Abstract
To evaluate the efficacy of laparoscopic-assisted Soave procedure of Hirschsprung’s Disease (HSCR) in neonates and infants within 3 months of age. Patients with HSCR who were admitted to the Department of Fetal and Neonatal Surgery of Hunan Children’s Hospital from June 2012 to July 2020 and underwent laparoscopic-assisted Soave procedure were selected. The clinical manifestations, surgical procedures, postoperative fecal contamination, constipation, enterocolitis, and defecation function were analyzed. A total of 267 children were included, 230 males and 37 females. Vaginal delivery occurred in 138 cases (51.7%) and cesarean delivery in 129 cases (48.3%). There were 217 cases (81.3%) of delayed excretion of meconium, preoperative HAEC (Hirschsprung’s Disease Associated enterocolitis) 116 cases (43.4%), postoperative HAEC 54 cases (20.2%), 1 cases of postoperative death, 266 cases (99.6%) were cured. There were 37 cases (13.9%) of long-segment type, 226 cases (84.6%) of common type, and 4 cases (1.5%) of short-segment type. Of the 267 cases, 214 cases were followed up (80.1%), 60 cases with fecal contamination, the incidence rate was 28.0%, and 5 cases were tertiary fecal contamination. The overall incidence of constipation was 3.7% (8 cases), and 2 cases were third-degree constipation. Evaluation of defecation function: The excellent rate was 94.4%. Laparoscopic-assisted Soave procedure in neonates and infants within 3 months of age is generally safe and feasible, most infants have good postoperative defecation function, and the incidence of postoperative fecal contamination, constipation, and enterocolitis is relatively low.
Similar content being viewed by others
Background
Hirschsprung’s disease (HSCR) is the most common congenital intestinal neuropathy characterized by the absence of enteric ganglion cells, with an incidence of 1/1500-1/50001. The absence of ganglion cells in the muscular layer and submucosa of intestine leads to persistent spasms and symptoms including constipation, vomiting and intestinal obstruction, which can be life-threatening in severe cases2. The only effective treatment for HSCR is surgery which need to resected the abnormally innervated bowel3. Soave is one of the most commonly used pull-through procedure3.
With the popularization of laparoscopic technology, most medical centers in China have routinely carried out laparoscopic-assisted Soave procedure. However, most of the studies focused on the surgical effects in older infants and young children, while there are few studies on the efficacy of laparoscopic-assisted surgery in neonates and young infants4. Therefore, mastering the effect of laparoscopic surgery in neonates and young infants is of great significance to deepen the understanding of diseases and guide the treatment. By summarizing the clinical data of 267 cases of HSCR treated with laparoscopic-assisted Soave procedure in our hospital, this paper provides reference for the clinical diagnosis and treatment of HSCR in neonates and young infants. The report is as follows.
Methods
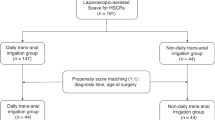
Patients
The clinical data of all the 267 patients who underwent laparoscopic-assisted Soave procedure at the Department of Fetal and Neonatal Surgery of Hunan Children’s Hospital from June 2012 and July 2020 were analyzed retrospectively. Inclusion criteria: (1) Received Soave pull-through surgery in our hospital within 3 months of age (total laparoscopy or laparoscopy converted to open); (2) HSCR was confirmed by intraoperative and postoperative pathologic examination both. Exclusion criteria: (1) Age of operation ≥ 3 months; (2) Patients who underwent laparoscopic-assisted Soave procedure in other hospitals; (3) Total colon aganglionosis, (4) Combined with anorectal malformation. This study was approved by the Ethics Committee of Hunan Children’s Hospital. Written informed consent was obtained from all parents of the patients. All research was performed in accordance with relevant guidelines/regulations.
The HSCR was classified into the following 3 categories based on the extent of aganglionosis, (1) Short-segment type (Lower rectum): aganglionosis restricted to the lower rectum (under peritoneal reflection); (2) Common type (Sigmoid colon): aganglionosis extended to the sigmoid colon; (3) Long-segment (Left-right colon): aganglionosis extended beyond the sigmoid colon but did not reach the cecum5.
Surgery
Cleaning irrigations were conducted every day preoperatively for 10–14 days, and intestinal preparation was performed 3 days before surgery, including taking oral metronidazole. Nutrition assessment was conducted for every patient after the admission and pre- or post- surgery according to the guideline6. After anesthesia, a 5 mm incision was made in the midpoint between the xiphoid and umbilical cord, and a 5 mm trocar was placed into the abdomen and then established a pneumoperitoneum (8mmHg). Another two trocars were placed at the upper and lower lateral right abdomen. After that we make sure whether the upper rectum and sigmoid colon were spasmodic and then resected 1 × 1 cm bowel wall for frozen biopsy. When the pathologist reported no ganglion cells found, we then mobilized the mesocolon close to the bowel to secure the colonic vessels. After that we did the Soave procedure. The Soave procedure was conducted according to the technique described by De la Torre-Mondragon and Ortega-Salgado7. The difference is that we preserved the muscular cuff 1–2 cm. When it is difficult to mobilize the proximal mesocolon and pull the proximal ganglionic bowel deep into the pelvis under laparoscopy, the surgery was converted to open. The postoperative feeding should commence 2–3 days after surgery. Dilation of the anus was started 2–3 weeks after surgery and lasted 4–6 months.
In patients with severe HAEC or intestinal perforation, a colon biopsy and ileostomy were performed firstly, then a radical surgery was performed in the second stage 2 months later. The diagnosis and treatment of the HAEC were according to the guideline conducted by American Pediatric Surgical Association Hirschsprung Disease Interest Group8.
Data collected and follow-up
All patients were regularly follow-up at the outpatient clinic after discharge, with monthly in the first three months and every three months thereafter. Growth and development, information of postoperative complications and bowel function was recorded every time. Digital rectal examinations, vertical anteroposterior and lateral abdominal X-ray radiographs, barium enema and anorectal manometry were conducted accordingly. Three years post-surgery, each child underwent a postoperative defecation function assessment based on Rintala’s criteria9, which evaluated defecation control ability, including Ability to hold back defecation, Feels/reports the urge to defecation, Frequency of defecation, Soiling, Accidents, Constipation, and social problems. Scores ranged from 17 to 20 (excellent), 12 to 16 (good), 9 to 11 (fair), and less than 8 (poor)9. Bowel movements and constipation were classified using the Krickenbeck score10: Soiling-Grade I: occasionally (1–2 times/week), Grade II: daily with no social problems, Grade III: constant with social problems; Constipation-Grade I: manageable with diet, Grade II: requires laxatives, Grade III: needs enema.
IBM SPSS 20.0 software was used for data sorting and statistical analysis. Continuous data were presented as median and interquartile range (median [IQR]) and categorical data were presented as n (%).
Results
Basic demographics of the patients
A total of 267 infants were included, 230 males (86.1%) and 37 females (13.9%). There were 12 preterm infants (4.5%) and 255 full-term infants (95.5%). Birth weight 3400 [3100 g-3600] g; There were 3 twins (1.1%), all delivered by cesarean section; 138 (51.7%) vaginal deliveries and 129 (48.3%) cesarean deliveries (see Table 1 for details). The median age at surgery was 62 (46–81) days.
Classification and clinical manifestations
All 267 patients had abdominal distension, 232 cases (86.5%) had a history of bilious vomiting, a history of delayed excretion of meconium (no first fetal defecation within 24 h after delivery) in 217 cases (81.3%), the number of preoperative enterocolitis 116 cases (43.4%), and postoperative enterocolitis 54 cases (20.2%). The type of HSCR were as follows: 4 cases (1.5%) of the short-segment type, 226 cases (84.6%) of the common type, and 37 cases (13.9%) of the long-segment type.
Surgical relevance and prognosis
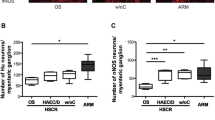
The length of the spastic segment resected in the surgery was 10 [6–15] cm, and the total length of the excised bowel was 23 [20–27] cm. 21 cases was converted the laparoscopy to open surgery. Among the 267 cases, 1 patients died after surgery due to HAEC, resulting in a cure rate of 99.6% (266 cases). Out of the cured cases, 214 patients (80.1%) were followed up, with 60 cases (28.0%) showing soiling, including 5 cases of tertiary soiling and 55 cases of secondary soiling. The overall incidence of constipation was 3.7%, with 8 cases reported, including 2 cases of tertiary constipation and 6 cases of primary constipation. We deal with soiling and postoperative constipation according to the age of the patients and the grades.
In terms of intraoperative details, postoperative complications, and treatment outcomes, the average operation time was 122.8 ± 30.2 min, with an intraoperative blood loss of 4.42 ± 2.04 ml. No cases of anastomotic leakage were observed postoperatively. Among the 214 followed-up patients, the Rintala scores were as follows: 188 cases (87.9%) scored excellent (17–20), 14 cases (6.5%) scored good (12–16), 10 cases (4.8%) scored medium (9–11), and 2 cases (0.9%) scored less than 8. The combined rate of excellent and good outcomes was 94.4%.
Discussion
There is a limited amount of literature available regarding the surgical outcomes in neonates and infants under 3 months of age with HSCR. HSCR is characterized by a lack of ganglionosis in the affected intestine, resulting in persistent spasms and impaired bowel movements. This condition can lead to symptoms such as recurrent abdominal distension, constipation, malnutrition, and in severe cases, HAEC, which can be life-threatening. While conservative treatments such as colonic decompression, crotoxin injection therapy11, biofeedback therapy12, and stem cell therapy13 have been documented, these interventions are primarily utilized for postoperative patients, while stem cell therapy is still in experimental research. Therefore, surgery remains the only definitive treatment for HSCR. The optimal operative procedures include Swenson, Soave, Duhamel, and modified versions of these procedures. The introduction of both laparoscopic surgery and transanal endorectal pull-through (TAEPT)14 has caused a revolution in the operative procedures. However, there is still ongoing debate regarding the optimal timing and choice of surgical procedure. In this retrospective analysis conducted at a single center, we observed that laparoscopic-assisted Soave procedure and short rectum muscular cuff surgery yield satisfactory results in neonates and infants within 3 months of age.
The preoperative diagnosis of HSCR in our center was based on clinical manifestations, physical examination, abdominal X-ray and barium enema in neonate and infants within 3 months of age. We didn’t perform anorectal manometry (ARM) and rectal suction biopsy (RSB) routinely. In recent years, ARM has been widely used in the diagnosis of HSCR because of its advantages such as less trauma, no radiation, convenient, but its diagnostic value is controversial, especially in neonate and young infants15. Preoperative RSB16 is of great significance for the diagnosis of HSCR, but its application in neonate and young infants is limited due to various factors, especially in developing counties. It has been reported abroad that needle-aspiration RSB, which can be safely used in preterm infants, can be applied to preterm infants of 1590 to 2000 g17. However, Nicole Green et al.18 found that in patient older than 6 months, the clear diagnosis rate of needle-aspiration RSB was significantly lower than that of excisional rectal biopsy. Therefore, more advanced biopsy techniques and pathological diagnostic techniques are needed to improve the diagnosis of rectal biopsy in HSCR.
The procedure for HSCR is also evolving. Recently, minimally invasive surgeries, including laparoscopic-assisted surgery and TAEPT, have been introduced as definitive surgeries for HSCR5, which is also the case in most medical institutions in China. Most surgeons advocate that laparoscopy is more suitable for the long-segment type5. In our cohort, since part of the dilated segment had to be resected during surgery, laparoscopy is more suitable for all types of HSCR except total colonic aganglionosis. Although TAEPT has been used more frequently, it is difficult to use in neonates and infants, so only a few cases have been performed in our department. When it is difficult to treat the mesentery of the transverse colon, open surgery is required for the long-segmental type. Some surgeons have made improvements that can be performed in laparoscopic surgery, which is worth mentioning19. Soave procedure has always been the preferred method in our department due to the limited operating space. For the treatment of muscle cuff, surgeons are also constantly exploring, from long muscular rectal cuff to short muscular rectal cuff, and we preferred short muscular rectal cuff, as postoperative constipation incidence is low. For children who need enterostomy in the first stage due to HAEC or intestinal perforation, it is recommended to close colostomy and HSCR radical surgery by laparoscopy.
In a retrospective analysis, Langer JC20 et al. found that HAEC and bowel obstruction were the main causes of readmission after surgery, which was comparable to our cohort. However, anastomotic stenosis and HAEC are the most common postoperative complications in HSCR21. Subsequently, anus dilation was started 2–3 weeks postoperatively, and parents need to continue this program at home after discharge to avoid recurrence of anastomotic stenosis and obstruction. In our cohort, there were 8 (3.7%) cases of constipation that did not continue this program due to parental compliance and were cured after anal dilation treatment. Another complication is the diseased bowel that is left behind. In our center, a routine biopsy was performed and the resection level was determined according to the biopsy results, and the colon was exposed under laparoscopy and completely removed. No residual lesions were found after the operation. With the exception of 2 cases in which reoperation was performed due to adhesive bowel obstruction, there were no cases in which reoperation was performed due to diseased bowel remnants.
As this is a retrospective study, this study also has some limitations. For example, only surgical cases less than 3 months of age were included in this study, and there may be errors in determining the surgical efficacy of HSCR. In addition, this study did not pay special attention to postoperative complications and the resulting errors in the assessment of postoperative defecation function. Therefore, there is an urgent need for nationwide, multicenter follow-up data to obtain relevant data such as surgical procedures and postoperative efficacy of HSCR in China.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Taguchi, T., Obata, S. & Ieiri, S. Current status of Hirschsprung’s disease: Based on a nationwide survey of Japan. Pediatr. Surg. Int. 33(4), 497–504. https://doi.org/10.1007/s00383-016-4054-3 (2017).
Tilghman, J. M. et al. Molecular genetic anatomy and risk profile of Hirschsprung’s disease. N. Engl. J. Med. 380(15), 1421–1432 (2019).
Widyasari, A., Pavitasari, W. A. & Dwihantoro, A. Functional outcomes in Hirschsprung disease patients after transabdominal Soave and Duhamel procedures. BMC Gastroenterol. 18(1), 56–56 (2018).
Feng Jiexiong, D. Several problems in diagnosis and treatment of Hirschsprung’s disease in neonates. Anhui Med. 44(10), 1160–1162 (2019).
Suita, S. et al. Hirschsprung’s disease in Japan: Analysis of 3852 patients based on a nationwide survey in 30 years. J. Pediatr. Surg. 40(1), 197–201 (2005).
Falcão, M. C. & Tannuri, U. Nutrition for the pediatric surgical patient: Approach in the peri-operative period. Rev. Hosp. Clin. Fac. Med. Sao Paulo. 57(6), 299–308 (2002).
De la Torre-Mondragón, L. & Ortega-Salgado, J. A. Transanal endorectal pull-through for Hirschsprung’s disease. J. Pediatr. Surg. 33(8), 1283–1286 (1998).
Gosain, A. et al. Guidelines for the diagnosis and management of Hirschsprung-associated enterocolitis. Pediatr. Surg. Int. 33(5), 517–521 (2017).
Rintala, R. J. & Lindahl, H. Is normal bowel function possible after repair of intermediate and high anorectal malformations?. J. Pediatr. Surg. 30(3), 491–494 (1995).
KyrklundK, Koivusalo, A. et al. Evaluation of bowel function and fecal continence in 594 Finnish individuals aged 4 to 26 years. Dis. Colon Rectum 55(6), 671 (2012).
Halleran, D. R. et al. Anal sphincter botulinum toxin injection in children with functional anorectal and colonic disorders: A large institutional study and review of the literature focusing on complications. J. Pediatr. Surg. 54(11), 2305–2310 (2019).
Yuan, Y. et al. The efficacy of biofeedback therapy for the treatment of fecal incontinence after soave procedure in children for Hirschsprung’s disease. Front. Pediatr. 9, 638120 (2021).
Workman, M. J. et al. Engineered human pluripotent-stem-cell-derived intestinal tissues with a functional enteric nervous system. Nat. Med. 23(1), 49–59 (2017).
Mao, Y. Z., Tang, S. T. & Li, S. Duhamel operation vs. Transanal endorectal pull-through procedure for Hirschsprung disease: A systematic review and meta-analysis. J. Pediatr. Surg. 53(9), 1710–1715 (2018).
Wu, J. F., Lu, C. H. & Yang, C. H. Diagnostic role of anal sphincter relaxation integral in high-resolution anorectal manometry for Hirschsprung disease in infants. J. Pediatr. 194, 136–141 (2018).
Zhang, Y. et al. Safety and accuracy of suction rectal biopsy in preterm infants. Front. Pediatr. 9, 642342 (2021).
Halleran, D. R. et al. Suction rectal biopsy is accurate in late preterm infants with suspected Hirschsprung disease. J. Pediatr. Surg. 55(1), 67–70 (2020).
Green, N. et al. Rectal suction biopsy versus incisional rectal biopsy in the diagnosis of Hirschsprung disease. Pediatr. Surg. Int. 38(12), 1989–1996 (2022).
Li Solin, L. & Yingqiu, L. Meng. Laparoscopic subtotal colectomy (Deloyers surgery). J. Clin. Pediatr. Surg. 1, 67–68 (2007).
Langer, J. C. et al. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr. Surg. Int. 33(5), 523–526 (2017).
Lin, Z. et al. Outcomes of preoperative anal dilatation for Hirschsprung disease. J. Pediatr. Surg. 56(3), 483–486 (2021).
Funding
Supported by Hunan provincial Natural Science Foundation of China (2023JJ30326) and Scientific Research Project of Hunan Provincial Health Commission (W20242013).
Author information
Authors and Affiliations
Contributions
Ren-peng Xia: Analyzed and interpreted the data; Wrote the paper.Ti-dong Ma: Analyzed and interpreted the data; Wrote the paper.Fan Zhao, Yong Xiao, Yong Feng and Ming Li: Contributed reagents, materials, analysis tools or data.Chan-juan Zou, Guang Xu, Chong-gao Zhou; Contributed reagents, materials, analysis tools or data.All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xia, R., Ma, T., Zhao, F. et al. The efficacy analysis of laparoscopic-assisted Soave procedure for Hirschsprung’s disease in neonates and infants within 3 months of age. Sci Rep 14, 31924 (2024). https://doi.org/10.1038/s41598-024-83422-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83422-3