Abstract
The study aimed to compare the oxidative stress status in the kidney tissue of rats treated with paraquat and nanoparaquat. The levels of oxidative stress markers, including malondialdehyde (MDA), total antioxidant capacity (TAC), and thiol groups (TTG), were measured in the kidney tissue samples. A total of forty male Wistar rats were randomly assigned to eight groups, each consisting of five rats: a control group, a paraquat (PQ) group, an N-acetylcysteine (NAC) group, groups receiving nanoparaquat α and β (α and β), groups receiving PQ and NAC (PQ + NAC), and groups receiving nanoparaquat α and β with NAC (+ NACα and β). Paraquat, a widely used herbicide, induces severe oxidative damage in kidneys through radical formation and cellular stress. Newly developed nanoparaquat formulations may modify its toxicity profile and tissue distribution patterns. The results revealed that rats treated with paraquat showed a significant increase in Lipid Peroxidation Oxidation (LPO) levels compared to the control group and those treated with NAC. However, treatment with nanoparaquat α and β resulted in a decrease in LPO levels compared to the paraquat-treated group. Additionally, when nanoparaquat α and β were administered in combination with NAC, a further reduction in LPO levels was observed compared to the PQ treated group. Regarding TAC levels, the PQ group exhibited a significant decrease compared to the control group and the NAC-treated group. However, treatment with nanoparaquat β resulted in higher TAC levels compared to the PQ group. Moreover, when nanoparaquat α and β were administered in combination with NAC, there was an increase in TAC levels compared to the PQ group. In terms of TTG levels, the PQ group showed a significant decrease compared to the control group and the NAC group. However, treatment with nanoparaquat β led to an increase in TTG levels compared to the PQ group. Furthermore, when nanoparaquat α and β were administered in combination with NAC, there was an increase in TTG levels compared to the PQ group. Overall, the results suggest that treatment with nanoparaquat, especially nanoparaquat β, may have a protective effect against oxidative stress induced by PQ toxicity in the kidney tissue of rats. Further studies are warranted to elucidate the underlying mechanisms and potential therapeutic implications of nanoparaquat in oxidative stress-related kidney disorders.
Similar content being viewed by others
Introduction
Paraquat (PQ) is a non-selective herbicide that is extensively utilized in agriculture because of its quick effectiveness, relatively affordable price, and wide range of effectiveness1,2. In this study, kidney tissue was selected for this study due to its vulnerability to oxidative stress and its critical role in detoxifying harmful substances3. Paraquat and nanoparaquat are known to induce significant oxidative damage, particularly in the kidneys, where they can disrupt cellular functions and lead to nephrotoxicity4. The kidneys also possess a high metabolic activity, making them susceptible to oxidative stress from toxic compounds3. By assessing oxidative stress status in kidney tissue, the study aims to understand the extent of damage caused by paraquat and nanoparaquat, providing insights into their nephrotoxic effects and potential protective strategies3.
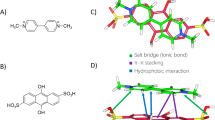
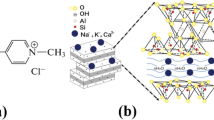
In this study, nanoparaquat α and β formulations, both with and without chitosan, were synthesized using a defined process. Typically, nanoparaquat formulations are prepared by dissolving paraquat in a suitable solvent, followed by the addition of chitosan to create a chitosan-nanoparaquat complex5,6. This mixture is then subjected to techniques such as sonication or high-speed stirring to achieve uniform dispersion and nanoparticle formation4. The resulting formulations are characterized by size and stability assessments to ensure their suitability for in vivo studies. This methodology allows for the evaluation of oxidative stress status in kidney tissue following treatment with these formulations4.
PQ poisoning is a highly lethal toxicity frequently encountered by physicians in hospital emergency departments7. PQ poisoning often results in systemic effects that vary depending on the level of toxin exposure8. PQ is eliminated by renal excretion9. PQ toxicity has been attributed to oxidative stress and the generation of superoxide anions, as indicated by performed investigations10. Furthermore, lipid peroxidation (LPO) has been identified as an additional route of PQ -induced harm in animals11. Additionally, glutathione and thiol groups have a significant function in counteracting the effects of PQ12. When it comes to using nanoscience in medication development and other materials, nanoparaquat may offer improved effectiveness and reduced toxicity compared to PQ6. The objective of this study was to examine the impact of two distinct compositions of PQ nanoparticles (one with chitosan and one without) on the oxidative condition of kidney tissues in rats that have been treated. In order to evaluate the level of oxidation in tissues, we will quantify the overall ability of antioxidants to counteract oxidative damage total antioxidant capacity (TAC), measure the concentration of LPOand determine the amount of total thiol groups (TTG) in kidney tissue. Furthermore, the levels of serum creatinine and blood urea nitrogen (BUN) will be assessed to determine the state of renal function4,13.
Specific biochemical markers, including malondialdehyde (MDA), total antioxidant capacity (TAC), and thiol groups (TTG), were selected in this study to comprehensively assess oxidative stress in the kidney tissue of male rats treated with paraquat and nanoparaquat4. MDA serves as an indicator of lipid peroxidation and oxidative damage, while TAC measures the overall antioxidant defenses in the tissue. Thiol groups reflect cellular integrity and redox status. Together, these markers provide critical insights into the extent of oxidative damage and nephrotoxicity induced by paraquat and nanoparaquat, facilitating a better understanding of their impact on renal health4.
Chitosan’s significance lies in its diverse range of beneficial properties, including its antioxidant activity, biocompatibility, effectiveness as a drug delivery system, ability to modify toxicity, capacity to reduce oxidative damage, and role in assessing histopathological changes14.
N-acetylcysteine (NAC) is important for assessing oxidative stress in kidney tissue due to its antioxidant properties, ability to enhance glutathione levels, and protective effects against nephrotoxicity. It also reduces oxidative damage and modulates inflammatory responses, making it valuable for evaluating therapeutic efficacy against paraquat and nanoparaquat-induced kidney injury15. Aparicio-Trejo et al. (2019)16found that the widely adopted experimental model of acute kidney injury (AKI) using folic acid (FA) has yet to be fully understood at the molecular level. Their investigation uncovered that within 24 h, FA administration leads to significant disruptions in multiple mitochondrial pathways, encompassing energy production, oxidative balance, structural changes, and cellular recycling mechanisms. The study highlights the protective role of N-acetyl-cysteine (NAC), a compound that proves essential in sustaining crucial mitochondrial components, particularly glutathione concentration and S-glutathionylation modifications. These processes are fundamental for cellular energy production and maintaining oxidative equilibrium. Prophylactic treatment with NAC successfully shielded both mitochondrial integrity and kidney function by stabilizing these vital cellular mechanisms. As the first research to establish this connection, their work identifies mitochondria as a key therapeutic target in FA-induced AKI. The results point toward innovative treatment strategies that emphasize mitochondrial protection to prevent both immediate kidney damage and long-term complications. Joshi et al. (2019)17 conducted research examining acute mercury toxicity and explored how protective compounds might mitigate its harmful effects. The investigation utilized laboratory rats to evaluate the therapeutic potential of two antioxidant agents: selenium (Se) and N-acetyl cysteine (NAC). Following mercuric chloride exposure, researchers observed substantial alterations in biochemical parameters, reflecting compromised organ function, particularly in the hepatic and renal systems. The poisoning led to significant mercury deposits in vital organs, triggered oxidative stress, and compromised the body’s natural antioxidant defense mechanisms. While independent administration of either Se or NAC demonstrated beneficial effects, the concurrent application of both compounds yielded remarkable results. This dual-treatment approach effectively counteracted mercury’s toxic impact by preserving cellular integrity and preventing oxidative stress-induced damage. These findings highlight the synergistic potential of combining Se and NAC as a therapeutic intervention for mercury poisoning, offering promising implications for clinical applications.
Materials and methods
The proposal of this study was approved by the animal ethics committee of the Hamadan University of Medical Sciences (IR.UMSHA.REC.1400.631), and all methods were carried out in accordance with relevant guidelines and regulations. In this study, 40 male Wistar rats weighing between 180 and 250 g were purchased from Pasteur Institute (Tehran, Iran). The animals were housed in standard laboratory conditions with ad libitum access to water and food and a 12-hour light-dark cycle.
In this study, PQ, nanoparaquat, and N-acetylcysteine (NAC) were co-administered via the intraperitoneal route simultaneously. The poisoning induced in the rats was acute and lasted for one day, and sample collection was performed 24 h after the last treatment4. All doses were determined after conducting pilot studies. Nanoparaquat α and β formulations (with and without chitosan) were studied on male Wistar rats as follows: eight groups were established, including paraquat and nanoparaquat effects over one week, compared to control and NAC as a supplement with antioxidant properties used in PQ poisoning4. The groups were: (1) Control group: received normal saline as control, intraperitoneally injected for one week. (2) PQ group: received PQ at a dose of 4 mg/kg intraperitoneally injected for one week. (3) NAC group: received NAC at a dose of 300 mg/kg intraperitoneally injected for one week. (4) Nanoparaquat α group: received nanoparaquat α equivalent to a dose of 4 mg/kg PQ intraperitoneally injected for one week. (5) Nanoparaquat β group: received nanoparaquat β equivalent to a dose of 4 mg/kg paraquat intraperitoneally injected for one week. (6) NAC and PQ group: received NAC (300 mg/kg) and PQ (4 mg/kg) intraperitoneally injected simultaneously for one week. (7) NAC and nanoparaquat α group: received NAC (300 mg/kg) and nanoparaquat α (equivalent to 4 mg/kg PQ) intraperitoneally injected simultaneously for one week. (8) NAC and nanoparaquat β group: received NAC (300 mg/kg) and nanoparaquat β (equivalent to 4 mg/kg PQ) intraperitoneally injected simultaneously for one week4.
After the end of the treatment period, the rats were injected with ketamine and xylazine to make them anesthetized and ready for sacrifice4. The abdomen was opened, and blood was drawn from the inferior vena cava using a 10 mL syringe. Serum was separated by centrifugation at 3000 rpm for 5 min at −20 °C for biochemical tests. One kidney was rinsed in physiological saline and stored in liquid nitrogen and then at −80°C until the tests were performed. The other kidney was placed in 10% formalin for histopathological studies. Frozen tissue was homogenized in homogenization buffer, and oxidative stress tests including LPO, TAC and TTG were assayed4.
For histopathological examination, one kidney from each rat was fixed in 10% formalin solution to preserve tissue architecture. The focus was on analyzing structural changes, tissue damage, cellular alterations, and potential protective effects of NAC against paraquat and nanoparaquat-induced renal injury under microscopic evaluation4.
The data were analyzed using Prism 6.0 for Windows software. Quantitative variables were expressed as Mean ± SEM. All differences between various groups were assessed using One-Way ANOVA if the distribution was normal, and Kruskal-Wallis one-way ANOVA if the distribution was not normal. A significance level of p< 0.05 was considered statistically significant4.
Results
The measurement of BUN
The study findings indicate that the level of blood urea nitrogen (BUN) in group PQ exhibited a notable elevation in comparison to groups control and NAC. Treatment with nano-particles α and β resulted in a reduction in BUN levels compared to group PQ, however this reduction did not reach statistical significance (Fig. 1).
The measurement of creatinine
The study findings indicate that there was no statistically significant variation in the level of creatinine across all the study groups (Fig. 2).
The measurement of TAC
Based on the study results, the level of TAC (Total Antioxidant Capacity) in group PQ shows a significant decrease compared to groups control and NAC. Additionally, treatment with nano-paracuat β demonstrates a higher level of TAC compared to group PQ. Furthermore, treatment with nano-paracuat α and β along with NAC leads to an increase in TAC levels compared to group PQ (Fig. 3).
The measurement of LPO
The findings of the research indicate that group PQ exhibits a statistically significant elevation in LPO levels in comparison to groups control and NAC. In comparison to group PQ, treatment with nano-paracuat α and β leads to a reduction in LPO levels. In addition to NAC, nano-paracuat α and β decrease LPO levels in comparison to group P (Fig. 4).
The measurement of TTG
The study findings indicate that group PQ exhibited a statistically significant reduction in TTG levels when compared to groups control and NAC. TTG levels increase in response to nano-paracuat treatment in comparison to group PQ. In addition to NAC, nano-paracuat α and β cause an elevation in TTG levels in comparison to group PQ (Fig. 5).
Histopathological results of kidney tissue.
The results obtained from hematoxylin and eosin staining of kidney tissue after tissue sectioning and hematoxylin-eosin staining were examined under a light microscope and images were prepared at a magnification of 400 (Fig. 6).
Representative kidney micrographs (H&E staining, 400x magnification) showing histological features across treatment groups. Control (A) and NAC (B) groups display normal renal architecture with intact glomeruli (GLU), well-defined Bowman’s space (BS), and healthy proximal (PCT) and distal convoluted tubules (DCT). Paraquat-treated group (C) exhibits severe tissue damage, including hemorrhage (H) and tubular necrosis (N). NAC co-treatment with paraquat (D) shows partial protection of renal structures. Nano-particle α treatment (E) and its combination with NAC (F) demonstrate modified tissue response compared to conventional paraquat. Similarly, nano-particle β alone (G) and with NAC (H) show distinct patterns of renal tissue alterations, suggesting different toxicity profiles from standard paraquat.
The examinations showed that in the control group and the NAC group, the structure of kidney tissue was completely normal, and the glomeruli and Bowman’s capsules showed complete integrity. There was no expansion in Bowman’s space, and the epithelial lining of both proximal and distal tubules was completely healthy, with no epithelial shedding observed.
Administration of paracuat resulted in expansion of Bowman’s space and hemorrhage in kidney tissue, as well as necrosis. Shedding of tubular epithelium was abundantly observed, making it difficult to distinguish between proximal and distal tubules. In the group that received NAC following paracuat administration, although less tubular epithelial shedding was observed, expansion of Bowman’s space and hemorrhage in kidney tissue still persisted. Administration of nano-particles α and β did not show any improvement. Although NAC administration with nano-particles α and β reduced the extent of hemorrhage, epithelial shedding and necrosis were more pronounced in these groups compared to control group.
Discussion
The objective of this study was to evaluate the toxicity of nanoparaquat in comparison to PQ, as well as their potential for causing acute renal impairment in Wistar rats in the presence of NAC. The toxic effects of nanoparaquat on oxidative stress in the kidney tissue of male rats treated with paraquat and nanoparaquat were investigated. Exposure to these substances resulted in significant oxidative damage, characterized by elevated levels of reactive oxygen species and decreased antioxidant capacity. Markers such as malondialdehyde (MDA) were increased, indicating lipid peroxidation, while total antioxidant capacity (TAC) and thiol groups were diminished. Histopathological examination revealed structural changes in kidney tissue, further highlighting the nephrotoxic potential of nanoparaquat. These findings underscore the need for further research into the mechanisms of toxicity and potential protective strategies against oxidative stress induced by these compounds.
Due to the extensive utilization and convenient availability of paraquat, incidences of PQ poisoning frequently transpire across the Asia-Pacific area, resulting in elevated fatality rates. Despite the availability of several suggested therapies for paraquat poisoning, the death rate remains alarmingly high, ranging from 50 to 90%18. Prior research has mostly concentrated on examining the effects of PQ nanoparticles in the fields of agriculture, herbicides, and cellular toxicity. Nevertheless, these investigations predominantly focus on the durability on soil surfaces and the avoidance of infiltration into the soil. Currently, there have been no investigations carried out at the intracellular level across different tissues. In a recent research, Karbasi et al. (2023) colleagues examined lung tissue to assess the impact of two specific forms of nanoparaquat4. The findings of their investigation closely align with the results of this study. The study found that the beta formulation of nanoparaquat was able to alter the pulmonary toxicity of paraquat when compared to PQ alone and when administered simultaneously with NAC.
Multiple studies have conducted comparisons between the methods of delivering chemicals in animal models and have presented data on the parallels in the development of toxicity by intraperitoneal (IP) injection and oral administration19,20. While IP injection exhibits greater bioavailability in comparison to oral delivery, these methods have important commonalities21,22. The pharmacokinetics and metabolic destiny of low molecular weight drugs via these channels exhibit similarities23. Just like when taken orally, these drugs are mostly absorbed into the portal vein when injected intraperitoneally24. It is important to acknowledge that gastric juice has the ability to modify the chemical composition of chemicals24. The structure of nanoparaquats is likely to be disrupted when administered orally, and this is attributed to the acidic gastrointestinal environment in mice (pH 2.0–4.1), leading to alterations in the compounds24. Moreover, based on research findings, intraperitoneal injection is a superior choice for delivering substantial amounts of substances24. As a result, it was determined to deliver PQ and nanoparaquat through the peritoneum. Irrespective of the specific properties of paraquat, inhaling it is the most effective method for evaluating the possible consequences of exposure. This aspect might be seen as a drawback in our study. PQ is dispersed across many organs in mammals and mostly accumulates in the lungs and kidneys, irrespective of the method of introduction into the body2,25. PQ has a broad impact on several organ systems in the body and can result in the development of multiple organ dysfunction syndrome in extreme instances. Due to the kinetic toxic mechanism of paraquat, the kidney is the main organ affected following poisoning. In all, 90% of paraquat is eliminated unchanged during a period of 12 to 24 h by renal excretion. The mechanisms of acute kidney damage produced by paraquat involve oxidative stress, inflammatory response, apoptosis, and hemodynamic alterations in the kidneys26.
PQ and nanoparaquat elicit oxidative stress in tissues. Elevated concentrations of LPO, reduced levels of TAC and TTG, together with histological alterations such as enlargement of Bowman’s space, bleeding, and necrosis in kidney tissue, are indicative of this condition. MDA is the end result of the oxidation of unsaturated fatty acids in the presence of reactive oxygen species (ROS) found in organelles and cell membranes7. PQ markedly elevated the levels of LPO in kidney tissue when compared to both the control group and NAC. Both α and β nanoparticle versions exhibited a substantial reduction in LPO levels when compared to paraquat. Furthermore, from a statistical standpoint, the levels of LPO were equivalent in the control, NAC, α, and β groups. Regarding LPO levels, there is data indicating that circumstances can be improved with the use of a nanoparaquat formulation. The levels of thiobarbituric acid reactive substances TAC in the group treated with PQ showed a substantial reduction compared to both the control group and the group treated with NAC. The administration of nanoparaquat β resulted in a notably elevated TAC level in comparison to the PQ group, suggesting less severe oxidative damage to the kidneys. However, this effect was not observed with nanoparaquat α. Based on the data, it can be inferred that nanoparaquat β exhibits higher efficacy in terms of TAC levels when compared to nanoparaquat α. The PQ group exhibited a substantial reduction in TTG levels compared to the control and NAC groups. The administration of nanoparaquat β resulted in a considerable elevation of TTG levels in comparison to the PQ group. The levels of TTG showed a little rise when exposed to nanoparaquat α compared to the PQ group, while the difference was not statistically significant. Based on the data, it can be inferred that nanoparaquat β outperforms nanoparaquat α in terms of TTG levels.
The primary processes of paraquat toxicity involve the production of reactive oxygen species and the cellular release of nicotinamide adenine dinucleotide phosphate (NADPH)27. Thus, antioxidants may serve as advantageous antidotes in cases of paraquat poisoning. NAC has a crucial role in providing cysteine, which is necessary for the production of glutathione. Glutathione is an antioxidant that is present inside cells and provides protection against reactive oxygen species (ROS) and oxidative stress28. Research indicates that administering NAC after PQ poisoning has been advantageous in decreasing LPO and enhancing the levels of beneficial glutathione29. Similar to air conditioning, the treatment of vitamin C, which is recognized as a powerful antioxidant, decreased the morphological damage caused by PQ toxicity in the livers and kidneys of the mice examined. Awadalla’s findings demonstrated the protective properties of vitamin C against the harmful effects of paraquat30. Thus, NAC is proposed as a potential antidote for PQ toxicity. We conducted an assessment of the therapeutic benefits of NAC on renal tissue in the context of paraquat and nanoparaquat toxicity. AC mitigated renal injury. Administration of nanoparaquats α and β, in combination with NAC, resulted in an elevation in TAC levels in mice, as compared to the PQ group. However, the combination of paraquat and NAC did not have a similar effect. To clarify, NAC demonstrated enhanced resistance to oxidative conditions in the presence of nanoparaquats, but not when exposed to PQ. Nanoparaquats α and β, in combination with NAC, resulted in a decrease in LPO levels as compared to the PQ group. In addition, the presence of nanoparaquats α and β with NAC resulted in higher amounts of TTG compared to the PQ group. These data suggest that the NAC with nanoparaquat formulation elicits a more favorable response to its antioxidant capabilities.
The BUN test quantifies the concentration of urea nitrogen present in the bloodstream. The BUN is a byproduct that results from the breakdown of proteins in the liver. The BUN is transported to the kidneys via the circulatory system, where it undergoes filtration and is subsequently eliminated from the body through urine31. If the liver is impaired, it may fail to adequately metabolize proteins. If the kidneys are compromised, they may exhibit inadequate filtration of urea. Each of these issues might result in elevated BUN levels in the body. Measuring BUN levels alone is not sufficient for accurately evaluating renal function. Nevertheless, when compared to creatinine levels, it can serve as a reliable predictor of renal function31. Serum creatinine serves as a prognostic indicator for clinical outcomes in individuals suffering from paraquat poisoning32. A study conducted by Suji Kim and her colleagues revealed a positive correlation between elevated levels of blood creatinine and higher death rates33. In this study, the levels of BUN were shown to be considerably higher in the PQ group compared to the C and NAC groups. Treatment with nanoparaquats α and β and NAC resulted in a decrease in BUN levels compared to the PQ group, however the difference was not statistically significant. Put simply, the nanoparaquat formulation did not result in a statistically significant improvement in BUN levels. There were no significant differences in creatinine levels among the research groups.
Nanoparaquat β induces lower levels of oxidative stress on the kidneys compared to both PQ and its α version. This suggests that the utilization of nanoparticle-based pesticides might potentially offer improved effectiveness and safety in the future.
Conclusion
This study highlights the toxic effects of paraquat and nanoparaquat on oxidative stress in the kidney tissue of male Wistar rats. The findings indicate that both compounds significantly increase oxidative damage, as evidenced by elevated levels of malondialdehyde and decreased total antioxidant capacity. The protective role of N-acetylcysteine (NAC) suggests potential therapeutic strategies for mitigating oxidative stress in cases of paraquat poisoning. Future research should explore long-term effects and different animal models to enhance our understanding of the mechanisms underlying nephrotoxicity and the efficacy of potential protective agents against these toxicants. This study’s strengths include a comprehensive evaluation of the effects of paraquat and nanoparaquat on oxidative stress in a controlled environment using male Wistar rats, which enhances the reliability of the findings. The use of N-acetylcysteine (NAC) as a potential protective agent adds significant value to the research. However, limitations exist, such as the short duration of acute poisoning, which may not adequately reflect the effects of chronic exposure. Additionally, the reliance on a single animal model could restrict the generalizability of the results to other species or conditions, warranting further investigation in diverse settings.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Gawarammana, I. B. & Buckley, N. A. Medical management of paraquat ingestion. Br. J. Clin. Pharmacol. 72 (5), 745–757 (2011).
Pasi, A. The toxicity of paraquat, diquat and morfamquat. Vienna: Hans Huber. 13 – 5. (1978).
Ozbek, E. Induction of oxidative stress in kidney. Int. J. Nephrol. 2012 (1), 465897 (2012).
Karbasi, A. et al. Is nanoparaquat safer than bulk paraquat? An in vitro and in vivo evaluation. Toxicology 484, 153398 (2023).
Fernandes, T., Soares, S. F., Trindade, T. & Daniel-da-Silva, A. L. Magnetic hybrid nanosorbents for the uptake of paraquat from water. Nanomaterials 7 (3), 68 (2017).
Nishisaka, C., Grillo, R., Sanches, G., Fraceto, L. & Lima, R. (eds) Analysis of the effects of pesticides and nanopesticides on the environment. BMC Proceedings; Springer (2014).
Suntres, Z. E. Role of antioxidants in paraquat toxicity. Toxicology 180 (1), 65–77 (2002).
Ranjbar, A. et al. Ameliorative effect of Matricaria chamomilla. L on paraquat: Induced oxidative damage in lung rats. Pharmacognosy Res. 6 (3), 199 (2014).
Weng, C. H. et al. Predictors of acute kidney injury after paraquat intoxication. Oncotarget 8 (31), 51345–51354 (2017).
Ranjbar, A. Evidence of oxidative damage in paraquat toxicity. Zahedan J. Res. Med. Sci. 16 (12), 1–8 (2014).
Bus, J. S. & Gibson, J. E. Paraquat: model for oxidant-initiated toxicity. Environ. Health Perspect. 55, 37–46 (1984).
Nakagawa, I., Suzuki, M., Imura, N. & Naganuma, A. Enhancement of paraquat toxicity by glutathione depletion in mice in vivo and in vitro. J. Toxicol. Sci. 20 (5), 557–564 (1995).
Silfeler, I. et al. Protective effect of ellagic acid on paraquat-induced kidney hazards in rats. Iran. J. Kidney Dis. 11 (1), 23 (2017).
Abd El-Hack, M. E. et al. Antimicrobial and antioxidant properties of chitosan and its derivatives and their applications: A review. Int. J. Biol. Macromol. 164, 2726–2744 (2020).
De Andrade, K. Q. et al. Oxidative stress and inflammation in hepatic diseases: therapeutic possibilities of N-acetylcysteine. Int. J. Mol. Sci. 16 (12), 30269–30308 (2015).
Aparicio-Trejo, O. E. et al. Protective effects of N-acetyl-cysteine in mitochondria bioenergetics, oxidative stress, dynamics and S-glutathionylation alterations in acute kidney damage induced by folic acid. Free Radic. Biol. Med. 130, 379–396 (2019).
Joshi, D., Mittal, D. K., Shukla, S., Srivastav, A. K. & Srivastav, S. K. N-acetyl cysteine and selenium protects mercuric chloride-induced oxidative stress and antioxidant defense system in liver and kidney of rats: a histopathological approach. J. Trace Elem. Med Biol. 28 (2), 218–226 (2014).
Gheshlaghi, F. et al. Prediction of mortality and morbidity following paraquat poisoning based on trend of liver and kidney injury. BMC Pharmacol. Toxicol. 23 (1), 67 (2022).
Grabenstatter, H. L., Clark, S. & Dudek, F. E. Anticonvulsant effects of carbamazepine on spontaneous seizures in rats with kainate-induced epilepsy: comparison of intraperitoneal injections with drug‐in‐food protocols. Epilepsia 48 (12), 2287–2295 (2007).
Hu, S-C. et al. Toxicokinetic and genotoxicity study of NNK in male Sprague Dawley rats following nose-only inhalation exposure, intraperitoneal injection, and oral gavage. Toxicol. Sci. 182 (1), 10–28 (2021).
Chen, M. M. et al. Intoxication by intraperitoneal injection or oral gavage equally potentiates postburn organ damage and inflammation. Mediators of inflammation. 2013. (2013).
Al Shoyaib, A., Archie, S. R. & Karamyan, V. T. Intraperitoneal route of drug administration: should it be used in experimental animal studies? Pharm. Res. 37, 1–17 (2020).
Lukas, G., Brindle, S. D. & Greengard, P. The route of absorption of intraperitoneally administered compounds. J. Pharmacol. Exp. Ther. 178 (3), 562–566 (1971).
Nebendahl, K. Routes of administration. The laboratory rat. Elsevier, pp. 463 – 83 (2000).
Smith, L. Paraquat toxicity. Philosophical Transactions of the Royal Society of London B. Biol. Sci. 311 (1152), 647–657 (1985).
Song, Y., Li, C., Luo, F. & Tao, Y. Clinical features and risk factors of acute kidney injury in children with acute paraquat intoxication. J. Int. Med. Res. 47 (9), 4194–4203 (2019).
Zhang, S. et al. Prognostic value of liver and kidney function parameters and their correlation with the ratio of urine-to‐plasma paraquat in patients with paraquat poisoning. Basic Clin. Pharmacol. Toxicol. 128 (6), 822–830 (2021).
Sadowska, A., Manuel-Y-Keenoy, B. & De Backer, W. Antioxidant and anti-inflammatory efficacy of NAC in the treatment of COPD: discordant in vitro and in vivo dose-effects: a review. Pulm. Pharmacol. Ther. 20 (1), 9–22 (2007).
Yeh, S. T. Y. et al. Protective effects of N-acetylcysteine treatment post acute paraquat intoxication in rats and in human lung epithelial cells. Toxicology 223 (3), 181–190 (2006).
Awadalla, E. A. Efficacy of vitamin C against liver and kidney damage induced by paraquat toxicity. Exp. Toxicol. Pathol. 64 (5), 431–434 (2012).
Smilde, T. D., van Veldhuisen, D. J., Navis, G., Voors, A. A. & Hillege, H. L. Drawbacks and prognostic value of formulas estimating renal function in patients with chronic heart failure and systolic dysfunction. Circulation 114 (15), 1572–1580 (2006).
Su, Y. et al. Investigation of simple, objective, and effective indicators for predicting acute paraquat poisoning outcomes. Toxicol. Ind. Health. 36 (6), 417–426 (2020).
Kim, S., Gil, H-W., Yang, J-O., Lee, E-Y. & Hong, S-Y. The clinical features of acute kidney injury in patients with acute paraquat intoxication. Nephrol. Dialysis Transplantation. 24 (4), 1226–1232 (2009).
Author information
Authors and Affiliations
Contributions
F.B.: Project administration, review & editing, Writing – original draft; M.V.: review & editing, Writing – original draft; A.R.: Project administration, review & editing, Writing – original draft; A.K.: review & editing, Writing – original draft; A.A.: review & editing, Writing – original draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no known competing financial or non-financial interests that could have appeared to influence the work reported in this paper.
Animal Ethical Considerations and Informed Consent
All protocols in this study were approved by the Committee on the Ethics of Animal Experiments of Hamadan University of Medical Sciences Ethics Committee on Animal Care, Hamadan, Iran (IR.UMSHA.REC.1400.631), in compliance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH publication no.85 − 23, revised 1996). All experimental procedures and reporting follow the ARRIVE guidelines for animal research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bahramibanan, F., Rad, M.V., Ranjbar, A. et al. Comparison of oxidative stress status in the kidney tissue of male rats treated with paraquat and nanoparaquat. Sci Rep 15, 389 (2025). https://doi.org/10.1038/s41598-024-83156-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-83156-2