Abstract
Febrile neutropenia is a major complication in patients with acute leukemia or those undergoing hematopoietic stem cell transplantation (HSCT). Understanding patient characteristics and susceptibility patterns in febrile neutropenia is essential for appropriate antimicrobial therapy. First-line agents should have Pseudomonas aeruginosa coverage, but with the increase in multi-drug resistant organisms, ceftazidime-avibactam has emerged as a new therapeutic option. This retrospective case–control study included 300 admissions (143 patients) between January 2009 and December 2022. Patients with hematologic neoplasms and patients that underwent HSCT, satisfying the criteria of febrile neutropenia and treated with ceftazidime-avibactam (CAZAVI) were included and compared to controls who received the best available therapy (BAT). A bivariate regression model explored independent predictors of septic shock and mortality. Patients who received CAZAVI were more likely to have a microbiologically documented infection (59.0% vs. 28.3%). Complications were significantly more frequent in the CAZAVI group, with sepsis being the most common (59.0%). Multivariable logistic regression analysis showed that receiving CAZAVI was an independent risk factor for both sepsis and mortality (aOR 6.33 [95% CI 2.81–14.30] and 7.82 [2.63–23.26], respectively). Knowing common organisms and patterns of resistance, with an understanding of risk factors for morbidity and mortality, is crucial for the antimicrobial management of febrile neutropenia. Further studies on the effectiveness of CAZAVI in this population are needed.
Similar content being viewed by others
Introduction
Patients with hematological malignancies are at an increased risk of developing serious infections, which significantly affect both their survival and quality of life. More than 80% of patients with hematological malignancies will present with fever during a chemotherapy cycle that has caused neutropenia1. Deficits in components of the innate immune system, as a result of the underlying malignancy, may predispose to the development of invasive bacterial and fungal infections2. The treatment itself, more commonly, can lead to neutropenia, which is a major predisposing factor for infections3. Cytotoxic antineoplastic therapy for hematological malignancies as well as stem cell transplantation are common causes of treatment-induced neutropenia due to a decrease in white blood cell production4. Fever is often the only sign of infection, since the intensity of the neutrophil-mediated inflammatory response may be blunted4. As such, a high index of suspicion followed by an extensive diagnostic work-up and prompt initiation of antimicrobial therapy are crucial5.
The epidemiology of microorganisms isolated from the blood of patients with neutropenic fever has changed over time. While Gram-negative pathogens predominated in the 1960s, the increased use of indwelling catheters in the 1980s and 1990s led to a higher incidence of Gram-positive organisms6. Currently, the most common blood isolates in most centers are coagulase-negative staphylococci6, although in some cases a trend reversal is being witnessed with the emergence of drug-resistant Gram-negative pathogens7,8. In our country, however, this variation has not been observed. Over the years, several studies from Lebanon have shown a consistently higher prevalence of Gram-negative infections in febrile neutropenic patients9,10,11. In addition, antimicrobial resistance among Gram-negative pathogens in Lebanon is substantial. The proportions of extended-spectrum beta-lactamase (ESBL) producing Enterobacterales exceed 30%12, while proportions of carbapenem-resistant Enterobacterales range from 3 to 6%13.
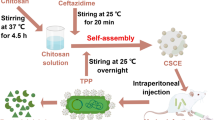
Empiric therapy for febrile neutropenia, while guided by international guidelines6, must also take into account the local epidemiology. Ceftazidime-avibactam (CAZAVI), a broad-spectrum beta-lactam/beta-lactamase inhibitor combination, has been increasingly used in patients with febrile neutropenia, whether empirically in patients who fail to respond to first-line therapy, or as directed therapy when a resistant Gram-negative pathogen is recovered from clinical cultures14,15.
The aim of our study is to characterize febrile neutropenia episodes in patients with acute leukemias and those undergoing hematopoietic stem cell transplantation (HSCT), and to compare the outcomes of patients who received traditional antimicrobial therapy to those who received CAZAVI.
Methods
Study design and population
This is a retrospective case–control study conducted at the American University of Beirut Medical Center (AUBMC), a tertiary care center in Lebanon. Our sample included all adult patients presenting with febrile neutropenia following induction therapy for acute leukemia or during HSCT. The medical records of febrile neutropenic patients admitted to AUBMC between 2009 and 2022 were reviewed. Patients were included more than once if they developed another febrile neutropenia episode at least 14 days after the initial one. Study subjects were classified into cases who received CAZAVI for the treatment of febrile neutropenia, and controls who were treated with the best available therapy (BAT). BAT was defined as therapy for febrile neutropenia according to the AUBMC guidelines (which are based on the IDSA guidelines). In these guidelines, the first-line therapy for febrile neutropenia is either cefepime or piperacillin-tazobactam, and the second-line therapy is imipenem or meropenem as monotherapy. Alternatively, combination therapy can be used; this would entail including any monotherapy treatment option in addition to an aminoglycoside or a quinolone. As for prophylaxis protocol, valacyclovir is used for viral prophylaxis. As for fungal prophylaxis, fluconazole is used in auto-transplant patients and voriconazole is used in those who receive an allo-transplant. Finally, bacterial prophylaxis with levofloxacin is indicated when absolute neutrophil count (ANC) is less than 1000. It is important to note that we do not currently routinely screen patients for rectal or oral colonization with antimicrobial resistant microorganisms.
In most common scenarios, ceftazidime-avibactam is used after persistent febrile episode after attempting first and second line treatment options. In addition, patients admitted with febrile neutropenia at our institution are usually looked after by the infectious diseases team; thus resorting CAZAVI as escalation is usually a decision made by an infectious disease expert.
Definitions and severity scores
We adopted the definitions of fever and neutropenia as set forth by the guidelines of the Infectious Diseases Society of America (IDSA): an oral temperature record of 38.3 °C (101 °F) or a temperature of ≥ 38.0 °C (100.4 °F) lasting for at least one hour, and a neutrophil count below 1500/mm316. Several indices were used to estimate baseline functioning and illness severity and were calculated based on published literature: the Charlson Comorbidity Index predicts the 10-year mortality for patients with a number of comorbidities17; the Multinational Association for Supportive Care in Cancer (MASCC) score index measures the risk of complications in patients with febrile neutropenia, where a score of < 21 indicates high risk of having a serious infection6; the Quick Sepsis Related Organ Failure Assessment (qSOFA) is a bedside tool used to screen for sepsis in patients with a suspected infection18; the Eastern Cooperative Oncology Group (ECOG) performance status is a scale used to determine the disease progression and its effect on daily living habits of cancer patients, with a score ranging from 0 (fully active) to 5 (dead)19.
Statistical analysis
Data were entered into SPSS. Bivariable analysis was performed to detect statistical associations using the Chi-square test for categorical variables and the independent samples t-test for continuous variables. Backward stepwise binary logistic regression was performed to test for independent associations, including effect of treatment with CAZAVI on sepsis and mortality, controlling for potential confounders. Variables with a p-value of 0.2 or less on bivariable analysis were included in the regression model.
Ethical considerations
All methods were performed in accordance with the guidelines and regulations of the Institutional Review Board at the American University of Beirut. Since this was a retrospective descriptive study, informed consent was waived.
Results
During the study period, we recorded 339 episodes of neutropenic fever, 39 of which were treated with CAZAVI and 300 with BAT. More patients who received CAZAVI treatment had an established source of infection compared to those who received BAT (89.7% vs. 57.0%; p < 0.001). The most common identified sources of infection in patients receiving CAZAFI were intravascular devices (33.3%) and respiratory infections (28.2%), whereas most common sources of infection in patients receiving BAT were gastrointestinal (15%), respiratory (14.7%) and urinary (12%). The baseline characteristics of patients are displayed in Table 1. Age and sex distribution were similar in both study arms. Compared to the BAT group, there was a higher proportion of patients in the CAZAVI group who were undergoing HSCT (33.3% allo-HSCT and 15.4% auto-HSCT), whereas most patients in the BAT group were receiving induction therapy for acute myeloid leukemia (62.0%; p < 0.001). As far as baseline severity scores, there was no difference in the mean Charlson and ECOG scores between the two study groups. However, the MASCC score, which is calculated upon developing the episode of febrile neutropenia, was significantly lower in the CAZAVI group (19.5 ± 4.1 vs. 21.9 ± 4.1; p = 0.001), indicating a high risk for developing complications from neutropenic fever. Patients in the CAZAVI arm were more likely to have a microbiologically documented infection (59.0% vs. 28.3%). The distribution of isolated organisms is shown in Table 2. Gram-negative organisms predominated in both CAZAVI and BAT arms (74.4% and 38.3%, respectively), whereas Gram-positive organisms trailed by a considerable margin (28.2% and 15.7%, respectively). As expected, a larger number of patients who received CAZAVI had antimicrobial-resistant Gram-negative organisms, including ESBL-producing and carbapenem-resistant E. coli. Up to 18.5% of study subjects had received carbapenem therapy for more than 48 h in the 30 days preceding the febrile neutropenia episode. In addition, 85% of the overall population had received antibacterial and antiviral prophylaxis, and 89% had received antifungal prophylaxis. In the BAT arm, carbapenems were the most commonly used antibiotics for empiric as well as for directed therapy, followed by cefepime, piperacillin-tazobactam, and glycopeptides. The febrile neutropenia episodes in our study were associated with various complications, and almost all were significantly more frequent in the CAZAVI group (Table 3). The most commonly observed complication was sepsis, which occurred in 59.0% of patients in the CAZAVI arm and in 15.0% of patients in the BAT arm (p < 0.001). Other important complications included intensive care unit (ICU) admission, respiratory failure, and persistent bacteremia. Patients who received CAZAVI-based regimens were more likely to have a fatal outcome compared to patients who received BAT (23.1% vs. 3.0%). The leading cause of death in the CAZAVI group was septic shock (50%), followed by disseminated intravascular coagulation (DIC) (14%), COVID pneumonia (7%), and ischemic stroke (7%). The remaining (21%) died after being discharged from the hospital and cause of death was not reported. It is important to note that this mortality was late, more than 15 days from the start of the febrile episode. As for the start of CAZAVI, 86% of the mortalities were late, compared to 14% of mortalities happening within the first 3 days after starting CAZAVI.
We conducted a multivariable logistic regression analysis to determine independent risk factors for sepsis and mortality, and we were particularly interested in evaluating whether the type of antibiotic treatment had an effect on patient outcome. The results of the multivariable models are shown in Table 4. Receiving CAZAVI was an independent risk factor for both sepsis and mortality, with a large effect size for both outcomes (aOR 6.33 [95% CI 2.81–14.30] and 7.82 [2.63–23.26], respectively). Recent receipt of steroids was a significant risk factor for sepsis (aOR 2.12 [95% CI 1.08–4.15]) but not for mortality. On the other hand, MASCC score was negatively correlated with both sepsis and mortality.
Discussion
This is a retrospective case–control study evaluating the effect of CAZAVI on patient outcomes with neutropenic fever compared to other treatment regimens. With the ever-increasing antimicrobial resistance rates among Gram-negative pathogens, broad-spectrum agents are more likely to be prescribed, despite not being traditional treatment options based on IDSA guidelines. This is particularly true for high-risk patients with hematological malignancies or HSCT recipients who experience more profound and prolonged neutropenia.
As such, evaluating the prevalence of potentially causative organisms in patients with neutropenic fever is crucial, as it facilitates prompt initiation of antimicrobial treatment, preventing rapid progression to sepsis and shock20. E. coli was the most common isolated organism among patients with febrile neutropenia in our study, consistent with the trend observed in Lebanon for the past 25 years9,10,11. We also note that we isolated more gram negative than gram positive microorganisms in both groups CAZAFI (74.4% vs 28.2%) and BAT (38.3% vs 15.7%). Other studies looking at bloodstream infections in patients receiving HSCT also show increased prevalence of gram-negative infections21. Few studies have been published from the Arab region regarding the epidemiology of febrile neutropenia in cancer patients, yielding variable results. Data from Saudi Arabia indicated a predominance of Gram-negative bloodstream infections in neutropenic patients, with E. coli being the most common isolated pathogen22. A retrospective study from Qatar, which included more than 1000 episodes of febrile neutropenia, showed a prevalence of 41% of ESBL-producing organisms23. The findings were different in Kuwait and the UAE, where there was a predominance of Gram-positive infections among febrile neutropenic patients24.
The emergence of multi-drug resistant Gram-negative pathogens can be attributed to the use of quinolones as prophylaxis, which in itself is a risk factor for colonization by such organisms25. This correlates with our findings, given that levofloxacin was the most commonly used drug for prophylaxis, as it reduces the incidence of bloodstream infections with no effect on mortality26. On the other hand, fluoroquinolone prophylaxis has been shown to reduce gram-negative bloodstream infections in patients that were not colonized with fluoroquinolone resistant gram-negative bacteria27.
Patients with acute leukemia usually acquire resistant bacteria due to their immunocompromised state28. They thus receive broad-spectrum antibiotics, eventually tailored to culture results. Initial empiric treatment in febrile neutropenia includes a beta-lactam with Pseudomonas aeruginosa coverage29,30,31. In our center, carbapenems were most commonly used as empiric treatment, correlating with the rising number of Gram negative ESBL organisms. Vancomycin and cefepime were equally used due to the rising number of central venous catheters reflecting an increase in the incidence of staphylococcus coagulase negative bacteremia. This is consistent with clinical practice guidelines6,32.
As expected, a larger number of patients who received ceftazidime-avibactam had antimicrobial resistant organisms. In fact, the increasing incidence of resistant pathogens remains a challenge in the management of febrile neutropenia and preliminary data have shown that CAZAVI can play a role as empiric therapy for those who had carbapenem-resistant Klebsiella bloodstream infections33.
Furthermore, patients who received CAZAVI-based regimens were more likely to have complications compared to the BAT group. Bacteremia represents 11.7% of all sources of infection, concordant with a study conducted in Saudi Arabia24. A previous study done in Lebanon showed that bacteremia was the source in 18% of all patients with febrile neutropenia11, while another study on patients with HSCT showed that the incidence of bacteremia was 41.2%34, a value much higher than what we currently observed. Septic shock, cardiovascular complications and persistent infection were all significantly associated with increased mortality. A retrospective cohort study conducted in 2021 showed that septic shock is one of the two main independent predictors of mortality in febrile neutropenia35,36. We also note that among patients receiving CAZAVI, a higher proportion had a microbiologically confirmed respiratory infection (28.2%) compared to patients receiving BAT (14.7%). In addition, previous studies showed that mortality rates are higher in patients with febrile neutropenia diagnosed with pneumonia compared to other groups, as well as an association between pneumonia and mortality in acute leukemia patients36,37.
Our multivariable logistic regression analysis also revealed that CAZAVI was an independent risk factor for both sepsis and mortality, with a large effect size for both outcomes. This raises concerns about the role of CAZAVI in treating febrile neutropenia in this population. Some studies have reported similar outcomes with CAZAVI. For instance, a large retrospective study by Jorgensen et al. (2019) reported a 30-day mortality of 17% in patients treated with CAZAVI38.
However, these results should be interpreted with caution and may be biased due to several limitations. First, a smaller number of patients received CAZAVI compared to BAT. This may have been influenced by the fact that CAZAVI was not always available at our institution during the study period and was provided based on patient need and financial capacity. Additionally, many patients received CAZAVI empirically and may have died from complications or infections unrelated to the administered drug. Nevertheless, CAZAVI has proven effective in several recent studies for febrile neutropenia, particularly in patients with Klebsiella pneumoniae carbapenemase (KPC)39 and has shown higher clinical cure rates40. Furthermore, limitations of this study include the retrospective nature of its design, the relatively small sample size, and its reliance on data generated from a single tertiary care center. Another limitation of our study is the possibility of selection bias, as we postulate that the CAZAVI group may have included more unwell patients due to the drug’s use being reserved for those who had failed first and second-line treatments as per our guidelines (supplementary material). We minimized this bias by controlling for MASCC and ECOG scores, which provide a way to compare patients with similar disease severity. However, the lack of control for organism type and infection focus introduces residual allows to maintain a risk of bias. We highlight the need for randomized controlled studies that allow us to better understand this correlation.
Conclusion
Awareness of the local patterns of infections and susceptibilities, as well as understanding the predictors for septic shock and mortality in patients with febrile neutropenia pave the way to successful treatment and prevention of neutropenic fever.
Reducing the morbidity and mortality risk relies on the above in order to successfully initiate proper empiric treatment. More studies are needed to investigate adverse events related to the introduction of ceftazidime-avibactam and to establish a benefit to risk ratio, as there is still no consensus on appropriate CAZAVI dosage in such scenarios and its efficiency in resolving the febrile neutropenia.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lyman, G. H. & Kuderer, N. M. Epidemiology of febrile neutropenia. Support Cancer Ther. 1(1), 23–35 (2003).
Logan, C., Koura, D. & Taplitz, R. Updates in infection risk and management in acute leukemia. Hematol. Am. Soc. Hematol. Educ. Program. 2020(1), 135–139 (2020).
Baden, L. R. et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc Netw. 14(7), 882–913 (2016).
Stern, A. et al. Early discontinuation of antibiotics for febrile neutropenia versus continuation until neutropenia resolution in people with cancer. Cochrane Database Syst. Rev. 1(1), CD012184 (2019).
Satyanarayana, G. Work-up for fever during neutropenia for both the stem cell transplant recipient and the hematologic malignancy patient. Infect. Dis. Clin. N. Am. 33(2), 381–397 (2019).
Freifeld, A. G. et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin. Infect. Dis. 52(4), e56-93 (2011).
Cattaneo, C. et al. Recent changes in bacterial epidemiology and the emergence of fluoroquinolone-resistant Escherichia coli among patients with haematological malignancies: results of a prospective study on 823 patients at a single institution. J. Antimicrob. Chemother. 61(3), 721–728 (2008).
Oliveira, A. L. et al. Epidemiology of bacteremia and factors associated with multi-drug-resistant gram-negative bacteremia in hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 39(12), 775–781 (2007).
Ghosn, M. et al. Infections in cancer patients with granulocytopenia. Retrospective studies of 59 febrile episodes with hospitalization. J. Med. Liban. 42(3), 117–122 (1994).
Hamzeh, F., Kanj, S. S. & Uwaydah, M. Febrile neutropenia in cancer patients in a tertiary care medical center in Lebanon: microbial spectrum and outcome. J. Med. Liban. 48(3), 136–142 (2000).
Kanafani, Z. A. et al. Bloodstream infections in febrile neutropenic patients at a tertiary care center in Lebanon: a view of the past decade. Int. J. Infect. Dis. 11(5), 450–453 (2007).
Moghnieh, R. A. et al. Epidemiology of common resistant bacterial pathogens in the countries of the Arab League. Lancet Infect. Dis. 18(12), e379–e394 (2018).
Moussally, M. et al. Prevalence of antibiotic-resistant organisms among hospitalized patients at a tertiary care center in Lebanon, 2010–2018. J. Infect. Public Health 14(1), 12–16 (2021).
Clerici, D. et al. The place of ceftazidime/avibactam and ceftolozane/tazobactam for therapy of haematological patients with febrile neutropenia. Int. J. Antimicrob. Agents 57(6), 106335 (2021).
Soriano, A. et al. Ceftazidime-avibactam for the treatment of serious gram-negative infections with limited treatment options: a systematic literature review. Infect. Dis. Ther. 10(4), 1989–2034 (2021).
Villafuerte-Gutierrez, P., Villalon, L., Losa, J. E. & Henriquez-Camacho, C. Treatment of febrile neutropenia and prophylaxis in hematologic malignancies: a critical review and update. Adv. Hematol. 2014, 986938 (2014).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chron. Dis. 40(5), 373–383 (1987).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8), 801–810 (2016).
Azam, F. et al. Performance status assessment by using ECOG (Eastern Cooperative Oncology Group) score for cancer patients by oncology healthcare professionals. Case Rep. Oncol. 12(3), 728–736 (2019).
Hansen, B. A. et al. Febrile neutropenia in acute leukemia. epidemiology, etiology, pathophysiology and treatment. Mediterr. J. Hematol. Infect Dis. 12(1), e2020009 (2020).
Akhmedov, M. et al. Incidence, etiology, risk factors, and outcomes of pre-engraftment bloodstream infections after first and second allogeneic hematopoietic cell transplantation. Transpl. Infect. Dis. 24(3), e13842 (2022).
Binkhamis, K. et al. Prevalence of bacterial bloodstream infections and association between neutropenia and 30-day mortality among oncology inpatients at a university hospital in Saudi Arabia. Ann. Saudi Med. 43(3), 172–178 (2023).
El Omri, H. et al. Dissecting bloodstream infections in febrile neutropenic patients with hematological malignancies, a decade-long single center retrospective observational study (2009–2019). J. Infect. Public Health 17(1), 152–162 (2024).
Al-Tawfiq, J. A. et al. Epidemiology and source of infection in patients with febrile neutropenia: a ten-year longitudinal study. J. Infect Public Health 12(3), 364–366 (2019).
Rodriguez-Bano, J. et al. Epidemiology and clinical features of infections caused by extended-spectrum beta-lactamase-producing Escherichia coli in nonhospitalized patients. J. Clin. Microbiol. 42(3), 1089–1094 (2004).
Mikulska, M. et al. Fluoroquinolone prophylaxis in haematological cancer patients with neutropenia: ECIL critical appraisal of previous guidelines. J. Infect. 76(1), 20–37 (2018).
Akhmedov, M. et al. Impact of fluoroquinolone administration and gut mucosal colonization on the risk of pre-engraftment bloodstream infections after allogeneic hematopoietic cell transplantation. Leuk Lymphoma 64(6), 1102–1111 (2023).
Satlin, M. J. & Walsh, T. J. Multidrug-resistant Enterobacteriaceae, Pseudomonas aeruginosa, and vancomycin-resistant Enterococcus: three major threats to hematopoietic stem cell transplant recipients. Transpl. Infect. Dis. 19, 6 (2017).
Averbuch, D0 et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica 98(12), 1826–1835 (2013).
Taplitz, R. A. et al. Outpatient management of fever and neutropenia in adults treated for malignancy: american society of clinical oncology and infectious diseases Society of America Clinical Practice guideline update. J. Clin. Oncol. 36(14), 1443–1453 (2018).
Groll, A. H. et al. Fourth European Conference on Infections in Leukaemia (ECIL-4): guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic haemopoietic stem-cell transplantation. Lancet Oncol. 15(8), e327-40 (2014).
Khoo, A. L. et al. Evaluation of a risk-guided strategy for empirical carbapenem use in febrile neutropenia. Int. J. Antimicrob. Agents 52(3), 350–357 (2018).
Sonya, K. et al. Overcoming resistance: antibiotic guidance for multidrug-resistant febrile neutropenia in patients with cancer. J. Hematol. Oncol. Pharm. 2021, 11 (2021).
Ogura, S. et al. Characteristics of gram-negative bacteremia during febrile neutropenia among allogeneic hematopoietic stem cell transplant recipients on levofloxacin prophylaxis. Eur. J. Clin. Microbiol. Infect. Dis. 40(5), 941–948 (2021).
Sereeaphinan, C., Kanchanasuwan, S. & Julamanee, J. Mortality-associated clinical risk factors in patients with febrile neutropenia: a retrospective study. IJID Reg. 1, 5–11 (2021).
Wanitpongpun, C. et al. Clinical factors predictive of mortality in acute leukemia patients with febrile neutropenia. Am. J. Blood Res. 11(1), 59–65 (2021).
Nattamol, H. et al. Prognostic factors for mortality with febrile neutropenia in hospitalized patients. Southwest Respir. Crit. Care Chron. 3, 9 (2015).
Jorgensen, S. C. J. et al. Real-world experience with ceftazidime-avibactam for multidrug-resistant gram-negative bacterial infections. Open Forum Infect Dis. 6(12), ofz522 (2019).
Herrera, F. et al. Ceftazidime-avibactam improves outcomes in high-risk neutropenic patients with Klebsiella pneumoniae carbapenemase-producing enterobacterales bacteremia. Microorganisms 12, 1 (2024).
Castón, J. J. et al. Clinical efficacy of ceftazidime/avibactam versus other active agents for the treatment of bacteremia due to carbapenemase-producing Enterobacteriaceae in hematologic patients. Int. J. Infect. Dis. 59, 118–123 (2017).
Author information
Authors and Affiliations
Contributions
J.A., F.A., R.M. wrote-up the protocol; J.A., F.A., C.D., A.K., R.G., and R.M. collected data; J.A., A.K., and R.G. wrote the manuscript, F.A. edited the manuscript, Z.K. conceptualized the study, designed the study and analyzed the data. Z.K. finalized manuscript revision and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
All methods were carried out in accordance with relevant guidelines and regulations.
Approval statement
All experimental protocols were approved by the Institutional Review Board at the American University of Beirut.
Informed consent
Since this was a retrospective descriptive study, informed consent was waived by the Institutional Review Board at the American University of Beirut.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Abi Frem, J., Khazzeka, A., Allaw, F. et al. Ceftazidime-avibactam for the treatment of febrile neutropenia in HSCT recipients and acute leukemia patients post induction chemotherapy. Sci Rep 14, 31322 (2024). https://doi.org/10.1038/s41598-024-82795-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-82795-9