to study CF phenotypes in vitro40. Furthermore, organoid co-cultures have recently been used to investigate the role of bacteria in colorectal cancer41,42. Thus, 3D organoids represent a powerful epithelial source for differentiation experiments in 2D air-liquid interface (ALI) setups. In the current study, we describe a new co-culture method using upper airway nasal 3D organoids - derived from one healthy individual and one CF subject - grown in 2D ALI to study P. aeruginosa infections. By performing dual RNA-seq43, this analysis captures the interaction between the host cells and the bacteria. Additionally, the benchmarking with publicly available datasets from transcriptomes of P. aeruginosa clinical isolates reveals that our model recapitulates key aspects of in vivo infections.
Results
Establishment of 2D airway organoid co-cultures with P. Aeruginosa
We aimed to study the interaction between P. aeruginosa and the airway epithelium during early infection. For this, we used upper airway (nasal) 3D organoid cultures derived from a healthy individual and from a CF individual. Subsequently, we established an epithelial co-culture system composed of organoids cultured in 2D and the well-characterized P. aeruginosa PAO1 strain constitutively expressing GFP. Organoid cultures were differentiated for 1 month in 2D air liquid interface (ALI) (Fig. 1A, Supplementary Fig. 1A). This approach gave rise to a pseudostratified epithelium containing the main cell types of the mature airway epithelium: goblet cells marked by MUC5AC, ciliated cells marked by acetylated tubulin, and basal cells marked by TP63 (Fig. 1B). 2D ALI cultures allow for easy apical exposure to PAO1 bacteria (Fig. 1C). After 14 h of co-culture, bacterial aggregates had formed on the epithelial cells implying that downstream pathways including biofilm formation are active in co-culture (Fig. 1D, E). At this timepoint, the epithelium was still intact (Supplementary Fig. 1B). Longer co-culture time was not feasible due to epithelial cell death caused by the bacteria. Wild type PAO1 cells and PAO1 strains ΔQS (rhlI/lasI knockout) and ΔpqsA (pqsA knockout) that display impaired QS were alive and proliferated during this time span (Fig. 1F).
Co-culture establishment of 2D-airway organoids with P. aeruginosa PAO1. (a) Schematic representation of line establishment, 3D organoid expansion and 2D ALI differentiation. (b) HE staining of the major cell types present in ALI differentiated airway organoids, goblet cells stained by MUC5AC, ciliated cells by acetylated (Ac) tubulin and basal cells by TP63. Scale bar indicates 25 μm (c) Schematic representation of co-culture establishment of PAO1-GFP and differentiated airway organoids. (d) Z projections and (e) cross-section of confocal imaging of the co-culture after 14 h. Red: F-Actin; green: PAO1-GFP; blue: DAPI. Scale bar indicates 10 μm. (f) CFU assay of WT PAO1 bacteria and PAO1 ΔQS and ΔpqsA strains following co-culture with organoids and in liquid medium at time points 0 h and 14 h. The mean of the triplicates was plotted and error bars represent standard error of the mean (SEM). To determine statistical significance between the time points, log-transformed data was analyzed using two-way ANOVA, corrected for multiple comparisons using Sidak’s test (*P < 0.05; **P < 0.005; ****P < 0.0001).
Dual RNA-sequencing of the co-culture model
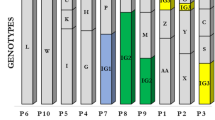
To study the interplay between upper airway epithelial organoids and P. aeruginosa, we subjected the 14 h co-cultures to dual RNA-seq, in order to capture the transcriptomic response of both components. For this, we used organoid lines derived from a healthy donor and from a CF subject and either WT, ΔpqsA or ΔQS PAO1 cells (Fig. 2A). Organoid cultures without bacteria and pure bacterial cultures were used as controls. As an initial step to validate the feasibility of our approach, we performed another bacterial RNA sequencing using only the PAO1-WT strain, both in co-culture and by itself (Supplementary Fig. 1C). We added the samples of this initial step to the analysis of the dual RNA-seq cohort unless otherwise stated. After a two-step mapping approach (Supplementary Fig. 1D), approximately half of the reads from co-culture samples were aligned to the bacterial or human genome, indicating that the dual RNA-seq approach efficiently captured the transcriptome of both components. As expected, the analysis of separately cultured 2D organoids and bacteria yielded almost 100% reads of the corresponding species (Fig. 2B). Therefore, both runs were integrated in one dataset (Supplementary Fig. 1E, F).
Co-culture characterization by Dual RNA-seq. (a) Schematic representation of the Dual RNA-seq experiment. (b) Distribution of human and bacterial reads across the different samples (technical replicates in triplicate) included in the run after performing the mapping and count assignment (as in Supplementary Fig. 1, see Supplementary Table 3). (c) Knock-out validation by gene expression. Normalized counts of pqsA, lasI and rhlI across the different samples of the cohort. Color code indicates culture condition (Green: mono-culture; magenta: co-culture) and PAO1 genotype (Dark: WT; middle: ΔpqsA; light: ΔQS). (d) PCA plot of PAO1 samples. (e) PCA plot of 2D organoid samples. Color code indicates PAO1 genotype, culture condition (co-culture or mono-culture) and organoid genotype (Healthy or CF).
We first validated the differential expression of the bacterial KO genes in the bacterial strains. As expected, the PAO1 ΔpqsA strain showed inhibition of pqsA, while not affecting lasI and rhlI. PAO1 ΔQS showed inhibition of all three QS pathways, including inhibition of pqsA due to the hierarchical QS system in P. aeruginosa PAO1 (Fig. 2C). These three strains allowed us to study and compare the effect of QS and of the PQS system in co-culture. Comparison of the PAO1 transcriptomes showed a major difference between PAO1 cells grown in mono-culture and in co-culture with organoids (Fig. 2D). The effect of ΔQS was also evident in co-culture and in bacterial mono-culture (Fig. 2D). However, ΔpqsA did not show a marked transcriptional change, other than pqsA expression itself, compared to the corresponding WT bacterial culture (either mono- or co-culture) (Fig. 2D). RNA expression of the organoids from the healthy donor and CF individual clearly segregated (Fig. 2E). However, since our analysis included only one healthy and one CF organoid line, conclusions about CF-specific effects of PAO1 cannot be drawn. Nevertheless, both organoid lines showed the potential for transcriptional response to the presence of PAO1 irrespectively of the bacterial genotype (Fig. 2E).
P. Aeruginosa induces epithelial inflammation
Next, we focused on the effect induced by the different PAO1 strains on the 2D organoid cultures from a healthy individual and from a CF individual (Fig. 3A). PAO1 WT and PAO1 ΔQS elicited a highly similar response (Fig. 3B). Coculture with PAO1 cells led to upregulation of 1610 genes in 2D organoids and downregulation of 638 genes. (Fig. 3C). For both healthy and CF 2D organoids, these changes reflected pathways involved in response to lipopolysaccharides (LPS), inflammatory response or cellular response to biotic stimulus, including genes like IL1A/B, TNFA, and various CXCL chemokines (Fig. 3D and E, Supplementary Fig. 2A, B). Whereas previous studies have shown that QS molecules affect epithelial cells44,45,46, no clear QS-derived effect was observed when organoids were exposed to PAO1 WT compared to ΔpqsA and ΔQS strains (Fig. 3B). Since the ΔpqsA and ΔQS strains lack expression of some or most QS signaling molecules, this observation contrasted with a previous report suggesting that the epithelium can sense and respond to QS molecules44. The response to LPS appeared to be reduced in CF organoids, compared to healthy organoids (Fig. 3E), but since our dataset is comprised of a single healthy and a single CF organoid line, general conclusions about disease-specific effects are not possible.
Transcriptional response of the epithelium to infection with the different PAO1 strains. (a) Schematic representation of the analysis. (b) Volcano plot showing the log2 fold change and -log10 adjusted p-value of all genes, when comparing the transcriptome of 2D organoids exposed to PAO1 WT or PAO1 ΔQS. (c) Volcano plot showing the Log2 fold change and -log10 adjusted p-value per gene comparing the transcriptome of 2D organoids exposed to PAO1 WT or unexposed controls. Green indicates differentially expressed genes (DEGs) (log2 fold change > 1 and adjusted p value < 0.05). (d) Gene ontology enrichment analysis showing top 10 categories enriched in 2D organoids exposed to PAO1 WT. Left panel: Healthy organoid line. Right: CF organoid line. (e) Gene expression heat map of genes from “Response to lipopolysaccharide” GO term category (GO:0032496). Color code indicates culture condition (co-culture or mono-culture) and PAO1 genotype (WT, ΔpqsA or ΔQS). Heatmaps were plotted using the pheatmap function of DESeq279 (version 1.36.0) in Rstudio.
The epithelium induces broad metabolic differences in P. Aeruginosa transcription
We next focused on the effect of the organoids on P. aeruginosa (Fig. 4A). Comparing the gene expression profile of PAO1 grown in co-culture versus mono-culture revealed a total of 2215 differentially expressed genes (DEGs) (979 upregulated in co-culture; 1136 upregulated in mono-culture) (Fig. 4B). Gene ontology enrichment analysis of these genes revealed broad metabolic differences between the two culture modes. Genes involved in iron acquisition (e.g., siderophore and pyoverdine processes) showed higher expression in pure bacterial cultures (Supplementary Fig. 3A). This contrasted with what has been observed in human infections19,47, but was in agreement with previous co-culture attempts35.
Transcriptional response of PAO1 to the presence of airway epithelium. (a) Schematic representation of the analysis. (b) Volcano plot displaying the Log2 fold change and –log10 adjusted p-value of all genes, when comparing the PAO1 transcriptomes of co-culture and bacterial mono-culture samples. Green indicates differentially expressed genes (DEGs) (log2 fold change > 1 and adjusted p value < 0.05). The number of genes upregulated in co-culture and bacterial mono-culture is indicated. (c) Gene ontology enrichment analysis showing top 10 categories enriched in PAO1 exposed to airway epithelium in co-culture. (d) Normalized count plots of genes involved in CCR pathway, crc and crcZ. (e) KEGG pathway pae00910 plot displaying the log2 fold change of genes involved in denitrification91. DEGs from co-culture vs. bacterial culture mono-culture comparison of PAO1 transcriptomes. (f) Normalized count plots of genes involved in P. aeruginosa antibiotic resistance. (g) Heat map displaying expression of genes involved in P. aeruginosa T6SS. Genes grouped by H1, H2 or H3 T6SS subtype50,85. Samples grouped by culture condition. Color code indicates culture condition (Green: bacterial mono-culture; magenta: co-culture) and PAO1 genotype (Dark: WT; middle: ΔpqsA; light: ΔQS). Heatmaps were plotted using the pheatmap function of DESeq279 (version 1.36.0) in Rstudio.
PAO1 cells co-cultured with airway cells increased their expression of genes related to peptide, glycolipid and amide biosynthetic pathways (Fig. 4C), suggesting major metabolic rearrangements. Interestingly, co-cultured PAO1 cells presented increased crc and decreased crcZ levels (Fig. 4D), two main regulators of the carbon catabolite repression (CCR) pathway48,49. This pathway is central to the hierarchical utilization of preferred carbon sources by P. aeruginosa. This finding suggested that the epithelium provides a source of preferred nutrients compared to the medium alone. Interestingly, expression change was observed in only a subset of genes known to be regulated by the CCR pathway (Supplementary Fig. 3B).
Another important aspect of P. aeruginosa infection of individuals with CF is its ability to perform denitrification50. This mechanism enables the utilization of nitrogenous oxides (nitrate, nitrite, and nitrous oxide) as electron acceptor for respiratory growth in anoxic conditions, such as during the course of infection51. We found that co-cultured PAO1 expressed increased levels of many genes involved in nitrogen metabolism (Supplementary Fig. 3C), and particularly those used in denitrification (Fig. 4E). This suggests that there is local anoxia due to the oxygen consumption by the epithelium and high-density bacterial population, which is similar as observed in airway infections6,52. Beyond metabolism, the bacteria also showed elevated levels of genes involved in resistance to antibiotics (Supplementary Fig. 3D). Particularly striking was the effect of the epithelium on genes encoding the MexXY efflux pump, porins, and genes like aph, PA5514, arnA and PA2528 encoding antibiotic degrading enzymes (Fig. 4F and Supplementary Fig. 3E). Of note, our co-culture system is performed in antibiotic-free conditions. Finally, the presence of epithelial cells induced the expression of type 3 (Supplementary Fig. 3F) and type 6 (Fig. 4G) secretion systems (T3SS and T6SS). These bacterial secretion systems are syringe-like structures used to inject toxins into the cytoplasm of target cells53,54,55,56. The epithelium mainly induced the expression of the H2-T6SS, and to a lesser extent H1-T6SS, but it repressed those belonging to the H3-T6SS subtype. H1 and H2 subtypes are known to act against other prokaryotes and eukaryotes, respectively53,57. Little is known about the role and regulation of H3-T6SS in infection.
The epithelium influences aspects of P. Aeruginosa QS regulation
Next, we investigated how the presence of the epithelium affected QS-regulated processes in P. aeruginosa PAO1. Since only the dual RNA-seq run contained samples from all three bacterial conditions (WT, ΔpqsA, and ΔQS), only samples from this run were included in the analysis to avoid batch-induced bias. In general, LasR- and RhlR-regulated genes and three out of eight of the PQS-regulated genes were downregulated in PAO1 WT co-culture conditions compared to bacterial mono-cultures (Fig. 5A). This correlates with previous descriptions of stronger QS-induced responses in pure bacterial cultures than in clinical infections19,52,58. Interestingly, the QS receptor levels (mvfR, lasR and rhlR) seemed to be more affected by ΔQS when the bacteria were co-cultured with the epithelium than in mono-culture. This could impact the QS regulatory network and therefore it is worth taking into consideration when interpreting results of QS regulation using in vitro models. Only 8 and 10 DEGs were found when comparing WT PAO1 with ΔpqsA in co-culture and in mono-culture respectively (Supplementary Fig. 4A-B). From these, the antABC operon was affected only in mono-culture (Supplementary Fig. 4C). This operon encodes the enzymes responsible for derivatizing the PqsA substrate anthranillic acid to catechol, before degradation to intermediates of the tricarboxylic acid (TCA) cycle59. The loss of PqsA in the ΔpqsA strain could lead to an accumulation of anthranillic acid. Via upregulation of antABC in bacterial mono-cultures, anthranillic acid might be used as a nutrient.
Epithelial effect on PAO1 QS regulation. (a) Gene expression heat map of genes involved in PQS, Las or Rhl QS pathways. (b) Volcano plots displaying gene log2 fold change and –log10 adjusted p-value when comparing the transcriptomes of WT and ΔpqsA PAO1 to those of ΔQS in co-culture (top) and in pure bacterial cultures (bottom). Venn diagrams display the overlap between genes up (right) and downregulated (left) in the comparisons. (c) Gene ontology enrichment analysis showing top 10 categories enriched in genes that are specifically upregulated in co-culture in WT and ΔpqsA PAO1 transcriptomes compared to ΔQS. (d) Gene expression heat map showing top 50 co-culture-specific DEGs. Genes are color-coded according to the following categories (Yellow: T6SS; purple: T2SS; green: Leucine metabolism; red: other pathways). (e) Gene expression heat map of T6SS eukaryotic and prokaryotic effectors. Sample color code indicates culture condition (Green: bacterial culture mono-culture; magenta: co-culture) and PAO1 genotype (Dark: WT; middle: ΔpqsA; light: ΔQS). Heatmaps were plotted using the pheatmap function of DESeq229 (version 1.36.0) in Rstudio.
In contrast, deletion of rhlI and lasI in ΔQS led to 308 and 465 DEGs in co-culture and in mono-culture, respectively (Fig. 5B). In order to dissect which QS-regulated processes were affected by the epithelium, we identified DEGs that occurred specifically in co-culture (52 up and 75 downregulated). Iron uptake pathways were downregulated only in ΔQS co-culture condition (Supplementary Fig. 4D). This highlighted the differences of the two culture systems regarding iron utilization by the bacteria. On the other hand, genes involved in leucine and tyrosine catabolism were upregulated (Fig. 5C-D). The amino acid utilization by P. aeruginosa is thought to be a key element of P. aeruginosa adaptation to the human airways, since amino acid auxotrophy is common in CF clinical isolates. This could explain why the QS effect is not observed in isolated bacterial cultures60. Furthermore, we found genes regulated by QS specifically in co-culture involved in bacterial adhesion and biofilm formation (pprB), and phosphatase and phosphodiesterase activities (eddA)61,62. Additionally, a number of T2SS and T6SS related genes (Fig. 5C-D) were specifically regulated by QS in co-culture. T2SS-related genes from WT PAO1 in co-culture showed slightly reduced levels compared to mono-culture. In contrast, QS mutants in co-culture showed a greatly reduced expression of T2SS-related genes. This suggested that the epithelium potentially inhibits T2SS, which can be counteracted by QS-regulated molecules in WT bacteria. The expression of T6SS-related genes was low in all PAO1 strains in mono-culture. Co-culture conditions specifically showed a QS-regulatory effect on the expression of these genes. This suggested that a combination of epithelial and QS factors induce the expression of some T6SS genes. In addition, T6SS effectors that are involved in pathogenicity of eukaryotic cells were both induced by a combination of epithelial and QS signals (Fig. 5E).
Benchmarking 2D co-culture model with chronic clinical samples
We addressed which aspects from in vivo P. aeruginosa infections were recapitulated in our 2D co-culture model, and how it compares to published co-culture models using primary airway cells. For this, we used a quantitative framework, previously established by Cornforth et al.63 Using this framework, the transcriptional profiles of PAO1 in our model were compared to PAO1 samples from CF sputum samples by comparison of our accuracy scores to the scores found in a recent paper by Lewin et al.64. Our co-culture model led to the accurate expression of more than 90% of the genes relative to the CF environment, comparable to what was observed in co-culture models using primary cells (Fig. 6A). Additionally, mono-cultures presented reduced accuracy, highlighting the importance of a human-pathogen co-culture model to mimic the in vivo infection.
Benchmarking co-culture model with in vivo P. aeruginosa transcriptomic datasets directly isolated from the airways of CF subjects. (a) Accuracy analysis using gene-wise mean and standard deviation values from in vivo samples in Lewin et al., 202358 as reference. Genes were considered accurate if their expression was within 2 standard deviations of the mean in the in vivo sample. (b) PCA plots showing sample distribution by condition (Magenta: co-culture; green: bacterial culture in isolates; purple: in vivo) or by study of origin (Orange: this study; purple: Cornforth et al., 201819; pink: Kordes et al., 201959; blue: Rossi et al., 201849). (c) Volcano plots displaying gene log2 fold change and -log10 adjusted p-value comparing transcriptomes of in vivo P. aeruginosa (left) or co-cultured PAO1 (right) to those of all pure bacterial culture samples. Green indicates differentially expressed genes (DEGs) (log2 fold change > 1 and adjusted p value < 0.05). Indicated in the boxes the number of up- or downregulated DEGs. (d) Venn diagrams displaying the overlap between genes that are upregulated (left), downregulated (middle), or both (right) in the previous in vivo and co-culture comparison to in vitro and mono-culture samples (b). (e) Expression heat map displaying the common up-(left) and downregulated (right) genes. Samples clustered based on the expression of all genes plotted per heat map. Color-code indicates condition (Magenta: co-culture; green: pure bacteria; purple: in vivo) and study of origin (Orange: this study; purple: Cornforth et al., 2018; pink: Kordes et al., 2019; blue: Rossi et al., 2018). Heatmaps were plotted using the pheatmap function of DESeq279 (version 1.36.0) in Rstudio. (f) Protein-protein interaction network of common DEGs (in vivo and co-culture. Each node represents a protein encoded by a DEG. Edges represent known protein-protein association (either physical or functional) with a confidence level higher than 0.7. Node color represent clusters generated MCL method. Highlighted the pathway to which the cluster proteins belong. (g) Log2 normalized count plots of representative genes from pathways highlighted by the network analysis. Color-code indicates Magenta: co-culture, green: pure bacteria and purple: in vivo.
Next, we compared the transcriptional profiles of clinical P. aeruginosa strains directly isolated from airway biopsies from CF subjects to the PAO1 co-culture samples. Pure bacterial culture samples from this and other studies were included in the comparison19,52,65 (Supplementary Fig. 5). After dataset integration, PCA analysis revealed that the origin of the bacterial samples (in vivo, co-culture, or mono-culture) explained the clustering of the samples best (Fig. 6B), in line with what was observed in the accuracy analysis (Fig. 6A). The comparison of the in vivo and co-culture transcriptomes to all mono-culture samples revealed a total of 1382 and 2045 DEGs, respectively (Fig. 6C). Despite the fact that our co-culture represented an early stage of infection compared to the chronic state of the clinical samples, 268 genes were common between both comparisons (4.7% of all PAO1 genes) (Fig. 6D-E). This core gene signature captured the aspects of an in vivo infection present in our co-culture model. In order to understand pathways enriched in this core gene signature, we performed protein-protein interaction network analysis (Fig. 6F). This confirmed that denitrification is an important process for P. aeruginosa infection and that this was captured by our model (Figs. 4E and 6F-G and Supplementary Fig. 6). Increased expression of mexYX antibiotic efflux pump (Figs. 4F and 6F-G, Supplementary Fig. 6) was also confirmed in vivo. Additionally, the expression of some T2SS proteins (Fig. 6F-G, Supplementary Fig. 6) was reduced in the core signature compared to in vitro cultures, which is in line with our previous analysis (Fig. 5D).
Beyond confirming the relevance of some of the pathways previously discovered by our cohort, the comparative analysis (Fig. 6) uncovered other processes relevant for in vivo infection. This included elevated levels of choline/betaine metabolic genes (betABI), responsible for the production of glycine-betaine (GB) (Fig. 6F-G, Supplementary Fig. 6). The accumulation of GB has been proposed as a bacterial osmo-protective mechanism52, and to be important in P. aeruginosa infection in mice66. Additionally, our 2D co-culture model captured the reduced levels of motility- and chemotaxis-related genes that are observed in vivo compared to pure bacterial cultures (Fig. 6F-G, Supplementary Fig. 6), which is another important aspect for biofilm formation.
Discussion
In this study, we describe a novel P. aeruginosa co-culture system using 2D human airway organoids derived from one healthy donor and one CF individual. Subjecting the co-culture to dual RNA-seq allowed us to gain insight into how both components interact with, and respond to each other, focusing on the role of QS molecules and downstream signaling. Finally, we benchmarked our findings with a cohort of publicly available RNA-seq datasets from clinical samples of P. aeruginosa infected airways. Our model accurately resembles the expression patterns of more than 90% of the genes compared to clinical CF sputum samples. In addition, our co-culture model recapitulates metabolic aspects, CCR and nitrogen usage, as well as the expression of several secretion systems, important for P. aeruginosa persistence and virulence. Furthermore, the upregulation of genes involved in P. aeruginosa antibiotic resistance could be of particular relevance for research of bacterial mechanisms of antibiotic resistance and discovery of novel antibacterial compounds. This is highly relevant in the case of P. aeruginosa due to its high intrinsic resistance11. Since it is not possible to study early stages of infection using clinical isolates, our model offers a tool to understand the initial steps of the infectious process in near-physiological conditions.
Previous attempts to co-culture P. aeruginosa in 2D have been performed using cancer cell lines32,33,34,35,36,67,68 or primary human airway cultures34,37, which were also focused on the epithelial-bacteria interaction and QS37. In contrast to cancer cell lines, primary airway epithelial cultures are non-transformed and thus are a better representation of epithelial biology. However, they present a limited expansion ability and are normally cultured in undefined media conditions, with the addition of serum or the presence of feeder layers34. In comparison to both systems, 3D organoids are non-transformed and can be expanded indefinitely under defined culture conditions. This makes organoids an ideal source of biomass to differentiate the organoid cells in 2D ALI culture methods. In contrast to pseudostratified primary epithelia grown in ALI, the expansion potential of organoids allows for longitudinal replicate experiments using a defined and constant biological sample. Additionally, this expansion potential will enable P. aeruginosa co-culture with genetically engineered organoid lines and isogenic wild type controls, once genome editing of airway organoids becomes efficient enough to perform experiments at this scale69. This will open the door to understanding which epithelial factors shape the course of P. aeruginosa infection and how to harness them to fight the infection.
In this dataset, we do not observe a major organoid response specific to QS pathways. Using live co-cultures could lead to lower effective concentrations of QS-induced molecules, compared to what has been used in studies testing the effect of single QS compounds on epithelial cells70,71. In addition, the strong LPS-induced inflammation, present in all conditions, might abrogate the effect of QS-derived molecules. Particularly, LPS is not accounted for in studies that solely focus on QS-derived molecules. It is likely that only specific cell types respond to QS molecules, i.e. chemosensory tuft cells72,73, and therefore bulk RNAseq would not allow the study of these cell-specific effects. Additionally, previous reports have also shown that co-culture with PAO1-WT strain induces slightly less inflammation in organoids compared with QS deficient PAO1 strains34. This difference compared to our results could be a result of the different co-culture timespans (14 h in this study compared to 24 h), the different MOI used at the start of the experiment and/or the different epithelial culture systems.
A limitation of the present study is that organoids from only a single healthy donor and a single CF individual were used. Future studies using a larger number of biological replicates per disease condition will enable to study CF-specific aspects of the infection process. Additionally, future expansion of the co-culture infection models, with the addition of immune cells, will yield insight into how this important aspect affects the behavior of the P. aeruginosa infections. Importantly, co-culture models that recapitulate a more complex tissue architecture74 will also help to understand biofilm formation under more physiological conditions. Furthermore, QS pathways coordinate the population-scale behavior of individual bacteria, which leads to the functional and spatial heterogeneity found in bacterial biofilms. The recent application of spatial transcriptomics to P. aeruginosa biofilms grown on solid surfaces have allowed detailed study of these two aspects75,76. It will be very interesting to address this spatial and functional heterogeneity in the presence of the epithelial and immune cells using co-cultures. Furthermore, our 14 h co-culture system represents an early stage of the infectious process. While this time span allows studying QS regulation, it is too short to focus on biofilm development and other aspects of chronic infections. Longer incubation using our method was technically challenging due epithelial damage caused by the bacterial cells. Developing co-culture strategies that enable sustained chronic infection of the mucosa will help to investigate these aspects of later infection stages.
In conclusion, 2D organoid co-cultures with P. aeruginosa represent a new development of the current methods to study host-bacterium interplay. The system recapitulates major infection traits from both bacteria and epithelium, including bacterial metabolism, expression of virulence factors and the induction of an inflammatory response in the epithelium.
Materials and methods
Bacterial strains and growth conditions
For this study, we used P. aeruginosa PAO1 strains, which constitutively express GFP. Stocks were stored in -80 °C in 20% glycerol solutions. PAO1 strains were plated on Luria agar (LA) at 37 °C and grown in medium specific for the assay. E. coli RHO3 strains were used for conjugation and medium was supplemented with 400 µg/mL 2,6-Diaminopimelic acid (Sigma-Aldrich, Merck Life Science, Amsterdam, The Netherlands) to support growth. The PAO1 ΔpqsA strain has been described before77. The PAO1 ΔlasI/ΔrhlI strain was generated using allelic exchange following the method described before78. For the generation of the mutants we inserted upstream (using UP.Fw and UP.Rv primers) and downstream (using DN.Fw and DN.Rv primers) regions of the gene of interest in pEX18Gm plasmids using Gibson assembly restriction cloning, using the restriction enzymes SacI and Sph1 (Primers and plasmids are listed in Supplementary Tables 1 and 2). After Gibson assembly, the plasmid was transformed into RHO3 E. coli donor strains before conjugation via puddle mating with PAO1 GFP strain. Mutant colonies were identified with colony PCR (using seq.FW and seq.Rv primers) and confirmed by sequencing (performed by Macrogen Europe BV).
Primary nasal epithelial cell lines establishment and initial 2D expansion
Nasal brushing-derived epithelial stem cells were collected and stored with informed consent of all donor and was approved by a specific ethical board for the use of biobanked materials TcBIO (Toetsingscommissie Biobanks), an institutional Medical Research Ethics Committee of the University Medical Center Utrecht (protocol ID: 16/586). All research was performed in accordance with relevant guidelines/regulations. Nasal epithelial stem cells isolation and initial expansion was performed in 2D as previously described in detail79,80. Briefly, nasal brush was initially dissociated by repeated pipetting using a sterile P1000 tip with the top cut off. Then, the cell suspension was centrifuged (400 g for 5 min) and the pellet was resuspended in TrypLE express enzyme79,80, supplemented with 1× Sputolysin (Calbiochem). Cell suspension was incubated at 37 ºC for 10 min, passed through a 100 μm strainer and the flow through centrifuged (400 g for 5 min). Cells were seeded in six-well plates coated with collagen IV (50 µg/ml) (Sigma-Aldrich). At this stage, cells were resuspended in isolation medium and seeded. Isolation medium was composed of 50% v/v Bronchial epithelial cell medium-basal (BEpiCM-b) (ScienCell), 23.5% v/v Advanced DMEM F12, 1% v/v B27 Supplement, 1% v/v GlutaMAX supplement, 10 mM HEPES (all from Thermo Fisher Scientific), 0.5 µg/ml (±)-Epinephrine hydrochloride, 0.5 µg/ml Hydrocortisone, 100nM 3,3′,5-Triiodo-L-thyronine sodium salt, 1.25mM N-acetyl-l-cysteine, 5mM Nicotinamide, 500nM SB202190 (p38i) (all from Sigma-Aldrich), 1 µM DMH-1 (BMPi) (Selleck Chemicals), 1µM A83-01 (TGF-βi) (Tocris), 5µM Y-27,632 (ROCKi) (Selleck Chemicals), recombinant human FGF7 (25 ng/ml), FGF10 (100 ng/ml), EGF(5 ng/ml) and HGF (25 ng/ml) (all from PeproTech), 20% v/v Rspondin1 conditioned medium (produced via the r-PEX protein expression platform at U-Protein Express BV), 1% v/v Penicilin-Streptomycin (Thermo Fisher Scientific), 100 µg/ml primocin (InvivoGen), 250 µg/ml Amphotericin B (Thermo Fisher Scientific), 50 µg/ml Gentamycin and 50 µg/ml Vancomycin (Both from Sigma-Aldrich).
After 7 days, isolation medium was exchanged with 2D expansion medium. Expansion medium is similar to isolation medium with the exception of the lack Amphotericin B, Gentamicin and Vancomycin, and the addition of 5µg/ml Notch inhibitor DAPT (Thermo Fisher Scientific). When at 90% confluency, cells were detached from the plate using TrypLE, and 2 × 105 or 5 × 105 cells were reseeded in 12-well or 6-well plate, respectively. Plates were precoated with 50 µg/ml collagen IV. This expansion step was performed until passage 2.
Nasal epithelial organoid expansion
After initial expansion in 2D, nasal cells were expanded indefinitely as 3D organoids as previously described39. In brief, organoids were cultured in organoid expansion medium containing Advanced DMEM F12, 1X GlutaMax (Life Technologies), 10mM HEPES (Life Technologies) (AdvDMEMF12++), supplemented with penicillin and streptomycin (10,000 IU/ml each; Life Technologies) 1× B27 supplement (Life Technologies), 1.25 mM N-acetyl-l-cysteine (Sigma-Aldrich), 10 mM nicotinamide (Sigma-Aldrich), 500 nM A83-01 (Tocris), 5 µM Y‐27,632 (Abmole), 1 µM SB202190 (Sigma-Aldrich), 100 ng/ml human FGF10 (PeproTech), 25 ng/ml FGF7 (PeproTech), 1% (vol/vol) RSPO3, and Noggin (produced via the r-PEX protein expression platform at U-Protein Express BV). For its passage, organoids were collected, washed and resuspended in TrypLE (Gibco) and incubated at 37 °C for 15 min. Then, organoids were mechanically disrupted into single cells and plated in droplets of Cultrex growth factor reduced BME type 2 (Biotechne | R&D systems).
Organoid cell differentiation in 2D air-liquid interface cultures
For the 2D culture of airway organoids, 105 cells were seeded into 24-well polystyrene membranes (Greiner Bio-One) and cultured for one week in organoid expansion medium in both top and bottom compartments until confluency. After confluency, cells were differentiated in air liquid interface during 1 month using PneumaCult™-ALI Medium (Stem cell technologies) supplemented with Hydrocortisone stock solution (5 µl/ml; Stem cell technologies) and Heparin solution (2 µl/ml; Stem cell technologies).
2D airway organoid -Pseudomonas aeruginosa co-culture
Bacterial colonies were picked and grown in DMEM medium (ThermoFisher Scientific), supplemented with 10mM HEPES (ThermoFisher Scientific) and 1X GlutaMAX (ThermoFisher Scientific) until an OD600 = 0.35–0.45. 1 mL of early log-phase bacterial culture was taken and centrifuged for 3 min at 15,000 g, before washing once with PBS. Bacterial cells were pelleted again and resuspended in AdvDMEMF12++ (without antibiotics) to normalize to OD600 = 0.4. Bacteria were diluted 100 x in the same medium before adding 50 µL to the organoids. Organoids in transwells were washed three times in AdvDMEMF12++ (without antibiotics) before addition of the bacteria. Co-cultures were incubated at 37 °C with 5% CO2 for 14 h. Parallel organoid transwells without bacteria were used as controls. The epithelial cells were checked for damage using the fluorescent EVOS FL Auto 2 microscope (ThermoFisher Scientific) at 14 h. Damaged co-cultures with disrupted epithelial integrity were readily detected by brightfield imaging and translocation of fluorescent bacteria to the basal side of the epithelium (Supplementary Fig. 1B). These wells were excluded from further analysis. We observed some variability in the number of bacteria that were added to the apical side of the transwell. The bacterial CFUs were determined immediately following addition to the wells with organoids (co-cultures), or in liquid medium as a control. The number of bacteria varied from 0.5 to 2.5 × 105 CFU/ well (Fig. 1F). The number of eukaryotic cells varied from 1.0 to 1.5 × 106 cells per well, indicating a multiplicity of infection (MOI) varying between 0.033 and 0.25.
Imaging of organoid 2D cultures and PAO1-GFP co-culture
Organoid 2D culture and PAO1 co-cultures were fixed with 4% formaldehyde for 2 h at room temperature. Then, 2D cultures were processed for immunohistochemistry following standard techniques and embedded in paraffin. After sectioning, hematoxicilin/eosin staining was performed according to manufacturer instructions. After blocking, the used primary antibodies included anti-MUC5AC (Thermo), anti-acetylated Tubulin (SantaCruz) and anti-P63 (Abcam). Co-cultures were processed for wholemount immunofluorescence imaging using standard techniques41. Then, co-culture was stained with Phalloidin Atto-647 and DAPI and imaged with SP8 confocal microscope (Leica).
Colony forming unit (CFU) test
For the Colony forming unit test, organoid infection protocol was followed as described before. For time point 0 h, plates were incubated for only 5 min. For time point 14 h, plates were incubated 14 h. After incubation, 50 µL of 0.5% saponin was added to the wells and incubated for 10 min at room temperature. Then, the volume was resuspended and transferred to Eppendorf tubes before centrifugation for 10 min at 15,000 g. Supernatant was aspirated and pellets were resuspended in PBS before making 10-fold dilutions. 5 µL of the dilutions were plated on tryptic soy agar and plates were incubated overnight at 34 °C before the colonies were counted.
RNA isolation
RNA was isolated from the cultures using the MasterPure Complete DNA and RNA Purification Kit (Immunosource, Belgium) following manufacturer instructions. This kit includes a lysis step and corresponding lysis buffer. RNA was collected via precipitation. To remove all the gDNA, two additional rounds of DNase treatment were performed using TURBO DNase (ThermoFisher Scientific) following manufacturer’s protocol. RNA was subsequently isolated again using the MasterPure RNA isolation kit and the RNA was dissolved in dionized water and stored at -80 °C until further use. For RNA-sequencing, RNA libraries were validated with Agilent 2100 bioanalyzer. Samples were sent for sequencing to the Utrecht Sequencing Facility (Useq), for library preparation using Truseq RNA stranded ribo-zero. RNAseq was performed using the Illumina NextSeq2000 platform (50 base pairs, paired-end reads).
Mapping of raw-reads to the genome
To analyze the dataset, a variety of bioinformatics tools were used and we followed a similar protocol as described before, with minor modifications (Supplementary Fig. 1)81. First, the reads were mapped to the human genome (hg19) using STAR mapping software82. Unmapped reads were written into a new FastQ-file. Gene counts were assigned to the mapped reads using FeatureCounts83. Unmapped reads were then mapped against the PAO1 genome (NCBI: txid208964)82,84,85. Gene counts were again assigned using FeatureCounts. The code for this pipeline is available on Github (https://github.com/GJFvanSon/Hubrecht_clevers.git).
Bioinformatic analysis
Human and PAO1 count tables were independently analyzed using DESeq286. DEGs were calculated using the lfcShrink function with argument type set to “apglm”. Volcano plots were generated using EnhancedVolcano package87. Heatmaps were plotted using the pheatmap function of DESeq2 with clutmethod set to average or to complete. For the human dataset, GO enrichment analysis was performed using the function enrichGO() from the package clusterProfiler()88 with arguments OrgDb = org.Hs.eg.db, ont=“BP”, pAdjMethod=“fdr”, minGSSize=“1”, maxGSSize=“2000”, qvalueCutoff= “0.05” and readable=“TRUE”. For PAO1 dataset, GO enrichment analysis was performed using the online tool PANTHER 17.0, with the following settings: analysis type: PANTHER overrepresentation test (Released 20221013), annotation version and release date: GO ontology database DOI: https://doi.org/10.5281/zenodo.6799722 released 2022-07-01, reference list: Pseudomonas aeruginosa (all genes in database), annotation data set: GO biological process complete, test type: Fisher’s exact, correction: calculate false discovery rate. KEGG pathway was generated using the Pathview R package. Pseudomonas category, antimicrobial resistance gene list and GO gene lists were downloaded from Pseudomonas Genome DB version 21.1 (2022-11-20)89. PCA were plotted using the DESeq2 function plotPCA().PCA plots of publicly available in vivo datasets, bacteria-only and co-culture samples were performed on VST-normalized counts integrated using the removeBatchEffect() function of the limma package.(version 3.52.2). ntop parameter was set to 1500 for PCA of in vivo and in vitro sample integration. Protein-protein association network analysis was performed using the STRING v11 online tool90. Common genes with a log2Foldchange / logSE > |4| were used as input. The input parameters were set as follow: Organism = “Pseudomonas aeruginosa PAO1”, Network Type = “full string network”, Required score = “high confidence (0.700)”, and FDR stringency = “medium (5%)”. MCL clustering was performed on the resulting network using the following parameters: inflation parameter = “3”, and edges between clusters = “Don’t show”.
Accuracy analysis was performed according to the description in Lewin et al., 202357,58. All the in vivo and co-culture (combined) raw counts from Lewin et al., 2023 were mapped following the pipeline described in this manuscript. VST normalization was performed on all samples together in DESeq2 with blind = TRUE. First, normalized counts from the in vivo sputum samples from Lewin et al., 2023 were used to determine the mean gene expression and standard deviation of the 5123 core genes in Lewin et al., 2023 present in our dataset58. Then, the accuracy of each model was calculated by determining the percentage of core genes having an expression level within ± 2 standard deviations of the in vivo samples mean expression.
Relevant sequencing datasets associated with Figs. 2, 3, 4, 5 and 6 are provided in Supplementary Tables 3–7.
Data availability
Raw sequencing data from samples containing human material are deposited and available at time of publication under controlled access at The European Genome-phenome Archive (EGA) (https://ega-archive.org/); accession code EGAS00001007463. The data release process can be initiated through the EGA website (https://ega-archive.org/access/request-data/how-to-request-data/). Due to privacy laws, data will be available following approval by Data Access Committee (DAC). JdH can be reached for data upon request (j.denhertog@hubrecht.eu). Raw bacteria-only sequencing samples are deposited and publicly available at time of publication at NCBI GEO database (https://www.ncbi.nlm.nih.gov/geo/) under accession code GSE240500 (token: ohmtekmahdcxbyh).
References
Malhotra, S., Hayes, D. & Wozniak, D. J. Cystic fibrosis and Pseudomonas aeruginosa: the host-microbe interface. Clin. Microbiol. Rev. 32, 1–46 (2019).
Quinton, P. M. Cystic fibrosis: Impaired bicarbonate secretion and mucoviscidosis. Lancet 372, 415–417 (2008).
Kunzelmann, K., Schreiber, R. & Hadorn, H. B. Bicarbonate in cystic fibrosis. J. Cyst. Fibros. 16, 653–662 (2017).
Forbes, E. & Abu-Sbaih, R. Cystic fibrosis. Nat. Rev. Dis. Primers. https://doi.org/10.1038/nrdp.2015.49 (2015).
De Boeck, K. Cystic fibrosis in the year 2020: A disease with a new face. Acta Paediatr. Int. J. Paediatrics. 109, 893–899 (2020).
Rossi, E. et al. Pseudomonas aeruginosa adaptation and evolution in patients with cystic fibrosis. Nat. Rev. Microbiol. 19, 331–342 (2021).
LiPuma, J. J. The changing microbial epidemiology in cystic fibrosis. Clin. Microbiol. Rev. 23, 299–323 (2010).
Fischer, A. J. et al. Sustained coinfections with Staphylococcus aureus and Pseudomonas aeruginosa in cystic fibrosis. Am. J. Respir Crit. Care Med. 203, 328–338 (2021).
Foundation, C. F. Cystic Fibrosis Foundation Patient Registry, 2021 Annual Data Report. Cyst. Fibros. Foundation Publications (2022).
Parkins, M. D., Somayaji, R. & Waters, V. J. Epidemiology, biology, and impact of clonal Pseudomonas aeruginosa infections in cystic fibrosis. Clin. Microbiol. Rev. 31, (2018).
Botelho, J., Grosso, F. & Peixe, L. Antibiotic resistance in Pseudomonas aeruginosa – mechanisms, epidemiology and evolution. Drug Resist. Updates. 44, 100640 (2019).
Bassler, B. L. & Losick, R. Bacterially Speaking Cell. 125, 237–246 (2006).
Whitehead, N. A., Barnard, A. M. L., Slater, H., Simpson, N. J. L. & Salmond, G. P. C. Quorum-sensing in gram-negative bacteria. FEMS Microbiol. Lett. 25, 365–404 (2001).
Lee, J. & Zhang, L. The hierarchy quorum sensing network in Pseudomonas aeruginosa. Protein Cell. 6, 26–41 (2014).
Hentzer, M. et al. Attenuation of Pseudomonas aeruginosa virulence by quorum sensing inhibitors. EMBO J. 22, 3803–3815 (2003).
Singh, V. K. et al. Tackling recalcitrant Pseudomonas aeruginosa infections in critical illness via anti-virulence monotherapy. Nat. Commun. 13, (2022).
Tang, H. et al. Epigallocatechin-3-Gallate ameliorates Acute Lung damage by inhibiting quorum-sensing-related virulence factors of Pseudomonas aeruginosa. Front. Microbiol. 13, (2022).
Azimi, S., Klementiev, A. D., Whiteley, M. & Diggle, S. P. Bacterial Quorum Sens. Dur. Infect. 201–219 (2020).
Cornforth, D. M. et al. Pseudomonas aeruginosa transcriptome during human infection. Proc. Natl. Acad. Sci. U S A. 115, E5125–E5134 (2018).
Marvig, R. L., Sommer, L. M., Molin, S. & Johansen, H. K. Convergent evolution and adaptation of Pseudomonas aeruginosa within patients with cystic fibrosis. Nat. Genet. 47, 57–64 (2015).
Smith, E. E. et al. Genetic adaptation by Pseudomonas aeruginosa to the airways of cystic fibrosis patients. Proc. Natl. Acad. Sci. U S A. 103, 8487–8492 (2006).
Turner, K. H., Wessel, A. K., Palmer, G. C., Murray, J. L. & Whiteley, M. Essential genome of Pseudomonas aeruginosa in cystic fibrosis sputum. Proceedings of the National Academy of Sciences 112, 4110–4115 (2015).
Gannon, A. D. & Darch, S. E. Tools for the real-time assessment of a Pseudomonas aeruginosa infection model. J. Visualized Experiments. 1–17 https://doi.org/10.3791/62420 (2021).
Tata, M. et al. RNAseq based transcriptional profiling of Pseudomonas aeruginosa PA14 after short and long-term anoxic cultivation in synthetic cystic fibrosis sputum medium. PLoS One. 11, 1–18 (2016).
Palmer, K. L., Aye, L. M. & Whiteley, M. Nutritional cues control Pseudomonas aeruginosa multicellular behavior in cystic fibrosis sputum. J. Bacteriol. 189, 8079–8087 (2007).
Fung, C. et al. Gene expression of Pseudomonas aeruginosa in a mucin-containing synthetic growth medium mimicking cystic fibrosis lung sputum. J. Med. Microbiol. 59, 1089–1100 (2010).
Rosen, B. H. et al. Animal and model systems for studying cystic fibrosis. J. Cyst. Fibros. 17, S28–S34 (2018).
O’Toole, G. A. et al. Model systems to study the chronic, polymicrobial infections in cystic fibrosis: Current approaches and exploring future directions. mBio 12, 1–8 (2021).
McCarron, A., Donnelley, M. & Parsons, D. Airway disease phenotypes in animal models of cystic fibrosis. Respir Res. 19, 1–12 (2018).
Harrington, N. E. et al. Antibiotic efficacy testing in an ex vivo model of Pseudomonas aeruginosa and Staphylococcus aureus biofilms in the cystic fibrosis lung. Journal of Visualized Experiments 1–16 (2021). (2021).
Harrington, N. E., Littler, J. L. & Harrison, F. Transcriptome analysis of Pseudomonas aeruginosa Biofilm infection in an Ex vivo Pig Model of the cystic fibrosis lung. Appl. Environ. Microbiol. 88, (2022).
Joseph, T., Look, D. & Ferkol, T. NF-κB activation and sustained IL-8 gene expression in primary cultures of cystic fibrosis airway epithelial cells stimulated with Pseudomonas aeruginosa. Am. J. Physiol. Lung Cell. Mol. Physiol. 288, 471–479 (2005).
Balloy, V. et al. Bronchial epithelial cells from cystic fibrosis patients express a specific long non-coding RNA signature upon Pseudomonas aeruginosa infection. Front. Cell. Infect. Microbiol. 7, 1–9 (2017).
Tang, M. et al. Evaluating bacterial pathogenesis using a model of human Airway Organoids infected with Pseudomonas aeruginosa Biofilms. Microbiol. Spectr. 10, (2022).
Frisk, A. et al. Transcriptome analysis of Pseudomonas aeruginosa after interaction with human airway epithelial cells. Infect. Immun. 72, 5433–5438 (2004).
Zulianello, L. et al. Rhamnolipids are virulence factors that promote early infiltration of primary human airway epithelia by Pseudomonas aeruginosa. Infect. Immun. 74, 3134–3147 (2006).
Tseng, J., Do, J., Widdicombe, J. H. & Machen, T. E. Innate immune responses of human tracheal epithelium to Pseudomonas aeruginosa flagellin, TNF-α, and IL-1β. Am. J. Physiol. Cell. Physiol. 290, 678–690 (2006).
Laucirica, D. R., Garratt, L. W. & Kicic, A. Progress in Model systems of cystic fibrosis mucosal inflammation to understand aberrant neutrophil activity. Front. Immunol. 11, 1–12 (2020).
Sachs, N. et al. Long-term expanding human airway organoids for disease modeling. EMBO J. 38, 1–20 (2019).
Dekkers, J. F. et al. A functional CFTR assay using primary cystic fibrosis intestinal organoids. Nat. Med. 19, 939–945 (2013).
Pleguezuelos-Manzano, C. et al. Establishment and culture of human intestinal organoids derived from adult stem cells. Curr. Protoc. Immunol. 130, (2020).
Puschhof, J. et al. Intestinal organoid cocultures with microbes. Nat. Protoc. 16, 4633–4649 (2021).
Westermann, A. J. & Vogel, J. Host-pathogen transcriptomics by dual RNA-seq. Methods Mol. Biol. 1737, 59–75 (2018).
Moura-Alves, P. et al. Host monitoring of quorum sensing during Pseudomonas aeruginosa infection. Science 366, 2019 (1979).
Hughes, D. T. & Sperandio, V. Inter-kingdom signaling: Communication between bacteria and their hosts. Nat. Rev. Microbiol. 6, 111–120 (2008).
Kendall, M. M. & Sperandio, V. What a dinner party! Mechanisms and functions of interkingdom signaling in host-pathogen associations. mBio 7, 1–14 (2016).
Vasil, M. L. & Ochsner, U. A. The response of Pseudomonas aeruginosa to iron: Genetics, biochemistry and virulence. Mol. Microbiol. 34, 399–413 (1999).
Bharwad, K. & Rajkumar, S. Rewiring the functional complexity between Crc, Hfq and sRNAs to regulate carbon catabolite repression in. Pseudomonas World J. Microbiol. Biotechnol. 35, 1–12 (2019).
Rojo, F. Carbon catabolite repression in Pseudomonas: Optimizing metabolic versatility and interactions with the environment. FEMS Microbiol. Rev. 34, 658–684 (2010).
Line, L. et al. Physiological levels of nitrate support anoxic growth by denitrification of Pseudomonas aeruginosa at growth rates reported in cystic fibrosis lungs and sputum. Front. Microbiol. 5, 1–11 (2014).
Palmer, K. L., Brown, S. A. & Whiteley, M. Membrane-bound nitrate reductase is required for anaerobic growth in cystic fibrosis sputum. J. Bacteriol. 189, 4449–4455 (2007).
Rossi, E., Falcone, M., Molin, S. & Johansen, H. K. High-resolution in situ transcriptomics of Pseudomonas aeruginosa unveils genotype independent patho-phenotypes in cystic fibrosis lungs. Nat. Commun. 9, 1–13 (2018).
Chen, L., Zou, Y., She, P. & Wu, Y. Composition, function, and regulation of T6SS in Pseudomonas aeruginosa. Microbiol. Res. 172, 19–25 (2015).
Sana, T. G., Berni, B. & Bleves, S. The T6SSs of Pseudomonas aeruginosa strain PAO1 and their effectors: Beyond bacterial-cell targeting. Front. Cell. Infect. Microbiol. 6, (2016).
Hauser, A. R. & The Type, I. I. I. Secretion system of Psueomonas Aeruginosa: Infection by injection. Nat. Rev. Microbiol. 7, 654–665 (2009).
Hernandez, R. E., Gallegos-Monterrosa, R. & Coulthurst, S. J. Type VI secretion system effector proteins: Effective weapons for bacterial competitiveness. Cell. Microbiol. 22, 1–9 (2020).
Sana, T. G. et al. The second type VI secretion system of Pseudomonas aeruginosa strain PAO1 is regulated by quorum sensing and fur and modulates internalization in epithelial cells. J. Biol. Chem. 287, 27095–27105 (2012).
Gifford, A. H. et al. Use of a multiplex transcript method for analysis of Pseudomonas aeruginosa gene expression profiles in the cystic fibrosis lung. Infect. Immun. 84, 2995–3006 (2016).
Bundy, B. M., Campbell, A. L. & Neidle, E. L. Similarities between the antABC-encoded anthranilate dioxygenase and the benABC-encoded benzoate dioxygenase of Acinetobacter sp. strain ADP1. J. Bacteriol. 180, 4466–4474 (1998).
Thomas, S. R., Anjana, R., Hodson, M. E. & Pitt, T. L. Increased sputum amino acid concentrations and auxotrophy of Pseudomonas aeruginosa in severe cystic fibrosis lung disease. Thorax 55, 795–797 (2000).
Huang, H. et al. An integrated genomic regulatory network of virulence-related transcriptional factors in Pseudomonas aeruginosa. Nat. Commun. 10, (2019).
Wilton, M., Halverson, T. W. R., Charron-Mazenod, L., Parkins, M. D. & Lewenza, S. Secreted phosphatase and deoxyribonuclease are required by Pseudomonas aeruginosa to defend against neutrophil extracellular traps. Infect. Immun. 86, 1–12 (2018).
Cornforth, D. M., Diggle, F. L., Melvin, J. A., Bomberger, J. M. & Whiteley, M. Quantitative framework for model evaluation in microbiology research using Pseudomonas aeruginosa and cystic fibrosis infection as a test case. mBio 11, (2020).
Lewin, G. R. et al. Application of a quantitative framework to improve the accuracy of a bacterial infection model. Proc. Natl. Acad. Sci. U S A 120, (2023).
Kordes, A. et al. Genetically diverse Pseudomonas aeruginosa populations display similar transcriptomic profiles in a cystic fibrosis explanted lung. Nat. Commun. 10, (2019).
Wargo, M. J. Choline catabolism to glycine betaine contributes to Pseudomonas aeruginosa Survival during murine lung infection. PloS One. 8, 1–7 (2023).
Randell, S. H., Fulcher, M. L., O’Neal, W. & Olsen, J. C. Primary epithelial cell models for cystic fibrosis research. Methods Mol. Biol. 742, 285–310 (2011).
Liu, Y. C. et al. Contribution of the alkylquinolone quorum-sensing system to the interaction of Pseudomonas aeruginosa with bronchial epithelial cells. Front. Microbiol. 9, (2018).
Geurts, M. H. & Clevers, H. CRISPR engineering in organoids for gene repair and disease modelling. Nat. Reviews Bioeng. 1, 32–45 (2023).
Moura-Alves, P. et al. Host monitoring of quorum sensing during Pseudomonas aeruginosa infection. Science 366, (2019).
Moura-Alves, P. et al. AhR sensing of bacterial pigments regulates antibacterial defence. Nature 512, 387–392 (2014).
Nadjsombati, M. S. et al. Detection of succinate by intestinal tuft cells triggers a type 2 innate immune circuit. Immunity 49, 33–41 (2018).
Tizzano, M. et al. Nasal chemosensory cells use bitter taste signaling to detect irritants and bacterial signals. Proc. Natl. Acad. Sci. U S A. 107, 3210–3215 (2010).
Rossy, T. et al. Pseudomonas aeruginosa contracts mucus to rapidly form biofilms in tissue-engineered human airways. bioRxiv 2 (2022).
Dar, D., Dar, N., Cai, L. & Newman, D. K. Spatial transcriptomics of planktonic and sessile bacterial populations at single-cell resolution. Science 373, (2021). (1979).
Shi, H. et al. Highly multiplexed spatial mapping of microbial communities. Nature 588, 676–681 (2020).
Beenker, W. A. G., Hoeksma, J., Bannier-Hélaouët, M. & Clevers, H. & den Hertog, J. Paecilomycone inhibits quorum sensing in Gram-negative bacteria. Microbiol. Spectr. 11 (2023).
Hmelo, L. R. et al. Precision-engineering the Pseudomonas aeruginosa genome with two-step allelic exchange. Nat. Protoc. 10, 1820–1841 (2015).
Rodenburg, L. W. et al. Protocol for generating airway organoids from 2D air liquid interface-differentiated nasal epithelia for use in a functional CFTR assay. STAR. Protoc. 4, (2023).
Amatngalim, G. D. et al. Measuring cystic fibrosis drug responses in organoids derived from 2D differentiated nasal epithelia. Life Sci. Alliance. 5, 1–14 (2022).
Aprianto, R., Slager, J., Holsappel, S. & Veening, J. W. Time-resolved dual RNA-seq reveals extensive rewiring of lung epithelial and pneumococcal transcriptomes during early infection. Genome Biol. 17, 1–16 (2016).
Dobin, A. et al. Ultrafast universal RNA-seq aligner. Bioinf. 29. STAR, 15–21 (2013).
Liao, Y., Smyth, G. K., & Shi, W. FeatureCounts: An efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2014).
Stover, C. K. et al. Complete genome sequence of Pseudomonas aeruginosa PAO1, an opportunistic pathogen. Nature 406, 959–964 (2000).
Schoch, C. L. et al. NCBI Taxonomy: A comprehensive update on curation, resources and tools. Database 1–21 (2020).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 1–21 (2014).
Blighe, K., Rana, S., Lewis, M. & Enhanced volcano publication-ready volcano plots with enhanced colouring and labeling. https://github.com/kevinblighe/EnhancedVolcano (2018).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. ClusterProfiler: An R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Winsor, G. L. et al. Enhanced annotations and features for comparing thousands of Pseudomonas genomes in the Pseudomonas genome database. Nucleic Acids Res. 44, 646–653 (2016).
Szklarczyk, D. et al. STRING v11: Protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 47, D607–D613 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592 (2023).
Acknowledgements
We would like to thank Dr. Tim Holm Jakobsen for kindly providing PAO1-GFP strain, Dr. Bart Bardoel for kindly providing E. coli RHO3 strain, and Joe J. Harrison for kindly providing the pEX18Gm plasmid.
Author information
Authors and Affiliations
Contributions
C.P-M. and W.A.G.B. conceived and designed the study with H.C and J.d.H. C.P-M. and W.A.G.B. performed experiments with help from G.J.F.v.S. and H.B. G.D.A and J.M.B. provided materials and deposited the human sequencing data set with C.P-M. C.P-M. and W.A.G.B. wrote the first draft of the manuscript. H.C. and J.d.H. supervised the project, acquired funding and administered the project. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
HC is the head of Pharma Research and Early Development at Roche, Basel and holds several patents related to organoids technology. HC’s full disclosure is given at https://www.uu.nl/staff/JCClevers/. The other authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pleguezuelos-Manzano, C., Beenker, W.A.G., van Son, G.J.F. et al. Dual RNA sequencing of a co-culture model of Pseudomonas aeruginosa and human 2D upper airway organoids. Sci Rep 15, 2222 (2025). https://doi.org/10.1038/s41598-024-82500-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-82500-w